Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Emerging Trends and Focus in Human Skin Microbiome Over the Last Decade: A Bibliometric Analysis and Literature Review
Authors Deng T, Zheng H, Zhu Y, Liu M, He G, Li Y, Liu Y, Wu J, Cheng H
Received 24 May 2023
Accepted for publication 29 July 2023
Published 10 August 2023 Volume 2023:16 Pages 2153—2173
DOI https://doi.org/10.2147/CCID.S420386
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Tinghan Deng,1 Huilan Zheng,1 Ying Zhu,2 Ming Liu,3 Guanjin He,1 Ya Li,1 Yichen Liu,1 Jingping Wu,4 Hongbin Cheng1
1Department of Dermatology, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, 610075, People’s Republic of China; 2Department of Gynecology, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, 610075, People’s Republic of China; 3Department of Medical Oncology/Gastric Cancer Center, West China Hospital, Sichuan University, Chengdu, Sichuan Province, 610041, People’s Republic of China; 4Department of Medical Cosmetology, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, 610075, People’s Republic of China
Correspondence: Jingping Wu; Hongbin Cheng, Email [email protected]; [email protected]
Background: Human skin microbiome is the first barrier against exogenous attack and is associated with various skin disease pathogenesis and progression. Advancements in high-throughput sequencing technologies have paved the way for a deeper understanding of this field. Based on the bibliometric analysis, this investigation aimed to identify the hotspots and future research trends associated with human skin microbiomes studied over the past decade.
Methods: The published research on skin microbiome from January 2013 to January 2023 was retrieved from the Web of Science Core Collection. Data cleaning processes to ensure robust data and the bibliometrix packages R, CiteSpace, VOSviewer, Origin, and Scimago Graphica for bibliometric and visual analyses were utilized.
Results: A total of 1629 published documents were analyzed. The overall publication trend steadily increased, with relatively fast growth in 2017 and 2020. The United States of America has the highest number of publications and citations and shows close collaborations with China and Germany. The University of California, San Diego, indicated a higher number of publications than other institutions and the fastest growth rate. The top three most publishing journals on this topic are Microorganisms, Frontiers in Microbiology, and Experimental dermatology. Gallo RL is the most influential author with the highest h- and g-index and most publications in skin microecology, followed by Grice EA and Kong HH. The top 10 most frequently used keywords in recent years included skin microbiome, microbiome, staphylococcus aureus, diversity, atopic dermatitis, skin, bacteria, infections, gut microbiota, and disease.
Conclusion: The skin microbiome is an area of research that requires continuous analysis, and even with much-achieved progress, future research will further be aided as technology develops.
Keywords: skin microbiome, bibliometric, trends, skin barrier, skin immune
Introduction
The skin is the largest heterogeneous organ in the human body, responsible for water homeostasis and surface thermoregulation. It also acts as the first host barrier against exogenous aggressions. Human microecosystem mainly includes oral, skin, urinary and gastrointestinal microecosystems, among which human skin microecosystem is the second largest microecosystem after intestinal microecosystem.1,2 Many symbiotic microbes - including bacteria, fungi, viruses, and parasites – coexist with humans,3 and most of them are beneficial and non-pathogenic, residing in a specific ecological site and working together to ensure skin balance.4 There are tens of thousands of microorganisms inhabiting human skin, most of which are harmless or even beneficial to the human body. The complex ecosystem composed of these microorganisms in human skin is called skin microecology. The microbe’s colonization is closely linked with skin immunity and metabolism.5 The colonized commensal bacteria stimulates the epidermis to produce antimicrobial peptides that are ineffective against themselves, thereby preventing the invasion by external pathogens.6 The diversity and community structure of skin microecology is impacted by a variety of parameters, including the local skin anatomy and conditions (including pH, sweat secretion, and sebum content), as well as gender, social environment, clothing material, etc.7–11
The Human Microbiome Project, launched in 2007, has dramatically advanced the field of microbiology.12 Humans are born with microbes, various delivery methods facilitate different colonization patterns on the skin.13 The past decade has indicated the importance of skin microecology in the etiology, severity, treatment strategies, and skin disorders prognosis.14,15 The association of skin microecology with skin disease initiation might be earlier than expected, with predictions since infancy.16,17 Moreover, compared with previous traditional microbial detection protocols, high throughput technologies such as 16S rRNA and metagenomic sequencing have emerged.18 However, microbiome research on gastrointestinal dominates more and skin microecology has not yet received sufficient attention. With the heated debate about the gut-skin axis and the resistance studies arising from topical antibiotics, it is essential to further elucidate the correlation of microorganisms with skin.
The bibliometric analysis targets academic publications and provides a comprehensive review of a specific topic by analyzing published documents for their country, institution, journal, author, keywords, and references during a particular period.19,20 By analyzing the citation relationship and publication trend of the literature related to skin microecology, bibliometrics can reveal the research trends and hotspots in academic circles. This is very helpful for researchers to choose research direction, discover new research areas and understand the development of academia. These aspects assess multiple dimensions, including frequency, co-occurrence, burst words, and co-citation analysis, to provide quantitative data to quickly understand the relevant topic. The human skin microbiome has not yet been the subject of any bibliometric analysis. Therefore, this study aims to illustrate the skin microbiome research hotspots in the past decade and visualize the overall landscape based on bibliometric analysis and data-cleaning methods.
Materials and Methods
Data Collection
We obtained the data for the bibliometric analysis from the Web of Science Core Collection database (WoSCC, Clarivate Analytics), a widely recognized and used literature search database.21,22 To avoid bias caused by daily database updates, all WoSCC screenings were carried out on February 01, 2023, for the period starting from 2013-01-01 to 2023-01-31. The search strategy included the mandatory word “skin” to avoid the impact of gastrointestinal flora. The search strategy was TS = ((“skin microbiome”) or (“skin microbiota”) or (“skin microflora”) or (“skin flora”) or (“skin microbiology”) or (“skin microecology”) or (“skin microorganism”) or (“skin micro-ecosystem”) and (“human”)). Subsequently, we utilized the page filtering feature of WoSCC and selected “articles” and “reviews” as the document types. The language of the publications was “English”. Finally, a total of 1949 documents were preprocessed and exported as Excel files for manual exclusion (Figure 1).
 |
Figure 1 Flowchart for literature filtration and data analysis. |
Data Pre-Processing
This study utilized data-cleaning techniques such as missing value supplementation, duplicate literature analysis, and merging synonyms. First, manual data cleaning was performed by Microsoft Excel software. Based on titles and abstracts, 320 papers on non-relevant topics were excluded. Because of the remarkable uniqueness of human skin microecology,23 all animal categories (including amphibians, marine mammal, horse, bat, canine, feline, insect, etc.) except for experimental mice and rats were excluded (n=304). Non-animal categories (n=16) included living environment, building, and plant categories. We retained 2 articles from 2012, despite them not strictly fitting the criteria, to avoid introducing human bias. Finally, 1629 articles were selected. A plain-text file was exported with all the full records and cited references in WoSCC for further analysis. A test using R revealed 26 missing publication year values, which were added manually. Cite Space software was used to check duplicates (n= 0). The keywords merging was carried out by thesaurus_terms.txt file (VOSviewer software) and citespace.alias file (CiteSpace software). Data collection and preprocessing were done by 2 researchers independently. In case of disagreement on the nesting of the documents, the decision was made by the 3rd researcher. The journal information was acquired from the 2022 Journal Citation Report (Clarivate Analytics, Philadelphia, PA, United States).
Data Analyses
The bibliophile website24 in the bibliometric R-package was used for frequency statistics and plotting. The relevant information was summarized in a table using Microsoft Excel (version 16.58). For bibliometric and visual analyses following software were used: CiteSpace (version 6.1.R6, Chaomei Chen,25,26), VOSviewer (version 1.6.19, van Eck and Waltman, 2010,27,28), Origin (version 2022) and SCImago Graphica (version 1.0.26, Yusef Hassan-Montero, V. Guerrero-Bote, and Félix De-Moya-Anegón,29,30).
