Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Epidermal Cyst on the Scalp Induced by Forceps Injury During Delivery: A Case Report and Epidemiological Analysis of 3949 Patients
Authors Liu M , Liu X , Wang Y, Wang Z , Tuo H, Feng Y, Zheng Y
Received 9 December 2022
Accepted for publication 1 February 2023
Published 8 March 2023 Volume 2023:16 Pages 593—601
DOI https://doi.org/10.2147/CCID.S399372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Meng Liu,1,* Xinyi Liu,1,* Yuqian Wang,1 Ziyang Wang,1 Huihui Tuo,1 Yiguo Feng,2 Yan Zheng1
1Department of Dermatology, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, People’s Republic of China; 2Department of Dermatology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yiguo Feng, The Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, People’s Republic of China, Email [email protected] Yan Zheng, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, People’s Republic of China, Email [email protected]
Background: Epidermal cysts are common benign epithelial tumors. They are known to result from penetrating-type injuries or infection of human papillomavirus. The differential diagnosis commonly includes multiplex steatocystoma, lipoma, and neurofibroma. Pathological examination is essential for diagnosis, and surgical excision is the recommended treatment.
Objective: We report a case in a man who presented with a cystic lesion on the scalp over 22 years to provide clinical evidence for mechanism of epidermal cysts. We conducted epidemiological analysis of 3949 patients with epidermal cysts to clarify the epidemiological characteristics and clinical features of epidermal cysts.
Patients and Methods: A total of 3949 individuals with confirmed epidermal cysts were collected for analysis. Data were expressed as mean ± SEM and analyzed using Student’s t-test.
Results: Our data showed that the mean age of diagnosis of males was statistically earlier than that of females (P< 0.001), but no significant difference in sex predilection was observed (P=0.55). The high incidence age of males and females was in the young and middle stage. Lesion locations were a bit different among age groups, but the face was the most common site of epidermal cyst at all age stages.
Conclusion: Our case offers clinical evidence to the theory which refers trauma as one of the main causes of epidermal cysts in hair-bearing area. According to analysis of large number of samples, we can further support the idea that epidermal cyst has equal sex predilection and mainly occurs on the young and middle-aged adults. It is usually solitary and most likely to be found on face and trunk.
Keywords: epidermal cysts, etiology, epidemiological analysis, treatment
Introduction
Epidermal cysts, also known as keratin cyst, are common benign intradermal tumors, which are induced by invagination of keratinized squamous epithelium into dermis.1,2 Epidermal cyst often occurs in middle age without obvious sex preference. The cysts are characterized by smooth, dome-shaped, moveable and firm swellings, growing slowly and varying in size from few millimeters to a few centimeters.3,4 Such cysts can occur anywhere in the body, including scalp, face, neck, trunk, limbs and perineum.2,5,6 Etiologically, the trauma to the pilosebaceous units gives rise to epidermoid cysts in the hair-bearing area. In areas without hair, the mechanism of epidermal cyst development is related to epidermal inclusion secondary to trauma or human papillomavirus infection.3,7
We report a case of epidermal cyst on the scalp with trauma on the same site caused by forceps delivery at his birth, which further indicates the mechanism of epidermal cysts that develop after trauma. Moreover, we analyzed 3949 patients’ data of our department from 2011 to 2019 to identify the epidemiology characteristics of epidermal cyst.
Materials and Methods
Study Population
A total of 3949 cases reported by the Department of Dermatology, the Second Affiliated Hospital of Xi’an Jiaotong University, from January 27, 2011 to December 27, 2019 were collected for analysis. Informed consent was taken from all the patients before surgery. The clinical details, including gender, age and sites, were achieved from the record systems of our hospital. Accurate diagnosis of all patients was confirmed by histopathological examination.
Statistical Analysis
Data were expressed as mean ± SEM. Data analysis was performed using GraphPad Prism (version 8; GraphPad Software, La Jolla, CA) and the SPSS 23.0 software (SPSS Inc, Chicago, IL). Student’s t-test was used for Statistical comparisons. P<0.05 was considered statistically significant.
