Back to Journals » Patient Preference and Adherence » Volume 16
Establishing Quality of Life in Southern Taiwan COPD Patients Using Long-Acting Bronchodilator
Authors Chin PQ, Sheu CC , Tsai JR, Chang HL, Lee LY, Chen CY
Received 21 December 2021
Accepted for publication 19 March 2022
Published 5 April 2022 Volume 2022:16 Pages 875—886
DOI https://doi.org/10.2147/PPA.S355023
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Pik-Qi Chin,1,* Chau-Chyun Sheu,2,3 Jong-Rung Tsai,4,5 Hsu-Liang Chang,6 Li-Yao Lee,7,* Chung-Yu Chen1,7,8
1Master Program in Clinical Pharmacy, School of Pharmacy, Kaohsiung Medical University, Kaohsiung, Taiwan; 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan; 3Department of Internal Medicine, School of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan; 4Division of Respiratory Therapy, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan; 5Department of Internal Medicine, Kaohsiung Municipal Cijin Hospital, Kaohsiung, Taiwan; 6Department of Internal Medicine, Kaohsiung Municipal Ta-Tung Hospital; Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 7Department of Pharmacy, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan; 8Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
*These authors contributed equally to this work
Correspondence: Chung-Yu Chen, Master Program in Clinical Pharmacy, School of Pharmacy, Kaohsiung Medical University, No. 100, Shihcyuan 1st Road, Sanmin District, Kaohsiung, 80708, Taiwan, Tel +886-7-3121101 ext 2375, Fax +886-7-3210683, Email [email protected]
Background: To assess the health-related quality of life (HRQoL) of Taiwan patients with different stages of chronic obstructive pulmonary disease (COPD) and using different combination therapies and to explore the factors affecting HRQoL in these patients.
Methods: This cross-sectional study included outpatient participants aged 35 years old and older who were receiving long-acting bronchodilator treatment in one of two hospitals in Southern Taiwan. Participants were categorized according to their Global Initiative for Obstructive Lung Disease (GOLD) classification as either their COPD group, based on symptoms and exacerbation risk, or their COPD stage, based on spirometry results. Patients’ HRQoL was assessed using the St. George’s Respiratory Questionnaire score (SGRQ), World Health Organization Quality of Life Quality of Life-BREF (WHOQOL-BREF), and EQ-5D-5L. The total scores of the SGRQ, WHOQOL-BREF, EQ-5D utility index, and EQ-VAS were presented as mean ± standard deviation (SD) among different combination treatments. Univariate and multivariate analyses were used to explore the association of patients’ baseline characteristics and environmental factors with HRQoL.
Results: A total of 218 patients were enrolled in the study. The distribution of patients using GOLD group classification were as follows: 73.39% in group A, 20.19% group B, 1.83% group C and 4.59% group D. Triple therapy patients mostly showed a lower quality of life than other combination therapies, regardless of the GOLD classification system. However, only the SGRQ scores of GOLD groups A and B were significantly different when using different drug combinations (p-value = 0.0072 and 0.0430, respectively). The COPD assessment test (CAT) score, a questionnaire to assess impact of COPD on health status, was found to be associated with all the questionnaires.
Conclusion: The HRQoL is impaired in patients with COPD, and it deteriorates with an increase of severity. The CAT was the strongest predictor of HRQoL.
Keywords: chronic obstructive pulmonary disease, long-acting bronchodilators, health-related quality of life, risk factors, Taiwan
Introduction
Chronic obstructive pulmonary disease (COPD) is a common but complex lung disease that has gained high attention due to its high morbidity and mortality worldwide. The World Health Organization (WHO) has estimated COPD to be the third leading cause of death by 2030.1 The prevalence of COPD is expected to increase over the next 40 years, and according to WHO estimations, COPD and other respiratory diseases may contribute to 4.6 million deaths annually by 2060.2 In Taiwan, the estimated prevalence of COPD is 6.1% in adults aged ≥ 40 years.3 COPD is usually associated with a progressive airflow limitation due to chronic inflammation of the airways and lungs. As the disease progress, patients suffer more from symptoms, including dyspnea, sputum production, cough, wheezing, and chest tightness. Such symptoms may lead to exercise intolerance and a limitation in physical activities, thereby affecting the health-related quality of life (HRQoL).4
Treatment goals of COPD are to improve the quality of life, reduce symptoms, and the risk of exacerbations and mortality.5 According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines of 2020,4 the treatment regimen for each individual varies according to their condition, based on the severity of their symptoms and risk of exacerbations. Inhaled bronchodilators are the mainstays of pharmacological treatment.6 Studies had shown that new dosage forms or new drugs, such as indacaterol/glycopyrronium, have a better therapeutic effect and lung function improvements than that of traditional treatments.7,8 Previous local studies focused on COPD and its comorbidities;9 thus, there is a lack of local studies focusing on the quality of life in patients with COPD. To the best of our knowledge, there are no studies that classified measured quality of life using drugs.10–12
Therefore, we conducted a cross-sectional study by collecting data on the quality of life in Taiwan patients with COPD when using different combination of drugs, including LABA monotherapy, LAMA monotherapy, LABA/LAMA, LABA/ICS, and LABA/LAMA/ICS. We aimed to (1) establish local patients’ COPD data according to GOLD guidelines classification, COPD groups based on symptoms and exacerbation risk, and COPD stages based on the forced expiratory volume in one second (FEV1) score alone, and to (2) investigate the factors affecting the quality of life in these patients.
