Back to Journals » Cancer Management and Research » Volume 13
Enhanced Efficacy of Neoadjuvant Chemotherapy with Nab-Paclitaxel and Platinum for Locally Advanced Cervical Cancer
Authors Yu XL, Wu MF, Ding L, Yang J, Bai SM
Received 9 October 2021
Accepted for publication 8 December 2021
Published 22 December 2021 Volume 2021:13 Pages 9297—9304
DOI https://doi.org/10.2147/CMAR.S343602
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Seema Singh
Xiao-Li Yu,1,2,* Miao-Fang Wu,1,3,* Lin Ding,1,2 Jin Yang,1,2 Shou-Min Bai1,2
1Guangdong Provincial Key Laboratory of Malignant Tumor Epigenetics and Gene Regulation, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, 510120, People’s Republic of China; 2Department of Radiation Oncology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, 510120, People’s Republic of China; 3Department of Gynecological Oncology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, 510120, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shou-Min Bai
Department of Radiation Oncology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, 510120, People’s Republic of China
Tel/Fax +86-20-34070680
Email [email protected]
Purpose: We aimed to determine the effect of neoadjuvant chemotherapy consisting of albumin-bound paclitaxel (“nab-paclitaxel”) and platinum (NACT-nPP) in patients with locally advanced cervical cancer (LACC).
Methods: Consecutive patients with newly diagnosed, non-metastatic LACC were recruited retrospectively between October 2016 and June 2020 in our hospital. All patients received concurrent chemoradiotherapy (CCRT) alone or neoadjuvant chemotherapy. We compared the complete response (CR) rate and 2-year progression-free survival (PFS) between patients receiving NACT-nPP and not receiving regimens or other regimens of neoadjuvant chemotherapy.
Results: A total of 195 patients were enrolled (78 in the NACT-nPP group and 117 in the control group). Upon chemoradiotherapy completion, 72 (92.3%) patients in the NACT-nPP group and 96 (82.1%) patients in the other group achieved CR (P = 0.042). For patients with squamous cell carcinoma, the NACT-nPP group had superior 2-year PFS than that of the control group (89.7% vs 74.1%, P = 0.027, HR = 2.486, 95% CI = 1.077– 5.739) whereas for adenocarcinoma, 2-year PFS was 37.5% and 36.5%, respectively (P = 0.863). In multivariate analysis, NACT-nPP and stage were independent prognostic factors (P = 0.046 and 0.012, HR = 2.357 and 2.499, 95% CI = 1.016– 5.465 and 1.216– 4.930, respectively). The acute hematological adverse events above grade 3 were manageable in the NACT-nPP group (46.2%, 36/78), and the rate was lower than that in the control group (55.6%, 65/117).
Conclusion: Compared with CCRT alone, NACT-nPP followed by CCRT could improve the CR rate and 2-year PFS of patients with locally advanced cervical squamous cell carcinoma, and the toxicity was tolerable. NACT-nPP was an independent prognostic factor for 2-year PFS. However, further prospective studies are needed to confirm our results.
Keywords: neoadjuvant chemotherapy, cervical cancer, complete response, nab-paclitaxel, progression-free survival
Introduction
Cervical cancer ranks the fourth most common and is the sixth leading cause of cancer-based death in women. Eighty-five percent of new patients are located in developing countries.1,2 For locally advanced cervical cancer (LACC), concurrent chemoradiotherapy (CCRT) is the main treatment modality.3–6 However, residual tumor is common after treatment (especially for those with large masses) and imperils tumor control and patient survival. The 5-year overall survival rate of LACC is only 50–75%.7,8 How to reduce the residual tumor and improve the long-term survival of patients with LACC remain clinical challenges.
Neoadjuvant chemotherapy (NACT) has been demonstrated to increase the tumor-resection rate and improve the survival of patients with breast cancer and esophageal cancer.9,10 However, the role of NACT in treatment of cervical cancer is controversial. It has been reported that NACT can help to implement fertility-sparing surgery or improve the resection and survival rate in cervical cancer.11,12 Conversely, some studies have demonstrated that NACT addition may be inferior to CCRT alone or surgery alone.8,13 Thus, clarifying the effect of NACT on cervical cancer is important.