Results
General Trend of Production and Citation
Altogether, 8458 authors published 1629 studies from 578 sources during 2013–2023, comprising 55,327 references through the main information panel in R analysis. 1207 articles and 422 reviews were found. Regarding authors and collaborations, there were 41 single-authored documents and 6.69 co-authors per other documents. International co-authorships were 28.18%, indicating very close international cooperation.
Supplementary Table 1 and Figure 2 show the annual scientific publication and citations trend. Since 2013, substantial growth has been observed twice in total in 2017 and 2020. After each rapid growth, steady growth was observed for two to three years. The average number of articles in the last 3 years was 267, while that in January 2023 was 16, indicating the gradual increase of attention to skin microecology as a research topic. Notably, despite a slight decrease in the number of publications in 2018, average citations/year peaked. However, a downward trend started afterward, suggesting that more attention is required on publication quality.
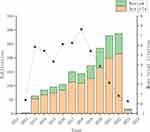 |
Figure 2 The trends of annual scientific production and citation. |
Analysis of Countries/Regions, Institutions, and Their Cooperation
To determine which countries/regions and institutions have made significant contributions to skin microecology research in the last decade, the frequency and network co-occurrence analyses were conducted (Figure 3).
Figure 3A shows the top 10 highest publishing countries. The United States of America (USA) has ranked 1st with 1798 studies. China ranked 2nd, but only at 31.03% of the USA’s. Germany and France participated in relatively high numbers of studies until 2020, but China overtook them. The total number of published articles by the top 10 countries is plotted using SCImago software (Figure 3C). Since Denmark and Spain have the same number of articles (n=137), both have been listed. It is seemed that 60% of the top 10 countries are concentrated in Europe. The USA also ranked 1st in terms of total citations (>1000), with 6.32 times more citations than Germany and France (2595), China (1554), and Denmark (1258) (Supplementary Table 2). According to the visual analysis of network co-occurrence (Figure 3D and E), the USA cooperated closely with China and Germany. Each circle = country/region, circle color = clustering result, and link thickness = degree of cooperation.
Figure 3B depicts the annual publication trends of the top 10 institutions. Half of the top 10 institutions were from the USA, with the University of California, San Diego (UCSD) having the highest publication number and the fastest growth rate. The University of Copenhagen from Denmark ranked 2nd with a publishing rate of 10 or more per year since 2019. The University of Helsinki, a leading Nordic institution, ranked 3rd. Regarding inter-institutional collaboration, three large groups (UCSD, the University of Copenhagen, and the University of Pennsylvania) and other smaller groups were observed (Figure 3F).
Analysis of Journals
The core and co-cited journals were analyzed. Bradford’s law states that 21 journals are core (Figure 4A, Table 1). The top five core journals in terms of publications include Microorganisms (52), Frontiers in Microbiology (47), Experimental Dermatology (46), Scientific Reports (44), and PLOS ONE (40).
 |
Table 1 The 21 Core Journals and Influence |
The journal impact evaluation was based on the h-index, g-index, impact factor (IF), and journal citation reports (JCR). H-index, introduced by Jorge Hirsch in 2005, refers to a journal/author with h articles cited at least h times.31 G-index, proposed by Leo Egghe in 2006, refers to a journal/author with g articles and at least g citations on average.32 As a derivative index of the H-index, it helps to identify single highly cited journals/authors. Although the Journal of Investigative Dermatology ranked 6th in the number of articles issued, it had the highest h-index (20) and was the highest locally cited journal (3986). British Journal of Dermatology and Frontiers in Microbiology showed the same h-index of 18; the latter had the highest total citation and g-index, suggesting that it has more highly cited articles. The top 10 core journal publication volumes (annual and cumulative) were also evaluated. According to Figure 4B and C, Microorganisms published 25 relevant papers in 2021, making it not only the highest-publishing journal in the calendar year but also the most-published journal in that year. However, its number of citations (642) and h-index (13) were not similar. Most journals are on a steady upward trend, with the number of articles published increasing in the last 3 years.
Supplementary Table 3 shows that all the top 10 locally cited journals have >1000 citations. Furthermore, a co-citation analysis was also carried out of 147 locally cited sources and >100 citations (Figure 4D and E), where nodes = a total number of citations, color = clustering result, and the line between two items = co-citation relevance. The intensity and thickness of the line increase as the number of co-citations increases. It can be divided into 4 clusters: (a) Dermatology field: Journal of Investigative Dermatology, Journal of Allergy and Clinical Immunology, British Journal of Dermatology, etc.; (b) Molecular biology field: Nature, PLOS One, Genome Research, etc.; (c) Microbiology field: Journal of Clinical Microbiology, Journal of Bacteriology, Infection, and Immunity, etc.; (d) Immunology field: Immunity, Journal of Immunology, Nature Reviews Immunology, etc.
Analysis of Core Author Distribution and Co-Authorship Networks
The core authors and related research in skin microecology were analyzed and clarified. Supplementary Table 4 enlists the top 10 writers’ publications, citations, and influence. Gallo RL is the most well-known author, publishes studies annually, and has the most publications among the 8458 writers with the highest h- and g-index. (Figure 5A). Grice EA (20) was the 2nd most published author, comparable to Gallo RL in impact, despite having no relevant publications in 2022. Kong HH (19) ranked 3rd and started publishing in 2014. Although Segre JA is 4th in terms of the number of publications and did not produce in 2015, he had the most local citations (n=1210), with Gallo RL (n=916) in 2nd and Kong HH (n=831) in 3rd position. Supplementary Table 5 shows the top 10 authors’ articles with total citations >300. Co-occurrence analysis revealed a close relationship between Kong HH and Segre JA, forming a core group of authors (Figure 5B). This group of authors has collaborative ties with Gallo RL, Grice EA, and Knight R, respectively. Gallo RL and Knight R belong to UCSD and contribute to most of the paper output (Figure 5C). Most authors are from the USA, contributing greatly to their publication volume.
Analysis of Keywords
To understand the hot spots of research and future directions in the last decade, keywords distribution, clustering, burst words, and timeline graph analysis was conducted. According to the statistics, the top 10 highly frequent keywords were skin microbiome, microbiome, staphylococcus aureus, diversity, atopic dermatitis, skin, bacteria, infections, gut microbiota, and disease. The cluster analysis (Figure 6A, Supplementary Table 6) of 100 high-frequency keywords (frequency > 20) indicated that currently, the research focuses on the following five areas: (a) epidemiology and preventive medicine; (b) epidermal barrier and microecology; (c) detection techniques for dermatological diseases and skin flora; (d) acne pathogenesis; (e) allergic diseases and probiotic treatment options. The last two have remained popular in recent years (Figure 6B and C).
Furthermore, the burst words were also assessed (Figure 6D), and the green and red lines indicate the time range and the period of pulse duration, respectively. In 2013, the understanding of skin microecology was mostly focused on identifying and recognizing flora, but by 2014 it was extended to molecular immune mechanisms. 2014 was also the year when sequencing technology 16S rRNA came into the limelight. Figure 6E is a timeline of keywords obtained by Citespace software, suggesting future research hotspots in skin microecology, including ultraviolet, oxidative stress, ph, skin aging, ceramide, skin cancer, gut-skin axis, prebiotics therapy, etc.