Methods
Study Population
Participants with COPD were identified using the International Classification of Disease (ICD-9: 490–492; ICD-10: J44.0, 44.1, 44.9). Participants included outpatients aged 35 years old and older who were diagnosed with COPD before the index date and who had been using any long-acting bronchodilators for more than one month. The index date of the study was the day the participant filled out the questionnaires. Patients with lung cancer, a life expectancy less than three months, without recognition, who were diagnosed before index date but did not use any long-acting bronchodilator more than one month, who required supplementary oxygen equipment, or with insufficient data for analysis were excluded.
Participants were recruited from a medical center, Kaohsiung Medical University Hospital (KMUH) and a regional hospital, Kaohsiung Da-Tung Hospital between September 2020, and April 2021. The study was conducted according to the Declaration of Helsinki was approved by the Institutional Review Boards of KMUH Ethics Committee (KMUHIRB-E(II)-20200044), and all participants provided written informed consent.
HRQoL Measurement
The HRQoL was captured by three instruments: St George’s Respiratory Questionnaire (SGRQ), World Health Organization Quality of Life-BREF (WHOQOL-BREF), and Euro Qol 5D (EQ-5D-5L). Previous studies have suggested that disease-specific and generic health status questionnaires should be used together to achieve the most holistic picture of the overall burden of COPD on patients’ quality of life.13,14 All three measurements were in the traditional Chinese version and had been validated by local researchers.15–17
The self-administered SGRQ consists of 50 items divided into three components that measure activity limitation, symptoms, and social functioning.17 SGRQ has several scales, including dichotomous and 4-Likert scales. Each item is weighted according to the severity of each component. An excel-based scoring calculator, obtained through the SGRQ score developer, was used to calculate the three SGRQ component scores and the total score. The scoring Program adjusts for up to 24% of missing items in the questionnaire. Overall scores range from 0–100, where a higher score represents a poorer quality of life.
The WHOQOL-BREF Traditional Chinese version is a 28-item self-administered questionnaire that comprises four domains, including physical, physiological, environmental, and social,15 and also two individually scored items regarding an individual’s overall perception of quality of life and general health. Each question score ranges from 0–5. In this questionnaire, the domain score is the average of the item scores in the same domain multiplied by four, thus each domain ranged from 4–20 accordingly. Responses from the two items of the Overall Quality of Life and General Health were calculated as a single score with a range of 4–20. The higher the score, the higher the quality of life.
EQ-5D-5L is a self-administered questionnaire that consists of two parts––the descriptive system and the EQ visual analog scale (EQ-VAS). The descriptive part measures the fives dimension of health (self-care, mobility, usual activities, anxiety/depression, and pain/discomfort) with five levels (no problems, slight problems, moderate problems, severe problems, and extreme problems). The health states can be derived into a utility index according to Taiwan’s value set.16 EQ-VAS is a vertical axis that ranges 0–100 that represents the patients’ perception of their overall health.
In this study, the total scores of the SGRQ, overall WHOQOL-BREF, EQ-5D-5L utility index, and EQ-VAS score were presented as the mean ± SD among different combination treatments.
Study Design
All eligible participants were referred by physicians. The study aim, methods, and consent form contents were explained clearly to the eligible participants by researchers before inclusion. The questionnaires were filled out only after the consent form was completed and signed. The estimated questionnaire response time was 20–30 minutes. Study patients were allowed to fill out the questionnaire independently on the index date. An evaluator internal to the research was available to answer any questions the study patients may have had throughout the questionnaire process. Each participant filled out only one of each questionnaire.