Results
Case Report
A 22-year-old man developed a painless swelling with a depression on his scalp. At his birth, his scalp was pinched by forceps and a scalp lesion developed, which gradually developed into this swelling and slowly growing in 22 years. On examination, a 3×4 cm soft and movable mass was noted on the top of his scalp, upon which was a round depression with a diameter of 2 cm (Figure 1). The lesion was successfully removed. Histopathological examination showed that the epidermis was normal and a cystic cavity was observed in the dermis. The cyst was lined by stratified squamous epithelium and contains a clear stratum granulosum. The cavity was filled with laminated keratin materials (Figure 2). Based on these features of histopathological sections, a diagnosis of an epidermoid cyst was made.
 |
Figure 1 Well-defined swelling with a depression on the top of the scalp. |
Epidemiological Analysis
In our study, 3949 cases of epidermal cysts were included. The number of diagnosed patients was increased by year (Table 1). Males accounted for 55.53% of the total number, and women accounted for 44.47%. There was no significant difference in sex ratio (P = 0.554 > 0.05). The age of the patients was relatively large, ranging from 10 months to 93 years. The total age of patients showed right skewed distribution with the mean age of 37.60 years and the median age of 34 years (Figure 3). As shown in Table 2 and Figure 4, the highest incidence in both groups was observed in the age group of 20–29 years (26.69%, 1054/3949) followed by age groups of 30–39 (21.80%, 861/3949) and 40–49 (15.35%, 606/3949) years, respectively. The mean age of diagnosis of males (36.59±16.57) was statistically earlier than that of females (38.85±17.30, P<0.001).
 |
Table 1 Number and Mean Age Distribution of Patients with Epidermal Cyst for Year |
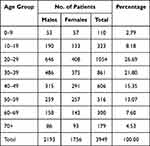 |
Table 2 Age and Sex Difference of Patients with Epidermal Cyst |
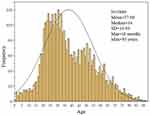 |
Figure 3 Age skewed distribution of patients with epidermal cyst (skewness=0.474). SD, standard deviation. |
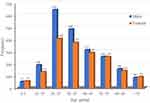 |
Figure 4 Age and sex difference of patients with epidermal cyst. |
We further analyzed the locations of epidermal cyst in 2793 cases. Here we show several epidermal cysts in different locations (Figure 5). The result showed that face (50.19%, 1405/2783) was the most common affected region in all age groups, followed by trunk (24.87%, 692/2783), neck (11.14%, 310/2783), limbs (6.83%, 190/2783), scalp (3.34%, 93/2783) and perineum (3.34%, 93/2783). Moreover, the rate of face in affected region showed a downward and then upward trend by age (Table 3 and Figure 6). The most uncommon sites observed in our study were all found in male patients, three in the palm and one in the sole of feet.
 |
Table 3 Age and Site Difference of Patients with Epidermal Cyst |
 |
Figure 5 Typical lesions in different sites. (A) Scalp. (B) Face. (C) Neck. (D) Trunk. (E) upper limb. (F) Palm of hand (G) Ventral of penis. (H) Great lips of pudendum. (I) Sole of foot. |
 |
Figure 6 Different lesion’s location of patients with epidermal cyst. |
Discussion
Epidermal cyst, also known as atheroma, is a common benign cystic lesion that originates from the infundibular portion of the hair follicle. Therefore, they mainly occur on hair-bearing area. The main causes of epidermal cysts are trauma, surgical operations and chronic irritation.8–11 Skolnik et al have reported multiple epidermal inclusion cysts on the plantar surface of the foot in patients after radiofrequency microtenotomy for plantar fasciitis.11 Guler et al reported a pediatric patient who developed penile epidermoid cysts after distal hypospadias surgery.12 A case reported a patient who developed a giant epidermal cyst on the upper lip after wearing a denture, suggesting that chronic irritation may be the cause of the epidermal cyst.10 Cases of epidermoid cysts after tattoo and radiotherapy have also been reported.13,14 In our case report, the patient presented with an epidermal cyst on the scalp. After a thorough history, the patient and his family indicated that he had been injured by forceps at birth in the same area and immediately developed a rupture on the scalp, which gradually healed after 1 week, but a swelling appeared at the site of this skin lesion. The patient denied any history of other trauma, medication or physical therapy at the site of his epidermal cyst. Because the forceps injury and the epidermoid cyst appeared at the same site and in the same period, and no other possible predisposing factors were identified, we reasonably concluded that the forceps entrapment was the cause of the epidermoid cyst in this patient. The case provides supports to the theory that trauma induces the development of epidermal cysts.