Analysis of Documents and References
To identify the most influential articles in skin microecology research, the included literature and references were assessed. Table 2 enlists the top 10 globally cited documents, which are the highly cited documents in WoSS. Of these, Gilbert JA’s review “Current understanding of the human microbiome”, published in Nature Medicine 2018, ranked 1st. The article describes the factors influencing the human microbiome, the dynamic balance of human microbes, and present and future directions of mechanistic research in detail.33 The 2nd was Byrd AL’s review of “The human skin microbiome”, also published in the same year in Nature Reviews Microbiology, and analyzed the skin microbiome in health and disease conditions.34 This is also the first locally cited document (Supplementary Table 7) and the most highly cited document included in this dataset. Byrd AL and Chen YE’s review “Skin microbiota-host interactions”, published in Nature in 2018, is likely to receive more citations in the future, according to the burst citation analysis (Figure 7B). The Historiography helped us understand the literature with high importance in the dataset (Figure 7A, Supplementary Table 8). Figures 7C and D depict the co-citation analysis of the references, indicating that Grice EA’s experimental article “Topographical and temporal diversity of the human skin microbiome”, published in Science in 2009, was also in the core position. Table 3 shows the top 10 locally cited references.
 |
Table 2 Top10 Global Cited Documents |
 |
Table 3 Top 10 Locally Cited References |
Discussion
The skin and the intestines are the sites with the most abundant microbes, but the former has received less published research than the latter.46 Skin microbes have a different composition than the intestines, comprising predominantly aerobic or partly anaerobic bacteria, whereas the intestines are mostly anaerobic.35,47 And the distribution of skin microbiota can vary across sites.41 Staphylococci species are frequently predominant at sebum-secreting and moist sites, where sweat is secreted commonly. Propionibacteria species predominate sebaceous sites, Corynebacteria species predominate moist sites, and β-Proteobacteria and Flavobacteriales predominate dry sites. Among them, the most studied were Staphylococci species, especially the highly pathogenic Staphylococcus aureus (S. aureus) (Figure 6C). Unlike Staphylococcus epidermidis, which seldom causes pathogenesis, S. aureus is the major pathogen of skin infections.48 It can specifically release inflammatory mediators (IL-1α, IL-24β) from keratinocytes to produce skin inflammation.6 Notably, S. aureus is also genetically variable and strengthens itself by genome alteration to expand territory, virulence, and immune evasion.49,50 Furthermore, it is known to promote wound healing and hair follicle regeneration. It enhances keratinocyte hypoxia, stimulates cellular glutamine metabolism, and exerts beneficial effects through the IL-1β-MyD88 signaling pathway.51,52 Compared with an 11% incidence in healthy skin, S. aureus has a relative abundance of ≥30% in infection-free surgical wounds. Some studies have proposed that the mechanism behind lower S. aureus infection may be related to the enrichment of Corynebacterium,53 implying that the skin microorganisms interactions could have a benign effect on the hosts, like how yin and yang are balanced in traditional Chinese medicine.
The skin barrier is currently a hot research topic for clinicians.54,55 The skin microorganisms are in a harmonious interaction with the body epidermis on which they depend. At one end, the epidermal barrier integrity determines the diversity and composition of microorganisms,56 and at the other end, the microorganisms influence the stability of the epidermal barrier. Commensal microbes can rebuild the epidermal barrier by turning on the aryl hydrocarbon receptor and restoring anti-infection function.57,58 Staphylococcus epidermidis helps preserve skin barrier integrity by secreting sphingomyelinase, which can produce ceramides that retain water and fight aging.59 In addition to the most superficial microbial barrier, skin barriers are functionally classified as chemical, physical, immune, and neuronal barriers.60,61 They exhibit growing networks from the outside to the inside, while neither is entirely independent. Among them, the chemical barrier is the acidic shield composed of lipid membranes (ceramides, cholesterol, and free fatty acids), sweat, and natural-moisturizing factors (amino acids, lactates, urea, and electrolytes, etc.) on the surface of the stratum corneum.61,62 The ph is the main determinant of the chemical barrier, which increases upon physical barrier disruption and has been the focus of multiple studies since 2021 (Figure 6D). Normal human stratum corneum has a ph range of 4.1 to 5.8.63 Elevated ph can damage the chemical barrier, reducing the skin’s antimicrobial capacity and thereby increasing the skin’s risk of infection. Since commensal microbes cannot tolerate a non-acidic environment, their ability to adhere to the skin surface deteriorates.64–66 This microecological imbalance due to ph alterations can occur because of daily skin cleansing routine.67 Therefore, a sound understanding of the connection between the skin barrier and microbes can be the foundation for healthy skin hygiene.
Streilein was the first to propose the idea of skin-associated lymphoid tissues in 1983, whereas the concept of the “skin immune system” was introduced by Bos and Kapsenberg in 1986.68,69 In general, the main cell populations that exert cutaneous immunity include the keratinocytes, epidermal Langerhans cells, dendritic cells, mast cells, and T cell subsets (mainly T regulatory and T resident memory cells) in the dermis.70,71 Currently, the most studied cells are keratinocytes, associated with innate immunity. It’s core immunological role is to produce constitutive epidermal antimicrobial proteins (AMPs) and various hornerin polypeptides-derived cationic intrinsically disordered antimicrobial peptides (CIDAMPs) against invading infections.72 The first AMP to be discovered was lysozyme.73 However, defensins are the most researched AMPs and can be classified into human α- and β-defensins.74–76 Together with cathelicidins, dermcidin, and psoriasis, these molecules have strong anti-inflammatory and antibacterial properties.77 Furthermore, recent studies have shown that a deficiency of IL-17 receptors in keratinocytes of mice is closely associated with S. aureus skin infection and acts as an activator of T cell proliferation.78 T cells are not only involved in skin immunity but also modulate skin homeostasis and promote wound healing, all of which have attracted the attention of researchers. It has been shown that there are 2.0×1010 T cells in healthy skin, nearly twice the total circulating T cells.79 Among them, the most discussed are the resident memory T cells (TRMs), which are important for skin immune responses and surveillance.80–82 Skin infections can encourage CD8 TRMs to produce immunological effectors, enabling long-lasting effects.83 Whereas CD4 TRMs release IL-17A, IL-22, IFN-γ, and TNF-α to kill S. aureus, thereby regulating skin microbes.84
Research on skin flora and dermatology is now focused on inflammatory, allergic, and immune skin diseases, and skin cancers are an emerging trend. Acne vulgaris is a widely studied inflammatory skin disease that often occurs in high sebum secretion sites such as the face, scalp, chest, and back.85,86 Cutibacterium acnes or Propionibacterium acnes are essentially linked with pathogenic mechanisms of the disease and are the theoretical cornerstone of the current application of antibiotic therapy.45,87,88 Moreover, Cutibacterium acnes interact with Staphylococcus epidermidis, and their dysregulation can release inflammatory cytokines.89 The next most studied skin diseases are atopic dermatitis (AD) and psoriasis.90 AD is characterized by polymorphic lesions with persistent and intense itching.38,91,92 Increased S. aureus colonization reduces the diversity of skin bacteria at AD-prone sites, which is strongly associated with the onset and severity of AD.36,42,93 Skin microecology is also involved in the pathogenesis and progression of psoriasis.14,37,94 Skin microecology had similar differences in healthy or in patients without lesions, as well as between patients’ lesion sites and contralateral non-lesion sites.15 Based on the pro-inflammatory and immune effects of skin microbial dysbiosis, the link between skin cancers and skin microecology has become a topic of interest.95 Malignant melanoma progression has been correlated with alterations in skin microecology.96 S. aureus has also been correlated with the progression of cutaneous squamous cell carcinoma97 and T -cell lymphoma.98 We may aspire for more research in this field, and these findings will also bring hope for cancer immunotherapy sensitization.