Comorbidities and Covariables
Demographic data were collected through the questionnaires and medical records. Patients’ demographics one year before the index date were retrieved from their medical records. Information on age, sex, smoking status (non-smoker, past smoker, and current smoker), vaccination history (pneumococcal vaccination and influenza vaccination), lung function data (forced expiratory volume in one second [FEV1], forced vital capacity [FVC], oxygen saturation [SpO2], and respiratory rate [RR]), the COPD Assessment Test (CAT) results, and the Modified British Medical Research Council (mMRC) questionnaire were collected. Lung function data within one year of the index date were retrieved through medical reports. The CAT is a simple, self-administered questionnaire that evaluates the impact of COPD on health status.18 The CAT score is classified as low (<10), medium (10–20), high (21–30), and very high (>30) based on the impact level of disease.19 The Modified British Medical Research Council (mMRC) questionnaire can be used to determine symptoms, health status, and mortality risk.4 An increasing mMRC score reflects high symptom burden and impaired HRQoL. Comorbidities, such as hypertension, hyperlipidemia, malignancy, congestive heart failure, coronary artery disease, and others, were also retrieved.
The air pollution data used in this study were collected through Environmental Protection Administration Executive Yuan Taiwan.20 The air pollution exposure of each participant was estimated based on the nearest monitoring station located by their residence. The mean concentrations of PM 2.5 and other pollutants, including sulfur dioxide (SO2), ozone (O3), nitrogen dioxide (NO2) and carbon monoxide (CO) were recorded at the (i) Index date, and (ii) 1 day, (iii) 7 days, (iv) 14 days, and (v) one year before the index date.
Sensitivity Analysis
The sensitivity analysis was conducted by changing the exposure period of air pollutants at 1, 7, and 14 days, and one year before the index date to detect the association of different exposure periods of air pollutants with the quality of life.
Statistical Analysis
For baseline demographics, normally distributed continuous variables, such as age, lung function and others, are presented as mean and SD, while categorical variables are presented as absolute numbers and percentages. Questionnaire scores are presented as mean + SD. The difference between groups was analyzed using the Kruskal–Wallis test for the three groups above and the Mann–Whitney U-test when comparing two groups.
The level of agreement between the three sets of questionnaires was determined using Spearman correlation coefficient. A Spearman correlation coefficient (rho, rs) range higher than 0.701 indicated a strong correlation; a rs range between 0.301 to 0.700 represented a moderate correlation; and a rs range smaller than 0.300 was defined as weak correlation.21 Univariate analysis was first used to investigate any potential predictors affecting the HRQoL of patients with COPD. Variables with a p-value < 0.05 according to the univariate analysis, the mean concentration of air pollutants, and variables regarded as clinically relevant, such as age and body mass index (BMI), were subjected to multivariate analysis to identify important factors associated with HRQoL.
Data processing was performed in Microsoft Excel, while statistical analysis was carried out in SAS 9.4 software. Statistical significance was determined for p-values < 0.05.
Results
Participant Characteristics
Figure 1 shows the flow chart of the study enrollment. Of the 232 eligible patients, 218 patients were included in our study. Table 1 shows the characteristics of the study population. Most of the patients were male and past smokers, with a mean age of 69.6 years old. Clinical characteristics showed a mean dyspnea severity score of 1.19, a mean CAT score of 6.6, and an exacerbation risk of 0.1 in recent years. The distribution of COPD stages according to the spirometry results was as follows: 23.3% in GOLD stage 1, 49.1% in GOLD stage 2, 23.4% in GOLD stage 3, and 4.1% in GOLD stage 4. Using the latest GOLD classification, 73.4%, 20.2%, 1.8%, and 4.6% were classified as group A–D, respectively.
 |
Table 1 Baseline Characteristics of COPD Population |
 |
Figure 1 Flow chart of chronic obstructive pulmonary disease population. |
Relationship Between Questionnaires
There was a significant negative, moderate correlation between the utility index and SGRQ total score (rs = −0.4). EQ-VAS and all SGRQ scores were negatively correlated (rs = −0.3 to −0.4), with moderate strength. The strength of the relationships varied from weak to moderate between SGRQ domains and EQ5D dimensions. Furthermore, the utility index and EQ-VAS were positively correlated with the WHOQOL-BREF overall score (rs = 0.4 and rs = 0.4, respectively). All WHOQOL-BREF domains were significant correlated to the EQ5D dimensions, except for EQ5D-Mobility and WHOQOL-Social relationships.
