Back to Journals » Journal of Multidisciplinary Healthcare » Volume 8
Establishing a framework for building multidisciplinary programs
Authors Meguid C, Ryan C, Edil B, Schulick R, Gajdos C, Boniface M, Schefter T, Purcell W, McCarter M
Received 15 September 2015
Accepted for publication 14 October 2015
Published 2 December 2015 Volume 2015:8 Pages 519—526
DOI https://doi.org/10.2147/JMDH.S96415
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Cheryl Meguid,1 Carrie E Ryan,2 Barish H Edil,1 Richard D Schulick,1 Csaba Gajdos,1 Megan Boniface,1 Tracey E Schefter,3 W Thomas Purcell,4 Martin McCarter1
1Department of Surgery, Division of GI, Tumor, and Endocrine Surgery, Section of Surgical Oncology, University of Colorado Hospital, Aurora, CO, 2Morsani College of Medicine, University of South Florida, Tampa, FL, 3Department of Radiation Oncology, University of Colorado Denver, Denver, CO, 4Department of Medicine, Division of Medical Oncology, University of Colorado Hospital, Aurora, CO, USA
Abstract: While most providers support the concept of a multidisciplinary approach to patient care, challenges exist to the implementation of successful multidisciplinary clinical programs. As patients become more knowledgeable about their disease through research on the Internet, they seek hospital programs that offer multidisciplinary care. At the University of Colorado Hospital, we utilize a formal multidisciplinary approach across a variety of clinical settings, which has been beneficial to patients, providers, and the hospital. We present a reproducible framework to be used as a guide to develop a successful multidisciplinary program.
Keywords: multidisciplinary clinic, patient centered, tumor board
Introduction
Today, many hospitals are promoting a health care system that is patient centered, in which the patients are actively involved in their personal care and treatment plan. From a patient’s perspective, the ideal health care setting includes input on his or her specific disease process from a multidisciplinary panel of expert specialty providers. Because of this, providers are leaving the traditional silo mentality of patient care behind and focusing more on the multidisciplinary approach. This is quickly evolving into the preferred method of treatment for complex diseases and cancers.1–5
Nowadays, multidisciplinary care is becoming more widely utilized in many major health care centers. Many tumor boards function as a type of multidisciplinary conference, which have in attendance a variety of specialty providers who discuss their own patient cases and then relay that information back to the patient.6 Unfortunately, this leads to a significant amount of unbillable physician time, including the conference itself and the subsequent conversation between the provider and the patient. In addition, the group’s recommendations are usually communicated to the patient over the phone, which results in challenges in coordinating the prescribed care. Alternatively, some patients have to follow-up with their physician in the clinic following review at the tumor board, resulting in frustrating delays in treatment initiation.
A newer, more formalized approach is a combination of weekly clinic and conference. This approach utilizes a clinic visit spread out over 1 day or 2 days in which the patient is scheduled for radiographic studies, laboratory tests, history and physical (H&P) examination, and consultations with members of the hospital support services (eg, a registered dietician and a social worker). Ultimately, after being reviewed by the expert multidisciplinary team in the conference, the patient meets all of the specialists who will be involved in his or her care. Although research on the impact of this approach is limited, data are suggestive of improved outcomes. For example, the Pancreatic Cancer Center at the Johns Hopkins Hospital found a 24% change in the recommended management based on a clinical review of their cases by the multidisciplinary team.7,8
At the University of Colorado Hospital, we utilize this formal approach in multiple clinical settings for complex diseases and cancers. To date, we have used this multidisciplinary model to build five successful clinics: Pancreas and Biliary; Esophageal and Gastric; Colorectal Cancer and Hyperthermic Intraperitoneal Chemotherapy (HIPEC); Liver and Neuroendocrine Tumor (NET); and Thoracic Oncology. Programs currently in development with this model include sarcoma, bladder cancer, orthopedic limb salvage, peripheral artery disease, and neuro-oncology.
