Back to Journals » Medical Devices: Evidence and Research » Volume 16
Endotracheal Intubation of Difficult Airways in Emergency Settings: A Guide for Innovators
Authors Maguire S , Schmitt PR , Sternlicht E, Kofron CM
Received 4 May 2023
Accepted for publication 5 July 2023
Published 18 July 2023 Volume 2023:16 Pages 183—199
DOI https://doi.org/10.2147/MDER.S419715
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Samantha Maguire, Phillip R Schmitt, Eliza Sternlicht, Celinda M Kofron
Center for Biomedical Engineering, School of Engineering, Brown University, Providence, RI, USA
Correspondence: Celinda M Kofron, School of Engineering, Brown University, 184 Hope Street, Providence, RI, 02912, USA, Tel +1 401 863 9992, Fax +1 401 863 1238, Email [email protected]
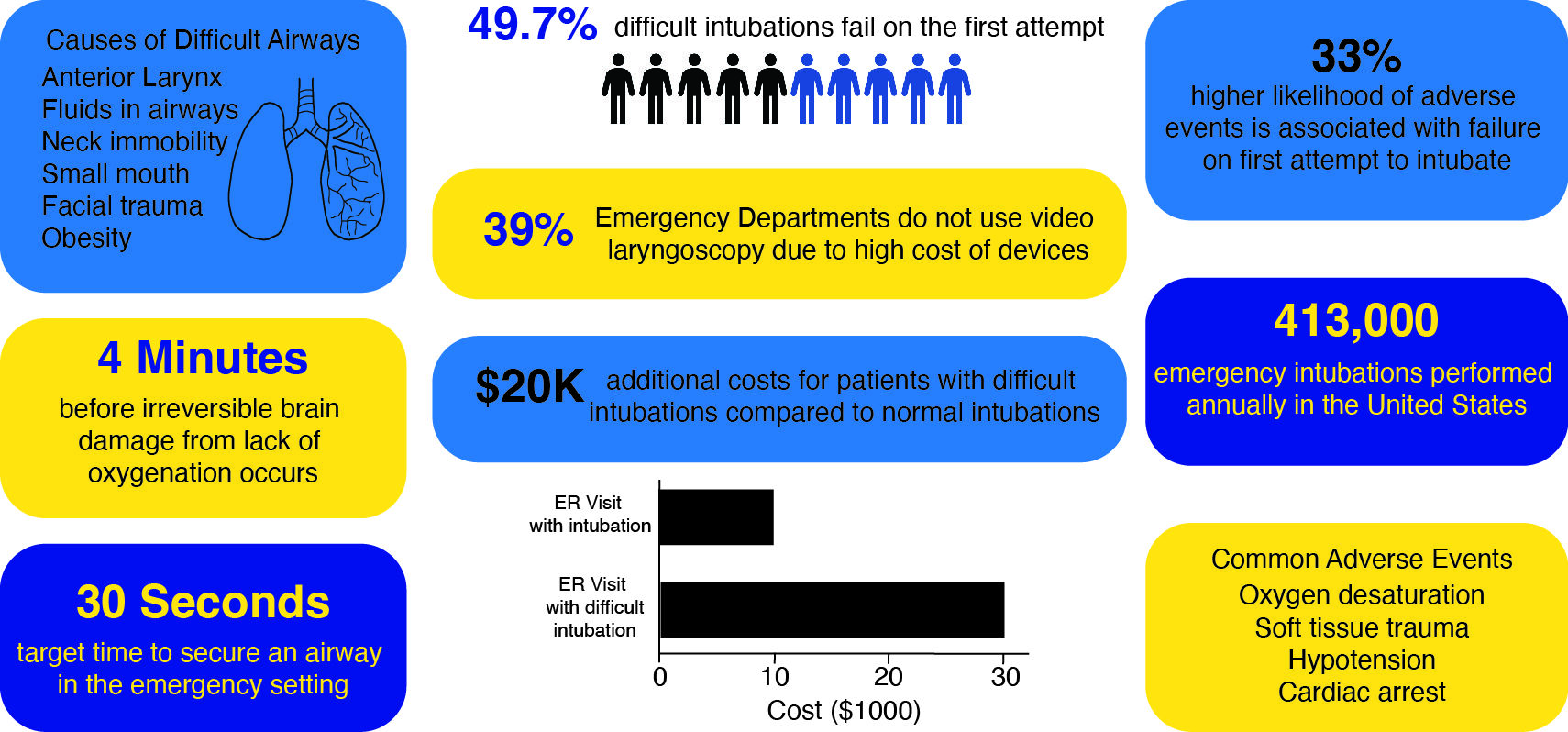
Abstract: Over 400,000 Americans are intubated in emergency settings annually, with indications ranging from respiratory failure to airway obstructions to anaphylaxis. About 12.7% of emergency intubations are unsuccessful on the first attempt. Failure to intubate on the first attempt is associated with a higher likelihood of adverse events, including oxygen desaturation, aspiration, trauma to soft tissue, dysrhythmia, hypotension, and cardiac arrest. Difficult airways, as classified on an established clinical scale, are found in up to 30% of emergency department (ED) patients and are a significant contributor to failure to intubate. Difficult intubations have been associated with longer lengths of stay and significantly greater costs than standard intubations. There exists a wide range of airway management devices, both invasive and noninvasive, which are available in the emergency setting to accommodate difficult airways. Yet, first-pass success rates remain variable and leave room for improvement. In this article, we review the disease states most correlated with intubation, the current landscape of emergency airway management technologies, and the market potential for innovation. The aim of this review is to inspire new technologies to assist difficult airway management, given the substantial opportunity for translation due to two key-value signposts of medical innovation: the potential to decrease cost and the potential to improve clinical outcomes.
Keywords: laryngoscopy, emergency airway management, innovation, difficult airway, intubation
Graphical Abstract:
Plain Language Summary
When analyzing the current medical device market, the available tools for emergency airway management (EAM) appear comprehensive and highly effective. However, there is a wide range of health conditions and patient circumstances that require EAM. Each patient may need a unique device to be successfully treated based on his or her condition. This range of needed tools suggests that niche gaps in the market may exist upon further investigation. Here, we find that most devices that are normally successful will often fall short of optimal performance in patients with difficult airways. Difficult airways encompass any abnormal anatomy or injury to the throat.
This review aims to provide a comprehensive guide for the current state of airway management. We report on the wide range of existing devices and types of EAM procedures. Additionally, we provide further evaluation of the healthcare market including cost, efficacy, and average speed of EAM to identify potential gaps. Thus, this review serves as an overview of EAM to motivate and guide potential innovators to design improved airway management devices, specifically geared towards difficult airways.
Introduction
Emergency airway management (EAM) is a temporary solution which aims to quickly establish a direct path of oxygen delivery to the lungs for patients in respiratory distress in emergency settings. The majority of EAMs are achieved by methods of intubation. Over 413,000 intubations are performed annually in US EDs, including roughly 1% of all emergency room visits.1 When the brain fails to signal for respiration, clinicians typically have less than 15–30 seconds to secure an airway before the potential onset of hypoxia and brain damage.2 There exists a wide range of airway management devices to accommodate the various conditions which indicate intubations, all of which are evaluated based on first-pass success rate (FSR) and time for insertion.3
Failure to intubate on the first attempt is associated with a 33% higher likelihood of patients experiencing adverse events, including oxygen desaturation, aspiration, soft-tissue trauma, hypotension, dysrhythmia, and cardiac arrest.4 The first-pass success heavily depends on whether an airway is considered difficult or typical, as difficult airways are primary predictors for complications.1,4,5 The estimated percent of airways classified as difficult ranges from 10.1% - 30%, comprising a significant portion of EAM patients.6,7 Difficult airways are associated with statistically significant decreased FSRs relative to typical airways, with average reports of 82.1% and 92.4%, respectively.8 In some reports, 49.7% of difficult airway intubations are unsuccessful on the first attempt. Additionally, these success rates depend on the use of an appropriate device for airway management.9,10 Thus, two crucial components to approaching successful intubation include systematic evaluation of difficult airways and adequate training with appropriate tools by the physician.