The incidence of epidermal cysts is mostly in young and middle-aged people. It has been reported that there is no difference in incidence between men and women.3 In our study, the most affected age is 20–29 years (26.69%, 1054/3949), and the mean age of diagnosis of males (36.59±16.57) is statistically younger than that of females (38.85±17.30). Although there are more male patients than female patients each year, no significance is observed in terms of sex ratio. The number difference between men and women patients is likely to be caused by willingness to seek medical treatment of patients in different gender.
Epidermal cyst is usually solitary. Multiple epidermal cysts are rare and maybe manifestation of Gardner’s syndrome.15 Consistently, we analyzed 2793 cases, of which only 40 cases (1.43%) have more than one cystic lesion but no more than three cysts. Epidermal cysts can be located in any part of the body, and mainly on the face, torso, extremities and scalp.1,2 In the present study, face is the most common site of the cyst, followed by trunk, neck, limbs, scalp and perineum. Difference in the distribution of epidermal cysts between men and women is not observed, but it lies in different age groups. Face is the most affected parts in all age groups, but the rate of face affected is lowest in 30–39 years. We supposed that this tendency may be related to the changes of ratio (face area/ body surface area) in different age groups.
Epidermal cyst is a common skin disease that can be complicated by infection, rupture, calcification and malignancy.16,17 Shah et al showed that in 20 cases of scrotal calcinosis, the etiology was traced to epidermoid cysts in 14 cases.17 Chronic and repeated irritation, infection, ultraviolet radiation, and immunosuppression may become the triggers of epidermoid cyst malignancy.18–22 HPV infection may also be associated with malignant transformation, and cases of squamous cell carcinoma of the skin caused by HPV-associated cysts have been reported by Pusiol et al.23 According to the literature, cutaneous squamous cell carcinoma is the most common among the malignant cases of epidermal cysts, accounting for about 70%–90%, second is cutaneous basal cell carcinoma.18,20,24 The possibility of malignant transformation should be warned when the existing epidermal cysts become hard in texture, pain, secretion, inflammation, bleeding, rapid increase in size, and refractory infection. Currently, routine surgical excision is not recommended for the removal of epidermoid cysts due to their slow growth, asymptomatic and low malignancy rate. However, surgical excision is recommended when the lesions are painful, when large lesions interfere with daily life and when there is a possibility of malignant transformation.18,25,26 Faltaous et al performed an wide excision without additional radiotherapy or chemotherapy in a patient with epidermal cyst transformed into squamous cell carcinoma of the skin, and the patient had no complications and good wound healing after surgery.26 Harada et al reported a patient with cutaneous basal cell carcinoma arising from an epidermal cyst, which was reviewed 2 years after extensive excision was performed with no evidences of recurrence, confirming surgical excision is an effective treatment for epidermoid cysts and their malignancy.20 The surgical excision should remove as much of the cystic membrane as possible to reduce the possibility of recurrence. Epidermoid cysts that are inflamed but not infected can be treated with intralesional drainage injection of triamcinolone acetonide to alleviate inflammation.27 All surgically removed cysts should undergo careful pathological examination to determine the presence of malignancy.18,26 Skroza et al reported systemic isotretinoin treatment at a dose of 0.5 mg/kg/day for 5 months in a patient with squamous cell carcinoma of the skin arising from an epidermoid cyst, who showed 70% remission of the lesions and no signs of recurrence. Therefore, it can be presumed that systemic isotretinoin treatment is effective for squamous cell carcinoma derived from epidermal cysts.28 In addition, carbon dioxide laser and erbium-YAG laser can be used to treat small epidermal cysts.24,29–31
Conclusion
According to our case report and literature review, we considered trauma as one of the main causes of epidermoid cysts. The epidemiological data we provided proved that epidermoid cysts are prevalent in young and middle-aged people, with the face and trunk as the majority sites. There is no clear gender preference for the onset of the disease. In addition, although surgical treatment has good outcomes for epidermoid cysts, the existence of more effective and less invasive treatment methods still needs to be further explored.
