Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 13
Epidemiology of Dermatophyte and Non-Dermatophyte Fungi Infection in Ethiopia
Authors Araya S , Tesfaye B, Fente D
Received 16 January 2020
Accepted for publication 31 March 2020
Published 8 April 2020 Volume 2020:13 Pages 291—297
DOI https://doi.org/10.2147/CCID.S246183
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Shambel Araya,1 Betelhem Tesfaye,2 Desalegn Fente1
1Department of Medical Laboratory Sciences, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Rank Higher Specialized Dermatology Clinic, Addis Ababa, Ethiopia
Correspondence: Shambel Araya Tel +251 939459529
Email [email protected]
Background: Dermatophytosis represents one of the common infectious diseases worldwide and it is a major public health problem around the globe. The disease causes considerable morbidity and still continues to increase especially in developing countries.
Objective: This study was undertaken to determine the prevalence of dermatophytes and the spectrum of fungal agents in patients attending Rank Higher Specialized Dermatology Clinic.
Methods: A cross-sectional study has been conducted, in which 318 samples from 318 suspected patients were collected. Samples include hair, nail, and skin. A portion of each sample was examined microscopically and the remaining portion of each sample was cultured onto plates of Sabouraud’s dextrose agar containing chloramphenicol with and without cycloheximide. Isolates were identified by studying the macroscopic and microscopic characteristics of the colonies.
Results: Tinea capitis was the predominant clinical manifestation accounting for 53.4% of the cases. Patients with age group 1– 14 years were more affected. Of 318 samples, fungi were detected in 133 (54.4%) by direct wet mount while 148/315 (46.5%) of them were culture positive. From these 72/148 (46.8%) were dermatophytes. T. tonsurans was the most common pathogen in tinea capitis, whereas T. mentagrophytes was the most common pathogen in tinea corporis. Among dermatophyte isolates, T. tonsurans 29/72 (40.2%) was the most common cause of infection. Among non-dermatophyte molds, Cladosporiumspp. 21/63 (33.3%) was predominant isolate followed by Neoscytalidim dimidatum 11/63 (17.4%) and Alternariaspp. 9/63 (14.2%), respectively. Yeasts also account for 13 (8.7%) of the total suspects of dermatophytosis.
Conclusion: In this study, the prevalence of dermatophytes was higher in tinea capitis 46/72 (63.8%) and T. tonsurans 29/72 (40%) was the dominant-isolated dermatophyte. Recovery of a large number of dermatophytes and non-dermatophyte fungi in our study showed that non-dermatophyte fungi are emerging as important causes of dermatophytosis warranting further intensive epidemiological studies that have public health significance are needed.
Keywords: dermatophytes, non-dermatophytes, dermatophytosis, fungi, infection
Background
Dermatophytosis represents one of the common infectious diseases worldwide and causes chronic morbidity, especially in developing countries.1 The condition is caused by dermatophytes, which are fungi that require keratin for growth. An increase in the incidence of dermatophytosis has been noted worldwide, especially in developing countries.2,3 Tinea capitis, an infection of the scalp, is one of the most common dermatophytosis and represents a major public health issue among children mainly in African and Caribbean regions.3,4
Dermatophytosis is a common public health problem and minor condition in Africa including Ethiopia. The distribution of these fungi varies considerably, depending on epidemiological factors and geographical area (4, 5, 6). T. rubrum, T. interdigitale, M. canis, M. gypseum, and E. floccosum are distributed worldwide. Other species have a partial geographic restriction, such as T. schoenleinii, T. violaceum and T. tonsurans are distributed in Eurasia and Africa; T. soudanense, distributed in Africa.7,8
Geographic location, health care, immigration, climate (temperature, humidity, wind, etc.), overcrowding, environmental hygiene culture, awareness to dermatophytes, age of individuals, hygiene and socioeconomic conditions have been described as major factors for these variations of dermatophyte epidemiology.9–12 Children’s between the ages of 4 and 16 years are more at risk due to more contact to different sources and inadequate amount of fungi-inhibiting fatty acids synthesized predisposed them to dermatophytic infections.13,14
Nowadays, there are about 52 known species in seven genera of dermatophytes.15 Of these species, about 20 species belong to the three most recognized and prevalent worldwide genera’s; Epidermophyton (1 species), Microsporum (3 species) and Trichophyton (16 species) and these genera’s are presently known to infect humans.12,15-17 Ethiopia is a developing nation located in the tropical region with a wet humid climate which makes it to fall into regions with a high prevalence of dermatophytosis.14,16 However, the distribution of pathogenic species and the predominating anatomical sites of infection vary with geographical location and change over time. The aim of this study was to determine the epidemiological and etiological fungal agents causing dermatophytosis regardless of the site of infection and age.