Most chemotherapy regimens used previously have been platinum combined with traditional paclitaxel or some non-preferred choice.8,13 Albumin-bound paclitaxel (“nab-paclitaxel”) has several advantages over traditional paclitaxel: higher therapeutic dose, higher distribution in the tumor, and lower toxicity.14,15 The recommended dose of nab-paclitaxel is almost twice that of traditional paclitaxel. We observed that NACT consisting of nab-paclitaxel and platinum (NACT-nPP) obtained a higher tumor response rate than that for patients using other regimens.
Thus, in the present study, we compared the complete response (CR) rate and 2-year progression-free survival (PFS) between patients who underwent NACT-nPP and patients who received no or other regimens of NACT followed by CCRT, retrospectively.
Materials and Methods
Patient Characteristics
Between October 2016 and June 2020, all patients with newly diagnosed, non-metastatic cervical cancer who received radical radiotherapy (including external-beam radiotherapy (EBRT) and brachytherapy) were screened in our hospital. All clinical records were reviewed by the authors.
The inclusion criteria were: (i) the diagnosis of cervical cancer was confirmed with a biopsy; (ii) no distant metastasis was confirmed by gynecological and imaging examinations; (iii) stage IIA to IIIB; (iv) the radiation dose was not less than the recommended dose; (v) pathology was squamous cell carcinoma, adenocarcinoma, or adenosquamous carcinoma; (vi) age >18 years.
The exclusion criteria were: (i) patients received surgery; (ii) presence of other cancer types; (iii) pregnant or lactating women; (iv) previous history of radiotherapy; (v) incomplete data on clinical treatment; (vi) imaging or gynecological examination showed obvious invasion of the inner wall of the bladder or rectum, but endoscopic biopsy was not confirmed.
Staging
All patients received systematic imaging examinations (chest radiography, computed tomography (CT) or ultrasonography of the abdomen, pelvic-enhanced magnetic resonance imaging (MRI), or whole-body 18F-fluorodeoxyglucose positron emission tomography/CT) to exclude distant metastasis.
Two experienced gynecological oncologists (>10 years of clinical experience) were consulted to determine disease staging, and disagreement was resoved through discussion. All patients had their disease staged according to the 2018 International Federation of Gynecology and Obstetrics (FIGO) classification.
Chemotherapy and Radiotherapy
Patients were divided into two groups. The test arm received NACT-nPP. The control arm received no or other regimens of NACT, such as cisplatin or carboplatin combined with traditional paclitaxel or liposomal paclitaxel. All patients received concurrent platinum-based chemotherapy. Before 2019, traditional paclitaxel combined with cisplatin was used primarily whereas, after 2019, the chemotherapy regimen changed gradually to nab-paclitaxel combined with platinum. Nab-paclitaxel and traditional paclitaxel was delivered, respectively, at a dose of 260 mg/m2 and 135 mg/m2, and the cisplatin dose was 50–75 mg/m2.
All patients received EBRT and brachytherapy. Intensity-modulated radiotherapy was used for EBRT with a total dose of 45–50.4 Gy in 25–28 fractions at 1.8 Gy/fraction to the planning target volume. Grossly involved nodes were boosted with an additional 10–15 Gy of highly conformal (and reduced-volume) EBRT. All patients were treated with one fraction daily over 5 days per week.
Upon near completion of EBRT, a high dose rate of brachytherapy was given using an iridium-192 source. Three-dimensional (3-D) planning was used in the first three fractions, and the remainder was 2-D planning. For 3-D planning, the target volume was contoured on CT according to interstitial needles and intracavitary applicators. If vaginal involvement was over 1/2, the whole vagina was included, otherwise, the upper half of the vagina was contoured. The rectum, bladder, and sigmoid colon were delineated as the organs at risk. The prescription was delivered to the outer edge of the target volume for 3-D planning and point A for 2-D planning. Brachytherapy was applied at a total dose of 30–36 Gy in 5–6 fractions at 6 Gy/fraction, 1 fraction daily over 1–2 days per week.