Building a multidisciplinary program takes a significant amount of time and coordination from all those involved. However, we have found that the upfront effort is worth the clinical and financial benefits it offers to patients, providers, and health care systems. In order to better prepare hospitals in implementing this model, we have developed a reproducible framework that can be used as a guide to help ensure a successful multidisciplinary program (Figure 1).
  | Figure 1 Steps to building a multidisciplinary program. |
Model
Develop a business plan
The first step in building a multidisciplinary program is to create a business plan that can be used to provide hospital administration with a vision of the multidisciplinary program and market share analysis of the specific disease type the multidisciplinary program will be focusing on. The business plan should provide current data of that disease, including historic and current institutional clinic volumes, procedures, and surgeries performed as well as the projected growth of these metrics with respect to hospital operating margins. The business plan should start with a detailed description of the multidisciplinary program and also include upfront costs, anticipated financial revenue, and ideas for marketing and outreach.
Obtain physician/administrative buy-in
The next step is to secure buy-in from the physician and hospital administrators. It is paramount to establish commitment from the participating physicians and their clinical leaders from the outset of the program as they are essential to the success of the multidisciplinary clinic. The clinic requires at least one assigned representative from each specialty to be present at the weekly conference. The hospital administration decides the majority of details regarding the use of hospital resources and funding, such as salary support for the program coordinator. Other considerations for funding include provision of food at the conferences (usually held early morning or at noon) and annual cost of providing continuing medical education (CME) hours. Although the latter may initially serve as an incentive for regular participation by key stakeholders, the anticipated and realized increase in the clinical volume will soon eclipse this fringe benefit.
Obtain hospital support
Many resources are utilized during the multidisciplinary clinic and conference and should be negotiated and agreed upon by stakeholders ahead of time to ensure its success. These include:
- Use of a conference room with availability of the necessary and appropriate technology, such as a computer with access to the hospital’s radiology imaging program for the radiologist, a microscope with projection capabilities for the pathologist, and multiple screens or projectors for viewing the diagnostic data.
- Clinic schedulers who can schedule the initial and associated clinic appointments for patients with providers.
- Multiple clinic rooms allocated to the patient population for the clinic.
- Ancillary staff, including medical assistants and front desk staff, to check in, room, and obtain required vital signs, height, weight, and initial intake information (allergies, medication reconciliation, and family history) of each patient.
Hire the multidisciplinary clinic coordinator
It is critical to hire a full-time dedicated coordinator to run the multidisciplinary program. This ensures a dedicated and consistent point of contact for in-house hospital referrals, outside referrals, and associated referring providers and patients. This initial contact is where patients and providers are educated on the disease process and what the clinic entails. Ideally, the program coordinator is a broadly trained advanced practice provider (APP) (nurse practitioner [NP] or doctor of nursing practice [DNP], physician assistant [PA], or clinical nurse specialist [CNS]). Specialty-trained nurses, such as a Certified in Care Coordination Transition Management Registered Nurse (CCCTM RN) and a nurse navigator, are also potential candidates as they have advanced training in care coordination, which is crucial in this role.
Coordinate scheduling logistics
Once commitment from the institution has been made and the program coordinator has been hired, the next step is to specify scheduling logistics. Establishing the time and location of the multidisciplinary clinic requires consideration of prior established clinic and conference schedules. Scheduling conflicts should be acknowledged and handled promptly; however, some providers may have to compromise to make the rotating multidisciplinary schedules work successfully. In our experience, pathologists and radiologists who were staffing early-morning tumor boards appreciated moving to a noon conference offering CME hours and lunch. Each multidisciplinary clinic will have an individualized schedule depending on which diagnostic studies are necessary for the multidisciplinary team to make an informed decision about the treatment. Two examples of clinics with different scheduling needs are as follows.
In our Esophageal and Gastric Multidisciplinary Clinic, an endoscopic ultrasound (EUS) is routinely required to determine esophageal cancer staging. Since the patients require sedation for EUS, the multidisciplinary clinic is run over 2 days. On day 1, the patients are scheduled for any necessary radiographic examination (such as positron emission tomography-computed tomography [CT], or magnetic resonance imaging), laboratory studies, and H&P examination by the program coordinator. Should an EUS be required to complete staging, patients are scheduled for that procedure in the afternoon. On day 2, the multidisciplinary conference is held from 7 to 8 am. Patients then meet all of the specialists who will be involved in their care at 8 am. Following the specialists, all patients have the opportunity to meet the members of the hospital support services, such as a dietician and a social worker.
