Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Emollient formulations containing antiseptics reduce effectively the level of Staphylococcus aureus on skin
Authors Spada F , Barnes TM, Greive KA
Received 8 May 2019
Accepted for publication 23 August 2019
Published 4 September 2019 Volume 2019:12 Pages 639—645
DOI https://doi.org/10.2147/CCID.S215023
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jeffrey Weinberg
Video abstract presented by Fabrizio Spada.
Views: 6436
Fabrizio Spada, Tanya M Barnes, Kerryn A Greive
Research & Development, Ego Pharmaceuticals, Braeside, Victoria, Australia
Correspondence: Fabrizio Spada
Ego Pharmaceuticals Pty Ltd, 21-31 Malcolm Road, Braeside, Victoria 3195, Australia
Tel +61 39 586 8874
Fax +61 39 580 7647
Email [email protected]
Background: Increased skin colonization by Staphylococcus aureus is associated with atopic eczema (AE) severity. Reduction of S. aureus levels on the skin results in an improvement in the clinical condition.
Methods: The antimicrobial activity of topical products including a bath oil, cream, and wash combining antiseptics and emollients (A+E) was compared to products containing emollients only. The preference of patients with AE for A+E cream or emollient only cream to relieve symptoms of itching, erythema, and inflammation when applied three times daily for 10 days is evaluated. Repeat insult patch testing of the products is also conducted.
Results: A significant reduction in microbial counts was found following use of A+E bath oil (4.09±0.32 vs 6.20±0.24 log10 cfu/mL S. aureus, P<0.001), A+E cream (5.50±0.63 vs 5.94±0.72 log10 cfu/foot S. aureus, P=0.002), and A+E wash (2.71±0.48 vs 3.57±0.31 log10 cfu/mL Escherichia coli, P<0.001) compared to the emollient only products. The A+E cream was preferred to the emollient only cream (P=0.004) by patients with AE. All three tested formulations were found to be non-irritating and non-sensitizing to the skin.
Conclusion: The bath oil, cream, and wash containing antiseptics and emollients decrease the level of bacteria on the skin, including S. aureus, compared to emollient only products. Patients with AE preferred the A+E cream compared to the emollient only cream to relieve symptoms of itching, erythema, and inflammation. The choice of formulation allows clinicians and patients to choose a suitable product for the short-term treatment of eczema flare-ups caused by bacterial infections.
Keywords: Staphylococcus aureus, atopic eczema, atopic dermatitis, benzalkonium chloride, triclosan, antimicrobial, antiseptic, emollient
Introduction
Among patients with atopic eczema (AE), Staphylococcus aureus is typically found in approximately 90% of the clinically involved skin areas, most without clinical signs of infection.1,2 In contrast, only 5–30% of healthy individuals harbor S. aureus on their skin.3 S. aureus adheres to the skin of patients with AE by means of receptors for dermal fibronectin and fibrinogen, which are exposed in damaged atopic skin compared to normal skin.4 Atopic skin is further susceptible to increased S. aureus colonization due to a decrease in endogenous antimicrobial peptides, which may result in defective innate immune responses.5
The density of S. aureus on eczematous lesions correlates with cutaneous inflammation and contributes to eczema severity.6 Increased severity may be due to a direct chemical irritation of protein components of the bacterium with immune cells.7 Further, S. aureus secretes a group of toxins (superantigens) which can stimulate T lymphocytes distant from the eczematous site, leading to widespread activation of existing lesions.8 Correlation has been shown between the presence of superantigens and the severity of AE.8 A reduction in S. aureus levels on eczematous skin is accompanied by a significant improvement in the clinical condition.9,10 Consequently, antimicrobial therapy may be an important treatment component in the management of AE.
Topical antiseptics represent an alternative to topical antibiotics to reduce S. aureus levels in patients with AE.11 The main advantages of antiseptics over antibiotics are that they have a low potential of inducing bacterial resistance and rarely cause hypersensitivity.11,12 In addition, it is well established that topical use of emollients improves inflammatory skin diseases, particularly if the skin is dry and pruritic.13 Moreover, concomitant use of emollients with corticosteroids can allow steroids to be used less frequently or in smaller quantities.14,15 The combination of antiseptics and emollients would, therefore, offer a dual action in treating AE flare-ups due to bacterial infection.