Evaluation of Tumor Response
Upon CCRT completion, two experienced gynecological oncologists undertook a complete gynecological examination, respectively, to evaluate the tumor situation. Disagreement was resolved through discussion, and the results were documented. Ultrasound or enhanced CT/MRI of the pelvis were undertaken. According to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, CR was assessed through gynecological examination and radiography after treatment completion.16
Follow-Up and Statistical Analyses
All patients were evaluated every 3 months during the first 2 years, and every 6 months during the next 3 years, and annually thereafter. All patients were followed up until death or 15 July 2021. For those followed-up >2 years, we collected data until 2 years after treatment initiation. “PFS” was defined as the time from first treatment to the date of disease progression or death as a result of any cause.17,18 Patients who did not experience disease progression or death were censored at the time of the final follow-up.
Data were analyzed using SPSS 21.0 (IBM, Armonk, NY, USA). The χ2 test or Fisher’s exact test was used to compare ordinal variables and the CR rate between groups. PFS was estimated using the Kaplan–Meier method, and differences in survival curves were compared by the Log rank test. Univariate and multivariate analyses using the Cox proportional hazards model were undertaken to evaluate the independent significance of predictors. P < 0.05 (two-tailed) was considered significant.
Results
Patient Characteristics
Between October 2016 and June 2020, 241 patients with non-metastastic cervical cancer received CCRT in our hospital. Forty-six patients were excluded due to the reasons listed in the exclusion criteria and 195 patients were enrolled. Of these, 78 patients received NACT-nPP (21, 36 and 21 patients received 1, 2, 3 cycles of NACT-nPP, respectively) and 117 in the control group (63, 22 and 3 patients received 1, 2, 3 cycles of NACT, respectively, and 29 patients received CCRT alone). Traditional paclitaxel or liposomal paclitaxel were the main chemotherapy regimens used in the control group.
In all patients, the median age was 55 years. At the time of the diagnosis, 132 patients were postmenopausal. The number of patients with stage-II and -III disease was 118 and 77, respectively. Ninety patients had complications, including cardiovascular and cerebrovascular diseases, diabetes mellitus, or severe diseases of the liver, kidneys, or lungs. A total of 105 patients experienced chief complaint symptoms for <3 months before treatment. The histology type included 178 squamous cell carcinomas and 17 adenocarcinomas. The serum level of antigens for squamous cell carcinoma was higher than the cutoff for the upper limit of normal in 139 patients. The distribution of the factors mentioned above was not significantly different between the two arms (Table 1).
 |
Table 1 Characteristics of the 195 Patients with Cervical Carcinoma Enrolled in This Study |
CR and 2-Year PFS
Through comprehensive assessment, we found that 72 (92.3%) achieved CR in the NACT-nPP group and 96 (82.1%) patients achieved CR in the control group (P = 0.042) (Table 2).
 |
Table 2 Comparison of Complete Response Between Patients Who Did or Did Not Undergo NACT-nPP |
Tumor progression occurred in 42 (21.5%) patients (9 in the NACT-nPP group and 33 in the control group (P = 0.042)). Overall, 18 patients had isolated distant metastasis; 11 patients had local-regional recurrences and 13 patients had local-regional recurrences combined with distant metastases. There was significant difference in 2-year PFS (87.6% vs 70.4%, P = 0.017, hazard ratio (HR) = 2.383, 95% confidence interval (CI) = 1.139–4.987) between the NACT-nPP group and control group (Table 3 and Figure 1A). Further subgroup analysis was undertaken according to histology type. We found the NACT-nPP had superior 2-year PFS than that in the control group for squamous cell carcinoma (89.7% vs 74.1%, P = 0.027, HR = 2.486, 95% CI = 1.077–5.739 (Table 3 and Figure 1B). However, this superiority was not observed for adenocarcinoma (37.5% vs 36.5%, P = 0.863) (Figure 1C).