HRQoL in COPD Patients
The utility indexes derived from the EQ-5D-5L and EQ-VAS scores were recorded as a mean of 0.9 and 67.4, respectively. The mean SGRQ total score was 21.4, and ranged from 0 to 86.7, while the mean WHOQOL-BREF overall score was 12.3, ranging from 4.0 to 20.0. These data showed a relatively high quality of life in patients with COPD who were using long-acting bronchodilators.
HRQoL in COPD Patients According to GOLD Group Classification
Table 2 shows the mean of the utility index, EQ-VAS, SGRQ total score, and WHOQOL-BREF overall score of patients in groups A to D with different drug combinations. Most patients in group A were treated with LABA+LAMA (46.3%), followed by LABA+LAMA+ICS (18.8%), ICS+LABA (15.6%), LAMA (14.4%), and LABA (5.0%). The SGRQ total score was the only questionnaire to show a significant difference among the different drug combination in group A, (p < 0.01). Group B patients were mostly treated with dual and triple therapy. There was a decreasing trend in the utility index and EQ-VAS scores obtained in this group of patients. Similar to group A patients, the SGRQ total score increased, which represented a lower HRQoL from ICS+LABA to LABA+LAMA+ICS therapy. Additionally, the SGRQ total score had a significant difference among different combination treatments (p < 0.04).
 |
Table 2 Health-Related Quality of Life in Group A–D Patients |
Only four patients were classified into group C in this study. Two patients were treated with LABA+LAMA, one with LAMA, and the other one with LABA+LAMA+ICS. The SGRQ scores also increased with the number of drugs used. Due to the small sample size in this group, the results were used as a reference only. Ten patients were classified in group D with combination therapy of LABA+LAMA and LABA+LAMA+ICS. Patients treated with triple therapy had higher EQ-VAS and WHOQOL-BREF scores, and a lower SGRQ score though there was no statistically significant difference among the two groups.
HRQoL in Patients According to Their GOLD Stage Classification
Participants were reclassified into GOLD Stages I to IV for further analysis (Table 3). Among the 51 participants in GOLD stage 1, 4 were LABA users, 8 were LAMA users, 12 were ICS+LABA users, 22 were LABA+LAMA users, and 5 were LABA+LAMA+ICS users. The SGRQ total score was lowest in the LAMA users (8.89 ± 10.34) and highest in the LABA+LAMA+ICS users (22.67 ± 9.72). Most GOLD stage 2 patients were treated with LABA+LAMA therapy. The mean total scores for each questionnaire were not significantly different among different combination therapies.
 |
Table 3 Health-Related Quality of Life in GOLD Stage 1–4 Patients |
Among the 51 patients in GOLD stage 3, only 1 patient used a monotherapy (LAMA), 4 were ICS+LABA users, 19 were LABA+LAMA users, and the remaining 27 patients were LABA+LAMA+ICS users. The LABA+LAMA+ICS group had a higher SGRQ total score (33.79 ± 19.55) than the other groups. The lowest utility, EQ-VAS, and WHOQOL-BREF overall scores were also found in the LABA+LAMA+ICS group. There was no statistical difference among the groups. Nine patients were considered to be in the very severe stage of GOLD classification. These patients were either treated with LABA+LAMA or LABA+LAMA+ICS. No significant difference was found among the two groups.
Factors Associated with the HRQoL
Table 4 outlines the results of the regression analysis for utility, EQ-VAS, SGRQ, and WHOQOL-BREF on the COPD population. Results of the univariate regression analysis showed that the potential factors associated with scores obtained varied among different instruments. The results of multivariate regression demonstrated the important factors affecting each measurements’ score. The model shows that with every increase of standard deviation (SD) in the CAT, the utility index decreased by 0.35 SDs (p < 0.001). With an increase of one standard deviation in the mMRC, the utility index decreased by 0.20 standard deviations (p = 0.02). Compared with patients without chronic kidney disease (CKD), those with CKD scored 0.09 points lower in the utility index when other variables were considered (p = 0.02). With an increase of one SD in the CAT, the EQ-VAS score decreased by 0.37 standard deviations (p < 0.0001). On the other hand, one SD increase in BMI led to a 0.14 SD increase in the EQ-VAS score (p = 0.03). Patients who had ever smoked scored 3.37 points lower for the EQ-VAS compared to those who had never smoked (p = 0.01). The stepwise multivariate analysis only pooled out the CAT and FEV1 to be correlated when other variables were controlled. For every one SD increase in the CAT, the SGRQ total score increased by 0.57 (p < 0.0001). A one SD increase in FEV1 led to a 0.22 SD decrease in the SGRQ total score (p < 0.0001). Besides age and CAT, the WHOQOL-BREF overall score was also found to be correlated with PM 2.5 concentration. Every one increase in the environmental factor PM 2.5 concentration at the index date decreased the WHOQOL-BREF overall score by 0.17 standard deviations in (p = 0.06).