Ethics Approval
All patients signed informed consent and consented to the publication of the article. Our project was ethically approved by Xi’an Jiaotong University.
Acknowledgments
We would like to thank Guanfei Zhang (Center for Mitochondrial Biology and Medicine, Xi’an Jiaotong University) for his help with data preparation and analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kirkham N. Tumors and Cysts of the Epidermis. Philadelphia, Pennsylvania, USA: Lippincott-Raven Publishers; 1997.
2. Singh M, Maheshwari B, Khurana N, Jain S. Epidermal inclusion cyst in breast: is it so rare? J Cytol. 2012;29(3):169–172. doi:10.4103/0970-9371.101165
3. Nigam JS, Bharti JN, Nair V, et al. Epidermal cysts: a clinicopathological analysis with emphasis on unusual findings. Int J Trichology. 2017;9(3):108–112. doi:10.4103/ijt.ijt_16_17
4. Lee KM, Park JH, Min KH, Kim EK. Epidermal cyst on the sole. Arch Plast Surg. 2013;40(4):475–476. doi:10.5999/aps.2013.40.4.475
5. Kumaraguru V, Prabhu R, Kannan NS. Penile epidermal cyst: a case report. J Clin Diagn Res. 2016;10(5):PD05–06. doi:10.7860/JCDR/2016/18246.7794
6. Pehlivan M, Ozbay PO, Temur M, Yilmaz O, Gumus Z, Guzel A. Epidermal cyst in an unusual site: a case report. Int J Surg Case Rep. 2015;8C:114–116. doi:10.1016/j.ijscr.2015.01.001
7. Gomi M, Naito K, Obayashi O. A large epidermoid cyst developing in the palm: a case report. Int J Surg Case Rep. 2013;4(9):773–777. doi:10.1016/j.ijscr.2013.06.003
8. Lincoski CJ, Bush DC, Millon SJ. Epidermoid cysts in the hand. J Hand Surg Eur Vol. 2009;34(6):792–796. doi:10.1177/1753193409347509
9. Vergles D, Horzic M, Cupurdija K, Lackovic Z, Vergles JM. Epidermoid cyst on top of the left arm thumb. Am J Dermatopathol. 2009;31(7):723–724. doi:10.1097/DAD.0b013e31818d0bec
10. Kim JC, Hong IP. Rare giant upper lip epidermal cyst in a patient wearing a denture. Arch Craniofac Surg. 2016;17(4):222–224. doi:10.7181/acfs.2016.17.4.222
11. Skolnik J, Pontious J, Hasenstein T. Development of multiple epidermal inclusion cysts after radiofrequency microtenotomy for plantar fasciitis: a case report. J Foot Ankle Surg. 2021;60(5):1088–1093. doi:10.1053/j.jfas.2021.03.017
12. Guler Y, Tatar Z, Ucpinar B, Erbin A. An epidermal cyst of the penis after distal hypospadias surgery: a case report. J Med Case Rep. 2018;12(1):378. doi:10.1186/s13256-018-1930-6