 |
Table 3 Two-Year PFS Among All Included Patients and Patients with Squamous Cell Carcinoma |
 |
Figure 1 Two-year PFS curve for all 195 patients (A), patients with squamous cell carcinoma (B) and pateints with adenocarcinoma (C). |
We conducted univariate and multivariate analysis for 2-year PFS among patients with squamous cell carcinoma. In univariate analysis, only NACT-nPP and stage (FIGO 2018) were associated with PFS (P < 0.05). These two factors and CR were analyzed further in multivariate analysis. NACT-nPP (HR = 2.357, 95% CI = 1.016–5.465, P = 0.046) and stage (FIGO 2018) (HR = 2.499, 95% CI = 1.216–4.930, P = 0.012) were significant independent indicators for PFS. Multivariate survival outcome analyses are summarized in Table 4.
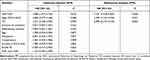 |
Table 4 Multivariate Analysis for 2-Year PFS Among Patients with Squamous Cell Carcinoma |
Toxicity
Hematological and gastrointestinal adverse effects were the most common types of acute toxicity, and most events were manageable. Hematological toxicity of grade 3–5 was presented in 100 patients during the entire treatment (35 (44.9%) in the NACT-nPP group and 65 (55.6%) in the control group). One patient using liposomal paclitaxel and carboplatin died shortly after CCRT completion due to thrombocytopenia and hemorrhage. The incidence rate of hematological toxicity above grade 3 in the NACT-nPC group (35/78) was lower than that in the control group (65/117). One patient without hematological toxicity above grade 3 in the NACT-nPP group and control group, respectively, had an intestinal perforation, and recovered after care in the intensive care unit and systemic treatment. Late adverse events in the NACT-nPP group included one case of radiation proctitis and one case of ureteral obstruction. In the control group, one patient suffered a colonic fistula and four cases had a ureteral obstruction.
Discussion
CCRT is first-line treatment for patients with LACC,3–6 but the tumor-control rate and long-term survival are unsatisfactory, especially for those with stage-IIIB or -IVA disease, many of whom have a residual tumor, tumor progression or even die shortly after CCRT.19 Therefore, reducing the residual tumor and improving survival of such patients are urgent clinical problems that need resolution.
NACT can lessen the tumor load and involvement of the lymph–vascular space, and increase the sensitivity to radiation.20 For many locally advanced tumors, NACT has been shown to improve tumor control and patient survival, and has become an important part of standard treatment.9,10 However, the role of NACT in cervical cancer is unclear, and determination of the role and exploration of the optimal regimens of NACT for LACC are needed.
We found the patients who received NACT-nPP following by CCRT had a higher CR rate than others upon CCRT completion (92.3% vs 82.1%, P = 0.042). Initally, we attributed this observation to the higher therapeutic dose of nab-paclitaxel, the recommended dose of which is 260 mg/m2, which is nearly twice that of traditional paclitaxel (135 mg/m2). Hence, the advantage of a higher dose translated into a higher rate of tumor regression.
After treatment completion, the CR rate of the control group was 82.1%, similar to that of patients who received CCRT alone in a previous study.8 This observation could be explained by three main factors: (i) the control group in our study included some patients who underwent CCRT alone; (ii) NACT regimens in this group included traditional paclitaxel or liposomal paclitaxel combined with cisplatin, carboplatin, or other types of platinum, which have been reported to offer no advantage on survival for LACC;8,13 (ii) the cisplatin dose intensity in our study was 17–25 mg/m2/week, lower than 25 mg/m2/week, which is the cutoff value that offers a benefit.21 However, a promising clinical CR rate of 92.3% in the NACT-nPP group was obtained. This value is higher than that reported previously: 56.3–86.54%.8,22 Besides the advantage of a stronger dose intensity of nab-paclitaxel elaborated above, three other factors might also explain this observation: (i) NACT reduced the tumor volume, and a massive tumor has more chance to be covered completely with a radical radiation dose; (ii) NACT decreased the hypoxia of tumor cells and increased their radiation sensitivity;23 (iii) the radiotherapy process from visiting the physician to CT simulation, delineation of the target volume, as well as planning, verification and starting radiotherapy took (on average) >1 month. During this period, patients undergoing CCRT alone did not receive any treatment, whereas patients undergoing NACT received chemotherapy usually 1 week after the visit and started the radiotherapy process simultaneously. One-to-two cycles of NACT were carried out upon radiotherapy initiation. Therefore, patients with NACT followed by CCRT received treatment earlier than those who had CCRT alone.
