Back to Journals » Open Access Emergency Medicine » Volume 11
Emergency Medical Services Providers’ Knowledge, Practices, And Barriers To Stroke Management
Authors Li T, Munder SP, Chaudhry A, Madan R, Gribko M, Arora R
Received 22 August 2019
Accepted for publication 23 October 2019
Published 15 November 2019 Volume 2019:11 Pages 297—303
DOI https://doi.org/10.2147/OAEM.S228240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Timmy Li,1 Sneh Preet Munder,2 Anisha Chaudhry,2 Rima Madan,2 Michele Gribko,2 Rohan Arora3
1Department of Emergency Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Manhasset, NY 11030, USA; 2Department of Neurology, North Shore University Hospital, Manhasset, NY 11030, USA; 3Department of Neurology, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Manhasset, NY 11030, USA
Correspondence: Timmy Li
Department of Emergency Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, 300 Community Drive, Manhasset, NY 11030, USA
Tel +1 516 562 1513
Fax +1 516 562 3680
Email [email protected]
Purpose: Many strokes are not recognized by emergency medical services (EMS) providers and many providers do not prenotify emergency departments (EDs) of incoming stroke patients. The objectives of this project were to survey EMS providers to (1) assess knowledge of prehospital care related to stroke identification, time window for intravenous tissue plasminogen activator (IV tPA) administration, and comprehensive stroke centers in our health system, (2) gain insight from EMS providers regarding barriers to providing prenotification, information they provide for a prenotification, and optimal methods of providing feedback, and (3) provide EMS providers with stroke care and management information.
Methods: A survey was administered to EMS providers at four hospital EDs. The survey included questions related to knowledge of prehospital stroke care and barriers to providing prenotification. EMS providers were also provided a one-page flyer with information related to prehospital stroke care. Descriptive statistics were used to describe results.
Results: Of 301 EMS providers surveyed, 96.0% report that they use the Cincinnati Prehospital Stroke Scale to identify stroke, and 11.0% correctly identified the time window for IV tPA administration for acute ischemic stroke as within 4.5 hrs from the last known well time. The majority (82.7%) correctly identified the comprehensive stroke center in our health system. Barriers to providing prenotification included short transport time (40.5%), information being lost in dispatch (39.5%), and not having direct communication with ED staff (30.2%). Most reported wanting to receive feedback on the stroke patients they transported (93.7%), and 49.5% reported that the optimal method of providing feedback is via a mobile application.
Conclusion: Deficits in stroke care knowledge among EMS providers were identified. Short transport time, inability to communicate with ED staff, and information lost in dispatch were cited as barriers to providing prenotification. Most EMS providers desire real-time feedback regarding patients via a mobile application.
Keywords: emergency medical services, prehospital care, stroke, neurology
Introduction
Stroke is the fifth leading cause of death and a leading cause of long-term disability among adults in the United States.1 Intravenous tissue plasminogen activator (IV tPA) needs to be administered within 4.5 hrs of the last known well time, and earlier treatmentis associated with improved patient outcomes.2–8 Early recognition, accurate emergency medical services (EMS) dispatch, rapid EMS transport,9 and stroke team activation have helped shorten door-to-IV tPA time, but EMS prenotification of stroke still remains crucial in saving time to treat a stroke patient. EMS prenotification allows the emergency department (ED) and hospital staff to prepare for the patient’s arrival so that appropriate care can be initiated promptly. Nationally, the proportion of ischemic stroke patients receiving IV tPA remains low, with estimates ranging from 1% to 15%,2–7 most of which are due to not being able to reach an acute stroke-ready hospital within the narrow therapeutic window.
Many strokes are not recognized by EMS providers in the prehospital setting; one study found that EMS providers did not recognize a stroke in approximately 42% of patients with a hospital discharge diagnosis of stroke.10 Nationally, EMS providers provide prenotification for approximately 67% of acute stroke patients.11 Without a prenotification from EMS, assessment and care of the acute stroke patient in the ED may be delayed, which may make them ineligible for IV tPA therapy. Therefore, much work remains to be done to increase the proportion of EMS providers providing prenotification for suspected stroke patients, thereby increasing the proportion of patients receiving IV tPA.
Reasons for lack of stroke recognition and prenotification by EMS providers remain unclear. Potential reasons include lack of knowledge, failure to use stroke screening tools, and/or barriers to providing prenotification. Therefore, the purpose of this quality improvement project was to survey EMS providers to (1) assess EMS providers’ knowledge of prehospital stroke care related to stroke identification, the time window for IV tPA administration, and comprehensive stroke centers in our health system, (2) gain insight from EMS providers regarding barriers to providing prenotification, information they provide for a prenotification, and optimal methods of providing feedback, and (3) provide EMS providers with information related to stroke care and management.