Airway management by tracheal intubation, or insertion of a tube into the trachea through the mouth to maintain an open airway, can be traced back to the Greek and Roman empires. The Romans notably used dental mirrors to visualize the airway, similar to modern direct laryngoscopy (DL).11 Alfred Kirstein, however, is the notable pioneer of DL after manufacturing an intubation device with an internal electrical source to illuminate the throat for direct visualization.12 Soon after during World War II, more advanced innovations introduced the straight Miller blade and curved Macintosh blade, which are commonly used today.13,14 In the 1990s, DL blades were combined with fiber-optic cables to enhance illumination. In the 2000s, this innovation was further enhanced to create the indirect video laryngoscope. The video laryngoscope (VL) has a small fiber-optic camera and light on the end of the blade, which is connected to a video screen to project a live image of the throat to guide intubation.15 In the United States, meta-analyses and retrospective studies have demonstrated that video laryngoscopy typically improves first pass success rate relative to DL across clinical settings.15 Video laryngoscopy facilitates shorter intubation times in patients with normal and difficult airways and higher first-pass success rates in difficult airways.16 Additionally, VL is associated with higher success rates in untrained physicians.16 However, while VL has improved outcomes, video laryngoscopes are limited in availability in emergency settings. With market analysis indicating that VLs cost between $500–15,000, the price point is a logical deterrent for purchase, which will be discussed in detail later in this review.3 Additional deterrents include non-reusable parts and required power supply, which are hardships in remote, low-resource settings. Retrospective studies suggest that video laryngoscopes also have higher bills for hospitalized patients compared to direct laryngoscopes.17
Intubations are indicated for patients unable to maintain airway patency, aspiration prevention, ventilation failures, or insufficient oxygenation, or anticipated respiratory failure.18 Before intubation in the ED, several metrics are used to evaluate if a patient has a difficult airway, including the Glasgow scale, the LEMON protocol, and Cormack-Lehane Grading. These three classifications, along with the physician’s subject opinion, help to determine the appropriate device for EAM. While these metrics determine the proper instrument before the procedure, the protocol for the utilization of different EAM tools follows the same standard steps, as described here. The patient is pre-oxygenated for at least 3 minutes, which saturates the blood to prolong the time available for intubation without complications. Rapid Sequence Intubation (RSI) is commonly implemented in 80–85% of ED intubations because it can reduce the risk of pulmonary aspiration while preventing coughing or straining of the throat which could impede intubation.19 If prescribed RSI, the patient receives a paralytic medication, an anesthetic or sedative, and a pain medication.19 Next, the physician will use the classification recommended device, as indicated by the previously mentioned metrics, for intubation to establish a secure airway, which is most commonly a direct or indirect laryngoscope.
Laryngoscopy intubation requires two steps: visualization of the vocal cords with a laryngoscope, either direct or indirect, and subsequent insertion of an endotracheal tube (ETT) past the laryngoscope, through the larynx, and into the trachea.20 DL involves visualization of the larynx by eyesight using light, whereas indirect laryngoscopy (IDL), or VL, achieves visualization with a fiber-optic camera attached to the end of the laryngoscope blade. The properly inserted ETT is connected to a ventilator which replaces autonomic respiration with positive-pressure ventilation. In the ED, the first-pass approach is most commonly video laryngoscopy, and if this fails, methods including a Bougie, laryngeal airway mask (LMA), or surgical airways may be employed, which will be discussed later in this review. When intubation is unsuccessful, it is likely attributable to the provider’s inability to visualize the larynx. For experienced providers, this often happens because of difficult anatomy for intubation, excess fluids in the airway, or trauma to the airway.21 When a patient is determined to have a difficult airway during the physician’s assessment before intubation, the risk for injury or failed first-pass attempt is drastically increased compared to typical airways.22 The related disease states and specific risk factors for difficult intubations will be reviewed here. Thus, the gap in success rates for difficult airway intubations presents an opportunity for improvement in innovation, to maximize first pass success rates and minimize the time for ETT insertion in emergency settings.
Here, we evaluate the current standard of care for EAM and highlight the potential for novel device innovation and further improvements. We review the disease states indicative of the need for intubation, the efficacy of existing technologies, and the market potential for airway management devices. Due to the already diverse approaches to airway management, the active goal of new technology development should be specific to address existing gaps in airway management. The need for improvement in intubation approaches is further motivated by the increased EAM incidence during the COVID-19 pandemic. One study found a 100% increase in their emergent non-operating-room intubations during April 2020, with most cases attributed to COVID-19-positive patients.23 Another report found a 300% increase in the prevalence of intubations for COVID-19 patients relative to total intubation prevalence in the ED.23 Case studies of individual clinics have reported up to a 17.8% intubation rate for COVID-19 patients.24 The unanticipated prevalence of emergency intubations during the pandemic further motivates the urgency of identifying and filling gaps in laryngoscopy innovation. This review aims to synthesize existing literature and technologies on methods of intubation for difficult airways, with the overarching goal of inspiring and guiding future innovations for improving the state of airway management.
Discussion
Intubation is Common and Indications Span Acute and Chronic Conditions
Endotracheal intubations are performed for roughly 1% of all emergency room visits.1 In US EDs, 12.7% of intubations are unsuccessful on the first attempt.4 Of the conditions which indicate the need for airway management, respiratory failure, airway obstruction, and cardiac arrest together account for the highest incidence of emergency intubation.1,2 Risk factors for requiring intubation include advanced age, obesity, history of substance abuse, diabetes, and seizure disorders, while risk factors for difficult intubations are mainly obesity and airway malformation.5 Additionally, loss of consciousness accompanied by vomiting and/or the presence of blood or other fluids near the airway, low peripheral oxygenation, wet respiratory sounds, or other indicators that the patient may lose breathing capacity are all indications for intubation.25 Acute respiratory failure incidence in the US has been reported to be close to 135 cases per 100,000 adults.26 Trauma to the airway is a common cause of obstruction in adults. Out of patients with chest and neck traumas, about 0.5–2% have airway obstructions.27 Anaphylaxis is a second cause of airway obstruction, with a prevalence of 2% in the US.27,28 One of the most common causes of airway obstruction in adults is reduced consciousness, due to the inability to control tongue and soft tissue position in the airway and increased risk of aspiration. Reduced levels of consciousness are often seen in patients with acute intoxication, seizure disorders, hypoglycemia, stroke, trauma, severe illness, neurological conditions, and cardiac arrest, among others.29
Outcomes are Not as Favorable Under Difficult Airway Conditions
Three main metrics are used to identify and characterize a difficult airway, which is a highly predictive factor of intubation complications.28 The Glasgow Coma scale for intubation determines the severity of traumatic brain injury, or the risk of such, in a trauma patient. Glasgow score evaluates eye opening, verbal response, and motor response, to generate a score ranging from 0–15. A Glasgow score less than or equal to 8 indicates emergency intubation, and scores 7–9 have the highest correlation with difficult intubations.30,31 A difficult airway is determined by using “LEMON”: a mnemonic of steps to evaluate, including Look externally, Evaluate 3-3-2 rule, Mallampati score (tongue: pharynx size ratio), Obstruction, and Neck Mobility. The LEMON protocol predicts difficult airways with 86% sensitivity.19 After looking for external features that might inhibit intubation such as trauma or facial hair, the 3-3-2 rule is evaluated for optimal intubations, which assesses the geometry and accessibility of the airway.32 The Mallampati scoring system is then used to predict airway difficulty based on the patient airway shape and size. Generally, a lower Mallampati score indicates easier intubation, but some airways may be more difficult or easier to intubate than initially anticipated.33,34 Additionally, physicians may use Cormack-Lehane Grading to grade airway visibility after insertion of a laryngoscope, depending on the ability to visualize the posterior larynx, glottis, and epiglottis. First attempt success rates for intubation drop drastically as airway difficulty score increases, with Cormack-Lehane Grades 1, 2, 3, 4, associated with first-pass success rates of 96%, 85%, 50%, and 14% respectively.34
Determining if a patient has a difficult airway, as indicated by Cormack-Lehane grade of 3–4, Mallampati score of 3–4, Glasgow score of 7–9, or an alternative subjective decision by the clinician, is crucial for identifying the proper intubation procedure. For example, patients with a lower Glasgow scale are more likely to undergo RSI, which uses sedation and neuromuscular blockers to facilitate easier airway management.31 If Cormack-Lehane grades suggest a difficult airway with reduced visualization, video laryngoscopy is the clinical standard for intubation.34 Overall, appropriate measures are required to assess a patient’s internal anatomy and proceed with optimal technology for intubation with maximal first-pass success and minimal insertion time.