Although the study of gastrointestinal flora was excluded, a high frequency of the keyword “gut” was still observed (Figure 6A). Due to the interaction between the skin and the gut, the gut-skin axis notion has steadily evolved.99,100 For instance, the pathophysiology of acne vulgaris may be influenced by disturbances in the gut microbial metabolism.101 Individuals with inflammatory bowel disease can also experience dysbiosis of the skin flora and may even indicate post-skin treatment adverse events.102 This highlights the treatment option of probiotics, prebiotics, and postbiotics, available as supplemental therapies in addition to the commonly used antimicrobial agents. As defined by the International Scientific Association for Probiotics and Prebiotics (ISAPP), probiotics are “live microorganisms which, when administered in adequate amounts, confer a health benefit on the host“.103 At the same time, prebiotics is “a substrate that is selectively utilized by host microorganisms conferring a health benefit”.104 Since these have been around for decades, much research is present. Until 2019, postbiotics were also called “preparation of inanimate microorganisms and, or their components that confer a health benefit on the host”.105 The synergistic probiotics and prebiotics, or synbiotics, were first introduced by Gibson and Roberfroid in 1995.106 Non-medical topical application of prebiotics-comprising cosmetic serum improves the skin’s ability to retain water in women.107 A moisturizer containing prebiotics and postbiotics has been found to reduce facial wrinkles in women.108 Oral administration of probiotic and prebiotic fermented milk improved the hydration of healthy women’s skin and ensured skin barrier function.109 Research reveals that clinical oral spore-based probiotic ingestion reduces sebum secretion and acne lesions in acne patients.110 Topical postbiotic application promoted wound healing in diabetic mice by releasing growth factors, chemokines, and cytokines.111 Prebiotic or symbiotic baths can alleviate AD severity and ameliorate the symptoms of itching and dryness.112 Probiotics and prebiotics can also counteract ultraviolet radiation-induced photoaging, immunosuppression, and inflammatory responses.113 Therefore, using microbiome-associated microorganisms to address skin diseases is a promising strategy.
There are several microbiome studies based on bibliometric analysis. Most publications are focused on gut microbes and their associated diseases, including pain,114 metabolic-associated fatty liver disease,115 Alzheimer’s disease,116 and rheumatic diseases.117 Some studies explored the mechanisms, including microbiome–gut–brain axis, dementia,118 and miRNA-microbiome interaction.119 Xingzhu Yuan et al46 separately focused on the human gastrointestinal microbiome and showed the highlights and recent trends of previous studies in this field. In contrast, the bibliometric articles on skin microbiomes are scant. Only 1 bibliometric study on allergic disease and microbes containing AD was identified, but it did not distinguish between the skin microbiome and gut flora.120 Another article discussing symbiotic microorganisms and AD lacked a clear distinction between them.121 Therefore, this study was designed to differentiate skin and gut microorganisms, making it the first bibliometric study on the skin microbiome.
Through a comprehensive literature review, it was proposed that future skin microecology research will have the following 3 directions: (1) antibiotic resistance and skin microbiome: antimicrobial resistance is a serious global health problem.122 Scholars have launched an integrated Human Skin Microbial Gene Catalog to describe skin resistome to discover antibiotic resistance genes and human skin flora distribution.123 This is crucial for the next step in complex skin microecology research. (2) Anti-aging and skin microbiome: human aging is inevitable and associated with gut microbiota dysregulation.124 With deepening aesthetic concepts and accelerating population aging, skin anti-aging is a key task for dermatologists and aestheticians.125 Streptococcus species have already been found to exert anti-aging effects by secreting spermidine.126 (3) Artificial intelligence and skin microbiome: the development of skin microecology is accompanied by new technologies. Next-generation sequencing and artificial intelligence technologies are now gradually being applied in this field, such as convolutional neural networks and machine learning.127 One study found that the accuracy rate in diagnosing onychomycosis can be improved with convolutional neural network,128 and by merging the patient’s other information, machine learning may thoroughly analyze the data in next-generation sequencing.
Limitations
There are also certain limitations to this study. 1) Data from only the last 10 years was studied, and earlier literature was not included; therefore, there is a lack of traceability of the research focus. 2) The known studies on skin microecology are still insufficient, common clinical pigmented skin diseases were rarely addressed, and the existing basic experiments still require clinical validation. 3) The limitations of bibliometric analysis were present, such as the inability to exclude data confounding by author renaming.
Conclusion
In conclusion, this bibliometric analysis involves a comprehensive literature review of publications from the past decade on skin microbiomes. Data cleaning processes such as missing value supplementation, and synonym merging were used to ensure data robustness. The results indicated that much had been achieved in this field; however, it still requires continuous progress. Current studies focus on skin microbe diversity, distribution characteristics, interaction with host epidermal immunity, and roles in skin disorders. Artificial intelligence and sequencing technology development will pave the way for future research. This bibliometric study is a reference for researchers to better grasp the trends and priorities of skin microbiology.
Abbreviations
UCSD, University of California, San Diego; IF, impact factor; JCR, journal citation reports; S. aureus, Staphylococcus aureus; AMPs, antimicrobial proteins; CIDAMPs, cationic intrinsically disordered antimicrobial peptides; TRMs, resident memory T cells; AD, atopic dermatitis; ISAPP, International Scientific Association for Probiotics and Prebiotics.
Data Sharing Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.
Consent for Publication
All authors agree publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the “Mechanistic study and clinical evaluation of Qichu Meibai Cream for melasma based on epidermal microecological theory”, no. 2022YFS0416, “Imaging evaluation of Qichu Meibai Cream for melasma in split-face mode”, no. 22XZ07. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
All authors report no competing interests in this work.
References
1. Rees J. Understanding barrier function of the skin. Lancet. 1999;354(9189):1491–1492. doi:10.1016/S0140-6736(99)00281-0
2. Fuchs E. Epithelial Skin Biology: three Decades of Developmental Biology, a Hundred Questions Answered and a Thousand New Ones to Address. Curr Top Dev Biol. 2016;116:357–374.
3. Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol. 2011;9(4):244–253. doi:10.1038/nrmicro2537
4. Dréno B, Dagnelie MA, Khammari A, Corvec S. The Skin Microbiome: a New Actor in Inflammatory Acne. Am J Clin Dermatol. 2020;21(Suppl 1):18–24. doi:10.1007/s40257-020-00531-1
5. Wang Y, Kuo S, Shu M, et al. Staphylococcus epidermidis in the human skin microbiome mediates fermentation to inhibit the growth of Propionibacterium acnes: implications of probiotics in acne vulgaris. Appl Microbiol Biotechnol. 2014;98(1):411–424.
6. Clayton K, Holbrook DJ, Vallejo A, et al. Skin programming of inflammatory responses to Staphylococcus aureus is compartmentalized according to epidermal keratinocyte differentiation status. Br J Dermatol. 2023;188(3):396–406. doi:10.1093/bjd/ljac088
7. Skowron K, Bauza-Kaszewska J, Kraszewska Z, et al. Human Skin Microbiome: impact of Intrinsic and Extrinsic Factors on Skin Microbiota. Microorganisms. 2021;9(3):543. doi:10.3390/microorganisms9030543
8. Robert C, Cascella F, Mellai M, et al. Influence of Sex on the Microbiota of the Human Face. Microorganisms. 2022;10(12):2470. doi:10.3390/microorganisms10122470
9. Melnik AV, Callewaert C, Dorrestein K, et al. The Molecular Effect of Wearing Silver-Threaded Clothing on the Human Skin. mSystems. 2023;8(1):e0092222. doi:10.1128/msystems.00922-22
10. Song SJ, Lauber C, Costello EK, et al. Cohabiting family members share microbiota with one another and with their dogs. eLife. 2013;2:e00458. doi:10.7554/eLife.00458
11. Lax S, Smith DP, Hampton-Marcell J, et al. Longitudinal analysis of microbial interaction between humans and the indoor environment. Science. 2014;345(6200):1048–1052. doi:10.1126/science.1254529
12. Gevers D, Knight R, Petrosino JF, et al. The Human Microbiome Project: a community resource for the healthy human microbiome. PLoS Biol. 2012;10(8):e1001377. doi:10.1371/journal.pbio.1001377
13. Dominguez-Bello MG, Costello EK, Contreras M, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107(26):11971–11975. doi:10.1073/pnas.1002601107
14. Choi JY, Kim H, Koo HY, et al. Severe Scalp Psoriasis Microbiome Has Increased Biodiversity and Relative Abundance of Pseudomonas Compared to Mild Scalp Psoriasis. J Clin Med. 2022;11(23):7133. doi:10.3390/jcm11237133
15. Boix-Amorós A, Badri MH, Manasson J, et al. Alterations in the cutaneous microbiome of patients with psoriasis and psoriatic arthritis reveal similarities between non-lesional and lesional skin. Ann Rheum Dis;2022.
