Back to Journals » International Journal of General Medicine » Volume 14
Epidemiology and Outcomes of Status Epilepticus
Authors Ascoli M, Ferlazzo E, Gasparini S, Mastroianni G, Citraro R, Roberti R, Russo E
Received 3 April 2021
Accepted for publication 15 June 2021
Published 28 June 2021 Volume 2021:14 Pages 2965—2973
DOI https://doi.org/10.2147/IJGM.S295855
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Michele Ascoli,1,2 Edoardo Ferlazzo,1,2 Sara Gasparini,1,2 Giovanni Mastroianni,2 Rita Citraro,3 Roberta Roberti,3 Emilio Russo3
1Department of Medical and Surgical Sciences, Magna Græcia University, Catanzaro, Italy; 2Regional Epilepsy Centre, Great Metropolitan Hospital, Reggio, Calabria, Italy; 3Science of Health Department, Magna Græcia University, Catanzaro, Italy
Correspondence: Emilio Russo
Science of Health Department, Magna Græcia University, Viale Europa, Catanzaro, 88100, Italy
Tel +39 0961 3697397
Fax +39 0961 3694192
Email [email protected]
Abstract: Status epilepticus (SE) is a neurological and medical emergency, defined as a condition resulting either from the failure of the mechanisms responsible of seizure self-limitation or from the initiation of mechanisms which lead to atypically prolonged seizures. Further than death, SE can have long-term consequences, including neuronal injury, depending on the type, cause and duration of seizures with severe associated disabilities. In Europe, SE shows an incidence rate ranging about 9 to 40/100,000/y. In adults, mortality of patients with SE is ∼ 30%, and even higher (up to 40%) in refractory status epilepticus. To date, etiology, duration, presence of comorbidity, level of consciousness, semiology and age are the main clinical predictors of SE outcome.
Keywords: status epilepticus, incidence, mortality, etiology, classification
Introduction
Status epilepticus (SE) is a life-threatening neurological and medical emergency. The International League Against Epilepsy (ILAE) defines SE as a condition resulting either from the failure of the mechanisms responsible of seizure self-limitation or from the initiation of mechanisms which lead to atypically prolonged seizures. SE is a condition that can have long-term consequences, including neuronal injury or death, and alteration of neuronal networks depending on the type and duration of seizures.1
This is a conceptual definition with two operational time dimensions. The first time-dimension (t1) is the time point at which the seizure should be regarded as an “abnormally prolonged seizure” Indeed, the second time dimension (t2) is the time of ongoing seizure activity beyond which there is a risk of long-term consequences. To date the two time points have been defined only for the convulsive (tonic-clonic) SE and focal motor SE based on clinical research and animal experimentation. Data are not available for other forms of SE. Time point values may change considerably among different SE semiology.1
SE characterization, according to ILAE,1 should be categorized according to an axed-based approach. Four axes have been defined: semiology, etiology, EEG correlates, age. Age of the patient and the semiology will be immediately assessable. On the contrary, etiology may take time to be identified and EEG recordings may not be available in many settings, particularly at presentation. However, EEG patterns influence clinical approach, aggressiveness of treatment and prognosis, so it should be performed as early as possible. Some authors suggest that the identification of the “clinical context” (eg, SE in subjects with no history of epilepsy and SE in patients with epilepsy) may be more important than etiology in leading to a faster diagnostic assessment and management.2
This subdivision division into two time points is crucial for clinical approach and management: t1 determines the time at which treatment should be considered or started, whereas t2 determines when aggressive treatments should be implemented to prevent long-term consequences. To date, in various regions of the world, a wide range of incidences of SE in adults was found. Although the incidence of SE appears to be higher in the elderly, data on census-based population are scarce. Regarding prognosis, many predictive factors of outcome have been considered in literature. In this review, we discuss the current knowledge about epidemiology and outcome of SE in adults.
Search Strategy
References were identified by PubMed and Google Scholar searches between January 1990 and March 2021 with the following search terms: “status epilepticus” in combination with “epidemiology”, “prevalence”, “incidence”, “prognosis” and “outcome”. Search results were reviewed and systematic reviews and meta-analyses related to SE were selected. Articles were also identified through searches of the authors’ own files. We only included original, English-written studies. The final reference list was generated based on novelty, importance, originality, quality, and relevance to the scope of this review.