The treatment response to NACT is an independent risk factor of the prognosis for patients with LACC.22,24 A meta-analysis involving 13 studies found that the clinical response to NACT was associated with longer overall survival (HR = 3.36, P < 0.00001) and disease-free survival (HR = 2.36, P < 0.00001), and the pathological response also predicted favorable overall survival (HR = 5.45, P < 0.00001) and disease-free survival (HR = 3.61, P < 0.00001).22 In another study, 58.9% of patients with stage-IB2–IIA2 disease receiving platinum-based NACT achieved a response and 8.7% of patients achieved a pathologic CR. NACT responders showed significantly better overall survival (HR = 2.453, P = 0.024) and PFS (HR = 2.196, P < 0.013).24 Unfortunately, in multivariate analysis, the improved CR was not an independent prognostic factor (HR = 0.899, 95% CI = 0.315–2.570, P = 0.843). This inconsistency was explicable: the previous studies evaluated the treatment response to NACT before radical treatment, whereas we evaluated the treatment response upon CCRT completion. Thus, the CR rate was much higher than that in previous studies and reflected the combined effect of NACT and CCRT, but not the effect of NACT alone. Besides, most of the previous studies reported the pathological response, whereas we evaluated the clinical response.
Patients in the NACT-nPP group had superior PFS (87.6% vs 70.4%, P = 0.017). This result is in accordance with a meta-analysis of 18 randomized trials comparing NACT with radical radiotherapy alone. The authors found that NACT addition could improve survival for LACC in trials with chemotherapy cycle lengths ≤14 days or a cisplatin dose intensity ≥25 mg/m2/week (HR = 0.83, P = 0.046).21 In another meta-analysis involving early or advanced cervical cancer, NACT addition could improve overall survival (HR = 0.77, P = 0.02) and PFS (HR = 0.75, P = 0.008) of patients undergoing radical surgery.25 Marita et al retrospectively analyzed the objective response, overall survival, and disease-specific survival of LACC patients. They found that NACT followed by CCRT resulted in higher response rates and improvements in disease-free survival and disease-specific survival compared with that using CCRT alone.26 Conversely, some studies deemed NACT to be detrimental to patients. Da Costa et al found that, compared with CCRT alone, addition of NACT comprsing cisplatin and gemcitabine was associated with inferior 3-year PFS (40.9% vs 60.4%, HR = 1.84; P = 0.033) and overall survival (60.7% vs 86.8%; HR = 2.79; P = 0.006), with even lower response rates discovered upon treatment cessation (56.3% vs 80.3%; P = 0.008).8
Upon subset analyses, the NACT-nPP group showed superior 2-year PFS in patients with squamous cell carcinoma (89.7% vs 74.1%, P = 0.027) but not adenocarcinoma (37.5% vs 36.5%, P = 0.863). In multivariate analysis, beside of the stage (FIGO 2018), the NACT-nPP (HR = 2.357, 95% CI = 1.016–5.465, P = 0.046) were the only two independent prognostic risk factors for 2-year PFS. This result is in accordance with a study that suggested CCRT benefits the survival of only postoperative patients with squamous cell carcinoma, but not those with adenocarcinoma.27,28 The higher 2-year PFS rate of squamous cell carcinoma than that of adenocarcinoma may be due to the histopathological characteristics of greater malignancy. In addition, the small number of patients (n = 17) with adenocarcinoma may also have led to deviation of survival results.