When primary attempts at intubation fail, which accounts for about 10% of intubated patients, the risk of complications increases drastically.8 After two unsuccessful attempts, hypoxemia incidence increases ninefold.34 Esophageal intubation, in which the tube is placed into the esophagus rather than the trachea, happens in 51.4% of cases where tracheal intubation had failed after the first two attempts.33,35 Similarly, aspiration and bradycardia incidences increase fourfold compared to successful first- or second-attempt intubations. Finally, the risk for cardiac arrest increases by 6% after two attempts.35 There is no data available for the mortality rate of failed intubations, but from the increased severe complications associated with more than two attempts of intubation, such as cardiac arrest, it can be reasonably inferred that mortality may also correspond to the number of intubation attempts.
Existing Solutions are Rooted in Laryngoscopy
A summary and comparison of the existing devices for EAM can be found in Table 1.
 |
Table 1 Comparison of Existing Airway Management Solutions |
Accessible Solutions Rely on Physician Training and Direct Visualization
When it has been determined that a patient requires intubation and proper preparative measures have been taken, the standard procedure in an ED is laryngoscopy. Laryngoscopy uses a laryngoscope handle, equipped with a light, which is attached to a blade to visualize the vocal cords for guiding insertion of an ETT. There are two types of laryngoscopes for airway management: direct and indirect laryngoscopes.
DL refers to intubation by placing an ETT through the oral cavity into the trachea using, as the name implies, direct visualization. DL is limited by the line-of-sight approach and the requirement for visualizing beyond the tip of a laryngoscope blade for successful laryngeal visualization.36
There are two major blades currently used for DL- the Macintosh and Miller blades.37,41 The Macintosh (Mac) blade is a curved, stainless-steel blade that is ideal for tongue control, which is necessary for proper visualization.38 Additionally, its curve indirectly lifts the epiglottis, facilitating easier ETT insertion. The Mac blade’s curved geometry, which mimics the curve of the tongue, allows for excellent pharynx visualization by tongue suppression, sufficient room for the passage of the ETT by fitting to the bottom of the mouth, and decreases potential trauma to the throat and epiglottis relative to the Miller blade since the Mac blade tip is less proximal to the back of the throat.36 The Miller Blade is a straight, stainless-steel blade with a curved tip.38 The tip directly lifts the epiglottis for visualization, thus providing great exposure, but its straight geometry limits the space available for ETT passage in the back of the airway. The Mac blade pushes the tongue down, allowing for more room to insert an ETT, greater first-pass success rates, and less trauma, while the Miller blade allows for better glottis visualization for floppy epiglottis patients, such as with pediatrics or an anterior larynx, making it more suitable for alternative airway geometries, a subclass of difficult airways.36,38,41 In a review of 500 patients to evaluate different DL blades, physicians reported larynx visualization 96% of the time with the Miller blade, but only 72% of the time with the Mac blade.53 In one study on the use of DL by relatively new clinicians, it was reported that the Mac blade resulted in 100% first-pass successful intubation, versus the Miller blade with a 78.4% success rate, and the mean time of insertion for Mac blades was significantly lower than that for successful insertion using Miller blades.38
DL is ideal for non-difficult airways and is favorable due to the variability in blade size and shape, such as the Miller blade, to accommodate anterior airways in obese patients and floppy glottis in children.9 DL is more widely available in clinical settings due to the disposable, interchangeable, and low-cost equipment it requires. DL can also be coupled with a Bougie (discussed further below) to increase first-pass success.9,32,39
Indirect Visualization Can Be Effective but Relies on Costly Technology
An alternative to DL is IDL, which uses optic assistance for indirect visualization of the oral cavity for ETT insertion. There are three main categories of IDL, including optical stylets, fiber-optic laryngoscopes, and video laryngoscopes.41 As of 2013, the American Society of Anesthesiologists issued a statement that recommended IDL by video laryngoscope (VL) as the initial approach to intubation.4 Since then, video laryngoscopy has been the most utilized and innovative branch of IDL. One meta-analysis reports that VL (encompassing all VL tools) has a 92% first-pass success rate in the ED compared to 86% for DL (encompassing all DL tools).10 Video laryngoscopes have a small camera embedded into the tip of their blade for visualization on a screen, often with a wider range of view than DL. The video is displayed on a screen either connected remotely or directly on the scope, making these tools easy to use for inexperienced practitioners. VLs may either be non-channeled, where the blade and ETT are inserted separately, or channeled, where the blade and ETT are inserted as a single unit and the blade is detached and removed after proper placement of the ETT.3
Common channeled VL include the Airtraq, King Vision Scope, and Pentax AWS.40 The Airtraq is a battery-powered, single-use scope with fog-resistant lenses and an attachable camera.42 The King Vision Scope is a modular non-channeled or channeled VL with an antifog lens and reusable handle. The Pentax AWS produces high-resolution images and has added benefits of channels for built-in suction or additional direct oxygenation but is only available in one-size. Channeled VLs are beneficial by automatically providing a pathway for ETT insertion, but face limitations in mobility and manipulation of the ETT to accommodate variable or irregular airways.4 Common non-channeled VL designs include the Glidescope, McGrath, and C-MAC.40 The Glidescope includes a high-resolution camera in the blade, an attached monitor, disposable blades, and is intended for both routine and difficult laryngoscopy.9,43 The McGrath is an adjustable, single-use blade with an attached monitor on the scope handle and has a greater range of motion (up to 90° swivel). The C-MAC is an adjustable blade with multiple size options and a detachable video technology, so the C-MAC can be used either for IDL or DL.9 The C-MAC also has a curved blade that mimics the geometry of the Mac Blade, which provides familiarity for physicians trained in DL. Both the Glidescope and the McGrath have steeper curves, blocking any direct visualization, but providing a wider view on the monitor.9,10
VL provides a larger visual field than DL, improves glottis exposure, and has been associated with higher first-pass success rate in the ED, higher success rates among trainees and experts, decreased esophageal intubations, and decreased dental and oral trauma.8,9 VL permits an enhanced teaching experience to train doctors, as multiple doctors can view the screen simultaneously, and procedures can be recorded for review. Additionally, VL is more successful in difficult and unusual airway intubation. A systematic review of IDL success reported an OR of 2.07 for first-pass success by VL versus DL in difficult airway patients.40
However, VL has several shortcomings. VL has increased reports of upper airway injury. There is a cost gap of the technology which limits widespread availability, due to its reliance on external power sources and technologies. Consequently, the distribution of video laryngoscopes is uneven, with a sample analysis indicating that only 43% of low-resource EDs in the US have access due to high costs.44 Overall, about 39% of EDs do not have access to VL in the US.54 Additionally, some reports associate VL with increased time for set up, but the total time until insertion between VL and DL is insignificant.19 2D visualization on a screen deprives doctors of depth perception, which has been reported to increase mispositioning and therefore increase time for intubation. Finally, an important disadvantage of VL is the presence of a blind spot during insertion through the pharynx. The oral cavity cannot be visualized on the screen for a brief time, which may increase the risk of trauma or mispositioning and reduces physician control of the field.9 Despite these limitations, VL is the standard of care for the highest first-pass success of EAM for both routine and abnormal laryngoscopy procedures.55
Video laryngoscopes offer the best success rate for difficult airways, but they are limited by their reliance on expensive video equipment, simultaneous manipulation of multiple tools for the physician, and the loss of 2D perception. Importantly, there are no well-defined approaches for treating a difficult airway, and further investigation should be done to fill this gap in standard airway management. The financial impact of VL as a standard of treatment has not been thoroughly investigated but is crucial to consider for the wide distribution of an airway management device.