Epidemiology
In Europe, SE shows an incidence rate between 8.52 and 36.1/100.000/y. In different studies, the reported incidence is 9.9/100.000/y in the French canton, Switzerland,3 10.7/100.000/y on the island of Funen, Denmark,4 13.1/100.000/y in Bologna, Italy,5 15.0/100.000/y in Emilia Romagna,6 27.2/100.000 in Ferrara,7 15.0/100.000/y in Germany,8 8.52/100.000 in La Reunion Island, France9 and 16.3/100.000/y in Geneva, Switzerland.10 A first study carried out in USA showed an incidence rate of 41/100.000/y.11 A second retrospective study conducted in Rochester showed an incidence of 18.3/100.000/y.12 Regarding the Asian continent, the incidence of SE was 5.20 patients/100,000/y in Thailand; a Taiwan study showed an incidence of 4.61 per 100,000/y from 2000 to 2011.13,14 In Auckland, New Zealand, SE (defined as seizures lasting ≥30 minutes) has an age‐adjusted incidence of 15.95 patients/100,000/y.15
SE appears to be more frequent in developing countries although literature data are scares.16 One study in conducted in Kenya sub-Saharan Africa, recorded a minimum incidence of convulsive SE (CSE) as 35/100,000/year in children (0–13 years), based on hospital admissions.17 This rate represented a minimum incidence, since a proportion of children usually dies before reaching hospital, and most of them are treated in private clinics.17
Discrepancy between different studies may be explained by several factors such as study design (prospective or retrospective), hospital setting (tertiary hospital or community/rural hospitals) and differences between study populations. Race, socioeconomic, cultural, and environmental differences may contribute to the different incidence of SE in different studied populations. Another bias is the use of different definitions of SE in the different studies and the diverse timing used to define SE, which varies between 5 and 20 minutes.1
A recent population-based study conducted in the city of Salzburg (Austria) with the new ILAE 2015 definition and classification of SE,18 showed a higher incidence of first SE of 36.1 per 100,000 adults per year. Annual incidence of non-convulsive SE (NCSE) resulted to be 12.1/100,000 (24.0/100,000 for SE with prominent motor phenomena). The detected increased incidence of SE is probably due to different factors, including the availability of emergency EEGs, new and more precise diagnostic criteria with the reduction of the diagnostic time from 30 to 5 minutes in convulsive SE, and lastly to increasing population age. Indeed, patients older than 60 years have a considerably increased incidence of SE compared with adults younger than 60 years.18,19
Regarding sex differences, although previous studies have found a greater incidence of SE in males than in females, recent estimates suggest that incidence of SE is higher in females than males.5,6,18
Interestingly, etiologies seem to vary among different populations. Acute symptomatic causes appear to be more common than remote symptomatic causes. In one prospective population-based study conducted in Germany,8 the most common etiologies were a prior stroke (36.0%) or other remote symptomatic causes (26.7%). In a study conducted in Richmond,11 the most common etiologies in adults result to be: low ASM levels (34%), remote etiology (24%), and stroke (22%). A Swiss study3 found that acute etiology was more common (62%) than remote (28%) or unknown etiology (10%). Overall, among acute symptomatic causes, stroke seems to be the most frequent. Instead, previous structural brain damage (such as tumors, prior stroke and prior traumatic brain injury) are common chronic causes, which can lead to SE after a latent period of weeks to years.20 Other important causes include anoxic or hypoxic injury, infection, alcohol intoxication/withdrawal, metabolic derangements (eg, hyponatremia, hypo/hyperglycemia) and autoimmune or presumed autoimmune encephalitis.21
The majority of cases of SE occur in the absence of a known diagnosis of epilepsy. SE in the context of a known epilepsy occurs generally in susceptible patients with breakthrough seizures or low ASM levels. It is an early manifestation in the course of the disease. Generally representing the first or second epileptic manifestation in the majority of the time. It also confers an approximately threefold increased risk of future seizures compared with the risk following a single, self-limited, seizure.20
Of all patients with SE, 12% to 43% progress to refractory SE and 10% to 15% progress to super-refractory SE. Of note, the studies evaluating this frequency are limited due to the retrospective nature, different inclusion criteria and different SE definitions.21 Overall, SE incidence was found to have a high variability spanning from 9.1 to 41/100,000/y depending on several factors (Table 1).
 |
Table 1 Worldwide Incidence of Status Epilepticus |
Prognostic Factors
In patients with SE, mortality reaches up to 30% in adults. Outcomes in refractory SE is worse, with mortality reaching up to 39%.22 Multiple factors have been reported as important determinants of poor outcome and mortality including: etiology, comorbidities, older age, ethnicity, semeiology, duration, EEG pattern and time to treatment.