16. Rapin A, Rehbinder EM, Macowan M, et al. The skin microbiome in the first year of life and its association with atopic dermatitis. Allergy. 2023;78(7):1949–1963. doi:10.1111/all.15671
17. Luna PC. Skin Microbiome as Years Go By. Am J Clin Dermatol. 2020;21(Suppl 1):12–17.
18. Ferretti P, Farina S, Cristofolini M, Girolomoni G, Tett A, Segata N. Experimental metagenomics and ribosomal profiling of the human skin microbiome. Exp Dermatol. 2017;26(3):211–219.
19. Ninkov A, Frank JR, Maggio LA. Bibliometrics: methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173–176. doi:10.1007/S40037-021-00695-4
20. George RJ, A PS. Bibliometric Analysis for Medical Research. Indian J Psychol Med. 2013. 02537176221103617.
21. Birkle C, Pendlebury DA, Schnell J, Adams J. Web of Science as a data source for research on scientific and scholarly activity. Quantitative Science Studies. 2020;1(1):363–376. doi:10.1162/qss_a_00018
22. Mongeon P, Paul-Hus A. The journal coverage of Web of Science and Scopus: a comparative analysis. Scientometrics. 2015;106:213–228. doi:10.1007/s11192-015-1765-5
23. Ross AA, Müller KM, Weese JS, Neufeld JD. Comprehensive skin microbiome analysis reveals the uniqueness of human skin and evidence for phylosymbiosis within the class Mammalia. Proc Natl Acad Sci U S A. 2018;115(25):E5786–e5795. doi:10.1073/pnas.1801302115
24. Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–975. doi:10.1016/j.joi.2017.08.007
25. Chen C, Song M. Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS One. 2019;14(10):e0223994. doi:10.1371/journal.pone.0223994
26. ChenC. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Assoc Inf Sci Technol. 2006;57:359–377. doi:10.1002/asi.20317
27. van Eck NJ, Waltman L. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi:10.1007/s11192-009-0146-3
28. Waltman L, Nees Jan van E, Noyons ECM. A unified approach to mapping and clustering of bibliometric networks. J Informetr. 2010;4(4):629–635. doi:10.1016/j.joi.2010.07.002
29. Hassan-Montero Y, De-Moya-Anegón F, Guerrero-Bote VP. SCImago Graphica: a new tool for exploring and visually communicating data. El Profesional de la información. 2022. doi:10.3145/epi.2022.sep.02
30. Hassan-Montero Y, Guerrero-Bote VP, De-Moya-Anegón F. Graphical interface of the SCImago Journal and Country rank: an interactive approach to accessinG bibliometric information. Profesional De La Informacion. 2014;23:272–278. doi:10.3145/epi.2014.may.07
31. Hirsch JE. An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A. 2005;102(46):16569–16572. doi:10.1073/pnas.0507655102
32. E L. Theory and practice of the g-index. Scientometrics. 2006;69:131–152. doi:10.1007/s11192-006-0144-7
33. Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. Current understanding of the human microbiome. Nat Med. 2018;24(4):392–400. doi:10.1038/nm.4517
34. Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nat Rev Microbiol. 2018;16(3):143–155.
35. Oh J, Byrd AL, Deming C, Conlan S, Kong HH, Segre JA. Biogeography and individuality shape function in the human skin metagenome. Nature. 2014;514(7520):59–64. doi:10.1038/nature13786
36. Nakatsuji T, Chen TH, Narala S, et al. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci Transl Med. 2017;9(378). doi:10.1126/scitranslmed.aah4680
37. Rendon A, Schäkel K. Psoriasis Pathogenesis and Treatment. Int J Mol Sci. 2019;20(6):1475. doi:10.3390/ijms20061475
38. Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nature Rev Dis Primers. 2018;4(1):1. doi:10.1038/s41572-018-0001-z
39. Oh J, Byrd AL, Park M, Comparative Sequencing Program NISC, Kong HH, Segre JA. Temporal Stability of the Human Skin Microbiome. Cell. 2016;165(4):854–866. doi:10.1016/j.cell.2016.04.008
40. Gupta VK, Paul S. Geography, Ethnicity or Subsistence-Specific Variations in Human Microbiome Composition and Diversity. Front Microbiol. 2017;8:1162. doi:10.3389/fmicb.2017.01162
41. Grice EA, Kong HH, Conlan S, et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009;324(5931):1190–1192. doi:10.1126/science.1171700
42. Kong HH, Oh J, Deming C, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012;22(5):850–859. doi:10.1101/gr.131029.111
43. Costello EK, Lauber CL, Hamady M, Fierer N, Gordon JI, Knight R. Bacterial community variation in human body habitats across space and time. Science. 2009;326(5960):1694–1697. doi:10.1126/science.1177486
44. Grice EA, Kong HH, Renaud G, et al. A diversity profile of the human skin microbiota. Genome Res. 2008;18(7):1043–1050. doi:10.1101/gr.075549.107
45. Fitz-Gibbon S, Tomida S, Chiu BH, et al. Propionibacterium acnes strain populations in the human skin microbiome associated with acne. J Invest Dermatol. 2013;133(9):2152–2160. doi:10.1038/jid.2013.21
46. Yuan X, Chang C, Chen X, Li K. Emerging trends and focus of human gastrointestinal microbiome research from 2010-2021: a visualized study. J Transl Med. 2021;19(1):327. doi:10.1186/s12967-021-03009-8
47. Coates M, Lee MJ, Norton D, MacLeod AS. The Skin and Intestinal Microbiota and Their Specific Innate Immune Systems. Front Immunol. 2019;10:2950. doi:10.3389/fimmu.2019.02950
48. Ray GT, Suaya JA, Baxter R. Microbiology of skin and soft tissue infections in the age of community-acquired methicillin-resistant Staphylococcus aureus. Diagn Microbiol Infect Dis. 2013;76(1):24–30. doi:10.1016/j.diagmicrobio.2013.02.020
49. Lindsay JA, Fischetti VA, Novick RP. Staphylococci: evolving Genomes. Microbiology Spectrum. 2019;7(6). doi:10.1128/microbiolspec.GPP3-0071-2019
50. Kwiecinski JM, Kratofil RM, Parlet CP, Surewaard BGJ, Kubes P, Horswill AR. Staphylococcus aureus uses the ArlRS and MgrA cascade to regulate immune evasion during skin infection. Cell Rep. 2021;36(4):109462. doi:10.1016/j.celrep.2021.109462
51. Wang G, Sweren E, Liu H, et al. Bacteria induce skin regeneration via IL-1β signaling. Cell Host Microbe. 2021;29(5):777–791.e776. doi:10.1016/j.chom.2021.03.003
52. Wang G, Sweren E, Andrews W, et al. Commensal microbiome promotes hair follicle regeneration by inducing keratinocyte HIF-1α signaling and glutamine metabolism. Sci Adv. 2023;9(1):eabo7555. doi:10.1126/sciadv.abo7555
53. Gupta S, Poret AJ, Hashemi D, et al. Cutaneous Surgical Wounds Have Distinct Microbiomes from Intact Skin. Microbiology Spectrum. 2023;11(1):e0330022. doi:10.1128/spectrum.03300-22
54. Luger T, Amagai M, Dreno B, et al. Atopic dermatitis: role of the skin barrier, environment, microbiome, and therapeutic agents. J Dermatol Sci. 2021;102(3):142–157. doi:10.1016/j.jdermsci.2021.04.007
55. Akdis CA. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat Rev Immunol. 2021;21(11):739–751.
56. Zhou L, Liu X, Li X, He X, Xiong X, Lai J. Epidermal Barrier Integrity is Associated with Both Skin Microbiome Diversity and Composition in Patients with Acne Vulgaris. Clin Cosmet Investig Dermatol. 2022;15:2065–2075. doi:10.2147/CCID.S377759
57. Uberoi A, Bartow-McKenney C, Zheng Q, et al. Commensal microbiota regulates skin barrier function and repair via signaling through the aryl hydrocarbon receptor. Cell Host Microbe. 2021;29(8):1235–1248.e1238.