Bougies and EGDs Can Establish Airways with Higher Complications
When the vocal cords cannot be visualized, or first-pass laryngoscopy fails, the next step to establish an airway is by using a Bougie. A bougie is a narrow, flexible tube that is inserted into the trachea, often with assistance from a Mac Blade or similar device to suppress the tongue. Bougie insertion into the trachea without visualization is confirmed by feeling the bougie against the tracheal “clicks”, or ridges. An ETT is then passed over the bougie for intubation. The small size of the bougie permits better manipulation and allows for blind intubation (without a direct or indirect view of the airway). Additionally, the bougie can be coupled with VL or DL as a more flexible, successful alternative to a traditional ETT-only approach.45 The bougie can easily be rotated as well to accommodate differential airways. Bougies have significantly higher first-pass success rates in emergency settings than traditional ETT laryngoscope insertions across all EAM indications.46 Parotto et al review reported a 96% bougie first-pass success rate compared to 82% for DL in difficult-airway patients in the ED.10 One meta-analysis found that the Bougie intubation has an overall 98% first-pass success rate compared to both DL and VL, with rates of 86% and 92%, respectively.10 Thus, a bougie may be statistically considered as the preferred option for first pass approach. Regarding limitations, bougies do present the risk of airway perforation and tissue damage. They also may lack shape retention, have insufficient tip pressure forces, and exhibit difficult steerability due to flexibility.45
When intubation fails or a patient has a difficult airway, extraglottic devices (EGDs) are used as rescue devices for oxygenation and/or ventilation until an airway can be achieved. The goal of an EGD is to provide temporary oxygenation, allow for gastric decompression, and to facilitate tracheal intubation.47 EGDs may be either supraglottic masks, which remain above the larynx, or retroglottic tubes, extending down to the upper esophagus. The most common EGD is a supraglottic laryngeal mask airway. An LMA is a mask surrounded by an inflatable cuff, attached to the end of a stiff airway tube, along with an inflation line.47,48 The patient is prepared in the same way as for traditional laryngoscope intubation, and once inserted, the LMA device cuff is inflated.
The traditional LMA comes in a wide variety of sizes to accommodate different airway sizes and ETT size needs. LMAs allow for blind intubation and may have conduits that permit for ETT placement after a successful seal has been formed.46 Additional LMA devices include LMA Fastrach, which facilitates intubation directly and is the most widely used LMA.48 Air-Q is another LMA designed for blind intubation, requires less inflation for a proper seal, accommodates intubation with standard ETT designs, and can be removed with greater injury-free success rates than LMA Fastrach.40,48 Another type of EGD is the i-Gel. Compared to traditional LMAs, the i-Gel has improved seals, includes an added tube for access to the esophagus and stomach, and has a bite block.49 I-Gel is noninflatable and has a wider tube for intubation. It has been reported to have high success rates in difficult airway management relative to other EGDs, with about a 93% first-pass attempt success rate and a reported 100% second-pass success rate.46,49 LMAs and other EGDs are limited in use, however, as they cannot be used for patients with spontaneous respirations, severe facial trauma, restricted or distorted airways, obstructions, or stiff neck or lungs. Additionally, they are not a viable option for patients with a gag reflex or threatened airway, such as with bleeding or vomiting. LMA insertion has complications including dysphagia, bronchospasm, and laryngeal and hypoglossal nerve injury. Additionally, EGDs have high failure rates in obese patients and with inexperienced physicians.1,55
Surgical Airway Management Serves as a Last Resort in the Emergency Room
When all first pass attempts at intubation have failed, when there are absolute contraindications to the aforementioned EAM solutions, or when it is necessary to establish a definitive airway, physicians will use a surgical approach. Surgical airways are required when there is an obstruction superior to the trachea, anaphylactic swelling, or severe facial trauma.51 There are two main approaches to surgical intubation: cricothyroidotomy or transtracheal needle ventilation. Rescue surgical airway management is required for < 0.5% of all ED intubation patients.51 In a cricothyroidotomy, a vertical incision is made in the neck midline, then a horizontal incision to expose the trachea, after which a bougie is inserted through the incision, inflated, and an ETT is inserted.40 Cricothyroidotomy limits the risk of esophageal placement and is an efficient solution for experienced physicians, but presents the risk of bleeding, vocal cord or airway damage, and perforation of other internal membranes by the blade. Needle ventilation is the preferred method of surgical airway management in children. During the procedure, a needle pierces the airway, a catheter is inserted over the needle, and the ETT is then inserted over the catheter. Needle ventilation is less invasive than cricothyroidotomy, but presents the risk of infection, hemorrhage, and perforation of the posterior trachea.40
Recent Advances in Artificial Intelligence Offer Promising Alternatives to Existing Solutions
In recent years, advancements in artificial intelligence (AI) and computer-assisted procedures have augmented the current techniques in laryngoscopy. Machine learning algorithms combined with VL can identify the location of the glottis to provide real-time feedback to providers.56 AI algorithms may also be used to visualize anatomical landmarks for intubation and label these structures on the video image.57 In 2021, Hayasaka et al published an AI model that can predict a difficult airway with 86% accuracy based on facial images, which may assist faster intubations in emergency cases or with inexperienced physicians.58 Other models use sex, BMI, weight, height, and age to predict difficult airways with >90% accuracy in preoperative care.59 Additional deep-learning models can use 3D CT scans to predict mortality and intubation rates in COVID-19 patients.60 However, the existing field of AI-informed intubation is largely limited to surgery, anesthesiology, and educational tools. There is great potential to use AI tools for predicting difficult airways and guiding intubations in the emergency setting, but existing research is insufficient to be included in the scope of this review. We propose artificial intelligence as a field with large potential to expand the field of emergency airway management among new innovators.
Analysis of Existing Solutions Reveals Opportunities for Innovation
Because proper airway management is essential for patient survival, and because intubation is a common procedure in hospital settings, many devices have emerged on the market. Surveying the market landscape was initiated by considering the total airway management market, rather than limiting it to the subsector of devices intended for difficult airways. Many devices used for difficult airways overlap with devices used for typical airways, so limiting the landscape early on could cause the innovator to overlook existing, pertinent technology. This analysis encompasses devices directly used for securing an airway, such as the endotracheal tube, and adjunct devices, such as the laryngoscope.
Efficacy Comparison Reveals a Gap in Technologies That Address Differential Airways
Solutions should address the clinical need while maintaining a cost within the range of relevant stakeholders’ willingness to pay. The first approach to surveying the market landscape considered current device performance and ease-of-use, as indicated by a qualitative estimation of efficacy, in comparison to the cost for various devices in each subtype.
The gaps identified in the preliminary efficacy versus cost analysis are very high efficacy with meager purchasing cost (less than $10) or low efficacy with high cost (Figure 1A).50,52,61–67 Very high efficacy with such cost constraints would severely limit innovation, and a device with low efficacy and high cost would never get adapted into clinical practice. Important takeaways from the first iteration of the market landscape assessment are that the acceptable upper bound of cost for airway management devices is approximately $5k, with median costs ranging between $20-$100.50,67 Adjunct devices typically have higher list prices than direct devices. Because endotracheal tubes are used in conjunction with laryngoscopes, if a developed solution does not necessitate the use of an adjunct device, the cost of the device can be higher. However, whereas direct solutions are disposable, adjunct devices are typically reusable, and thus the cost per use would be much lower for laryngoscopes than initial purchasing. The initial dimension of the market landscaping has provided insight into the target cost and upper-bound cost constraints of the final solution while meriting further analysis.
 |
Figure 1 (A) Market landscape analysis comparing cost and efficacy of current solutions. Qualitative efficacy was determined from a combination of reported physician importance, intubation success rates for no more than three attempts, and efficacy reports from peer-reviewed journals. Costs were determined using medical device purchasing platforms and clinical reports. Data from these studies.50,52,61–67 (B) Market landscape analysis comparing first-attempt success rate and cost. Note that the data used to populate first-pass success rate has studies pertaining to typical airway management as the upper bounds, and difficult airways as the lower bounds, when applicable. Data from these studies.68–76 (C) Market landscape analysis comparing time for intubation and cost. Note that times may overlap for adjunct devices and respective devices whose insertion they assist. **Indicates device with learning curve in medical trainees as indicated by literature. Data from these studies.71–74,76–79,80 Abbreviations: OPA, oropharyngeal airway; NPA, nasopharyngeal airway. |
There exists a major gap in the market for devices accommodating differential airway geometries.8,10,63 Airway physiologies can differ based on the stage of development (child versus adult), body weight (obesity), different lengths of the trachea, or different positions of the trachea (anterior). Most existing solutions are standardized for both intubation protocol and for airway geometries, but many patients have deviations in their physiology that do not accommodate standard approaches. Therefore, the more solutions that exist for niche populations, such as children or obese patients, then the more prepared physicians can be to accommodate different needs in the fastest way possible. The prioritization of first-pass success rates and minimal time for effective intubation should drive future research for designs that cater to niche airway geometries.