In our Pancreas and Biliary Multidisciplinary Clinic, patients are seen over a 1-day clinic visit. In the morning, patients are scheduled for radiographic examinations, laboratory studies, H&P examination by the program coordinator, and meetings with hospital support services. The multidisciplinary conference is held at noon, concurrent with patients breaking from meetings for lunch. This is followed by the patients meeting with all of the specialists who will be involved in their care.
As noted earlier, there are several participating departments involved within each multidisciplinary clinic throughout the patient appointments. Therefore, several key factors need to be in place in order to run an efficient clinic each week. One top priority was to reserve “slots” in radiology and gastroenterology to guarantee availability to the program coordinators should they need to add on patients with minimal notice. It is important to have a meeting with the schedulers and managers in radiology and gastroenterology to establish how communication between the program coordinator and all schedulers will be relayed each week. The pathology staff prepares and reviews all specimen slides for review at the conference. Therefore, it is important to meet with this group to establish routes of communication with the program coordinator.
Regarding provider scheduling, we utilize an Intake and Access Coordinator who schedules all provider appointments during the conference once we determine which provider(s) will see each patient. Our Intake and Access Coordinators are also crucial in obtaining medical records, pathology slides, and radiology disks as well as in assisting with insurance authorization to ensure everything needed for the specialists to make a plan is available at the time of the clinic’s review conference.
Provider schedule
Obtaining a schedule in advance listing all of the involved physicians is done to ensure a hosting physician from each specialty is present every week. We use a rotating physician assignment to even the work load across all specialty providers. This schedule is also helpful when scheduling patients who have been directly referred to a specific physician or when scheduling restaging patients to confirm they will be seeing the same team they met on prior visits. Our master schedule of providers is created at least 3 months in advance.
Support services
Utilization of support services is an important component of each patient’s comprehensive treatment plan. Depending on the disease process, the type of support services required for each patient population will vary. Our multidisciplinary clinics offer the following services for each patient: social work, registered dietician, tobacco cessation treatment, financial counselor, patient support and education groups, American Cancer Society patient navigator, genetic counseling, psychology, integrative medicine, and palliative care. The majority of these services are provided free to patients at our institution. If pastoral or spiritual care is requested, we are able to accommodate this on an as-needed basis.
The use of support services for each multidisciplinary clinic varies. For example, in the Pancreas and Biliary Multidisciplinary Clinic and the Colorectal Cancer and HIPEC Multidisciplinary Clinic, we offer a 30-minute combined registered dietician and social worker discussion before the patient goes to lunch. If a patient does not wish to participate in the group discussion, we are able to accommodate his or her needs and offer an individual appointment in the afternoon. In our Liver and NET Multidisciplinary Clinic, because of the various needs of these patient populations, appointments with these services are offered during the H&P examination and the patients meet one-on-one with them before lunch.
Patient flow template
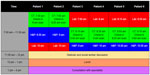
Developing a patient flow template is useful in structuring each patient’s appointments associated with the clinic visit. In the Pancreas and Biliary Multidisciplinary Clinic, a template for six patients is used weekly so that the coordinator can easily schedule a patient for the whole day’s clinic appointment using the reserved radiology slots in a manner that flows smoothly with the other appointments that day (Figure 2).
Weekly handout
Every week, a handout should be created by the coordinator, which lists each patient to be discussed in clinic that week. A description of each patient’s clinical course to date is described in detail, including, but not limited to, pertinent past medical history, radiology, endoscopy, and pathology reports. This handout is useful for the providers to refer to when the patient is presented during the conference. The day prior to the conference, the handout is distributed electronically to the entire team for review, if so desired. It also helps the radiologists and pathologists to prepare for the conference by reviewing each patient’s imaging and pathology slides ahead of time.