Methods
Study Areas and Population
A prospective cross-sectional institution-based study was carried out from January 2019 to June 2019 among dermatophytosis-suspected patients who visit Rank higher specialized dermatology clinic, Addis Ababa, Ethiopia.
Sample Size Determination and Sampling Technique
The required sample size of the study was determined using the formula for single population proportion and 318 study participants were included. A total of 318 clinical samples from 318 suspected patients (one sample from every patient based on their clinical manifestation) were collected from patients visiting the Dermatology clinic during the study period were included in the study.
Biological Sample Collection
Before collecting the sample, the infected area was cleaned with 70% (v/v) ethanol. Scraping samples from skin, nail, and finger-based on their clinical manifestation were collected aseptically using sterile blades and transferred into sterile plastic Petri-dishes. In tinea capitis suspects, dull broken hairs from the margin of the scalp lesion with forceps were sampled and transferred to sterile folded papers and transferred into sterile Petri dishes.
Culture and Microscopic Examination
A portion of each sample was mounted in a drop of 10% (w/v) potassium hydroxide on a clean microscopic slide. After 5 min, the mount preparation was examined under low (×10) and high (×40) power magnification for the presence of any fungal elements. The clinical sample was cultured onto Sabouraud’s dextrose agar plates containing chloramphenicol with and without cycloheximide (Oxoid, Basingstoke, England) prepared according to the instruction of the manufacturer. All inoculated plates were then incubated at an inverted position at 25–30°C for 4–6 weeks. Culture plates containing the Sabouraud’s dextrose agar were examined twice a week for any fungal growth. In the absence of growth during the 6th week, the results were considered negative. Those suspected colonies for dermatophytes were sub-cultured into potato dextrose agar (Oxoid, Basingstoke, UK) for the production of spores. Cultures of dermatophytes were identified by examining macroscopic and microscopic characteristics of their colony on Sabouraud’s dextrose agar. For the macroscopic identification, the rate of growth, texture, topography, and pigmentation of the reverse and front side of the culture were employed. Mold isolates were identified microscopically by placing pieces of the colony from Sabouraud’s dextrose agar and Potato Dextrose agar plates in to clean microscopic slide and stained using lactophenol cotton blue stain. Each preparation was observed microscopically after placing a coverslip. In addition,; the urease test was also used in differentiating between some members of Trichophyton species. For the identification of yeasts, conventional routine diagnostic methods, and chromogenic medium, CHROMagar Candida (bioMérieux, France) as per the instruction of the manufacturer were used. All ethical considerations were dully addressed and the study was conducted after the approval of the ethical review committee of Medical Laboratory science, college of health sciences, Addis Ababa University. Written consent was obtained from study subjects after ethical approval.
Statistical Analysis
Data were collected, double entered, cleaned and analyzed using SPSS version 20 software according to the study objectives. Frequency and percentage were used for investigation of the outcome.
Results
From the total of 318 clinical samples from suspected patients, 193 were females. The age of the study subjects ranged from 1 to 88 years with a mean age of 16 years. Among these, fungi were detected in 133/318 (41.8%) samples using potassium hydroxide wet mount while, 148 (46.5%) were culture positive (Table 1).
 |
Table 1 Correlation of Direct Microscopy with Culture (N=318) |
Tinea capitis was the dominant clinical manifestation 170/318 (53.4%) and this was more present in females than males 98/170 (74.5%). This was followed by tinea corporis and tinea unguium accounting for 30.50% and 16% of the cases, respectively (Table 2).