Cost Comparison Reveals Need for Improvement in Limited Resource Settings
It is critical to consider the cost of existing devices to address the issue of standardized care across various clinical settings with limited resources, in addition to the consideration of stakeholders. If a novel device for airway management is to become the standard approach for any of the current market gaps, then it must be widely available. Thus, the cost must be considered. The cost of airway management devices ranges from $5–20 for a bougie up to $15,000 for a video laryngoscope alone, so the financial impact of intubation is varied and can be significant.40 As previously cited, the distribution of laryngoscopes is largely limited by the cost of video laryngoscopes, which thus reduces access to the standard of care for difficult airways and creates a disparity in care for patients with difficult airways. 69% of EDs without VL attributed this deficiency to the cost of VL implementation.54 This deficit worsens in low-resource areas internationally, with just a quarter of emergency centers in areas such as the Western Cape of South Africa having any VLs.81 With market analysis indicating that VLs cost between $500–15,000, price point is a logical deterrent for purchase. Developing a technology to assist airway management has substantial opportunity for translation due to two key-value signposts of medical innovation: the potential to decrease cost and improve clinical outcomes.
Low-Cost Options Have a Higher Training Burden
One major gap in current approaches to airway management devices is the analysis of the learning curve for efficient application. For example, video laryngoscopes often have lower first-pass success rates than DL among physicians in training due to the requirement for manipulation of multiple tools, loss of depth perception, and the lack of VL standardization in clinical settings.1,19,36 One study reports a direct correlation between post-graduate residency years and intubation success, with post-graduate year 1 residents reporting up to 20% first pass failures.66 Another analysis compared crude number of intubation attempts, rather than experience longevity, to intubation success rates among medical students and anesthesiologists. This study identified a direct correlation between the number of intubation and first-pass success rates in emergency intubations.82 Additionally, less experience in providers is also linked to longer times for intubation, use of incorrect instruments or faulty techniques, and greater first-pass failures in difficult airways.82 Regarding difficult airways, first-pass success rate shows a significant decrease with increasing Mallampati scores or Cormack-Lehane grading, indicating more difficult airways.82,83 Thus, devices that aim to improve intubation success for difficult airways can also address some of the burdens associated with less trained clinicians.
While it is logical that experience should improve a provider’s performance, the high risk associated with failures for emergency intubations highlights an important potential for innovation to steepen the learning curve for EAM. Video laryngoscopes are associated with higher first-pass success rates and shorter intubation times in less trained physicians, relative to direct laryngoscopes. Thus, VL may be an important consideration into innovations to address gaps with provider experience.84 Additionally, it is important that future innovations both establish a standard protocol for their application and consider the skills of unpracticed physicians to generate the most effective device. Given the issue with training required for effective solutions, an opportunity for innovation lies in the expertise required versus time for successful insertion comparison. Less time required for intubation is associated with better patient outcomes, making this gap a crucial consideration for future research.
High First-Pass Success, Low-Cost Devices Have Largest Potential Market
The first approach to surveying the market landscape considered current device performance and ease-of-use, as indicated by a qualitative estimation of efficacy, in comparison to the cost for various devices in each subtype (Figure 1A).50,52,61–67 Because only a limited gap in the market was found in comparing efficacy to cost, two other dimensions affecting clinical outcome were selected: the rate of first-pass success and the time for intubation when using the device (Figure 1B and 1C, respectively). It was identified that first-attempt success rate is the primary factor affecting intervention costs, likelihood of failed airway management, and overall clinical outcomes (Figure 1B).68–76 Therefore, it is a standard indicator of device performance. It can be ascertained that a gap exists for devices with a high first-pass success rate (exceeding 80%), that also costs between $4 - $100 (Figure 1C).71–80
The LMA, as previously stated, has been integrated into the current approach of managing difficult airways. While the LMA falls under similar parameters as the identified gap (albeit with a slightly higher cost range), an important consideration not analyzed in this landscape is the time duration in which the device can be deployed. A primary reason endotracheal tubes remain the gold standard for intubation is that LMAs have a recommended use time of approximately thirty minutes, with an upper limit of three hours85 Therefore, LMAs should only be considered first-line devices if major surgery is not anticipated. While not a key performance indicator, any novel technology should have the capacity to maintain the airway during major procedures and not need to be replaced by an endotracheal tube. With this additional metric, the market gap can be broadened to include devices costing several hundred dollars at efficacy surpassing 80%.
Innovator Challenges Include a Need for Market Disruption and Willingness to Pay
Important to note when surveying a market is how many competitors exist. At least 75 companies manufacture products for airway management, including Medtronic Plc, Teleflex Inc, Avanos Medical Inc, Indian Ocean Medical Inc, Becton, Dickinson & Co, Trudell Medical International, Ambu, Well Lead, Armstrong Medical, Flexicare Medical, ConvaTec, Asid BonzM Guangzhou Orcl Medical, Smiths Medical, and others. Medtronic Plc, one of the largest medical device companies globally, also dominates the airway management market.69 Combined with information about the number of active patents, from a competition standpoint, the market is crowded (Figure 2).86 Therefore, any new technology developed must be disruptive. The competitive advantage for such a device must lie in incorporating novel technology rather than merely a combination of existing technologies. Solutions without this disruptive nature will likely be superseded by other advancements or see a poor rate of adoption into clinical practice.
 |
Figure 2 Airway management device patents. Only the devices indicated with an asterisk can maintain the airway independently and are thus referred to as direct devices in this report. The remainder of the devices are either adjuncts, meaning they are assistive devices for insertion, or they are unable to both maintain patency and allow for oxygenation and are used in the pre-hospital setting or before intubation. To probe the number of devices manufactured in each category, the number of active patents was ascertained. Note that the number of patents will be much greater than the number of FDA-approved devices on the market, but this information is less readily available. Data from Home. Anesthesia Airway Management (AAM). https://aam.ucsf.edu/.86 |
Intubations are performed in a variety of hospital and pre-hospital settings, including EDs, intensive care units, ambulances, and operating rooms. Segmentation of the market, coupled with quantitative analysis of the number of patients belonging to each subpopulation will allow the innovators to decide the target population for the solution. With a focused target, the ability of the device to meet this subsection’s needs can be optimized, which is preferable to substandard performance for the entirety of the population. Market segmentation began with the total number of intubations performed annually. Based on the original proposed clinical need, the initial chosen segments of the market were patients undergoing emergency intubations with difficult airways, and further refined to address variation in the characteristics of difficult airways. The market can also be segmented based on population age, encompassing adult, pediatrics, and neonatal populations.87 Because devices for pediatric and neonatal populations target a smaller niche than devices for adults, accounting for about 0.01% of all ED patients, and the obtainable population needs to be large enough to attract innovators and investors, market segmentation in this report was limited to adults (Figure 3).88
 |
Figure 3 Patient segmentation for airway management. Although difficult airway attributions can be further segmented, unless current technologies fail to meet the needs of a subsection of the population, over-limiting the target population will negatively impact investor opportunity. Target segments of the population are shown in blue. Data from these studies.7,87,89 |
Current data on epidemiological growth is not available for intubations, but older retrospective studies show an annual growth rate of 4.22%.90 Because anterior larynxes are most prevalent in obese and elderly populations, both of which are growing demographics in the United States, current growth rates of intubations, especially as it pertains to difficult intubations, are likely higher.91,92
Because difficult airway characteristics are not uniform, a universal approach in management cannot be utilized. Differences in difficult airway classification and source attribution will affect the success of a solution. When choosing which segments of the difficult airway population to focus on, the size of the demographic is a prime consideration. The largest cause of difficult airways is the anterior positioning of the larynx.87 Therefore, the selected market is adult patients with difficult airways attributed to anterior larynxes requiring intubation in the emergency setting (Figure 3).7,87,92
The estimated global market size for airway management devices is $1.9 billion. Of course, markets are not stagnant, and equally important to the fiscal opportunity is the growth rate. The airway management device market has a compound annual growth rate (CAGR) of 5.8%.69 The United States represents the largest regional market share, accounting for an estimated 32.3% of expenditures. The United States market is growing faster than the global average, with a CAGR of 8.7%.93 Market sizes are on target to remain attractive to investors, with a total addressable market (TAM) exceeding the $1 billion recommendation and a serviceable obtainable market representing less than 1% of the TAM.