Etiology and Comorbidities
Etiology is the most powerful factor defining outcome in SE patients. Moreover, it cannot always be easily defined in emergency conditions. The underlying cause of SE is categorized in classified as “known” or “unknown” at diagnosis. The term “known” is used for SE caused by structural, metabolic, inflammatory, infectious, toxic, or genetic causes. We distinguish: 1) SE due to symptomatic acute causes (that occur within seven days from: stroke, intoxication, infectious or autoimmune encephalitis, metabolic disturbances, abrupt drug or alcohol withdrawal, etc.); 2) SE due to symptomatic remote causes (occurring more than one week following brain injuries, encephalitis, stroke, etc …); 3) SE due to symptomatic progressive causes (ie, brain neoplasms, dementias, etc.). In a proportion of patients, the etiology is unknown (“cryptogenic SE”).1 Regarding etiology, some authors suggest a distinction between SE in patients with known epilepsy and SE in subjects without history of epilepsy. Indeed, patients with previous epilepsies diagnosis can present SE related to triggering factors, for example, sleep deprivation, inappropriate antiseizures medication (ASM) prescription, reduced ASM plasmatic levels (due to vomiting, diarrhea, drug–drug interactions, etc.) toxic-metabolic disorders and lack of adherence to therapy. SE can also represent a typical manifestation of definite electroclinical syndromes, such as Ohtahara syndrome, West syndrome, Angelman syndrome, etc.1,2,23–25
SE in the context of a previously diagnosed epilepsies is associated with a more favorable prognosis.26–30 About 40% of patients with SE have a history of epilepsy, and up to 60% of cases are related to acute symptomatic causes.31–33 Cerebrovascular diseases and low ASM levels seem to be the most common etiologies. Low ASM levels (in epilepsy patients) and alcohol abuse have a relatively good prognosis (with reported mortality of less than 10%) as compared to SE associated with stroke,26 meningo-encephalitis,28,34 and cerebral anoxia.30,35 Acute symptomatic SE after stroke has a higher mortality and morbidity compared with other SE etiologies.27 Encephalitis is strongly associated with refractory SE with a considerable risk of developing subsequent epilepsy.26,36 Brain injury is an unusual cause of SE, associated with favorable outcomes.37,38 Cryptogenic SE is associated with variable outcomes, with generally low mortality but high risk of epilepsy.39,40
Studies looking at the role of prior comorbidities found them to be important in survival and in a return to baseline functional outcome. Higher comorbidity index was associated with higher mortality. Diabetes mellitus, extracranial malignancy, sodium imbalance, anoxic brain injury, pneumonia, sepsis, valvular heart disease, renal failure, and liver disease, are often associated with worse outcomes and higher mortality.41–44
Ethnicity and Age
Among people of Afro-American heritage, incidence of SE is higher and mortality generally lower.45 This may be probably due to underlying illness, access to medical care, compliance, or to other intrinsic biologic factors.
Regarding age, five age groups are distinguished in SE classification: neonatal (0 to 30 days), infancy (1 month to 2 years), childhood (>2 to 12 years), adolescence and adulthood (>12 to 59 years), elderly (≥60 years). Different age of presentation may require different diagnostic approach and treatment.1,44
Older age is an independent factor of death in SE. Leitinger et al observed that SE fatality in elderly was 22.5% and 4.1% in patients younger than 60 years.18,19 Age is part of different scoring systems for outcome prediction such as the STESS and EMSE.46,47 Age over 65 was a significant predictor of death as evidenced by several studies.48 Older patients are somewhat more likely to suffer from SE associated with stroke and CNS tumors, conditions that “per se” have an overall high mortality.43 Other explanations should be that patients of more advanced age are more prone to SE complications and ASM severe adverse effects.
Semeiology
The presence of prominent motor signs or symptoms may be summarized as convulsive SE as opposed to NCSE. The second determinant of semiology classification is the degree (qualitative or quantitative) of awareness: SE can be classified as with or without coma. Classification by semiology is complicated by the fact that clinical forms of seizures in SE evolve and because, especially in non-convulsive SE, the definition relies fundamentally on EEG findings (focal vs generalized).19 Notably, proposed clinical terms for SE differ from recent new seizures classification and a term revision is urgently needed. Different studies have examined the relation between SE semeiology and prognosis. Prominent motor phenomena seem to predispose to a better outcome as compared to NCSE.18,19 Studies showed that patients with focal or absence seizures at SE onset, as compared to patients with bilateral tonic clonic seizures or NCSE, had significant higher relative risks of death.49–51 Myoclonic SE has been associated with poor outcomes and higher mortality, probably due to underlying etiology.52 The presence/absence of impaired awareness has been considered in different studies as a possible prognostic factor in patients with SE. Impaired awareness at SE onset has been associated with higher mortality. In a recent retrospective population-based study of adult patients with SE, impaired awareness was associated with higher mortality, 33% vs 8.2% in awake patients.18 Of interest, in the same study, patients with prominent motor semiology had a lower mortality as compared with somnolent, stuporous or comatose patients.18
EEG Pattern
To date, no evidence-based EEG criteria for SE exist. None of the ictal EEG patterns of SE is specific. ILAE proposed that an EEG pattern classification may take into account location (generalized, including bilateral synchronous patterns; lateralized; bilateral independent; multifocal), type of the pattern (periodic discharges, rhythmic delta activity or spike-and-wave subtypes), morphology (sharpness, number of phases, absolute and relative amplitude, polarity), time-related features (prevalence, frequency, duration, daily pattern duration and index, onset and dynamics), modulation (stimulus-induced vs spontaneous), effect of intervention (medication) on EEG.1
In literature, non-reactive background EEGs activities were associated with poor outcome.53 Concerning morphology, multiple status patterns in EEGs have been independently associated with mortality. Ictal lateralized periodic discharges in the EEGs had higher mortality, although patients with lateralized rhythmic activity had a better functional outcome.54,55
Duration and Time to Treatment
In relation to the response to drug treatment, SE can be defined as drug-responsive, refractory or super-refractory. Refractory SE (RSE) occurs when seizures persist despite the administration of a benzodiazepine and another adequately dosed ASM, often requiring treatment with anesthetic drugs. Super-refractory status epilepticus (SRSE) is defined as SE that persists despite 24-hour treatment with intravenous anesthetic or recurs when weaning the patient off the anesthetic. New-onset refractory status epilepticus (NORSE) is defined as new-onset RSE where no detectable cause is identifiable in otherwise healthy subjects. Most of the time, it is difficult to know the exact SE duration considering that exact time of onset is frequently not detected.