58. Fernández-Gallego N, Sánchez-Madrid F, Cibrian D. Role of AHR Ligands in Skin Homeostasis and Cutaneous Inflammation. Cells. 2021;10(11):3176. doi:10.3390/cells10113176
59. Zheng Y, Hunt RL, Villaruz AE, et al. Commensal Staphylococcus epidermidis contributes to skin barrier homeostasis by generating protective ceramides. Cell Host Microbe. 2022;30(3):301–313.e309. doi:10.1016/j.chom.2022.01.004
60. Eyerich S, Eyerich K, Traidl-Hoffmann C, Biedermann T. Cutaneous Barriers and Skin Immunity: differentiating A Connected Network. Trends Immunol. 2018;39(4):315–327.
61. Lefèvre-Utile A, Braun C, Haftek M, Aubin F. Five Functional Aspects of the Epidermal Barrier. Int J Mol Sci. 2021;22(21):11676. doi:10.3390/ijms222111676
62. Shamaprasad P, Frame CO, Moore TC, et al. Using molecular simulation to understand the skin barrier. Prog Lipid Res. 2022;88:101184.
63. Proksch E. pH in nature, humans and skin. J Dermatol. 2018;45(9):1044–1052. doi:10.1111/1346-8138.14489
64. Bewick S, Gurarie E, Weissman JL, et al. Trait-based analysis of the human skin microbiome. Microbiome. 2019;7(1):101.
65. Lambers H, Piessens S, Bloem A, Pronk H, Finkel P. Natural skin surface pH is on average below 5, which is beneficial for its resident flora. Int J Cosmet Sci. 2006;28(5):359–370. doi:10.1111/j.1467-2494.2006.00344.x
66. Gonçalves LG, Santos S, Gomes LP, Armengaud J, Miragaia M, Coelho AV. Skin-to-blood pH shift triggers metabolome and proteome global remodelling in Staphylococcus epidermidis. Front Microbiol. 2022;13:1000737.
67. Blaak J, Staib P. The Relation of pH and Skin Cleansing. Curr Probl Dermatol. 2018;54:132–142.
68. Streilein JW. Skin-associated lymphoid tissues (SALT): origins and functions. J Invest Dermatol. 1983;80:12s–16s. doi:10.1111/1523-1747.ep12536743
69. Bos JD, Kapsenberg ML. The skin immune system Its cellular constituents and their interactions. Immunol Today. 1986;7(7–8):235–240.
70. Nestle FO, Di Meglio P, Qin JZ, Nickoloff BJ. Skin immune sentinels in health and disease. Nat Rev Immunol. 2009;9(10):679–691. doi:10.1038/nri2622
71. Chambers ES, Vukmanovic-Stejic M. Skin barrier immunity and ageing. Immunology. 2020;160(2):116–125. doi:10.1111/imm.13152
72. Latendorf T, Gerstel U, Wu Z, et al. Cationic Intrinsically Disordered Antimicrobial Peptides (CIDAMPs) Represent a New Paradigm of Innate Defense with a Potential for Novel Anti-Infectives. Sci Rep. 2019;9(1):3331. doi:10.1038/s41598-019-39219-w
73. Papini M, Simonetti S, Franceschini S, Scaringi L, Binazzi M. Lysozyme distribution in healthy human skin. Arch Dermatol Res. 1982;272(1–2):167–170. doi:10.1007/BF00510410
74. Dong X, Limjunyawong N, Sypek EI, et al. Keratinocyte-derived defensins activate neutrophil-specific receptors Mrgpra2a/b to prevent skin dysbiosis and bacterial infection. Immunity. 2022;55(9):1645–1662.e1647. doi:10.1016/j.immuni.2022.06.021
75. Fruitwala S, El-Naccache DW, Chang TL. Multifaceted immune functions of human defensins and underlying mechanisms. Semin Cell Dev Biol. 2019;88:163–172. doi:10.1016/j.semcdb.2018.02.023
76. Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol. 2003;3(9):710–720. doi:10.1038/nri1180
77. Rademacher F, Gläser R, Harder J. Antimicrobial peptides and proteins: interaction with the skin microbiota. Exp Dermatol. 2021;30(10):1496–1508. doi:10.1111/exd.14433
78. Moos S, Regen T, Wanke F, et al. IL-17 signaling in keratinocytes orchestrates the defense against Staphylococcus aureus skin infection. J Invest Dermatol. 2023;143(7):1257–1267.e10. doi:10.1016/j.jid.2023.01.016
79. Clark RA, Chong B, Mirchandani N, et al. The vast majority of CLA+ T cells are resident in normal skin. J Immunol. 2006;176(7):4431–4439. doi:10.4049/jimmunol.176.7.4431
80. LeibundGut-Landmann S. Tissue-Resident Memory T Cells in Antifungal Immunity. Front Immunol. 2021;12:693055. doi:10.3389/fimmu.2021.693055
81. Sasson SC, Gordon CL, Christo SN, Klenerman P, Mackay LK. Local heroes or villains: tissue-resident memory T cells in human health and disease. Cell Mol Immunol. 2020;17(2):113–122. doi:10.1038/s41423-019-0359-1
82. Emmanuel T, Mistegård J, Bregnhøj A, Johansen C, Iversen L. Tissue-Resident Memory T Cells in Skin Diseases: a Systematic Review. Int J Mol Sci. 2021;22(16):9004. doi:10.3390/ijms22169004
83. Jiang X, Clark RA, Liu L, Wagers AJ, Fuhlbrigge RC, Kupper TS. Skin infection generates non-migratory memory CD8+ T(RM) cells providing global skin immunity. Nature. 2012;483(7388):227–231. doi:10.1038/nature10851
84. Hendriks A, Mnich ME, Clemente B, et al. Staphylococcus aureus-Specific Tissue-Resident Memory CD4(+) T Cells Are Abundant in Healthy Human Skin. Front Immunol. 2021;12:642711. doi:10.3389/fimmu.2021.642711
85. Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–372. doi:10.1016/S0140-6736(11)60321-8
86. O’Neill AM, Gallo RL. Host-microbiome interactions and recent progress into understanding the biology of acne vulgaris. Microbiome. 2018;6(1):177. doi:10.1186/s40168-018-0558-5
87. Lomakin IB, Devarkar SC, Patel S, Grada A, Bunick CG. Sarecycline inhibits protein translation in Cutibacterium acnes 70S ribosome using a two-site mechanism. Nucleic Acids Res. 2023;51(6):2915–2930. doi:10.1093/nar/gkad103
88. Mias C, Mengeaud V, Bessou-Touya S, Duplan H. Recent advances in understanding inflammatory acne: deciphering the relationship between Cutibacterium acnes and Th17 inflammatory pathway. J Eur Acad Dermatol Venereol. 2023;37(2):3–11. doi:10.1111/jdv.18794
89. Dagnelie MA, Corvec S, Timon-David E, Khammari A, Dréno B. Cutibacterium acnes and Staphylococcus epidermidis: the unmissable modulators of skin inflammatory response. Exp Dermatol. 2022;31(3):406–412. doi:10.1111/exd.14467
90. Fyhrquist N, Muirhead G, Prast-Nielsen S, et al. Microbe-host interplay in atopic dermatitis and psoriasis. Nat Commun. 2019;10(1):4703. doi:10.1038/s41467-019-12253-y
91. Sroka-Tomaszewska J, Trzeciak M. Molecular Mechanisms of Atopic Dermatitis Pathogenesis. Int J Mol Sci. 2021;22(8):4130. doi:10.3390/ijms22084130
92. Wasserbauer N, Ballow M. Atopic dermatitis. Am J Med. 2009;122(2):121–125. doi:10.1016/j.amjmed.2008.09.014
93. Rauer L, Reiger M, Bhattacharyya M, et al. Skin microbiome and its association with host cofactors in determining atopic dermatitis severity. J Eur Acad Dermatol Venereol. 2022.