As previously discussed, overall willingness to pay for a direct device has been estimated between $20-$100.50,52,61–67 As is commonplace in the medical industry, insurance companies ultimately bear most of these costs, and patients incur a copayment. EDs are responsible for purchasing the equipment and are subject to reimbursement by payers. If over 48k difficult emergency intubations within the target demographic are performed annually, and problems intubating difficult airways increase the cost by $20k, a solution could save the healthcare system up to $960 million.55,87,89 Overall, a combinatorial effect of user requirements, including physicians and students, investors, including private equities and commercial licenses, and innovators define the opportunity for innovation. Thus, we identify the primary opportunities and risks which should be considered among these three parties when approaching the potentially transformative innovations in the intubation healthcare sector (Table 2).94
 |
Table 2 Rational for Innovative Focus, Weighing the Pros and Cons of Key Categories of Decision-Makers to Determine the Product’s Commercial Viability to Validate the Selected Target Market. The Graphic Contains Synthesis from This Market Report, Knowledge Obtained from Previous User Interviews and Zenios et al94 |
Conclusions
Airway management is a critical procedure in emergency settings, enabling providers to secure airway patency to promote patient survival. We have discussed the fundamentals of airway management, particularly endotracheal intubation, the current standard of care and the existing technologies available to providers and have demonstrated a significant potential to innovate in the airway management device market. Specifically, new technology development should focus on not only improving ease of use and compatibility with difficult airways, but especially on maximizing first-pass success rates of intubation. Existing airway management devices either address a niche population or aim to fulfill a generalizable role, meaning the tool accommodates a wide range of patients and contexts. Therefore, identifying a target population could guide innovators toward a clearer, achievable approach. The market analysis demonstrates a sufficient need to develop a technology for difficult airway management to improve clinical outcomes and save the healthcare system substantial avoidable expenditures. Difficult airways are associated with not only decreased clinical outcomes but higher emergency visit expenditures. The average admission cost for visits associated with intubating difficult airways is $20k higher than typical airways, at $33k and $13k, respectively.29,85,95 Thus, while the market is crowded and conventional value gaps do not drive the opportunity, the difficult airway opportunity remains attractive to investors, users, and innovators. We provide a comprehensive review of intubation procedures, existing solutions, and disease states to guide future improvements. We report that cost and personnel training are limiting factors in the widespread implementation of new technologies. We find that addressing specific niches in the field holds greater potential when compared to universal solutions. We motivate the need for innovation in EAM to specifically address difficult airways, with particular interest in anterior larynxes, while considering affordability, ease of use, and market saturations. Improvements should prioritize the standards of minimized intubation time and maximized first-pass success rates while introducing novel means of enhancing patient care.
Abbreviations
AI, artificial intelligence; CAGR, compound annual growth rate; DL, direct laryngoscopy; EAM, emergency airway management; ED, emergency department; EGD, Extraglottic device; ETT, endotracheal tube; IDL, indirect laryngoscopy; LMA, laryngeal airway mask; Mac, Macintosh; NPA, Nasopharyngeal airway; OPA, Oropharyngeal airway; RSI, rapid sequence intubation; SAM, serviceable available market; SOM, serviceable obtainable market; TAM, total addressable market; VL, video laryngoscopy.
Acknowledgments
We would like to thank Dr. Marissa Gray and Dr. Anubhav Tripathi for discussions and input. We would like to thank Dr. Andrew Beck and Dr. Austin Quinn for clinical input and advice. We also thank the Brown University Center for Biomedical Engineering and the Brown Design Workshop for resources and funding.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Doris M. and Norman T. Halpin Prize for Senior Capstone Projects at Brown University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. National Hospital Ambulatory Medical Care Survey. 2018 emergency department summary tables; 2018.
2. Chua MT, Khan FA, Ng WM, et al. Pre- and apnoeic high flow oxygenation for RApid sequence intubation in the emergency department (Pre-AeRATE): study protocol for a multicentre, randomised controlled trial. Trials. 2019;20(1):195. doi:10.1186/s13063-019-3305-8
3. Kim YS, Song J, Lim BG, Lee IO, Won YJ. Different classes of videoscopes and direct laryngoscopes for double-lumen tube intubation in thoracic surgery: a systematic review and network meta-analysis. PLoS One. 2020;15(8):e0238060. doi:10.1371/journal.pone.0238060
4. Kim C, Kang HG, Lim TH, Choi BY, Shin YJ, Choi HJ. What factors affect the success rate of the first attempt at endotracheal intubation in emergency departments? Emerg Med J. 2013;30(11):888–892. doi:10.1136/emermed-2012-201708
5. De Jong A, Molinari N, Pouzeratte Y, et al. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br J Anaesth. 2015;114(2):297–306. doi:10.1093/bja/aeu373
6. Koh W, Kim H, Kim K, Ro YJ, Yang HS. Encountering unexpected difficult airway: relationship with the intubation difficulty scale. Korean J Anesthesiol. 2016;69(3):244–249. doi:10.4097/kjae.2016.69.3.244
7. UpToDate. Management of the difficult airway for general anesthesia in adults; 2023. https://www.uptodate.com/contents/management-of-The-difficult-airway-for-general-anesthesia-in-adults.
8. Pacheco GS, Hurst NB, Patanwala AE, Hypes C, Mosier JM, Sakles JC. First pass success without adverse events is reduced equally with anatomically difficult airways and physiologically difficult airways. West J Emerg Med. 2021;22(2):360–368. doi:10.5811/westjem.2020.10.48887
9. Amornyotin S, Prakanrattana U, Vichitvejpaisal P, Vallisut T, Kunanont N, Permpholprasert L. Comparison of the clinical use of Macintosh and Miller laryngoscopes for orotracheal intubation by second-month nurse students in anesthesiology. Anesthesiol Res Pract. 2010;2010. doi:10.1155/2010/432846
10. Parotto M, Cooper R. Recent advances in laryngoscopy in adults. F1000Res. 2019;8:797. doi:10.12688/f1000research.18544.1
11. Bailey B. Laryngoscopy and laryngoscopes--who’s first?: the forefathers/four fathers of laryngology. Laryngoscope. 1996;106(8):939–943. doi:10.1097/00005537-199608000-00005
12. Burkle CM, Zepeda FA, Bacon DR, Rose SH. A historical perspective on use of the laryngoscope as a tool in anesthesiology. Anesthesiology. 2004;100(4):1003–1006. doi:10.1097/00000542-200404000-00034
13. Henderson J. Airway management in the adult. In: Miller’s Anesthesia. Elsevier; 2010:1573–1610.
14. Unzueta MC, Casas JI, Merten A. Macintosh’s laryngoscope. J Am Soc Anesthesiol. 2005;102(1):242.
15. van Zundert A, Pieters B, Doerges V, Gatt S. Videolaryngoscopy allows a better view of the pharynx and larynx than classic laryngoscopy. Br J Anaesth. 2012;109(6):1014–1015. doi:10.1093/bja/aes418
16. Yong SA, Chaou CH, Yu SR, et al. Video assisted laryngoscope facilitates intubation skill learning in the emergency department. J Acute Med. 2020;10(2):60–69. doi:10.6705/j.jacme.202003_10(2).0002
17. Thaler. Cost comparison of 2 video laryngoscopes in a large academic center. J Clin Outcomes Manag. 2021;28(4). doi:10.12788/jcom.0055
18. Şahiner Y. Indications for endotracheal intubation. Tracheal Intubation; 2018. Available from: https://books.google.com/books?hl=en&lr=&id=HXeQDwAAQBAJ&oi=fnd&pg=PA59&dq=%C5%9Eahiner+Y+Indications+for+Endotracheal+Intubation+IntechOpen+2018&ots=B2UHSZjrl9&sig=KOk838VG4vWW42I9uJ5cWoZ95rg.