Aggressive treatment has been recommended for SE, indeed the risk of death appears to be higher if treatment is delayed. This is best documented for generalized convulsive SE but there is no consensus about the best therapeutic approach to NCSE or focal SE.
Several studies evaluated the possible role of SE duration as an unfavorable prognostic factor. Longer duration appears to be associated with higher mortality. Evidence suggests that SE lasting more than 30 min is less likely to terminate spontaneously and is associated with a higher mortality than SE lasting less than 30 min.18 However, NORSE can be associated with significant recovery even after prolonged duration of SE.
To date, no randomized clinical trial has compared aggressive prompt treatment with intravenous ASM to non-aggressive or delayed approach to SE. The prognostic role of time to treatment initiation in SE is still debated. Some studies found a positive association with poor outcome others found no correlation; some authors have shown that untreated SE carries a high risk of deleterious neurological and systemic complications, but others did not confirm this association.46,47,56–60 One possible explanation is that time to treatment is critical for extremely severe SE cases, but not for all types of SE. Definitely, patient comorbidities play a significant role in outcomes and can affect determination of the baseline risk for aggressive treatment.12,61–63 This view has some limitations because it is not possible to easily separate complications caused by SE from those caused by ASM and the weight of each type of complication in the final outcome.
Continuous intravenous anesthetic drugs administration benefits for treatment of refractory status epilepticus (RSE) are debated. Prescribing them early may have a positively impact outcome. Furthermore, patients who do not have a severe RSE etiology and who experienced a shorter seizure duration seem to have a better outcome.64
Prognostic Scores
In patients presenting with SE baseline symptoms and comorbidities may be useful to predict outcomes and shape treatment decisions. Two previously published scoring systems exist to predict outcomes: STESS and ESME scores46,47 (Table 2).
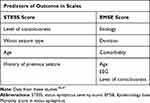 |
Table 2 Prognostic Scores |
The STESS was published in 2006. It includes four weighted clinical variables available to the neurologist at SE presentation: consciousness before treatment, worst type of seizure, age, and history of previous seizures (because etiology is often not instantly available in emergency setting), giving a total ranging from 0 to 6. STESS score has been validated on 171 patients with SE treated in an intensive care environment. This study confirms the good discrimination of this score between survivors and nonsurvivors.65 Modified STESS was developed with inclusion of the modified Rankin Scale (mRS) to STESS to improve the prediction of mortality. Modified STESS (mSTESS) relies on the assessment of age, history of previous seizure, consciousness, and worst seizure type the same as STESS except age cut-off at 70 years and the addition of mRS (0 point if mRS is 0, 1 point if mRS is 1–3, 2 points if mRS is ≥4).
The EMSE, described in 2015, combines several variables, including etiology, age, comorbidity, and EEG characteristics. Each item has a weighted score between 0 and 60. EMSE has been on 46 patients validated and has showed high sensitivity for mortality.66
Literature data showed that EMSE, STESS and mSTESS may be useful to predict outcomes of SE in populations with few comorbidities. Prospective trials should be carried out to evaluate their utility in patients with higher number of comorbidities.