94. Chen D, He J, Li J, et al. Microbiome and Metabolome Analyses Reveal Novel Interplay Between the Skin Microbiota and Plasma Metabolites in Psoriasis. Front Microbiol. 2021;12:643449. doi:10.3389/fmicb.2021.643449
95. Woo YR, Cho SH, Lee JD, Kim HS. The Human Microbiota and Skin Cancer. Int J Mol Sci. 2022;23(3):1813. doi:10.3390/ijms23031813
96. Mekadim C, Skalnikova HK, Cizkova J, et al. Dysbiosis of skin microbiome and gut microbiome in melanoma progression. BMC Microbiol. 2022;22(1):63. doi:10.1186/s12866-022-02458-5
97. Wood DLA, Lachner N, Tan JM, et al. A Natural History of Actinic Keratosis and Cutaneous Squamous Cell Carcinoma Microbiomes. mBio. 2018;9(5). doi:10.1128/mBio.01432-18
98. Talpur R, Bassett R, Duvic M. Prevalence and treatment of Staphylococcus aureus colonization in patients with mycosis fungoides and Sézary syndrome. Br J Dermatol. 2008;159(1):105–112. doi:10.1111/j.1365-2133.2008.08612.x
99. De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut-Skin Axis: current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms. 2021;9(2):353. doi:10.3390/microorganisms9020353
100. Sinha S, Lin G, Ferenczi K. The skin microbiome and the gut-skin axis. Clin Dermatol. 2021;39(5):829–839. doi:10.1016/j.clindermatol.2021.08.021
101. Huang Y, Liu L, Hao Z, et al. Potential roles of gut microbial tryptophan metabolites in the complex pathogenesis of acne vulgaris. Front Microbiol. 2022;13:942027. doi:10.3389/fmicb.2022.942027
102. Reiss Z, Rob F, Kolar M, et al. Skin microbiota signature distinguishes IBD patients and reflects skin adverse events during anti-TNF therapy. Front Cell Infect Microbiol. 2022;12:1064537. doi:10.3389/fcimb.2022.1064537
103. Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–514. doi:10.1038/nrgastro.2014.66
104. Gibson GR, Hutkins R, Sanders ME, et al. Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491–502. doi:10.1038/nrgastro.2017.75
105. Salminen S, Collado MC, Endo A, et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol. 2021;18(9):649–667. doi:10.1038/s41575-021-00440-6
106. Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr. 1995;125(6):1401–1412. doi:10.1093/jn/125.6.1401
107. Hong KB, Hong YH, Jung EY, Jo K, Suh HJ. Changes in the Diversity of Human Skin Microbiota to Cosmetic Serum Containing Prebiotics: results from a Randomized Controlled Trial. J Personalized Med. 2020;10(3):91. doi:10.3390/jpm10030091
108. Iglesia S, Kononov T, Zahr AS. A multi-functional anti-aging moisturizer maintains a diverse and balanced facial skin microbiome. J Appl Microbiol. 2022;133(3):1791–1799. doi:10.1111/jam.15663
109. Mori N, Kano M, Masuoka N, et al. Effect of probiotic and prebiotic fermented milk on skin and intestinal conditions in healthy young female students. Biosci Microbiota Food Health. 2016;35(3):105–112. doi:10.12938/bmfh.2015-022
110. Rybak I, Haas KN, Dhaliwal SK, et al. Prospective Placebo-Controlled Assessment of Spore-Based Probiotic Supplementation on Sebum Production, Skin Barrier Function, and Acne. J Clin Med. 2023;12(3):895. doi:10.3390/jcm12030895
111. Nam Y, Kim J, Baek J, Kim W. Improvement of Cutaneous Wound Healing via Topical Application of Heat-Killed Lactococcus chungangensis CAU 1447 on Diabetic Mice. Nutrients. 2021;13(8):2666. doi:10.3390/nu13082666
112. Noll M, Jäger M, Lux L, Buettner C, Axt-Gadermann M. Improvement of Atopic Dermatitis by Synbiotic Baths. Microorganisms. 2021;9(3):527. doi:10.3390/microorganisms9030527
113. Patra V, Gallais Sérézal I, Wolf P. Potential of Skin Microbiome, Pro- and/or Pre-Biotics to Affect Local Cutaneous Responses to UV Exposure. Nutrients. 2020;12(6):1795. doi:10.3390/nu12061795
114. Mao M, Zhou Y, Jiao Y, et al. Bibliometric and visual analysis of research on the links between the gut microbiota and pain from 2002 to 2021. Front med. 2022;9:975376. doi:10.3389/fmed.2022.975376
115. Li Y, Zhou Y, Wang L, et al. Emerging trends and hotspots in the links between the gut microbiota and MAFLD from 2002 to 2021: a bibliometric analysis. Front Endocrinol (Lausanne). 2022;13:990953. doi:10.3389/fendo.2022.990953
116. Trejo-Castro AI, Carrion-Alvarez D, Martinez-Torteya A, Rangel-Escareño C. A Bibliometric Review on Gut Microbiome and Alzheimer’s Disease Between 2012 and 2021. Front Aging Neurosci. 2022;14:804177. doi:10.3389/fnagi.2022.804177
117. Huang R, Zhang M, Lu Y, et al. Effects of intestinal microbes on rheumatic diseases: a bibliometric analysis. Front Microbiol. 2022;13:1074003. doi:10.3389/fmicb.2022.1074003
118. Sun HL, Feng Y, Zhang Q, et al. The Microbiome-Gut-Brain Axis and Dementia: a Bibliometric Analysis. Int J Environ Res Public Health. 2022;19(24):16549. doi:10.3390/ijerph192416549
119. Yan XY, Yao JP, Li YQ, et al. Global trends in research on miRNA-microbiome interaction from 2011 to 2021: a bibliometric analysis. Front Pharmacol. 2022;13:974741. doi:10.3389/fphar.2022.974741
120. Lv H, Wang Y, Gao Z, et al. Knowledge mapping of the links between the microbiota and allergic diseases: a bibliometric analysis (2002-2021). Front Immunol. 2022;13:1045795. doi:10.3389/fimmu.2022.1045795
121. Chai R, Tai Z, Zhu Y, Chai C, Chen Z, Zhu Q. Symbiotic microorganisms: prospects for treating atopic dermatitis. Expert Opin Biol Ther. 2022;22(7):911–927. doi:10.1080/14712598.2022.2089560
122. Dessinioti C, Katsambas A. Antibiotics and Antimicrobial Resistance in Acne: epidemiological Trends and Clinical Practice Considerations. Yale J Biol Med. 2022;95(4):429–443. doi:10.1016/j.jaad.2021.11.066
123. Li Z, Xia J, Jiang L, et al. Characterization of the human skin resistome and identification of two microbiota cutotypes. Microbiome. 2021;9(1):47. doi:10.1186/s40168-020-00995-7
124. Saccon TD, Nagpal R, Yadav H, et al. Senolytic Combination of Dasatinib and Quercetin Alleviates Intestinal Senescence and Inflammation and Modulates the Gut Microbiome in Aged Mice. J Gerontol a Biol Sci Med Sci. 2021;76(11):1895–1905. doi:10.1093/gerona/glab002
125. Boyajian JL, Ghebretatios M, Schaly S, Islam P, Prakash S. Microbiome and Human Aging: probiotic and Prebiotic Potentials in Longevity. Skin Health Cell Senescence Nutrients. 2021;13(12):56.