The aim of this study was to test the antimicrobial activity of a range of topical products comprising a bath oil, cream, and wash formulated to combine antiseptics and emollients (A+E) compared to products containing emollients (E) only. In addition, the preference of patients with AE for the A+E cream or the E only cream to relieve symptoms of itching, erythema, and inflammation is evaluated. Repeat insult patch testing (RIPT) of the products is also conducted.
Materials and methods
Topical preparations
QV Flare Up Bath Oil AUST R 142064 (referred to as A+E bath oil) containing benzalkonium chloride 2.0% (w/w), triclosan 0.7% (w/w), and paraffin liquidum base; QV Flare Up Cream AUST L 165214 (A+E cream) containing glycerol 10% (w/w), and benzalkonium chloride 0.1% (w/w); QV Flare Up Wash ARTG 167618 (A+E wash) containing glycerin, myrtrimonium bromide 2% (w/w), and benzalkonium chloride 4% (w/w); QV Bath Oil (referred to as E only bath oil) containing paraffinum liquidum; QV cream (E only cream) containing paraffinum liquidum, glycerin, and petrolatum. All preparations were from Ego Pharmaceuticals, Pty. Ltd. (Braeside, VIC, Australia).
Study participants
The microbial studies involving healthy volunteers were approved by the Independent Ethics Committees of Microtech Laboratories, Pty Ltd. (Blackburn, VIC, Australia) and Silliker Microtech, Pty. Ltd. (Blackburn, VIC, Australia). The microbial study involving patients with AE was approved by the Independent Ethics Committee of Dermatest, Pty. Ltd. (Rockdale, NSW, Australia). The RIPT studies involving healthy volunteers were approved by the Institutional Review Boards of Cantor Research Laboratories, Inc. (Blauvelt, NY, USA) and AMA Laboratories, Inc (New City, NY, USA). All operate in accordance with the International Conference on Harmonization Good Clinical Practice guidelines. All participants provided written informed consent, in accordance with the Declaration of Helsinki.
Eligible participants for the microbial and RIPT studies included healthy men and women aged 18–70 years who: were not taking medication or under the care of a doctor for a period of 1 month prior to commencement and throughout the entire test period; completed an extensive medical history form; were free of any dermatological or systemic disorder that would interfere with the results; were available for the study duration and gave written informed consent. Exclusion criteria were individuals: under doctor’s care; taking medication which could mask or interfere with test results; with a history of sensitivity to cosmetics; with any form of skin cancer or any disease that could interfere with test results; diagnosed with chronic skin allergies; with excessive hair on the test sites and females who indicated that they were pregnant or nursing an infant.
Eligible participants for the AE study included men and women aged 18–65 years diagnosed with AE by a clinician that had previously been treated mainly with topical steroids. All other inclusion and exclusion criteria were the same as described above.
Antimicrobial activity of A+E bath oil
The antimicrobial activity of A+E bath oil was assessed using the Storey patch test. Twelve healthy volunteers (5 female, 7 male) took part in the study. To remove transient flora, hands and forearms were washed with an unpreserved toilet soap for 1 min, rinsed and dried. Three 10 cm2 circles were marked on each inner forearm and 0.3 mL S. aureus MT42 (ATCC 6538) cultured for 24 hrs was applied to each patch, spread evenly, and allowed to dry.
Pre-treatment counts were determined from one patch on each arm by placing a sterile polycarbonate cylinder over the patch and pressing firmly to seal it onto the skin. Recovery broth (10 mL) was added to the cylinder and a sterile cotton swab used to rub the surface of the patch to release the bacteria. A sterile syringe was used to collect the recovery broth containing the bacteria. Recovery broth was plated in duplicate onto mannitol salt agar without salt to minimize any inhibition of stressed cells. Each patch was sampled separately. Plates were incubated at 37°C for 48 hrs and the number of S. aureus counted based on colonial morphology; S. aureus produces deep yellow colonies of uniform color.