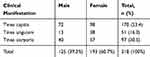 |
Table 2 Frequency and Distributions of Clinical Manifestations in Relation to Sex (N= 318) |
Dermatophytic infection rate was high in the age group of 1–14 years. Clinical manifestation in relation to age group was highest with age group <14, 144/318 (45.2%) followed by age group 25–44 years accounting for 96/318 (30.1%). Among 170 tinea capitis, 115/170 (67.6%) was found to be in patients age <14 years old and tinea corporis, the second-most clinical manifestation 97/318 (30.6%) was highest in patients of age group 25–44 years, 43/97 (44.3%). Tinea unguium was common in patients of age group of 25–44 years (Table 3).
 |
Table 3 Frequency of Clinical Manifestation in Different Age Groups (n=318) |
Tinea capitis was the predominant clinical manifestation accounting for 53.4% of the cases; of which 98 (57.6%) were females and 72 (42.4%) males. This was followed by tinea corporis and tinea capitis accounting for 30.5% and 16% of the cases, respectively (Table 4). According to species frequency in different areas of involvement, T. tonsurans was the most common pathogen in tinea capitis, whereas T. mentagrophytes was the most common pathogen in tinea corporis (Table 4).
 |
Table 4 Frequency and Distribution of Dermatophytes in Relation to Clinical Manifestation |
A total of 148/318 (46.5%) fungi were cultured from skin, hair and nail samples. Of these, 72/148 (48.6%) were dermatophytes, 63/148 (42.56%) non-dermatophyte molds and (13/148) 8.7% were yeasts. T. tonsurans 29/72 (40.2%) was the predominant dermatophyte followed by T. mentagrophytes 13/72 (18%) and M. audoouinii 13/72 (18%) whereas Trichophyton schoenleinii1/72 (1.3%) was the least common (Figure 1).
 |
Figure 1 Frequency and distribution of dermatophytes 2019, Addis Ababa, Ethiopia. |
Among non-dermatophyte molds Cladosporium spp. 21/63 (33.3%) was the predominant isolate followed by Neoscytalidim dimidatum 11/63 (17.4%) and Alternariaspp. 9/63 (14.2%), respectively. Cladosporiumspp., Neoscytalidim dimidiated, Alternariaspp. were the dominant isolates in tinea corporis, tinea unguium, tinea capitis, respectively. Yeasts were the least common isolates accounting 13 (8.7%) of the total suspects of dermatophytosis (Figure 2)
 |
Figure 2 Frequency and distribution of non-dermatophyte fungi 2019, Addis Ababa, Ethiopia. |
Discussion
Dermatophytosis is a major and common public health challenge in many parts of Africa.5–7,11,14 Accurate diagnosis based on the clinical symptoms alone is nearly impossible. Currently, the diagnosis of dermatophytosis in developing countries is confirmed by clinical examination and using microscopic and culture methods as conventional diagnostic tools.14,18,19 In the present study, direct microscopy positivity rate is 133/318 (41.8%) and culture positivity rate is 148/318 (46.5%) (Table 1). Earlier studies conducted in Addis Ababa, Ethiopia found that 42.6%, 74% and 85.2% culture-positive for dermatophytes.4,6,14 This occurrence is due to that; Ethiopia is a tropical country with wet humid climate, large population size, and low socioeconomic status and correlations between dermatological infections and low socioeconomic conditions, geographical locations, climate, overcrowding, health care, and hygiene have been demonstrated by many researchers.14,20,21
Tinea capitis was the most common clinical manifestations followed by tinea unguium and tinea corporis and this is in line with studies conducted in Addis Ababa, Ethiopia (4, 6, 14, 22). And this is due to low socioeconomic status, overcrowding and poor personal hygiene. T. tonsurans (56.5%), M. audouinii(17.3%), T. verrucosum (8.4%), and T. mentagrophytes (6.3%) were found the predominant causal agents of tinea capitis in this study. These findings seem to agree with the findings made by Tekleberhan et al,Raccurt et al, Enwean et al, and Al Shimma et al.3,14,23-25 The most susceptible persons to tinea capitis were patients 1–14 years old 115/170 (67.6%) and this is due to the inadequacy of natural protective fatty acids synthesized in their scalp among prepubescent children. Earlier, several authors have supported this finding.14,26,27 Many cases occurring in adults is involved with hormonal disorders resulting in carryover of tinea capitis from childhood or in patients with severe immune depression due to HIV/AIDS, leukemia, lymphoma, or treatment with immunosuppressant drugs.20,28,29