Prognostic Biomarkers
Neuronal damage and inflammation biomarkers have been evaluated as potentials determinants of poor outcome in SE. Elevated neuron-specific enolase levels can be indicative of neuronal injury.67 The increase of neuron-specific enolase in SE was reported in a few patients with a serum peak from 24 to 48 hours after SE. There was a possible association of higher levels with worse outcome and longer duration of SE, but findings were inconclusive in this small cohort.68
Tau protein is considered an indicator of both axonal and neuronal damage and can be a diagnostic and prognostic marker in traumatic brain injury.69 Tau CSF levels were studied in SE and were associated with higher SE duration and use of general anesthesia (propofol). The role of tau as a biomarker in SE is still debated and needs further evaluation. Serum albumin of,35 g/L at SE onset was also found to be an independent predictor for refractoriness in SE patients.
Seizure activity may cause systemic inflammatory reactions represented by changes in cytokine, increased circulating immune cells and blood–brain barrier dysfunction.31 Conversely, systemic inflammation can trigger or sustain seizures and influence the course of SE, so is very difficult demonstrate the causal link between the increase of these molecules and SE prognosis. Procalcitonin was found to be independently associated with unfavorable outcomes.31
Conclusions
SE represents a clinical emergency in which undoubtedly time is brain. Prompt identification and adequate treatment is essential in the management of SE. The ILAE classification clearly represents the best tool while an update is currently needed according to the new seizure/epilepsy classification.1,70,71 The incidence of SE is highly variable according to studies ranging about 10 to 40/100,000/y; this depends on several factors including the period in which studies were performed but also on the area and the level of clinical services available. On the other hand, it could also depend on specifically influencing factor in some geographic areas including environmental and genetic factors.
Moreover, studies on the epidemiology of SE are characterized by a large heterogeneity in design and population, definitions of SE, and case ascertainment, as well as age and gender adjustment.
SE represents a rare not so rare event; being the etiology, so variable it can outbreak during the course of other pathologies such as brain tumors and therefore in some cases this higher risk should influence clinical practice and management. This latter point also remains a major problem in some areas in which it is not always easy to reach an early diagnosis and then have an early appropriate treatment. This is strictly linked to our current knowledge on SE outcome; in fact, this is also variable and difficult to be evaluated. Mortality can reach up 40% in some cases with several factors influencing this specific outcome but also permanent or temporary disabilities as a consequence of SE are not exactly established or may not be definitively established.
Regarding SE prognosis, at first evaluation, older age, awareness impairment, prominent motor signs and duration more than 30 minutes seem to be strongly predictive of poor outcome. Specific etiologies such as stroke, anoxic encephalopathy, brain tumors, CNS infections, and alcohol/drug toxicity also appear to be related to high mortality in SE. Though SE etiology and duration are often unknown at presentation, age, level of consciousness, SE semeiology are immediately available to the treating neurologist, and knowledge of these predictive variables may help to design prospective studies to investigate how to improve treatment approach. Indeed, despite an evident negative predictive value, STESS and EMSE, are still not enough to guide treatment decisions.
In conclusion, we believe that despite our ability and the need to have exact measures for incidence and outcomes, specific protocols should be capillary implemented in every health system to prevent at the most the dreadful outcomes of SE. Finally, biomarkers for prognostic evaluation of SE development risk would also be extremely useful to apply strategies for prevention although a quote of SE unfortunately arise in subjects without any previous history of epilepsy or other know and predictable risk factors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus - Report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56(10):1515–1523. doi:10.1111/epi.13121
2. Aguglia U, Sueri C, Gasparini S, et al. Relevance of clinical context in the diagnostic-therapeutic approach to status epilepticus. Epilepsia. 2016;57(9):1527–1529. doi:10.1111/epi.13475
3. Coeytaux A, Jallon P, Galobardes B, Morabia A. Incidence of status epilepticus in French-speaking Switzerland: (EPISTAR). Neurology. 2000;55(5):693–697. doi:10.1212/wnl.55.5.693