Meeting the patient and welcome folders
In the morning of the multidisciplinary clinic, it is beneficial for the coordinator to greet each patient at his or her starting destination to present them with a welcome folder that includes a letter describing the layout and listing of appointments for the day (Figure 3). We understand that patients may be delayed to their H&P examination by radiology or laboratory testing and hence tell each patient to focus more on the flow of the appointments rather than focusing on the times they are scheduled. This is because the timing of the H&P examination is simply logistical and made based on a clinic scheduling template to avoid double booking. We are always able to accommodate our patients for the H&P examination, as we block out 9–11.30 am and room them as they arrive. While this is not necessarily needed, it has proved to be a positive and reassuring start for the patient and his or her family. The welcome folder also includes a map of the facility, showing where each visit is located (including radiology, phlebotomy, and the clinic), and a handout from the University of Colorado Cancer Center, describing various details such as locations of the cafeteria, the Cancer Resource Center, and the pharmacy. A letter from our cancer center support services is also included, which allows patients to see the services offered.
  | Figure 3 Welcome letter. |
Mock day
Shortly before the opening of the multidisciplinary clinic, it is important to prepare a mock conference to look for obstacles that may be encountered on the day of the clinic. We recommend test running of the pathologist’s microscope, all computers, TV screen, and/or projector and making sure conference call systems are functioning and able to be set up.
Tracking patients
When each patient is scheduled, it may be possible to “flag” each patient who comes through the multidisciplinary clinic. This is dependent on the hospital’s electronic health record and only important if there is a need to capture and track patient visits for financial reasons, growth, or other purposes.
Marketing
In anticipation of the multidisciplinary clinic opening, an upfront marketing strategy is best. As mentioned earlier, nowadays, patients are utilizing the Internet more in deciding where to get the treatment. More specifically, patients are learning about specific centers for treatment through online blogs and social media; therefore, a strong webpage presence is essential. It is important for the website to clearly list the contact number of the multidisciplinary coordinator, as this makes it much easier for patients to navigate the health care system, and provide a “face” with a name. Patients also find the website helpful if it has educational content on the webpage, describing the disease and treatment options available at the facility. Along with a website, creating a brochure for referring providers is important in describing the unique and cutting-edge procedures offered by the clinic. The brochure should also emphasize that by the end of the day, the patients are seen by all of the specialists who will be involved in their treatment plan, as this is an important component of the multidisciplinary program and a major benefit for patients. Another marketing strategy includes creating an easy access phone number for patients and referring providers to call. This can be a toll-free number, which is dedicated to the clinic and easy to place on the brochure and hospital website. Having a successful marketing campaign greatly impacts the recruitment and retention of patients.
Community outreach
Physicians within the specialties participating in the multidisciplinary program should be encouraged to take part in outreach discussions or presentations with potential referring physicians and practice groups. Participation in national or local support group events, such as survivor groups, helps promote recognition of the multidisciplinary program within the local community.
Data collection
Starting a new clinical program is a great opportunity to collect data for future research and tracking such as volume growth (visits, surgical procedures, and referrals to other specialists), demographic information, and change in diagnosis identified during workup in the clinic. Keeping track of information such as utilization of radiology and review of pathology slides is useful to refine resource allocation and determine downstream revenue acquired through the multidisciplinary program, as this may be helpful in the future when justifying resources to support the program. Keeping a list of all the patients who have undergone surgery is a useful resource for future patients who may want to discuss “patient-to-patient” details regarding that surgery.
Other recommendations
Once the multidisciplinary clinic is established and running, allow room for change and change as needed. The multidisciplinary coordinator should continue to work with all participating departments so that the patient flow remains seamless. It is also important to maintain communication with all contributing disciplines for better coordination of care. Keeping this information in mind will help address barriers before they become impediments to the success of the program.
Multidisciplinary coordinator – benefits of hiring an APP or a specialty-trained RN
The benefits of hiring an APP (NP, DNP, PA, or CNS) or a specialty-trained RN (CCCTM or nurse navigator) are considerable. APPs are licensed providers with the ability to examine patients, prescribe medications, and write orders. Utilizing an NP, a DNP, a PA, or a CNS will greatly decrease the time needed from physicians for triaging, ordering diagnostic testing for patient workup, and performing the H&P examination prior to the conference. Similarly, specialty-trained RNs have a high level of skill and training in process and systems management, which are valuable skills needed to be a successful multidisciplinary coordinator. While the cost of supporting an APP or a specialty-trained RN is higher than that of, for example, a medical assistant, the added costs are made up by this enhanced efficiency in coordinating patient care. Dedicating the coordinator to one multidisciplinary program allows that person to become an expert in his or her field, which is useful when discussing the plan of care with patients or referring physicians. Moreover, APPs are able to bill for their clinic consultations, which is financially advantageous for the institution.