Tinea corporis (33/318) (10.8%) was the second-most common infection with a significant incidence among age groups of 25–44. The site of infection was mostly restricted to face and neck. T. mentagrophytes, T. rubrum, and M. audionii were the main causative agents and this is in line with a study conducted in Ethiopia.14,22,28
Tinea unguium 51/318 (16%) was observed mainly at the age of 25–44; 19/51 (30.1%) (Table 3). Several authors suggested that an increase in trauma rates, reduced growth rate of the ungual plate, poor peripheral circulation, frequent housework, cosmetic reasons and inability to maintain good nail care could be attributed to this manifestation.21,29,30
T. tonsurans 26/46 (56.5%) were the most abundant dermatophyte causing tinea followed by M. audouinii 8/46 (17.3%) and T. verrucosum 4/46 (8.6%). Even though it is not in line with the current finding; a similar study in Ethiopia showed that the prevalence of T. tonsurans in the rate of 5.8% and 18.4%.14,22 This discrepancy could be due to study area, immigration, population characteristics and a changing epidemiology from T. violaceum to T. tonsurans. These findings were similar to those obtained from previous studies in developing countries such as Kenya (33.3%), Egypt (31.5%) and Nigeria (29%).31–33 A similar study in India also reported T. tonsurans in the rate of 22.5%.34 This could be due to its ubiquitous in nature, abundance among human carriers, and social phenomena of today on the continent could explain T. tonsurans is circulating in the population.22–25,34,35
Non-dermatophyte molds were isolated from 63/148 (42.56%) cases, with Cladosporiumspp. as a major isolate accounting 21/63 (33.3%) of the total non-dermatophyte mold isolates followed by Neoscytalidium dimidiatum 11/63 (17.4%). A study in Addis Ababa, Ethiopia found a similar finding to our current study.22 Cladosporium species are the most widely spread fungi in the world. It is true also; most of the time appears as a contaminant. But some studies showed that they are associated as an opportunistic infection in subcutaneous and disseminated form, especially among immune-depressed individuals.14,22,37 Neoscytalidum dimidiated was isolated from skin and nail scrapings predominantly of toenails. Neoscytalidium dimidiatum and Scytalidium hyalinum are common causative agents of human superficial infections in different parts of the world, especially in tropical and subtropical regions.22 Similarly, yeasts were isolated from 13/148 (8.78%) cases with C. albicans as a major isolate accounting 5/13 (38.4%) of the total yeast isolated and this study was similar to a study conducted in Saudi Arabia.33 Non-dermatophyte fungi were isolated as a cause of dermatophytosis in many studies.14,18,36,38,39
Conclusion
This study showed that the prevalence of dermatophytosis was 46.5% but in developed countries, it was less than 5%8 which indicates that dermatophytosis is still a common problem in developing countries. Tinea capitis was identified as the most prevalent clinical presentation and children’s are the most vulnerable group. This study found that T. tonsurans was the most common etiologic agent followed by M.audoouinii and T.mentagrophyte. We recommend further research on the possible risk factors and spectrum for dermatophytes and non-dermatophyte molds in large clinical setting and the community.
Data Sharing Statement
The data sets used or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics and Consent Statement
Ethical clearance for this study was provided from Medical Laboratory science, college of health sciences, Addis Ababa University ethical review committee and the study was conducted in accordance with the declaration of Helsinki. Written informed consents were obtained from participants after ethical approval and we also explained to them the purpose of the study verbally. Assent form was completed and signed by family members and/or adult guardian for participants under the age of 18 years.
Acknowledgments
We thank Dr. Zemenu Tamir, Daniel Kahase for proofreading and revision of the manuscript. We are also thankful for the help of Dr. Adane Bitew and Addis Ababa University, Medical Laboratory Science department staffs for helping with the laboratory activities. We also thank the study participants.
Funding
The study was supported by Addis Ababa University, College of health science, department of medical laboratory science. The funder had no role in data collection, study design, data analysis and interpretation.
Disclosure
The authors declare that they have no financial or non-financial competing interests.