4. Rodin E, Krogstad MH, Aukland P, et al. High long-term mortality after incident status epilepticus in adults: results from a population-based study. Epilepsia. 2019;60(1):33–41. doi:10.1111/epi.14602
5. Vignatelli L, Tonon C, D’Alessandro R. Incidence and short-term prognosis of status epilepticus in adults in Bologna, Italy. Epilepsia. 2003;44(7):964–968. doi:10.1046/j.1528-1157.2003.63702.x
6. Vignatelli L, Rinaldi R, Galeotti M, De Carolis P, D’Alessandro R. Epidemiology of status epilepticus in a rural area of northern Italy: a 2-year population-based study. Eur J Neurol. 2005;12(11):897–902. doi:10.1111/j.1468-1331.2005.01073.x
7. Govoni V, Fallica E, Monetti VC, et al. Incidence of status epilepticus in southern Europe: a population study in the health district of Ferrara, Italy. Eur Neurol. 2008;59(3–4):120–126. doi:10.1159/000111873
8. Knake S, Rosenow F, Vescovi M, et al. Incidence of status epilepticus in adults in Germany: a prospective, population-based study. Epilepsia. 2001;42(6):714–718. doi:10.1046/j.1528-1157.2001.01101.x
9. Bhalla D, Tchalla AE, Mignard C, et al. First-ever population-based study on status epilepticus in French Island of la Reunion (France) - Incidence and fatality. Seizure. 2014;23(9):769–773. doi:10.1016/j.seizure.2014.06.009
10. Jallon P, Coeytaux A, Galobardes B, Morabia A. Incidence and case-fatality rate of status epilepticus in the Canton of Geneva. Lancet. 1999;353(9163):1496. doi:10.1016/S0140-6736(99)00583-8
11. DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46(4):1029–1035. doi:10.1212/WNL.46.4.1029
12. Hesdorffer DC, Logroscino G, Cascino G, Annegers JF, Hauser WA. Incidence of status epilepticus in Rochester, Minnesota, 1965–1984. Neurology. 1998;50(3):735–741. doi:10.1212/WNL.50.3.735
13. Tiamkao S, Pranboon S, Thepsuthammarat K, Sawanyawisuth K. Incidences and outcomes of status epilepticus: a 9-year longitudinal national study. Epilepsy Behav. 2015;49:135–137. doi:10.1016/j.yebeh.2015.04.040
14. Ong CT, Sheu SM, Tsai CF, et al. Age-dependent sex difference of the incidence and mortality of status epilepticus: a twelve year nationwide population-based cohort study in Taiwan. PLoS One. 2015;10:1–9. doi:10.1371/journal.pone.0122350
15. Bergin PS, Brockington A, Jayabal J, et al. Status epilepticus in Auckland, New Zealand: incidence, etiology, and outcomes. Epilepsia. 2019;60(8):1552–1564. doi:10.1111/epi.16277
16. Newton CR, Kariuki SM. Status epilepticus in sub-Saharan Africa: new findings. Epilepsia. 2013;6:50–53. doi:10.1111/epi.12277 PMID: 24001073.
17. Sadarangani M, Seaton C, Scott JA, et al. Incidence and outcome of convulsive status epilepticus in Kenyan children: a cohort study. Lancet Neurol. 2008;7(2):145–150. doi:10.1016/S1474-4422(07)70331-9
18. Leitinger M, Trinka E, Giovannini G, et al. Epidemiology of status epilepticus in adults: a population-based study on incidence, causes, and outcomes. Epilepsia. 2019;60(1):53–62. doi:10.1111/epi.14607
19. Leitinger M, Trinka E, Gardella E, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15(10):1054–1062. doi:10.1016/S1474-4422(16)30137-5
20. Betjemann JP, Lowenstein DH. Status epilepticus in adults. Lancet Neurol. 2015;14(6):615–624. doi:10.1016/S1474-4422(15)00042-3
21. Johnson EL, Kaplan PW. Status epilepticus: definition, classification, pathophysiology, and epidemiology. Semin Neurol. 2020;40(6):647–651. doi:10.1055/s-0040-1718722
22. Nelson SE, Varelas PN. Status epilepticus, refractory status epilepticus, and super-refractory status epilepticus. Contin Lifelong Learn Neurol. 2018;24(6):1683–1707. doi:10.1212/CON.0000000000000668
23. Genton P, Ferlazzo E, Thomas P. Absence status epilepsy: delineation of a distinct idiopathic generalized epilepsy syndrome. Epilepsia. 2008;49(4):642–649. doi:10.1111/j.1528-1167.2007.01467.x
24. Gasparini S, Ferlazzo E, Cianci V, et al. Rapidly fatal late-onset status epilepticus due to occult bi-frontal cortical dysplasia. A case report. J Neurol Sci. 2015;358(1–2):492–495. doi:10.1016/j.jns.2015.09.018
25. Ascoli M, Mastroianni G, Gasparini S, et al. Diagnostic and therapeutic approach to drug-resistant juvenile myoclonic epilepsy. Expert Rev Neurother. 2021;25:1–9. doi:10.1080/14737175.2021.1931126
26. Knake S, Rochon J, Fleischer S, et al. Status epilepticus after stroke is associated with increased long-term case fatality. Epilepsia. 2006;47(12):2020–2026. doi:10.1111/j.1528-1167.2006.00845.x
27. Waterhouse EJ, Vaughan JK, Barnes TY, et al. Synergistic effect of status epilepticus and ischemic brain injury on mortality. Epilepsy Res. 1998;29(3):175–183. doi:10.1016/S0920-1211(97)00071-5
28. Zoons E, Weisfelt M, de Gans J, et al. Seizures in adults with bacterial meningitis. Neurology. 2008;70(22 Pt 2):2109–2115. doi:10.1212/01.wnl.0000288178.91614.5d
29. Thömke F, Marx JJ, Sauer O, et al. Observations on comatose survivors of cardiopulmonary resuscitation with generalized myoclonus. BMC Neurol. 2005:5. doi:10.1186/1471-2377-5-14.