The nab-paclitaxel dose was higher than that used for traditional paclitaxel, which improved the CR rate of the tumor but did not improve acute or chronic adverse events. Conversely, possibly because of preventive use of polyethylene glycol recombinant human granulocyte colony-stimulating factor, the hematological toxicity was lower. Besides hematological toxicity, grade-1–2 diarrhea was also common, which could be relieved after symptomatic treatment. In addition, NACT-nPP did not increase long-term toxicity.
Conclusions
Compared with CCRT alone, NACT-nPP followed by CCRT could improve the CR rate and 2-year PFS of patients with locally advanced cervical squamous cell carcinoma, and the toxicity was tolerable. NACT-nPP was an independent prognostic factor for 2-year PFS. However, further prospective studies are needed to confirm our results.
Abbreviations
LACC, locally advanced cervical cancer; NACT-nPP, neoadjuvant chemotherapy consisting of nab-paclitaxel and platinum; CCRT, concurrent chemoradiotherapy; NACT, neoadjuvant chemotherapy; CR, complete response; FIGO, International Federation of Gynecology and Obstetrics; EBRT, external beam radiotherapy.
Data Sharing Statement
The datasets for this study has been uploaded in the additional files section.
Ethics Approval
This retrospective study was approved by the Ethics Committees of Sun Yat-sen Memorial Hospital, Sun Yat-sen University, and the requirement to obtain informed consent was waived [SYSEC-KY-KS-2021-108]. All the data were analyzed anonymously. This study was conducted in accordance with the Declaration of Helsinki.
Funding
There is no funding to report.
Disclosure
The authors indicated no financial disclosures or potential conflicts of interest.
References
1. Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. doi:10.3322/caac.21654
2. Ferlay J, Soerjomataram L, Dikshit R, et al. Cancer incidence andmortality worldwide: sources, methods and major patterns in GLOBOCAN2012. Int J Cancer. 2015;136(5):E359–86. doi:10.1002/ijc.29210
3. Rose PG, Bundy BN, Watkins EB, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340(15):1144–1153. doi:10.1056/NEJM199904153401502
4. Morris M, Eifel PJ, Lu J, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999;340(15):1137–1143. doi:10.1056/NEJM199904153401501
5. Lanciano R, Calkins A, Bundy BN, et al. Randomized comparison of weekly cisplatin or protracted venous infusion of fluorouracil in combination with pelvicradiation in advanced cervix cancer: a gynecologic oncology group study. J Clin Oncol. 2005;23(33):8289–8295. doi:10.1200/JCO.2004.00.0497
6. Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: asystematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. 2008;26(35):5802–5812. doi:10.1200/JCO.2008.16.4368
7. Wang YM, Wang CJ, Fang FM, et al. Differences in the outcomes and complications between elderly and younger uterine cervical cancer patients treated by definitive radiotherapy - A propensity score-matched study. Gynecol Oncol. 2017;145(2):277–283. doi:10.1016/j.ygyno.2017.02.034
8. da Costa SCS, Bonadio RC, GabrielliF CG, et al. Neoadjuvant chemotherapy with cisplatin and gemcitabine followed by chemoradiation versus chemoradiation for locally advanced cervical cancer: a randomized Phase II trial. J Clin Oncol. 2019;37(33):3124–3131. doi:10.1200/JCO.19.00674
9. Mougalian SS, Soulos PR, Killelea BK, et al. Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer. 2015;121(15):2544–2552. doi:10.1002/cncr.29348
10. Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681–692. doi:10.1016/S1470-2045(11)70142-5
11. Tesfai FM, Kroep JR, Gaarenstroom K, et al. Fertility-sparing surgery of cervical cancer >2 cm (International Federation of Gynecology and Obstetrics 2009 stage IB1-IIA) after neoadjuvant chemotherapy. Int J Gynecol Cancer. 2020;30(1):115–121. doi:10.1136/ijgc-2019-000647
12. Fröbe A, Jones G, Bokulić T, et al. High-dose-rate brachytherapy and concurrent chemoradiotherapy followed by surgery for stage Ib-IIb cervical cancer: single institution experience. Anticancer Res. 2014;34(7):3861–3866.