References
1. Ramaraj V, Vijayaraman RS, Rangarajan S, Kindo AJ. Incidence and prevalence of dermatophytosis in and around Chennai, Tamilnadu, India. Int J Res Med Sci. 2016;4(3):695700. doi:10.18203/2320-6012.ijrms20160483
2. Chepchirchir A, Bii C, Ndinya-Achola JO. Dermatophyte infections in primary school children in Kibera slums of Nairobi. East Afr Med J. 2009;86:59–68. doi:10.4314/eamj.v86i2.46934
3. Moriarty B, Hay R, Morris-Jones R. The diagnosis and management of tinea. BMJ. 2012;345:e4380. doi:10.1136/bmj.e4380
4. Fentaw S, Gentachew T, Assefa M. A five-year retrospective study of dermatophytosis and dermatomycoses at the Mycology Referral Laboratory of EHNRI, Addis Ababa, Ethiopia. Ciencias Biol. 2010;41:1–7.
5. Komba EV, Mgonda YM. The spectrum of dermatological disorders among primary school children in Dar es Salaam. BMC Public Health. 2010;10(1):765. doi:10.1186/1471-2458-10-765
6. Woldeamanuel Y, Leekassa R, Chryssanthou E, et al. Clinico-mycological profile of dermatophytosis in a reference centre for leprosy and dermatological diseases in Addis Ababa. Mycopathologia. 2006;161:167–172. doi:10.1007/s11046-004-3141-5
7. Nweze EI, Eke IE. Dermatophytes and dermatophytosis in the eastern and southern parts of Africa. Med Mycol. 2018;56(1):13–28. doi:10.1093/mmy/myx025
8. Bongomin F, Gago S, Oladele RO, Denning DW. Global and multi-national prevalence of fungal diseases-estimate precision. Journal of Fungi (Basel, Switzerland). 2017;3:4. doi:10.3390/jof3040057
9. Metintas S, Kiraz N, Arslantas D, et al. Frequency and risk factors of dermatophytosis in students living in rural areas in Eskişehir, Turkey. Mycopathologia. 2004;4(157):379–382. doi:10.1023/B:MYCO.0000030447.78197.fb
10. Gürcan S, Tikveşli M, Eskiocak M, Kiliç H, Otkun M. Investigation of the agents and risk factors of dermatophytosis: a hospital-based study. Mikrobiyol Bul. 2008;42(1):95–102.
11. Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51(4):2–15. doi:10.1111/j.1439-0507.2008.01606.x
12. Ndako JA, Osemwegie OO, Spencer THI, Olopade BK, Yunusa GA, Banda J. Prevalence of dermatophytes and other associated fungi among school children. Global Advan Res J Med Med Sci. 2012;1((3):):049–056.
13. Sheikh HA. Epidemiology of dermatophytes in the Eastern Province of Saudi Arabia. Res J Microbiol. 2009;4(6):229–234. doi:10.3923/jm.2009.229.234
14. Teklebirhan G, Bitew A. Prevalence of dermatophytic infection and the spectrum of dermatophytes in patients attending a Tertiary Hospital in Addis Ababa, Ethiopia. Int J Microbiol. 2015;2015:1–5. doi:10.1155/2015/653419
15. De Hoog GS, Dukik K, Monod M, et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 2017;182(1–2):5–31. doi:10.1007/s11046-016-0073-9
16. Woldeamanuel. Y, Leekassa R, Chryssanthou. E, Menghistu. Y, Petrini. B. Prevalence of tinea capitis in Ethiopian schoolchildren. Mycoses. 2005;48(2):137–141. doi:10.1111/j.1439-0507.2004.01081.x
17. Ameen M. Epidemiology of superficial fungal infections. Clin Dermatol. 2010;28(2):197–201. doi:10.1016/j.clindermatol.2009.12.005
18. Rajagopalan M, Inamadar A, Mittal A, et al. Expert Consensus on the Management of Dermatophytosis in India (ECTODERM India). BMC Dermatology. 2018;18(1):6. doi:10.1186/s12895-018-0073-1
19. Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7(2):77–86. doi:10.4103/2229-5178.178099