13. Koh MJ, Teo RY, Liu TT. Multiple epidermal cysts occurring in a tattoo. Singapore Med J. 2009;50(11):e376–377.
14. Lee A, Griffiths WAD. Multiple milia due to radiotherapy. J Dermatol Treat. 2002;13(3):147–149. doi:10.1080/09546630260199523
15. Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2009;67(1):52–57. doi:10.1016/j.joms.2007.05.023
16. Gupta R, Verma P, Bansal N, Semwal T. A Case of ruptured perineal epidermal cyst. Cureus. 2020;12(10):e11099. doi:10.7759/cureus.11099
17. Shah V, Shet T. Scrotal calcinosis results from calcification of cysts derived from hair follicles: a series of 20 cases evaluating the spectrum of changes resulting in scrotal calcinosis. Am J Dermatopath. 2007;29(2):172–175. doi:10.1097/01.dad.0000246465.25986.68
18. Park BS, Shin DH, Kim SH, Jung HJ, Son GM, Kim HS. Perineal squamous cell carcinoma arising from an epidermal cyst: a case report. World J Surg Oncol. 2018;16(1):155. doi:10.1186/s12957-018-1442-2
19. Sumi Y, Yamamoto N, Kiyosawa T. Squamous cell carcinoma arising in a giant epidermal cyst of the perineum: a case report and literature review. J Plast Surg Hand Su. 2012;46(3–4):209–211. doi:10.3109/2000656x.2012.677403
20. Harada T, Fukumoto T, Shimizu H, Nishigori C. Basal cell carcinoma developed from an epidermal cyst: a case report and review of the literature. Dermatol Reports. 2021;13(2):9273. doi:10.4081/dr.2021.9273
21. Veenstra JJ, Choudhry S, Krajenta RJ, Eide MJ. Squamous cell carcinoma originating from cutaneous cysts: the Henry Ford Experience and review of the literature. J Dermatolog Treat. 2016;27(1):95–98. doi:10.3109/09546634.2015.1054779
22. Al-Zawi ASA, Memon S, Shah A, Eldruki S, Tan E, Alowami SO. A squamous cell carcinoma arising from scrotal epidermal cyst. A case report and review of 94 cases from the world literature. Nowotwory J Oncol. 2019;69(3–4):150–156. doi:10.5603/njo.2019.0028
23. Pusiol T, Piscioli F, Zorzi MG. Squamous cell carcinoma arising from human papillomavirus associated cyst. Am J Dermatopathol. 2011;33(1):105–106. doi:10.1097/DAD.0b013e3181d77723
24. Tchernev G, Temelkova I, Yungareva I, Wollina U. Multiple epidermal cysts of the scalp: dermatosurgical approach with favourable outcome! Open Access Maced J Med Sci. 2019;7(9):1509–1511. doi:10.3889/oamjms.2019.257
25. de Mendonca JCG, Jardim ECG, Dos Santos CM, et al. Epidermoid cyst: clinical and surgical case report. Ann Maxillofac Surg. 2017;7(1):151–154. doi:10.4103/ams.ams_68_16
26. Faltaous AA, Leigh EC, Ray P, Wolbert TT, Rare A. Transformation of epidermoid cyst into squamous cell carcinoma: a case report with literature review. Am J Case Rep. 2019;20:1141–1143. doi:10.12659/AJCR.912828
27. Jakhar D, Kaur I. Intralesional drainage injection of triamcinolone acetonide for epidermal cyst. J Am Acad Dermatol. 2018;78(6):e149–e150. doi:10.1016/j.jaad.2017.12.008
28. Skroza N, Proietti I, Tolino E, et al. Isotretinoin for the treatment of squamous cell carcinoma arising on an epidermoid cyst. Dermatol Ther. 2014;27(2):94–96. doi:10.1111/dth.12062
29. Calderon-Castrat X, Santos-Duran JC, Roman-Curto C, Fernandez-Lopez E. Carbon dioxide laser: a therapeutic approach for multiple vulvar epidermoid cysts. Dermatol Surg. 2016;42(2):264–267. doi:10.1097/DSS.0000000000000614
30. Feng CJ, Ma H. Treatment of epidermal cysts with erbium:YAG laser fenestration: an alternative to surgical intervention. Ann Plast Surg. 2015;74(Suppl 2):S89–92. doi:10.1097/SAP.0000000000000463
31. Wollina U, Langner D, Tchernev G, Franca K, Lotti T. Epidermoid cysts - a wide spectrum of clinical presentation and successful treatment by surgery: a retrospective 10-year analysis and literature review. Open Access Maced J Med Sci. 2018;6(1):28–30. doi:10.3889/oamjms.2018.027
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