 |
Table 4 Regression Analysis for Utility, EQ-VAS, SGRQ and WHOQOL on COPD Population |
Sensitivity Analysis
Table 5 shows the sensitivity analysis results of factors associating the WHOQOL-BREF overall score with different exposure periods of air pollutants. Age and CAT were significantly associated with the WHOQOL-BREF overall score in all exposure periods. When changing the exposure period of air pollutants, only the mean NO2 concentration 1 and 7 days before the index date were correlated with the WHOQOL-BREF overall score (p = 0.01 and 0.03, respectively).
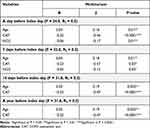 |
Table 5 Sensitivity Analysis of Factors Associating WHOQOL Overall Score with Different Exposure Periods of Air Pollutants |
Discussion
In this cross-sectional study among patients with COPD, we found that the distribution of patients enrolled varied among grouping systems. LABA+LAMA+ICS users had a lower quality of life compared to other combination therapies, regardless of their GOLD group classification or GOLD stage classification. The findings proposed that patients’ baseline characteristics (age, BMI and CKD comorbidity) and clinical characteristics (CAT scores, mMRC dyspnea score and FEV1) are the main factors affecting the HRQoL in patients with COPD.
The mean utility of the COPD population was 0.9, indicating that this patient population had high satisfaction in their level of physical, mental, and social functioning. A study conducted by local researchers reported a mean utility of 0.9458 in the general population.22 However, the study only included patients between 20–64 years old, while the mean age of our study population was 69.6 ± 10.4, which may have decreased the mean utility index. Such results may prove that the usage of long-acting bronchodilators in patients with COPD can improve their health status by helping them to live a normal life as the general population. As this is the first report of the utility index in the Taiwan COPD population, there is a need to collect further domestic data to improve understanding and for comparison.
Most patients in this study had a GOLD stage 2 classification (49.1%), in accordance with a previous study.23 Moreover, most had an FEV1 between 50% and 80%. However, when classified according to symptoms and exacerbation history, most patients were in group A (73.4%), followed by groups B, D, and C (20.2%, 4.6%, and 1.8%, respectively). This distribution was similar to that found in a Norway study comparing the discrimination ability of different GOLD classifications.24 However, another local study found the GOLD group distribution to be 23.3%, 63.2%, 1.9% and 11.6% in groups A, B, C, and D, respectively.25 Comparing the baseline characteristics of both studies, we noted that our study enrolled patients with lower CAT scores and mMRC scores, which indicates lower respiratory symptoms in the COPD population, thus impacting the distribution between studies.
The quality of life among patients using LABA+LAMA+ICS was lower compared to that of patients using other combination treatments in groups A and B. Though the EQ-VAS score was slightly higher in triple therapy patients than that of LABA monotherapy and LABA+LAMA patients, there was no significant difference. However, there was a significantly higher SGRQ total score, which indicates a lower quality of life in the triple therapy patients compared with the other treatment groups. In contrast, Lutter et al26 investigated the relationship of ICS use with clinical and functional outcomes and concluded that ICS treatment led to improvements in generic quality of life, such that there might be a subgroup of patients in groups A and B who experienced l benefits when treated with ICS. The difference in the results may be due to a few reasons. The classification of patients into A/B differed between the studies; while Lutter et al used the mMRC score, we classified patients according to the CAT or mMRC score. Next, the study included other ICS treatments, including LABA+ICS and LAMA+ICS users in ICS treatment groups. However, it should be noted that LAMA+LABA+ICS patients comprised the majority (72%) of the study. The results of our study are commensurate with previous research27 that had found potential overuse of LABA+LAMA+ICS therapy in those who were not recommended use by current GOLD guidelines. This indicates that there is a need for further attention and investigation on the use of triple therapy. The study findings provided only an overview of this issue, as information, such as medication switching and usage of oral corticosteroids, were not recorded or analyzed.