126. Kim G, Kim M, Kim M, et al. Spermidine-induced recovery of human dermal structure and barrier function by skin microbiome. Commun biol. 2021;4(1):231. doi:10.1038/s42003-020-01619-4
127. Sun T, Niu X, He Q, Chen F, Qi RQ. Artificial Intelligence in microbiomes analysis: a review of applications in dermatology. Front Microbiol. 2023;14:1112010. doi:10.3389/fmicb.2023.1112010
128. Yilmaz A, Göktay F, Varol R, Gencoglan G, Uvet H. Deep convolutional neural networks for onychomycosis detection using microscopic images with KOH examination. Mycoses. 2022;65(12):1119–1126. doi:10.1111/myc.13498
129. Capone KA, Dowd SE, Stamatas GN, Nikolovski J. Diversity of the human skin microbiome early in life. J Invest Dermatol. 2011;131(10):2026–2032. doi:10.1038/jid.2011.168
130. Barnard E, Shi B, Kang D, Craft N, Li H. The balance of metagenomic elements shapes the skin microbiome in acne and health. Sci Rep. 2016;6:39491. doi:10.1038/srep39491
131. Zeeuwen PL, Boekhorst J, van den Bogaard EH, et al. Microbiome dynamics of human epidermis following skin barrier disruption. Genome Biol. 2012;13(11):R101. doi:10.1186/gb-2012-13-11-r101
132. Shu M, Wang Y, Yu J, et al. Fermentation of Propionibacterium acnes, a commensal bacterium in the human skin microbiome, as skin probiotics against methicillin-resistant Staphylococcus aureus. PLoS One. 2013;8(2):e55380. doi:10.1371/journal.pone.0055380
133. McDowell A, Barnard E, Nagy I, et al. An expanded multilocus sequence typing scheme for Propionibacterium acnes: investigation of ‘pathogenic’, ‘commensal’ and antibiotic resistant strains. PLoS One. 2012;7(7):e41480. doi:10.1371/journal.pone.0041480
134. Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207–214. doi:10.1038/nature11234
135. Naik S, Bouladoux N, Wilhelm C, et al. Compartmentalized control of skin immunity by resident commensals. Science. 2012;337(6098):1115–1119. doi:10.1126/science.1225152
136. Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26(19):2460–2461. doi:10.1093/bioinformatics/btq461
137. Iwase T, Uehara Y, Shinji H, et al. Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature. 2010;465(7296):346–349. doi:10.1038/nature09074
138. Kennedy EA, Connolly J, Hourihane JO, et al. Skin microbiome before development of atopic dermatitis: early colonization with commensal staphylococci at 2 months is associated with a lower risk of atopic dermatitis at 1 year. J Allergy Clin Immunol. 2017;139(1):166–172. doi:10.1016/j.jaci.2016.07.029
139. Paller AS, Kong HH, Seed P, et al. The microbiome in patients with atopic dermatitis. J Allergy Clin Immunol. 2019;143(1):26–35. doi:10.1016/j.jaci.2018.11.015
140. Dréno B, Pécastaings S, Corvec S, Veraldi S, Khammari A, Roques C. Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol. 2018;32 Suppl 2:5–14.
141. Lai Y, Cogen AL, Radek KA, et al. Activation of TLR2 by a small molecule produced by Staphylococcus epidermidis increases antimicrobial defense against bacterial skin infections. J Investigative Dermatol. 2010;130(9):2211–2221. doi:10.1038/jid.2010.123
142. Kong HH. Skin microbiome: genomics-based insights into the diversity and role of skin microbes. Trends Mol Med. 2011;17(6):320–328. doi:10.1016/j.molmed.2011.01.013
143. Bieber T. Atopic dermatitis. N Engl J Med. 2008;358(14):1483–1494. doi:10.1056/NEJMra074081
144. Wang Q, Garrity GM, Tiedje JM, Cole JR. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73(16):5261–5267. doi:10.1128/AEM.00062-07
145. Sanford JA, Gallo RL. Functions of the skin microbiota in health and disease. Semin Immunol. 2013;25(5):370–377. doi:10.1016/j.smim.2013.09.005
146. Chen YE, Fischbach MA, Belkaid Y. Skin microbiota-host interactions. Nature. 2018;553(7689):427–436. doi:10.1038/nature25177
147. Kong HH, Segre JA. The Molecular Revolution in Cutaneous Biology. Invest Skin Microbiome J Invest Dermatol. 2017;137(5):e119–e122. doi:10.1016/j.jid.2016.07.045
148. Oh J, Conlan S, Polley EC, Segre JA, Kong HH. Shifts in human skin and nares microbiota of healthy children and adults. Genome Med. 2012;4(10):77. doi:10.1186/gm378
149. Lomholt HB, Kilian M. Population genetic analysis of Propionibacterium acnes identifies a subpopulation and epidemic clones associated with acne. PLoS One. 2010;5(8):e12277. doi:10.1371/journal.pone.0012277
150. Belkaid Y, Segre JA. Dialogue between skin microbiota and immunity. Science. 2014;346(6212):954–959. doi:10.1126/science.1260144
151. Fierer N, Lauber CL, Zhou N, McDonald D, Costello EK, Knight R. Forensic identification using skin bacterial communities. Proc Natl Acad Sci U S A. 2010;107(14):6477–6481. doi:10.1073/pnas.1000162107
152. Chng KR, Tay AS, Li C, et al. Whole metagenome profiling reveals skin microbiome-dependent susceptibility to atopic dermatitis flare. Nat Microbiol. 2016;1(9):16106. doi:10.1038/nmicrobiol.2016.106
153. Findley K, Oh J, Yang J, et al. Topographic diversity of fungal and bacterial communities in human skin. Nature. 2013;498(7454):367–370. doi:10.1038/nature12171
154. Nakatsuji T, Chiang HI, Jiang SB, Nagarajan H, Zengler K, Gallo RL. The microbiome extends to subepidermal compartments of normal skin. Nat Commun. 2013;4:1431. doi:10.1038/ncomms2441
155. Meisel JS, Hannigan GD, Tyldsley AS, et al. Skin Microbiome Surveys Are Strongly Influenced by Experimental Design. J Invest Dermatol. 2016;136(5):947–956. doi:10.1016/j.jid.2016.01.016
156. Lai YP, Lin CC, Liao WJ, Tang CY, Chen SC. CD4+ T cell-derived IL-2 signals during early priming advances primary CD8+ T cell responses. PLoS One. 2009;4(11):e7766. doi:10.1371/journal.pone.0007766
157. Christensen GJ, Brüggemann H. Bacterial skin commensals and their role as host guardians. Benef Microbes. 2014;5(2):201–215. doi:10.3920/BM2012.0062
158. Rosenthal M, Goldberg D, Aiello A, Larson E, Foxman B. Skin microbiota: microbial community structure and its potential association with health and disease. Infect Genet Evol. 2011;11(5):839–848. doi:10.1016/j.meegid.2011.03.022
159. Byrd AL, Deming C, Cassidy SKB, et al. Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis. Sci Transl Med. 2017;9(397):eaal4651. doi:10.1126/scitranslmed.aal4651
160. Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5):335–336. doi:10.1038/nmeth.f.303
161. Kong HH, Segre JA. Skin microbiome: looking back to move forward. J Invest Dermatol. 2012;132(3 Pt 2):933–939. doi:10.1038/jid.2011.417
162. Myles IA, Earland NJ, Anderson ED, et al. First-in-human topical microbiome transplantation with Roseomonas mucosa for atopic dermatitis. JCI Insight. 2018;3(9):e120608. doi:10.1172/jci.insight.120608
163. Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121–141. doi:10.1016/j.cell.2014.03.011
164. Alekseyenko AV, Perez-Perez GI, De Souza A, et al. Community differentiation of the cutaneous microbiota in psoriasis. Microbiome. 2013;1(1):31. doi:10.1186/2049-2618-1-31
165. Naik S, Bouladoux N, Linehan JL, et al. Commensal-dendritic-cell interaction specifies a unique protective skin immune signature. Nature. 2015;520(7545):104–108.
166. McMurdie PJ, Holmes S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS One. 2013;8(4):e61217. doi:10.1371/journal.pone.0061217
167. Schommer NN, Gallo RL. Structure and function of the human skin microbiome. Trends Microbiol. 2013;21(12):660–668. doi:10.1016/j.tim.2013.10.001
168. Oh J, Freeman AF, Comparative Sequencing Program NISC, et al. The altered landscape of the human skin microbiome in patients with primary immunodeficiencies. Genome Res. 2013;23(12):2103–2114. doi:10.1101/gr.159467.113
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