30. Wijdicks EFM, Young GB. Myoclonus status in comatose patients after cardiac arrest. Lancet. 1994;343(8913):1642–1643. doi:10.1016/S0140-6736(94)93100-3
31. Alkhachroum A, Der-nigoghossian CA, Rubinos C, Claassen J. Markers in status epilepticus prognosis. J Clin Neurophysiol. 2020;37(5):422–428. doi:10.1097/WNP.0000000000000761
32. Ferlazzo E, Gasparini S, Sueri C, Aguglia U. Status epilepticus of inflammatory etiology: a cohort study. Neurology. 2016;86(11):1076. doi:10.1212/WNL.0000000000002508
33. Ferlazzo E, Raffaele M, Mazzù I, Pisani F. Recurrent status epilepticus as the main feature of Hashimoto’s encephalopathy. Epilepsy Behav. 2006;8(1):328–330. doi:10.1016/j.yebeh.2005.11.005
34. Shorvon S, Trinka E, Walker M. The seventh London-innsbruck colloquium on status epilepticus and acute seizures. Epilepsy Behav. 2019;101(PtB). doi:10.1016/j.yebeh.2019.106532
35. Holtkamp M, Othman J, Buchheim K, Meierkord H. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry. 2005;76(4):534–539. doi:10.1136/jnnp.2004.041947
36. Jayalakshmi S, Ruikar D, Vooturi S, et al. Determinants and predictors of outcome in super refractory status epilepticus-A developing country perspective. Epilepsy Res. 2014;108(9):1609–1617. doi:10.1016/j.eplepsyres.2014.08.010
37. Neligan A, Shorvon SD. Frequency and prognosis of convulsive status epilepticus of different causes: a systematic review. Arch Neurol. 2010;67(8):931–940. doi:10.1001/archneurol.2010.169
38. Koubeissi M, Alshekhlee A. In-hospital mortality of generalized convulsive status epilepticus: a large US sample. Neurology. 2007;69(9):886–893. doi:10.1212/01.wnl.0000269791.96189.70
39. Sculier C, Gaínza-Lein M, Sánchez Fernández I, Loddenkemper T. Long-term outcomes of status epilepticus: a critical assessment. Epilepsia. 2018;59(SupplSuppl 2):155–169. doi:10.1111/epi.14515
40. Chin RF, Neville BG, Peckham C, et al. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. Lancet. 2006;368(9531):222–229. doi:10.1016/S0140-6736(06)69043-0
41. Alvarez V, Januel JM, Burnand B, Rossetti AO. Role of comorbidities in outcome prediction after status epilepticus. Epilepsia. 2012;53(5). doi:10.1111/j.1528-1167.2012.03451.x
42. Belluzzo M, Furlanis G, Stragapede L, Monti F. Role of comorbidities and in-hospital complications in short-term status epilepticus outcome. Clin Neurol Neurosurg. 2017;154:13–18. doi:10.1016/j.clineuro.2016.12.017
43. Mendiratta P, Dayama N, Wei JY, Prodhan P, Prodhan P. Status epilepticus among older adults in the United States. Geriatr. 2019;4(3). doi:10.3390/geriatrics4030045
44. Mastroianni G, Iannone LF, Roberti R, et al. Management of status epilepticus in patients with liver or kidney disease: a narrative review. Expert Rev Neurother. 2020;00(00):1–14. doi:10.1080/14737175.2021.186264942
45. Dham BS, Hunter K, Rincon F. The epidemiology of status epilepticus in the United States. Neurocrit Care. 2014;20(3):476–483. doi:10.1007/s12028-013-9935-x
46. Millán Sandoval JP, Escobar Del Rio LM, Gómez EA, et al. Validation of the Status epilepticus severity score (STESS) at high-complexity hospitals in Medellín, Colombia. Seizure. 2020;81:287–291. doi:10.1016/j.seizure.2020.08.020
47. Leitinger M, Höller Y, Kalss G, et al. Epidemiology-based mortality score in status epilepticus (EMSE). Neurocrit Care. 2015;22(2):273–282. doi:10.1007/s12028-014-0080-y
48. Wu YW, Shek DW, Garcia PA, Zhao S, Johnston SC. Incidence and mortality of generalized convulsive status epilepticus in California. Neurology. 2002;58(7):1070–1076. doi:10.1212/WNL.58.7.1070
49. Rossetti AO, Logroscino G, Milligan TA, Michaelides C, Ruffieux C, Bromfield EB. Status Epilepticus Severity Score (STESS): a tool to orient early treatment strategy. J Neurol. 2008;255(10):1561–1566. doi:10.1007/s00415-008-0989-1
50. Rossetti AO, Hurwitz S, Logroscino G, Bromfield EB. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry. 2006;77(5):611–615. doi:10.1136/jnnp.2005.080887
51. Sutter R, Marsch S, Fuhr P, Rüegg S. Mortality and recovery from refractory status epilepticus in the intensive care unit: a 7-year observational study. Epilepsia. 2013;54(3):502–511. doi:10.1111/epi.12064
52. Hui ACF, Cheng C, Lam A, Mok V, Joynt GM. Prognosis following postanoxic myoclonus status epilepticus. Eur Neurol. 2005;54(1):10–13. doi:10.1159/000086755
53. Rossetti AO, Oddo M, Liaudet L, Kaplan PW. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72(8):744–749. doi:10.1212/01.wnl.0000343006.60851.62
54. Goselink RJM, van Dillen JJ, Aerts M, et al. The difficulty of diagnosing NCSE in clinical practice; external validation of the Salzburg criteria. Epilepsia. 2019;60(8). doi:10.1111/epi.16289;
55. Baysal-Kirac L, Cakar MM, Altiokka-Uzun G, Guncan Z, Guldiken B. Electroclinical patterns in patients with nonconvulsive status epilepticus: etiology, treatment, and outcome. Epilepsy Behav. 2020;107611.