Previous studies have compared the health status of patients using a particular long-acting bronchodilator with those using an active comparator or placebo.28–32 Some studies divided patients into subgroups of GOLD stages; however, most studies pooled the results of all patients without considering their disease severity. Huijsmans et al33 investigated the clinical utility of GOLD classification based on COPD disease severity; however, they focused on pulmonary rehabilitation not on long-acting bronchodilators. A pooled analysis involving dual bronchodilators concluded that dual therapy showed more consistent benefits in the GOLD III/IV group than in the GOLD I/II group; however, the study focused only on group B patients classifying them into gold stage I–IV.34 This was the first study to investigate the effect of long-acting bronchodilators on health status by stage and group.
Our study findings found that only the SGRQ total score showed a trend of deterioration in the HRQoL with the increase in COPD severity. The SGRQ questionnaire has been used to measure the effect of pharmacology treatment on respiratory health quality of life as well as the health status when treated by non-pharmacological treatments, such as pulmonary rehabilitation.35 Moreover, differences identified as clinically important by the SGRQ questionnaire have been proven to reflect associations of clinical importance.36 Thus, the establishment of an EQ-5D-adjusted utility based on the SGRQ score may obtain a more precise utility index of the COPD population. Although a previous study invented a model to predict EQ5D utility using SGRQ total score,37 it used United Kingdom population preferences; thus, there is a need to develop an algorithm based on Taiwan population for a better prediction.
Interestingly, we found that the CAT was the strongest predictor of HRQoL in COPD patients. Magdalena Brandi et al38 found a negative association of CAT with SF-12, another generic questionnaire. Another study reported good correlations between the CAT and SGRQ total score (r = 0.7, p < 0.0001).39 Yet, all evidence indicates that the CAT is a good indicator, regardless of the questionnaire used during the HRQoL assessment.
COPD is usually associated with exposure to cigarette smoke, environmental particles, and other noxious gases. However, this is the first study to evaluate the association between exposure period and the HRQoL of COPD patients. The sensitivity analysis reported that only the daily mean concentration of NO2 at 1 and 7 days before the index day were associated with the WHOQOL-BREF score. Previous studies showed that lung function performance is affected by concentrations of air pollutants in the days before taking the test in asthmatic patients.40 As air pollutants are also common COPD triggers, the result of that study can be used as an indirect comparison with our study. Both results indicate that a short-term exposure may have effects on health status.
This study did have some limitations that should be acknowledged. First, because of the cross-sectional study design we could not determine the causal relationship between HRQoL and patient characteristics. Second, the small sample size of the study may have resulted in insufficient power, leading to difficulty in detecting important differences across the GOLD group and stage classification. Finally, as the area of the study was focused on Southern Taiwan, the results may not be extrapolated to the whole Taiwan COPD population.
Conclusion
The study showed that the HRQoL is impaired in patients with COPD, and it deteriorates with increase in severity. The mean utility index derived from the Taiwan value set was 0.86 in COPD patients, which means that using long-acting bronchodilators may help patients improve their health status to that of the general population. The HRQoL was significantly lower in those treated with triple therapy patients in groups A and B. However, there was no significant difference among combination therapies according to the GOLD stage classification. The findings of our study found that the strongest predictor of HRQoL appeared to be CAT. Short-term exposure to certain air pollutants may also an important factor affecting the HRQoL in COPD patients. Based on our findings, we would recommend future studies to include in-hospital patients for a more comprehensive understanding of the HRQoL of Taiwan patients with COPD.
Data Sharing Statement
Corresponding author (Prof. Chung-Yu Chen) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgments
We thank physicians of Kaohsiung Medical University and Da-Tung Hospital for their efforts in referring patients. Thanks are also extended to nurses of both hospitals for helping me approach COPD subjects. Pik-Qi Chin and Li-Yao Lee contributed equally to this work and should be considered co-first authors for this study.
Funding
The research reported in this publication was supported by grant from Kaohsiung Medical University Hospital (KMUH109- M925) and Kaohsiung Medical University (KMU-S109032).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Portegies MLP, Lahousse L, Joos GF, et al. Chronic obstructive pulmonary disease and the risk of stroke. The Rotterdam Study. Am J Respir Crit Care Med. 2015;193(3):251–258. doi:10.1164/rccm.201505-0962OC
2. World Health Organization. Projections of mortality and causes of death, 2016 to 2060. Available from: https://www.who.int/healthinfo/global_burden_disease/projections/en/.
3. Cheng SL, Chan MC, Wang CC, et al. COPD in Taiwan: a national epidemiology survey. Int J Chron Obstruct Pulmon Dis. 2015;10:2459–2467. doi:10.2147/copd.S89672
4. Vogelmeier C, Anzueto A, Barnes P. Global strategy for diagnosis, management and prevention of COPD 2021 update. Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf.
5. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease NHLBI/WHO workshop report. Review. Rev Port Pneumol. 2001;7(6):621–667.
6. Gary TF, Make B. Stable COPD: initial pharmacologic management. UptoDate. 2019.
7. Moretz C, Sharpsten L, Bengtson LG, et al. Real-world effectiveness of umeclidinium/vilanterol versus fluticasone propionate/salmeterol as initial maintenance therapy for chronic obstructive pulmonary disease (COPD): a retrospective cohort study. Int J Chron Obstruct Pulmon Dis. 2019;14:1721–1737. doi:10.2147/COPD.S204649
8. Frampton JE. Qva149 (indacaterol/glycopyrronium fixed-dose combination): a review of its use in patients with chronic obstructive pulmonary disease. Review. Drugs. 2014;74(4):465–488. doi:10.1007/s40265-014-0194-8
9. Chen YF, Cheng YC, Chou CH, Chen CY, Yu CJ. Major comorbidities lead to the risk of adverse cardiovascular events in chronic obstructive pulmonary disease patients using inhaled long-acting bronchodilators: a case-control study. BMC Pulm Med. 2019;19(1):233. doi:10.1186/s12890-019-0999-z
10. Chuang HY, Chang H, Fang YY, Guo SE. The effects of threshold inspiratory muscle training in patients with chronic obstructive pulmonary (COPD) disease: a randomized experimental study. J Clin Nurs. 2017;26:4830–4838. doi:10.1111/jocn.13841
11. Lan CC, Yang MC, Huang HC, et al. Serial changes in exercise capacity, quality of life and cardiopulmonary responses after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Heart Lung. 2018;47(5):477–484. doi:10.1016/j.hrtlng.2018.06.006
12. Liou HL, Huang YT, Lai ZY, et al. Improving self-care efficacy and quality of life with a self-management program among patients with chronic obstructive pulmonary disease: a quasi-experimental study. Nurs Health Sci. 2020;22(3):629–638. doi:10.1111/nhs.12703
13. Engström CP, Persson LO, Larsson S, Sullivan M. Health-related quality of life in COPD: why both disease-specific and generic measures should be used. Eur Respir J. 2001;18(1):69–76. doi:10.1183/09031936.01.00044901
14. Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27(3 Suppl):S217–32. doi:10.1097/00005650-198903001-00018
15. Yao G, Chung CW, Yu CF, Wang JD. Development and verification of validity and reliability of the Whoqol-Bref Taiwan version. J Formos Med Assoc. 2002;101(5):342–351.
16. Lin H-W, Li C-I, Lin F-J, et al. Valuation of the Eq-5d-5l in Taiwan. PLoS One. 2018;13(12):e0209344. doi:10.1371/journal.pone.0209344
17. Wang KY, Chiang CH, Maa S, Shau Y-W, Tarn YH. Psychometric assessment of the Chinese language version of the St. George’s respiratory questionnaire in Taiwanese patients with bronchial asthma. J Formosan Med Assoc. 2001;100:455–460.
18. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
19. Ghobadi H, Ahari SS, Kameli A, Lari SM. The relationship between COPD assessment test (cat) scores and severity of airflow obstruction in stable COPD patients. Tanaffos. 2012;11(2):22–26.