Each arm was subsequently soaked in either A+E bath oil (diluted 1:133) or E only bath oil (diluted 1:174 to match the concentration of liquid paraffin in A+E bath oil) in 4 L of 40°C tap water for 10 mins. The arms, but not patches, were dried and residual S. aureus on the patches were recovered by the technique described above. After sampling, arms were wiped with 70% methanol and washed with chlorhexidine to remove any remaining bacteria.
Antimicrobial activity of A+E cream
To assess the antimicrobial activity of A+E cream, the toe webs were used as a model of bacterial colonization and/or secondary bacterial infection with S. aureus.16 Twelve healthy volunteers (5 female, 7 male) were randomly divided into two groups, one group using A+E cream on the right foot and E only cream on the left foot, and vice versa. The cross over study was performed 2 weeks later.
The toe webs were swabbed to determine pre-treatment counts. Swabs were transferred to 4 mL of Nutrient Broth No. 2, vortexed for 1 min and then plated onto cystine-lactose-electrolyte deficient agar in duplicate. Each foot was sampled separately. Plates were incubated at 37°C for 48 hrs and the total microbial load was counted as well as the number of S. aureus based on colonial morphology.
The A+E cream (1.5 g) was gently massaged into the toe webs and surrounding areas of one foot for 5 mins. Similarly, E only cream (1.5 g) was applied to the other foot. To avoid contamination hands were washed between applications. Volunteers replaced their socks and shoes and resumed normal activities between treatment application and sampling. The toe webs were swabbed again after 6 hrs. The swab was transferred to 4 mL of Nutrient Broth with 3% lecithin and 2% Tween 80 and the flora enumerated as described for the pre-treatment counts.
Antimicrobial activity of A+E wash
The antimicrobial activity of A+E wash was assessed using the BS EN 1499:1997 hygienic handwash protocol.17 Fifteen healthy volunteers were randomly divided into two groups, one using A+E wash and the other using linseed oil soft soap. The cross over study was performed 1 week later.
To remove transient flora, hands and forearms were washed with 5 mL of linseed oil soft soap for 1 min, rinsed for 30 s and dried. The hands were subsequently contaminated with Escherichia coli K12 MT316 (NCTC 10,538) grown in tryptone soy broth (TSB) for 24 hrs to the mid-meta carpels for 5 s with the fingers spread apart. Excess culture was allowed to drain from the hands and hands were air dried. Pre-treatment counts were determined by rubbing fingers against the bottom of sterile petri dishes containing 10 mL TSB for 1 min, which was plated onto tryptone soy agar plates in duplicate. Each hand was sampled separately. Plates were incubated at 36°C for 18–24 hrs and counted for E. coli colonies.
Hands were subsequently washed using either 5 mL A+E wash or 5 mL linseed oil soft soap following the standard hand wash procedure for 60 s.17 Hands were rinsed under running tap water for 15 s with fingertips upright. The wrist and lower arms were dried to prevent recontamination of the fingertips. Fingertips were rubbed for 1 min against the base of sterile petri dishes containing 10 mL TSB with 3% Tween, 3% saponin, 0.1% histidine, and 0.1% cysteine and the flora enumerated as described for pre-treatment counts. After sampling, hands were washed with chlorhexidine to remove any remaining bacteria.
Evaluation of A+E cream in patients with AE
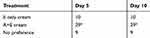
Fifty patients were enrolled in the study. Patients were required to abstain from using deodorants, soaps, cosmetic moisturizers, and other topical preparations on the test areas for a period of 3 days prior to and throughout the study period. Pairs (A and B) of treatment sites where eczema was active and of equivalent size and severity were determined, for example, on opposing legs. Patients were given the E only cream (Product A) and the A+E cream (Product B) and were instructed to apply the products to the two treatment sites, Product A to site A, and so on three times daily for a period of 10 days. Patients were blinded as to the nature of the material being applied. Patients returned to the laboratory after 5 and 10 days to complete a questionnaire and to express an overall preference for one product over the other, giving consideration to the relative degree of relief offered from itching, erythema, and inflammation at each of the two treatment sites. The results were analyzed using the following scoring system: −2 if Product A was preferred on both occasions, +2 if Product B was preferred on both occasions, and 0 if there was no preference or the patient changed his or her preference.