19. Jung JY. Airway management of patients with traumatic brain injury/C-spine injury. Korean J Anesthesiol. 2015;68(3):213–219. doi:10.4097/kjae.2015.68.3.213
20. Peterson K, Ginglen JG, Desai NM, Guzman N. Direct laryngoscopy. In: StatPearls. StatPearls Publishing; 2023.
21. Themes UFO. The difficult airway. Anesthesia Key; 2018. Available from: https://aneskey.com/the-difficult-airway-3/.
22. Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the glidescope in difficult airway management: an analysis of 2004 glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:5. doi:10.1097/ALN.0b013e3182023eb7
23. Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020;132(6):1317–1332. doi:10.1097/ALN.0000000000003296
24. Di Domenico SL, Coen D, Bergamaschi M, et al. Clinical characteristics and respiratory support of 310 COVID-19 patients, diagnosed at the emergency room: a single-center retrospective study. Intern Emerg Med. 2021;16(4):1051–1060. doi:10.1007/s11739-020-02548-0
25. Baek MS, Han M, Huh JW, Lim CM, Koh Y, Hong SB. Video laryngoscopy versus direct laryngoscopy for first-attempt tracheal intubation in the general ward. Ann Intensive Care. 2018;8(1):83. doi:10.1186/s13613-018-0428-0
26. Prokakis C, Koletsis EN, Dedeilias P, Fligou F, Filos K, Dougenis D. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J Cardiothorac Surg. 2014;9:117. doi:10.1186/1749-8090-9-117
27. Yu JE, Lin RY. The epidemiology of anaphylaxis. Clin Rev Allergy Immunol. 2018;54(3):366–374. doi:10.1007/s12016-015-8503-x
28. Reed MJ, Dunn MJG, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22(2):99–102. doi:10.1136/emj.2003.008771
29. Behrendt CE. Acute respiratory failure in the United States: incidence and 31-day survival. Chest. 2000;118(4):1100–1105. doi:10.1378/chest.118.4.1100
30. Jain S, Iverson LM. Glasgow Coma Scale. StatPearls Publishing; 2022.
31. Adnet F, Borron SW, Finot MA, Lapandry C, Baud FJ. Intubation difficulty in poisoned patients: association with initial Glasgow Coma scale score. Acad Emerg Med. 1998;5(2):123–127. doi:10.1111/j.1553-2712.1998.tb02596.x
32. Latimer AJ, Harrington B, Counts CR, et al. Routine use of a bougie improves first-attempt intubation success in the out-of-hospital setting. Ann Emerg Med. 2021;77(3):296–304. doi:10.1016/j.annemergmed.2020.10.016
33. Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99(2):607–613. doi:10.1213/01.ANE.0000122825.04923.15
34. Saracoglu KT, Yilmaz M, Turan AZ, et al. Evaluation of rescue techniques following failed laryngoscopy: a multicenter prospective observational study. North Clin Istanb. 2023;10(2):212–221. doi:10.14744/nci.2021.76402
35. Kj DP, Shekar B. Adverse events in failed first-pass intubation vs. Successful first-pass intubation in the emergency department - an analytical hospital-based study. J Evid Based Med Healthc. 2021;8(06):283–287. doi:10.18410/jebmh/2021/55
36. Arino JJ, Velasco JM, Gasco C, Lopez-Timoneda F. Straight blades improve visualization of the larynx while curved blades increase ease of intubation: a comparison of the Macintosh, Miller, McCoy, Belscope and Lee-Fiberview blades. Can J Anaesth. 2003;50(5):501–506. doi:10.1007/BF03021064
37. Collins SR. Direct and Indirect Laryngoscopy: equipment and TechniquesDiscussion. Respir Care. 2014;59(6):850–864. doi:10.4187/respcare.03033
38. Wojewodzka-Zelezniakowicz M, Madziala A, Madziala M. Comparison of the Miller and Macintosh laryngoscopes in simulated pediatric trauma patient: a pilot study. Disaster Emerg Med J. 2017;2. doi:10.5603/DEMJ.2017.0001
39. Gawlowski P, Smereka J, Madziala M, Szarpak L, Frass M, Robak O. Comparison of the Macintosh laryngoscope and blind intubation via the iGEL for intubation with C-spine immobilization: a randomized, crossover, manikin trial. Am J Emerg Med. 2017;35(3):484–487. doi:10.1016/j.ajem.2016.11.064
40. Goto T, Goto Y, Hagiwara Y, Okamoto H, Watase H, Hasegawa K. Advancing emergency airway management practice and research. Acute Med Surg. 2019;6(4):336–351. doi:10.1002/ams2.428
41. Berkow LC, Morey TE, Urdaneta F. The Technology of Video Laryngoscopy. Anesth Analg. 2018;126(5):1527. doi:10.1213/ANE.0000000000002490
42. Airtraq. Airtraq; 2016. Available from: https://www.airtraq.com/.
43. GlideScope medical devices. Available from: https://www.verathon.com/glidescope/.
44. Breedon P, Siena F, Armstrong J. Tracheal intubation: improving first pass success with smart material solutions. J Healthc Des. 2017;2(3):15–18.
45. UpToDate. Extraglottic devices for emergency airway management in adults. Available from: https://www.uptodate.com/contents/extraglottic-devices-for-emergency-airway-management-in-adults.
46. Das B, Mitra S, Jamil SN, Varshney RK. Comparison of three supraglottic devices in anesthetised paralyzed children undergoing elective surgery. Saudi J Anaesth. 2012;6(3):224–228. doi:10.4103/1658-354X.101212
47. Cost of unplanned tracheal intubation: evidence from the premier hospital database. Available from: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm?year=2015&index=14&absnum=4676.
48. Ostermayer DG, Gausche-Hill M. Supraglottic airways: the history and current state of prehospital airway adjuncts. Prehosp Emerg Care. 2014;18(1):106–115. doi:10.3109/10903127.2013.825351
49. Das B, Mitra S, Samanta A, Vijay BS. Comparison of i-gelTM supraglottic device with classic laryngeal mask airway in anesthetized paralyzed children undergoing elective surgery. Anesth Essays Res. 2012;6(2):180–183. doi:10.4103/0259-1162.108305
50. Pournajafian A, Alimian M, Rokhtabnak F, Ghodraty M, Mojri M. Success rate of airway devices insertion: laryngeal mask airway versus supraglottic gel device. Anesth Pain Med. 2015;5(2):e22068. doi:10.5812/aapm.22068
51. Offenbacher J, Nikolla DA, Carlson JN, et al. Incidence of rescue surgical airways after attempted orotracheal intubation in the emergency department: a National Emergency Airway Registry (NEAR) study. Am J Emerg Med. 2023;68:22–27. doi:10.1016/j.ajem.2023.02.020
52. Heymans F, Feigl G, Graber S, Courvoisier DS, Weber KM, Dulguerov P. Emergency cricothyrotomy performed by surgical airway–naive medical personnel: a randomized crossover study in cadavers comparing 3 commonly used techniques. Obstet Anesth Dig. 2017;37(2):79. doi:10.1097/01.aoa.0000515750.60577.e7
53. Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003;98(1):23–27. doi:10.1097/00000542-200301000-00007
54. Raja AS, Sullivan AF, Pallin DJ, Bohan JS, Camargo CA
55. Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. 2022;136(1):31–81. doi:10.1097/ALN.0000000000004002
56. Carlson JN, Das S, De la Torre F, et al. A novel artificial intelligence system for endotracheal intubation. Prehosp Emerg Care. 2016;20(5):667–671. doi:10.3109/10903127.2016.1139220
57. Zang Q, Cui H, Guo X, Lu Y, Zou Z, Liu H. Clinical value of video-assisted single-lumen endotracheal intubation and application of artificial intelligence in it. Am J Transl Res. 2022;14(11):7643–7652.