Benefits for patients
Patients benefit greatly from a multidisciplinary approach to care. Often, we find a change in diagnosis or detection of other abnormalities on review of the CT scan, pathology, or other diagnostic tests. The 1-day model is helpful for patients traveling from afar who otherwise would have to make several trips to the hospital to see the various specialists. Furthermore, since each patient’s treatment plan is decided among all specialists, any discordance is avoided, further streamlining patient care. As a result of cohorting provider visits, patients are only charged one facility fee during their visit, limiting costs otherwise associated with multiple visits to specialists. A documentation of the tumor board discussion and treatment plan is available in the electronic medical record as well, unlike many tumor board discussions. Since our APP coordinators review patients in advance and therefore guide appropriate workup prior to arrival of the patient, redundant testing is avoided and the majority of patients leave the clinic with a specific coordinated plan for their treatment. Finally, having a dedicated coordinator for the multidisciplinary program is valuable for patients who have a hard time navigating the complex health care system and can rely on a familiar face during their workup and treatment.
Benefits for providers
Multidisciplinary programs provide many benefits for the physicians involved. Having the attendance of multiple specialists from each discipline leads to dynamic discussion and learning opportunities for all, especially students and trainees. During the multidisciplinary conference, the specialists who are seeing patients that day are appreciative of having complete patient histories, diagnostic testing, and pertinent procedures completed ahead of time so that a finalized plan can be established rapidly. At our hospital, CME hours are earned for each multidisciplinary conference attended. Referring providers are also grateful of the ability to quickly schedule patients into the clinics, with a goal of being seen in less than five business days.
Benefits for the hospital
Multidisciplinary programs are beneficial for the hospital as well. Multidisciplinary care not only attracts new patients to be evaluated by our comprehensive approach, but it also brings in the ancillary income associated with pathology review and diagnostic testing that may be missed if patients were merely being referred to individual providers for treatment such as surgery or chemotherapy alone. In addition, this has allowed our center to become a site for “destination care”. We find many patients travel from out of state to receive the benefits of our program; however, we support the delivery of appropriate care (such as neoadjuvant or adjuvant chemotherapy) to be given closer to home by the patient’s local health care provider whenever possible. In addition, we provide the referring provider with a comprehensive update on diagnosis and recommended treatment plan for patients.
Conclusion
Today, fewer patients with complex diseases are being treated with single-modality therapy. Instead, they are being diagnosed and treated with a combination of multiple specialists, including surgery, chemotherapy, radiation therapy, interventional radiology, and gastroenterology. At the University of Colorado Hospital, we have developed several multidisciplinary programs as described earlier. These have proven to be successful in increasing the satisfaction of both the patient and provider and beneficial for patients and providers involved, as evidenced by patient testimonials via hospital satisfaction surveys and discussion with providers. These programs are run over 1 day or 2 days, with the patient undergoing diagnostic testing early on and ending with a consultation with the specialists involved and departing with a coordinated and detailed plan regarding next steps in their care.
In order to ensure a successful launch of a multidisciplinary clinic, we have developed a reproducible framework to be used as a guide. We hope that this framework limits barriers and enhances collaboration when building a new program.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006;296(23):2848–2851. | |
Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20:600–607. | |
Barry MJ, Edgman-Levitan S. Shared decision making – the pinnacle of patient-care. N Engl J Med. 2012;366(9):780–781. | |
Perlin JB, Kolodner RM, Roswell RH. The veterans health administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10:828–836. | |
Epstein RM, Street RL. The values and value of patient-centered care. Ann Fam Med. 2011;9:100–103. | |
Fleissig A, Jenkins V, Catt S, Fallowfield L. Multidisciplinary teams in cancer care: are they effective in the UK? Lancet Oncol. 2006;7:935–943. | |
Wright FC, DeVito C, Langer B, Hunter A. Multidisciplinary cancer conferences: a systematic review and development of practice standards. Eur J Cancer. 2007;43:1002–1010. | |
Pawlik TM, Laheru D, Hruban RH, et al. Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Ann Surg Oncol. 2008;15(8):2081–2088. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.