20. Jacobsen AA, Tosti A. Predisposing factors for onychomycosis. Onychomycosis. 2017;11–919.
21. Toukabri N, Dhieb C, El Euch D, Rouissi M, Mokni M, Sadfi-Zouaoui N. Prevalence, etiology, and risk factors of Tinea pedis and Tinea unguium in Tunisia. Can J Infect Dis Med Microbiol. 2017;2017:1–9. doi:10.1155/2017/6835725
22. Bitew A. Dermatophytosis: prevalence of dermatophyte and non-dermatophyte fungi from patients attending Arsho advanced medical laboratory, Addis Ababa, Ethiopia. Dermatol Res Pract. 2018;2018:8164757. doi:10.1155/2018/8164757
23. Raccurt CP, Dorsainvil D, Boncy M, Auguste G. The emergence of Trichophyton tonsurans in Port-au-Prince, Haiti. Med Mycol. 2009;47:197–200. doi:10.1080/13693780802192676
24. Enweani IB, Ozan CC, Agbonlahor DE, Ndip RN. Dermatophytosis in school children in Ekpoma, Nigeria. Mycoses. 1996;39:303–305. doi:10.1111/j.1439-0507.1996.tb00143.x
25. Al Shimaa ME, Ouf SA, Tarek AAM, Eltahlawi SMR. Dermatophyte and other associated fungi in patients attending to some hospitals in Egypt. Braz J Microbiol. 2015;46(3):799–805. doi:10.1590/S1517-838246320140615
26. Adou-Bryn KD, Assoumou A, Haddad RN, Aka BR, Ouhon J. Epidemiology of Tinea capitis in Abidjan, Cote d’Ivoire. Med NTrop (Mars). 2004;64:171–175.
27. Kalinowska K. Epidemiology of dermatomycoses in Poland over the past decades. Mikol Lek. 2012;17(3):165–168.
28. Alemayehu A, Minwuyelet G, Andualem G. Prevalence and etiologic agents of dermatophytosis among primary school children in Harari Regional State, Ethiopia. J Mycol. 2016;2016:1–5. doi:10.1155/2016/1489387
29. Szepietowski CJ, Reich. A, Garlowska. E, Kulig. M, Baran E. Factors influencing coexistence of toenail onychomycosis with tinea pedis and other dermatomycoses: a survey of 2761 patients. Arch Dermatol. 2006;10(142):1279–1284. doi:10.1001/archderm.142.10.1279
30. Cheng. S, Chong L. prospective epidemiological study on tinea pedis and onychomycosis in Hong Kong. Chin Med J. 2002;115(6):860–886.
31. Abd E, Al Shimaa M, Ouf SA, Moussa TAA, Eltahlawi MR. Dermatophytes and other associated fungi in patients attending to some hospitals in Egypt. Braz J Microbiol. 2015;
32. Moto NJ, Maing MJ, Nyamache KA. Prevalence of Tinea capitis in school-going children from Mathare, informal settlement in Nairobi, Kenya. BMC Res Notes. 2015;8:274. doi:10.1186/s13104-015-1240-7
33. Oke OO, Onayemi O, Olasode AO, Omisore GA, Oninla AO. The prevalence and pattern of superficial fungal infections among school children in Ile-Ife, South-Western Nigeria. Dermatol Res Pract. 2014. doi:10.1155/2014/842917
34. Kalita JM, Sharma A, Bhardwaj A, Nag VL. Dermatophytoses and spectrum of dermatophytes in patients attending a teaching hospital in Western Rajasthan, India. J Family Med Prim Care. 2019;8(4):1418–1421. doi:10.4103/jfmpc.jfmpc_159_19Adefemi
35. Odeigah SA, O L, Alabi KM. Prevalence of dermatophytosis among primary school children in Oke-oyi community of Kwara state. Niger J Clin Pract. 2011;1(14):23–28.
36. Ellabib MS, Khalifa Z, Kavanagh K. Dermatophyte and other fungi associated with skin mycoses in Tripoli, Libya. Mycoses. 2002;45:101–110. doi:10.1046/j.1439-0507.2002.00731.x
37. Bensch K, Braun U, Groenewald JZ, et al. The genus Cladosporium. Stud Mycol. 2012;72:1–401. doi:10.3114/sim0003
38. Khaled JM, Golah HA, Khalel AS, Alharbi NS, Mothana RA. Dermatophyte and non-dermatophyte fungi in Riyadh City, Saudi Arabia. Saudi J Biol Sci. 2015;22(5):604–609. doi:10.1016/j.sjbs.2014.12.006
39. Teklebirhan G, Bitew A. Profile of dermatophyte and non-dermatophyte fungi in patients suspected of dermatophytosis. Am J Life Sci. 2015;3(5):352–357. doi:10.11648/j.ajls.20150305.13
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