58. Hayasaka T, Kawano K, Kurihara K, Suzuki H, Nakane M, Kawamae K. Creation of an artificial intelligence model for intubation difficulty classification by deep learning (convolutional neural network) using face images: an observational study. J Intensive Care Med. 2021;9(1):38. doi:10.1186/s40560-021-00551-x
59. Zhou CM, Wang Y, Xue Q, Yang JJ, Zhu Y. Predicting difficult airway intubation in thyroid surgery using multiple machine learning and deep learning algorithms. Front Public Health. 2022;10:937471. doi:10.3389/fpubh.2022.937471
60. Di Napoli A, Tagliente E, Pasquini L, et al. 3D CT-inclusive deep-learning model to predict mortality, ICU admittance, and intubation in COVID-19 patients. J Digit Imaging. 2023;36(2):603–616. doi:10.1007/s10278-022-00734-4
61. Fiala A, Lederer W, Neumayr A, et al. EMT-led laryngeal tube vs. face-mask ventilation during cardiopulmonary resuscitation - A multicenter prospective randomized trial. Scand J Trauma Resusc Emerg Med. 2017;25(1):104. doi:10.1186/s13049-017-0446-1
62. Effective use of oropharyngeal and nasopharyngeal airways. ACLS.com. 2019. Available from: https://acls.com/articles/nasopharyngeal-oropharyngeal-airways/.
63. Narang AT, Oldeg PF, Medzon R, Mahmood AR, Spector JA, Robinett DA. Comparison of intubation success of video laryngoscopy versus direct laryngoscopy in the difficult airway using high-fidelity simulation. Simul Healthc. 2009;4(3):160–165. doi:10.1097/SIH.0b013e318197d2e5
64. Shop our products. Available from: https://mms.mckesson.com/catalog?utm_campaign=mms+inline+links&utm_medium=referral&sort=&utm_source=McKesson.com.
65. MedicalExpo. The B2B marketplace for medical equipment: medical material, medical imagery, hospital furniture, laboratory equipment, etc. Available from: https://www.medicalexpo.com/.
66. Medical supplies and products from top manufacturers for EMS providers - theEMSstore. Available from: https://www.theemsstore.com/.
67. Lascarrou JB, Boisrame-Helms J, Bailly A, et al. Video laryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients: a randomized clinical trial. JAMA. 2017;317(5):483–493. doi:10.1001/jama.2016.20603
68. Nicholson A, Cook TM, Smith AF, Lewis SR, Reed SS. Supraglottic airway devices versus tracheal intubation for airway management during general anaesthesia in obese patients. Cochrane Database Syst Rev. 2013. doi:10.1002/14651858.CD010105.pub2
69. Endotracheal tube market size, share & trends analysis report by product type (regular, reinforced), by route type (orotracheal, nasotracheal), by application, by end-user, by region, and segment forecasts, 2023–2030. Available from: https://www.grandviewresearch.com/industry-analysis/endotracheal-tubes-market.
70. Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci. 2014;4(1):65–70. doi:10.4103/2229-5151.128015
71. Schober P, Biesheuvel T, de Leeuw MA, Loer SA, Schwarte LA. Prehospital cricothyrotomies in a helicopter emergency medical service: analysis of 19,382 dispatches. BMC Emerg Med. 2019;19(1):12. doi:10.1186/s12873-019-0230-9
72. Driver BE, Prekker ME, Klein LR, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA. 2018;319(21):2179–2189. doi:10.1001/jama.2018.6496
73. de Alencar JCG, Marques B, Marchini JFM, et al. First-attempt intubation success and complications in patients with COVID-19 undergoing emergency intubation. J Am Coll Emerg Phys Open. 2020;1(5):699–705. doi:10.1002/emp2.12219
74. Eric M, Rottenberg AAS. Increasing intubation first-attempt success rates in patients of all ages. EMS Airway. 2020. Available from: https://emsairway.com/2020/09/29/increasing-intubation-first-attempt-success-rates-in-patients-of-all-ages/.
75. Joshi R, Hypes CD, Greenberg J, et al. Difficult airway characteristics associated with first-attempt failure at intubation using video laryngoscopy in the intensive care unit. Ann Am Thorac Soc. 2017;14(3):368–375. doi:10.1513/AnnalsATS.201606-472OC
76. von Goedecke A, Bowden K, Wenzel V, Keller C, Gabrielli A. Effects of decreasing inspiratory times during simulated bag-valve-mask ventilation. Resuscitation. 2005;64(3):321–325. doi:10.1016/j.resuscitation.2004.09.003
77. Ahmed SM, Doley K, Athar M, Raza N, Siddiqi OA, Ali S. Comparison of endotracheal intubation time in neutral position between C-Mac® and Airtraq® laryngoscopes: a prospective randomised study. Indian J Anaesth. 2017;61(4):338–343. doi:10.4103/ija.IJA_564_16
78. Castle N, Owen R, Hann M, Naidoo R, Reeves D. Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Emerg Med J. 2010;27(11):860–863. doi:10.1136/emj.2009.084343
79. Eglen M, Kuvaki B, Günenç F, et al. Comparação de três técnicas diferentes de inserção com a máscara laríngea LMA‐Unique™ em adultos: resultados de um estudo randômico [Comparison of three different insertion techniques with LMA-UniqueTM in adults: results of a randomized trial]. Rev Bras Anestesiol. 2017;67(5):521–526. French. doi:10.1016/j.bjan.2017.04.007
80. Huang TY, Lin JR, Chung YT. A preinstalled nasopharyngeal airway in the right nasal passageway to facilitate nasogastric intubation in anesthetized and intubated patients: a prospective randomized controlled trial. BMC Gastroenterol. 2020;20(1):365. doi:10.1186/s12876-020-01514-6
81. Jooste WJL, van Hoving DJ. The availability of alternative devices for the management of the difficult airway in public emergency centres in the Western Cape. Afr J Emerg Med. 2015;5(1):19–23. doi:10.1016/j.afjem.2014.11.001
82. Chao A, Chou WH, Huang HH, Yeh YC, Lin CJ. Evaluation of tracheal intubation: a retrospective study of skill acquisition by medical students in the operating theater. J Formos Med Assoc. 2015;114(9):855–859. doi:10.1016/j.jfma.2013.07.019
83. Singhal SK, Kaur K, Yadav P. A study to evaluate the role of experience in acquisition of the skill of orotracheal intubation in adults. J Anaesthesiol Clin Pharmacol. 2021;37(3):469–474. doi:10.4103/joacp.JOACP_133_19
84. Woollard M, Mannion W, Lighton D, et al. Use of the Airtraq laryngoscope in a model of difficult intubation by prehospital providers not previously trained in laryngoscopy. Anaesthesia. 2007;62(10):1061–1065. doi:10.1111/j.1365-2044.2007.05215.x
85. Moucharite MA, Zhang J, Giffin R. Factors and economic outcomes associated with documented difficult intubation in the United States. Clinicoecon Outcomes Res. 2021;13:227–239. doi:10.2147/CEOR.S304037
86. Anesthesia Airway Management (AAM). Home. Available from: https://aam.ucsf.edu/.
87. Wong E, Ng YY. The difficult airway in the emergency department. Int J Emerg Med. 2008;1(2):107–111. doi:10.1007/s12245-008-0030-6
88. Long E, Sabato S, Babl FE. Endotracheal intubation in the pediatric emergency department. Paediatr Anaesth. 2014;24(12):1204–1211. doi:10.1111/pan.12490
89. Turner JS, Bucca AW, Propst SL, et al. Association of checklist use in endotracheal intubation with clinically important outcomes: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(7):e209278. doi:10.1001/jamanetworkopen.2020.9278
90. Pfuntner A, Wier LM, Stocks C. Most frequent procedures performed in U.S. hospitals, 2011. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2013.
91. Waite LJ. The demographic faces of the elderly. Popul Dev Rev. 2004;30(Supplement):3–16.
92. Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34(4):717–732. doi:10.1016/j.psc.2011.08.005
93. Global Industry Analysts, Inc. Global airway management devices market to reach $1.8 billion by 2024. PR Newswire; 2021. Available from: https://www.prnewswire.com/news-releases/global-airway-management-devices-market-to-reach-1-8-billion-by-2024--301350115.html.
94. Zenios S, Makower J, Yock P. Biodesign: The Process of Innovating Medical Technologies. Cambridge University Press; 2010.
95. Phillips K, Moucharite M, Wong T, May R. Cost burden associated with difficult intubation in the United States. Trends Anaesth Crit Care. 2020;30:e131. doi:10.1016/j.tacc.2019.12.320
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