Skin irritancy and sensitization by RIPT
Healthy volunteers aged over 18 years participated in this study according to the RIPT protocol previously described.18 Fifty-five volunteers (41 female, 14 male) received A+E bath oil diluted 1:33, 55 (48 female, 7 male) received A+E cream and 105 (79 female, 26 male) received A+E wash.
Statistical analyses
Statistical analysis was performed using Sigmaplot 14.0 (Systat Software, Inc., San Jose, CA, USA). The Wilcoxon matched pairs signed rank test was used to compare microbial counts and is calculated as the sum of ranks of the negative differences from (log10 pre-treatment) − (log10 post-treatment). Statistical analysis was performed on the combined data only (ie, patch 1+ patch 2 or left limb + right limb). P<0.05 was considered to be statistically significant.
Results
Antimicrobial activity of A+E bath oil
There was a significant reduction in S. aureus counts from 6.77±0.11 to 6.20±0.24 log10 cfu/mL (P<0.001) following treatment with E only bath oil, and an even larger significant reduction in S. aureus counts from 6.77±0.11 to 4.09±0.32 log10 cfu/mL (P<0.001) following treatment with A+E bath oil for 10 mins (Table 1). The A+E bath oil was found to be significantly more effective against S. aureus than E only bath oil (P<0.001).
Antimicrobial activity of A+E cream
There was no difference in total bacterial counts of the toe web following treatment with E only cream for 6 hrs (Table 2). However, there was a significant reduction in total bacterial counts from 6.64±0.60 to 6.13±0.52 log10 cfu/foot (P=0.007) following treatment with A+E cream. The A+E cream was therefore found to be significantly more effective against total bacteria than E only cream (P=0.001).
Similarly, there was no difference in S. aureus counts of the toe web following treatment with E only cream for 6 hrs (Table 3). However, there was a significant reduction in S. aureus counts from 6.08±0.39 to 5.50±0.63 log10 cfu/foot (P=0.024) following treatment with A+E cream. The A+E cream was therefore found to be significantly more effective against S. aureus than E only cream (P=0.002).
Antimicrobial activity of A+E wash
There was a significant reduction in E. coli counts from 6.29±0.20 to 3.57±0.31 log10 cfu/mL (P<0.001) following treatment with linseed oil soap, and an even larger significant reduction in E. coli counts from 6.30±0.28 to 2.71±0.48 log10 cfu/mL (P<0.001) following treatment with A+E wash for 60 s (Table 3). The A+E wash was subsequently found to be significantly more effective against E. coli than linseed oil soap (P<0.001).
Evaluation of A+E cream in patients with AE
Two out of 50 patients did not complete the study due to events unrelated to the study protocol. Table 4 shows the number of patients who expressed an overall preference for one formulation over the other. Significantly more volunteers (29/48) preferred A+E cream compared to E only cream (10/48; P=0.004). None of the patients changed their preference from day 5 to day 10 of the study. No adverse events were reported.
Skin irritancy and sensitization
Fifty-two volunteers completed the study in the A+E bath oil group, 54 in the A+E cream group, and 101 in the A+E wash group. The eight volunteers who did not complete the study withdrew due to reasons unrelated to the study protocol. No erythema, edema, or adverse reactions of any kind were observed during the course of the study. Therefore, when tested under semi-occlusive conditions, A+E bath oil, cream, and wash are all non-irritating and non-sensitizing to the skin.
Discussion
The bath oil, cream, and wash tested in this study containing both antiseptic(s) and emollients can rapidly decrease the level of bacteria on the skin, including S. aureus, compared to an emollient alone. The different formulations offer a choice for both clinicians and patients alike to choose an appropriate and/or preferred treatment; bath oils are effective for treating large body areas, creams can be used to treat localized skin areas, while washes can be used on any part of the body in the shower, bath, or hand basin. All formulations were found to be non-irritating and non-sensitizing to the skin. In addition, A+E cream was found to be preferred to E only cream by patients with AE to relieve symptoms of itching, erythema, and inflammation.