56. Lothman E. The biochemical basis and pathophysiology of status epilepticus. Neurology. 1990;40(Suppl 2):13–23.
57. Fountain NB, Lothman EW. Pathophysiology of status epilepticus. J Clin Neurophysiol. 1995;12:326–342. doi:10.1097/00004691-199512040-00004
58. Treiman DM. Electroclinical features of status epilepticus. J Clin Neurophysiol. 1995;12:343–362. doi:10.1097/00004691-199512040-00005
59. Lowenstein DH, Bleck T, MacDonald RL. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40:120–122. doi:10.1111/j.1528-1157.1999.tb02000.x
60. Walker MC. Status epilepticus in the intensive care unit. J Neurol. 2003;250:401–406. doi:10.1007/s00415-003-1042-z
61. Rossetti AO, Reichhart MD, Schaller MD, et al. Propofol treatment of refractory status epilepticus: a study of 31 episodes. Epilepsia. 2004;45:757–763. doi:10.1111/j.0013-9580.2004.01904.x
62. Chin RFM, Neville BGR, Scott RC. A systematic review of the epidemiology of status epilepticus. Eur J Neurol. 2004;11:800–810. doi:10.1111/j.1468-1331.2004.00943.x
63. Sagduyu A, Tarlaci S, Sirin H. Generalized tonic-clinic status epilepticus: causes, treatment, complications and predictor of fatality. J Neurol. 1998;245:640–646. doi:10.1007/s004150050260
64. Madžar D, Reindl C, Giede-Jeppe A, et al. Impact of timing of continuous intravenous anesthetic drug treatment on outcome in refractory status epilepticus. Crit Care. 2018;22(1):317. doi:10.1186/s13054-018-2235-2
65. Sutter R, Kaplan PW, Rüegg S. Independent external validation of the status epilepticus severity score. Crit Care Med. 2014;41(12):e475–9. doi:10.1097/CCM.0b013e31829eca06
66. Yechoor N, Adeli A, Hafeez S. External validation of the epidemiology based mortality score in status epilepticus in an American intensive care population. Epilepsy Res. 2018;148:32–36. doi:10.1016/j.eplepsyres.2018.10.001
67. Royds JA, Timperley WR, Taylor CB. Levels of enolase and other enzymes in the cerebrospinal fluid as indices of pathological change. J Neurol Neurosurg Psychiatry. 1981;44:1129–1135. doi:10.1136/jnnp.44.12.1129
68. DeGiorgio CM, Correale JD, Gott PS, et al. Serum neuron-specific enolase in human status epilepticus. Neurology. 1995;45:1134–1137. doi:10.1212/WNL.45.6.1134
69. Rubenstein R, Chang B, Yue JK, et al. Comparing plasma phospho tau, total tau, and phospho tau-total tau ratio as acute and chronic traumatic brain injury biomarkers. JAMA Neurol. 2017;74:1063–1072. doi:10.1001/jamaneurol.2017.0655
70. Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the international league against epilepsy: position paper of the ILAE commission for classification and terminology. Epilepsia. 2017;58(4):522–530. doi:10.1111/epi.13670
71. Scheffer IE, Berkovic S, Capovilla G, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–521. doi:10.1111/epi.13709
72. Vijiala S, Alvarez V. Epidemiology of status epilepticus in a non-urban area in Switzerland. Acta Neurol Scand. 2021;143(4):413–420. doi:10.1111/ane.13383
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