13. Gupta S, Maheshwari A, Parab P, et al. Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. J Clin Oncol. 2018;36(16):1548–1555. doi:10.1200/JCO.2017.75.9985
14. Zhao P, Wang Y, Wu AH, et al. Roles of albumin-binding proteins in cancer progression and biomimetic targeted drug delivery. Chembiochem. 2018;19(17):1796–1805. doi:10.1002/cbic.201800201
15. Chen N, Brachmann C, Liu XP, et al. Albumin-bound nanoparticle (nab) paclitaxel exhibits enhanced paclitaxel tissue distribution and tumor penetration. Cancer Chemother Pharmacol. 2015;76(4):699–712. doi:10.1007/s00280-015-2833-5
16. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. doi:10.1016/j.ejca.2008.10.026
17. Stone A, Wheeler C, Carroll K, et al. Optimizing randomized phase II trials assessing tumor progression. Contemp Clin Trials. 2007;28(2):146–152. doi:10.1016/j.cct.2006.05.003
18. Dancey JE, Dodd LE, Ford R, et al. Recommendations for the assessment of progression in randomised clinical trials. Eur J Cancer. 2009;45(2):281–289. doi:10.1016/j.ejca.2008.10.042
19. McCormack M, Kadalayil L, Hackshaw A, et al. A phase II study of weekly neoadjuvant chemotherapy followed by radical chemoradiation for locally advanced cervical cancer. Br J Cancer. 2013;108(12):2464–2469. doi:10.1038/bjc.2013.230
20. Wang Y, Wang G, Wei LH, et al. Neoadjuvant chemotherapy for locally advanced cervical cancer reduces surgical risks and lymph-vascular space involvement. Chin J Cancer. 2011;30(9):645–654. doi:10.5732/cjc.011.10050
21. Neoadjuvant Chemotherapy for Locally Advanced Cervical Cancer Meta-analysis Collaboration. Neoadjuvant chemotherapy for locally advanced cervical cancer: a systematic review and meta-analysis of individual patient data from 21 randomised trials. Eur J Cancer. 2003;39(17):2470–2486. doi:10.1016/S0959-8049(03)00425-8
22. Zhu YS, Yang JH, Zhang X, et al. Acquired treatment response from neoadjuvant chemotherapy predicts a favorable prognosis for local advanced cervical cancer: a meta-analysis. Medicine. 2018;97(17):e0530. doi:10.1097/MD.0000000000010530
23. Panici PB, Scambia G, Greggi S, et al. Neoadjuvant chemotherapy and radical surgery in locally advanced cervical carcinoma: a pilot study. Obstet Gynecol. 1988;71(3 Pt 1):344–348.
24. Huang YH, Liu L, Cai J, et al. The efficacy and response predictors of platinum-based neoadjuvant chemotherapy in locally advanced cervical cancer. Cancer Manag Res. 2020;12:10469–10477. doi:10.2147/CMAR.S270258
25. Rydzewska L, Tierney J, Vale CL, et al. Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev. 2012;12(12):CD007406. doi:10.1002/14651858.CD007406.pub3
26. Marita A, Ordeanu C, Rancea A, et al. Long-term survival following neoadjuvant chemotherapy and concomitant radiochemotherapy in locally advanced cervical cancer: results of the oncology institute “Prof. Dr. Ion Chiricuta” experience. J Med Life. 2018;11(1):42–50.
27. Kim YJ, Lee KJ, Park KR, et al. Prognostic analysis of uterine cervical cancer treated with postoperative radiotherapy: importance of positive or close parametrial resection margin. Radiat Oncol J. 2015;33(2):109–116. doi:10.3857/roj.2015.33.2.109
28. Dávila Fajardo R, van Os R, Buist MR, et al. Post-operative radiotherapy in patients with early stage cervical cancer. Gynecol Oncol. 2014;134(1):52–59. doi:10.1016/j.ygyno.2014.04.045
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