Emollients, such as liquid paraffin and glycerin used in the study, play an important role in the management of AE and other dry skin disorders.13 They soften the skin by forming an occlusive film on the stratum corneum which prevents excessive evaporation of water from the upper skin layers, which helps to counteract skin dryness.18
The antiseptics used in this study, include benzalkonium chloride and triclosan, have been used successfully in medical and cosmetic products since 193519 and 1960,20 respectively. Both have low toxicity and are rarely sensitizing.21,22 Benzalkonium chloride has been shown to cause irritation at high concentrations, but is unlikely to cause irritation at the low concentrations used in this study.23 The main advantages of antiseptics over antibiotics are that they have a low potential of inducing bacterial resistance and rarely cause hypersensitivity.11,12 These attributes are important in light of increasing antibiotic resistance, including methicillin-resistant S. aureus, which not only contributes significantly to the mortality and morbidity of healthy people, but is also a costly public health issue.24 The formulations tested in this study offer a non-antibiotic alternative for the short-term treatment of eczema flare-ups caused by bacterial infections.
There have been a small number of clinical studies investigating the use of topical benzalkonium chloride and/or triclosan in patients with AE, which suggest a benefit from these antiseptics. For example, a significant improvement was found in clinical scores and S. aureus counts in 15 patients with moderate to severe atopic dermatitis with S. aureus present on the skin, who bathed daily for 4 weeks in Oilatum Plus bath oil (emollient plus 6% benzalkonium chloride and 2% triclosan), but not in Oilatum bath oil (emollient only).25 On comparing the two treatments, the changes observed were only significantly different after 2 weeks of therapy as the trial was complicated by poor adherence, with 5/8 patients in the Oilatum group failing to complete the study.25 This did not occur in the Oilatum Plus group, possibly indicating dissatisfaction with the emollient only treatment.25 In a crossover study of Oilatum and Oilatum Plus in 30 children with atopic dermatitis and recurrent infection, two 4 week treatment periods using the same protocol described above were separated by two treatment free weeks.26 There was a significant improvement in total clinical score, signs and symptoms score and area effected in the Oilatum Plus but not in the Oilatum group.26
A significant decrease in SCORAD was found for 60 patients with mild to moderate AE who applied emollient cream containing 1% triclosan compared with emollient only cream twice daily for 14 days.27 Although there was an improved mean reduction in SCORAD after 27 days, this was no longer significant.27 Of note, topical corticosteroid use in the triclosan group was half that of the emollient only group, suggesting a steroid-sparing potential of triclosan.27 In another trial, a mean decrease in SCORAD and bacterial concentration was observed in 46 patients with staphylogenic-triggered atopic dermatitis after 1 and 2 weeks who applied either 2% triclosan cream or a cream containing 0.3% triclosan and 0.34% chlorhexidine dihydrochloride (Lipoderm; regimen not stated).28
In a further trial in 55 patients with atopic dermatitis, the total number of bacteria including S. aureus was significantly reduced after 2 and 4 weeks of treatment with either 2% triclosan or 1% erythromycin applied twice daily.29 Clinical improvement of lesions was closely correlated to the reduction in the number of bacteria. These results support the use of topical antiseptic agents for the treatment of AE, since the development of resistance is unlikely compared to that of antibiotics.29
The use of household bleach baths to decrease skin infections in patients with AE has been suggested.30 However, bleach purchased from supermarkets can vary greatly in its concentration and excipients.31 As bleach ages, the active components decompose and it can lose half its activity by the expiry date.31 Consequently, depending on the size of the bath, the final concentration of sodium hypochlorite will vary and as a result may cause burns and irritation from adding too much, or be ineffective from adding too little.31 Furthermore, sodium hypochlorite has been reported to cause contact dermatitis.31
In conclusion, the formulations tested in this study containing both emollients and antiseptics can decrease the level of bacteria on the skin, including S. aureus, and offer an alternative treatment to antibiotics. The dual action of the combination of emollients and antiseptics was preferred by patients with AE compared to emollients only to relieve symptoms of itching, erythema, and inflammation. The choice of formulation allows both clinicians and patients alike to choose an appropriate and/or preferred option for the short-term treatment of infected eczema flare-ups.