20. Air quality monitoring data. Available from: https://data.epa.gov.tw/dataset?q=%E7%A9%BA%E6%B0%A3%E5%93%81%E8%B3%AA.
21. Biswas M, Chattopadhyay K. Relationship between health-related quality of life and respiratory health status among coal-based sponge iron plant workers in Barjora, India. J Public Health (Bangkok). 2018;26(3):355–359. doi:10.1007/s10389-017-0861-9
22. Yu ST, Chang HY, Yao KP, Lin YH, Hurng B-S. Validity of Eq-5d in general population of Taiwan: results of the 2009 national health interview and drug abuse survey of Taiwan. Qual Life Res. 2015;24(10):2541–2548. doi:10.1007/s11136-015-0978-7
23. Criner RN, Labaki WW, Regan EA, et al. Mortality and exacerbations by global initiative for chronic obstructive lung disease groups ABCD: 2011 versus 2017 in the Copdgene® cohort. Chronic Obstruct Pulmon Dis. 2019;6(1):64–73. doi:10.15326/jcopdf.6.1.2018.0130
24. Bhatta L, Leivseth L, Mai X-M, et al. Gold classifications, COPD hospitalization, and all-cause mortality in chronic obstructive pulmonary disease: the hunt study. Int J Chron Obstruct Pulmon Dis. 2020;15:225–233. doi:10.2147/COPD.S228958
25. Hsieh MJ, Huang SY, Yang TM, et al. The impact of 2011 and 2017 global initiative for chronic obstructive pulmonary disease (gold) guidelines on allocation and pharmacological management of patients with COPD in Taiwan: Taiwan obstructive lung disease (told) study. Int J Chron Obstruct Pulmon Dis. 2018;13:2949–2959. doi:10.2147/copd.S176065
26. Lutter JI, Jörres RA, Trudzinski FC, et al. Treatment of COPD groups gold A and B with inhaled corticosteroids in the cosyconet cohort - determinants and consequences. Int J Chron Obstruct Pulmon Dis. 2021;16:987–998. doi:10.2147/copd.s304532
27. Cataldo D, Derom E, Liistro G, et al. Overuse of inhaled corticosteroids in COPD: five questions for withdrawal in daily practice. Int J Chron Obstruct Pulmon Dis. 2018;13:2089–2099. doi:10.2147/COPD.S164259
28. Singh D, Jones PW, Bateman ED, et al. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combinations compared with individual components and placebo in patients with COPD (Acliform-COPD): a multicentre, randomised study. BMC Pulm Med. 2014;14:178. doi:10.1186/1471-2466-14-178
29. Feldman G, Maltais F, Khindri S, et al. A randomized, blinded study to evaluate the efficacy and safety of umeclidinium 62.5 Μg compared with tiotropium 18 Μg in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:719–730. doi:10.2147/COPD.S102494
30. Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. doi:10.1056/NEJMoa0805800
31. Dahl R, Chung KF, Buhl R, et al. Efficacy of a new once-daily long-acting inhaled Beta2-agonist indacaterol versus twice-daily formoterol in COPD. Thorax. 2010;65(6):473–479. doi:10.1136/thx.2009.125435
32. Donohue JF, Maleki-Yazdi MR, Kilbride S, Mehta R, Kalberg C, Church A. Efficacy and safety of once-daily umeclidinium/vilanterol 62. 5/25mcg in COPD. Respir Med. 2013;107(10):1538–1546. doi:10.1016/j.rmed.2013.06.001
33. Huijsmans RJ, de Haan A, ten Hacken NN, Straver RVM, Van’t Hul AJ. The clinical utility of the gold classification of COPD disease severity in pulmonary rehabilitation. Respir Med. 2008;102(1):162–171. doi:10.1016/j.rmed.2007.07.008
34. Kang J, Lee JS, Lee SW, Lee JB, Oh Y-M. Dual versus monotherapy with bronchodilators in gold group B COPD patients according to baseline Fev1 level: a patient-level pooled analysis of phase-3 randomized clinical trials. Respir Res. 2021;22(1):55. doi:10.1186/s12931-021-01648-5
35. Sciriha A, Lungaro-Mifsud S, Scerri J, Magro R, Camilleri L, Montefort S. Health status of COPD patients undergoing pulmonary rehabilitation: a comparative responsiveness of the Cat and Sgrq. Chron Respir Dis. 2017;14(4):352–359. doi:10.1177/1479972317694622
36. Weatherall M, Marsh S, Shirtcliffe P, Williams M, Travers J, Beasley R. Quality of life measured by the St George’s respiratory questionnaire and spirometry. Eur Respir J. 2009;33(5):1025. doi:10.1183/09031936.00116808
37. Starkie HJ, Briggs AH, Chambers MG, Jones P. Predicting Eq-5d values using the Sgrq. Value Health. 2011;14(2):354–360. doi:10.1016/j.jval.2010.09.011
38. Brandl M, Böhmer MM, Brandstetter S, et al. Factors associated with generic health-related quality of life (HRQOL) in patients with chronic obstructive pulmonary disease (COPD): a cross-sectional study. J Thorac Dis. 2018;10(2):766–775. doi:10.21037/jtd.2018.01.122
39. Ringbaek T, Martinez G, Lange P. A comparison of the assessment of quality of life with Cat, Ccq, and Sgrq in COPD patients participating in pulmonary rehabilitation. Copd. 2012;9(1):12–15. doi:10.3109/15412555.2011.630248
40. Luttmann-Gibson H, Dockery DW, Speizer FE. Short-term and long-term effects of air pollution on lung function. Epidemiology. 2004;15(4):S42. doi:10.1097/00001648-200407000-00096
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