Acknowledgment
The authors wish to thank AMA Laboratories, Inc., Cantor Research Laboratories, Inc., Dermatest, Pty. Ltd., Microtech Laboratories, Pty. Ltd. and Silliker Microtech, Pty. Ltd. for their help performing these studies.
Disclosure
Fabrizio Spada, Tanya M Barnes and Kerryn A Greive are, or at the time of the research were employed by Ego Pharmaceuticals, the sponsor of the study and manufacturer of the QV Flare Up product range. The authors report no other conflicts of interest in this work.
References
1. Leyden JJ, Marples RR, Kligman AM. Staphylococcus aureus in the lesions of atopic dermatitis. Br J Dermatol. 1974;90(5):525–530. doi:10.1111/j.1365-2133.1974.tb06447.x
2. Hauser C, Wuethrich B, Matter L, Wilhelm JA, Sonnabend W, Schopfer K. Staphylococcus aureus skin colonization in atopic dermatitis. Dermatologica. 1985;170(1):35–39. doi:10.1159/000249493
3. Aly R, Maibach HI, Shinefield HR. Microbial flora of atopic dermatitis. Arch Dermatol. 1977;113(6):780–782. doi:10.1001/archderm.1977.01640060076008
4. Cole GW, Silverberg NL. The adherence of Staphylococcus aureus to human corneocytes. Arch Dermatol. 1986;122(2):166–169. doi:10.1001/archderm.1986.01660140056017
5. Ong PY, Ohtake T, Brandt C, et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002;347(15):1151–1160. doi:10.1056/NEJMoa021481
6. Higaki S, Morohashi M, Yamagishi T, Hasegawa Y. Comparative study of staphylococci from the skin of atopic dermatitis patients and from healthy subjects. Int J Dermatol. 1999;38(4):265–269. doi:10.1046/j.1365-4362.1999.00686.x
7. Guzik TJ, Bzowska M, Kasprowicz A, et al. Persistent skin colonization with Staphylococcus aureus in atopic dermatitis: relationship to clinical and immunological parameters. Clin Exp Allergy. 2005;35(4):448–455. doi:10.1111/j.1365-2222.2005.02210.x
8. Zollner TM, Wichelhaus TA, Hartung A, et al. Colonization with superantigen-producing Staphylococcus aureus is associated with increased severity of atopic dermatitis. Clin Exp Allergy. 2000;30(7):994–1000. doi:10.1046/j.1365-2222.2000.00848.x|
9. Lever R, Hadley K, Downey D, Mackie R. Staphylococcal colonization in atopic dermatitis and the effect of topical mupirocin therapy. Br J Dermatol. 1998;119(2):189–198. doi:10.1111/j.1365-2133.1988.tb03201.x
10. Breuer K, Häussler S, Kappa T, Werfel T. Staphylococcus aureus: colonizing features and influence of an antibacterial treatment in adults with atopic dermatitis. Br J Dermatol. 2002;147(1):55–61. doi:10.1046/j.1365-2133.2002.04872.x
11. Schnopp C, Ring J, Mempel M. The role of antibacterial therapy in atopic eczema. Expert Opin Pharmacother. 2010;11(6):929–936. doi:10.1517/14656561003659992
12. Lee M, Van Bever H. The role of antiseptic agents in atopic dermatitis. Asia Pac Allergy. 2014;4(4):230–240. doi:10.5415/apallergy.2014.4.4.230
13. Rajka G. Emollient therapy in atopic dermatitis. J Dermatol Treat. 1997;8(Suppl 1):S19–S21. doi:10.3109/09546639709160942
14. Cork MJ. The importance of skin barrier function. J Dermatol Treat. 1997;8(Suppl 1):S7–S13. doi:10.3109/09546639709160948
15. Lucky AW, Leach AD, Laskarzewski P, Wenck H. Use of an emollient as a steroid sparing in the treatment of mild to moderate atopic dermatitis in children. Pediatr Dermatol. 1997;14(4):321–324. doi:10.1111/j.1525-1470.1997.tb00968.x|
16. Whitefield M. Effectiveness of a new antimicrobial emollient in the management of eczema/dermatitis. J Dermatol Treat. 1998;9(2):103–109. doi:10.3109/09546639809161381
17. BS EN 1499:1997. Chemical Disinfectants and Antiseptics. Hygienic Handwash. Test Methods and Requirements (phase 2/step 2). London, UK: British Standards Institute; 1997.
18. Spada F, Barnes TM, Greive KA. Skin hydration is significantly increased by a cream formulated to mimic the skin’s own natural moisturizing systems. Clin Cosmet Invest Dermatol. 2018;11:491–497. doi:10.2147/CCID.S177697
19. Marple B, Roland P, Benninger M. Safety review of benzalkonium chloride used as a preservative in intranasal solutions: an overview of conflicting data and opinions. Otolaryngol Head Neck Surg. 2004;130(1):131–141. doi:10.1016/j.otohns.2003.07.005
20. Queckenberg C, Meins J, Wachall B, et al. Absorption, pharmacokinetics, and safety of triclosan after dermal administration. Antimicrob Agents Chemother. 2010;54(1):570–572. doi:10.1128/AAC.00615-09
21. Fisher AA. Contact Dermatitis. Chapter 12.
22. Jackson EM. Triclosan in leave-on products. Cosmet Dermatol. 1998;11:23–26.
23. Bruckner-Tuderman L, Konig A, Schnyder UW. Patch test results of the dermatology clinic Zurich in 1989: personal computer aided statistical evaluation. Dermatology. 1992;184(1):29–33. doi:10.1159/000247495
24. Chaptini C, Quinn S, Marshman G. Methicillin-resistant Staphylococcus aureus in children with atopic dermatitis from 1999 to 2014: a longitudinal study. Australas J Dermatol. 2016;57(2):122–127. doi:10.1111/ajd.12371
25. Holland KT, Bojar RA, Cunliffe WJ. A Comparison of the Effect of Treatment of Atopic Eczema with and without Antimicrobial Compounds IN Round Table Series No. 37: the Bacteriology of Eczema. London: The Royal society of Medicine Press Limited; 1995:34–41.
26. Harper J. Double Blind Comparison of an Antiseptic Oil-based Bath Additive (oilatum Plus) with Regular Oilatum (oilatum Emollient) for the Treatment of Atopic Eczema IN Round Table Series No. 37: the Bacteriology of Eczema. London: The Royal society of Medicine Press Limited; 1995:42–47.
27. Tan WP, Suresh S, Tey HL, Chiam LY, Goon AT. A randomized double-blind controlled trial to compare a triclosan-containing emollient with vehicle for the treatment of atopic dermatitis. Clin Exp Dermatol. 2010;35(4):e109–e112. doi:10.1111/j.1365-2230.2009.03719.x
28. Wohlrab J, Jost G, Abeck D. Antiseptic efficacy of a low-dosed topical triclosan/chlorhexidine combination therapy in atopic dermatitis. Skin Pharmacol Physiol. 2007;20(2):71–76. doi:10.1159/000097653
29. Gehring W, Forssman T, Jost G, Gloor M. The germ-reducing effect of erythromycin and triclosan in atopic dermatitis. Aktuelle Derm. 1996;22(1):28–31.
30. Maarouf M, Shi VY. Bleach for atopic dermatitis. Dermatitis. 2018;29(3):120–126. doi:10.1097/DER.0000000000000358
31. Barnes TM, Greive KA. Use of bleach baths in the treatment of infected atopic eczema. Australas J Dermatol. 2013;54(4):251–258. doi:10.1111/ajd.12015
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.