Materials And Methods
Project Design
This was a quality improvement project conducted at the ED of four hospitals in New York State affiliated with Northwell Health between June 2018 and August 2018. Our health system’s Institutional Review Board determined that this was a quality improvement project and determined that obtaining informed consent was not required.
Project Setting And Population
This project was conducted by surveying a convenience sample of individual EMS providers arriving at the ED of one of four hospitals (Table 1) within the Northwell Health system. North Shore University Hospital, located in Manhasset, New York (a hamlet in Nassau County, New York, on the outskirts of New York City) is a 738-bed tertiary care facility, a Joint Commission-certified Comprehensive Stroke Center, and cares for approximately 90,000 patients in the ED per year. Long Island Jewish Medical Center, located in New Hyde Park, New York is a 1025-bed tertiary care facility with an ED volume of approximately 100,000 patients per year. Long Island Jewish Forest Hills Hospital, located in Forest Hills, New York is a 312-bed community hospital and cares for approximately 50,000 patients in the ED per year. Lenox Hill Hospital, located in Manhattan, New York is a 632-bed tertiary care facility with an ED volume of approximately 58,000 patients per year. Although all four of these hospitals are affiliated with the Northwell Health system, patients arriving by any ambulance service, regardless of affiliation, are accepted in the EDs.
 |
Table 1 Survey Administration Sites And Characteristics |
The New York City area uses a tiered response EMS system, comprised of basic life support ambulances, staffed by Emergency Medical Technicians, and advanced life support ambulances, staffed by Paramedics. The EMS system in New York City is controlled by the Fire Department of New York Bureau of EMS. Approximately two-thirds of all ambulances in New York City are Fire Department of New York Bureau of EMS municipal ambulances and approximately one-third are hospital-based ambulances that work in conjunction with the Fire Department of New York Bureau of EMS. Private and volunteer ambulance services also supplement the EMS system in New York City. Similarly, in Nassau County, EMS is provided by a combination of municipal ambulances from the Nassau County Police Department Emergency Ambulance Bureau, hospital-based ambulance services, private ambulance services, and numerous volunteer EMS agencies. Each ambulance agency has its own mechanism for its EMS providers to communicate with a medical control physician for advice and orders when necessary.
Although EMS providers in the New York City and Nassau County areas may be affiliated with various agencies (municipal, hospital-based, private, and volunteer agencies, or a combination of agencies), all EMS providers are certified by the New York State Department of Health. EMS providers in the New York City and Nassau County area also follow uniform treatment and assessment protocols for stroke. In addition to obtaining the required EMS certification through the New York State Department of Health, some EMS providers may also choose to become certified through the National Registry of Emergency Medical Technicians, although this is not a requirement to practice in the New York City and Nassau County areas. Further, specific EMS agencies and hospitals may also offer additional stroke education through continuing medical education events, such as conferences and case studies. For example, the Northwell Health system offers approximately four stroke educational events per year, including an annual EMS award dinner symposium, an annual stroke conference, and lectures, with topics specifically related to prehospital stroke management, prenotification, hospital processes and procedures to treat large vessel occlusion or severe strokes beyond IV tPA, capabilities of primary stroke centers vs comprehensive stroke centers, and the impact of prehospital care on stroke patient outcomes. All EMS providers are welcomed to attend these educational events, but attendance is optional.
EMS Protocol For Suspected Stroke
Per New York State EMS protocol, at the time this survey was administered, EMS providers are first instructed to assess suspected stroke patients using the Cincinnati Prehospital Stroke Scale, which includes assessing for facial droop, arm drift, and abnormal speech. If there are any positive findings, EMS providers are to establish the time of symptom onset. Lastly, EMS providers are expected to transport the patient to the nearest New York State Department of Health designated Stroke Center, unless the patient is in cardiac arrest, the patient has other conditions that warrant transport to another appropriate ED, the time of symptom onset exceeds 5 hrs, or a medical control physician directs otherwise. All four hospitals in which the survey was administered are the New York State Department of Health designated Stroke Centers capable of administering IV tPA. Further, all EMS providers in New York State have received education regarding the importance of providing prenotification to the ED of incoming stroke patients.
Survey Administration
Summer volunteers staffed the ED of the four hospitals and administered a voluntary survey to a convenience sample of EMS providers (Emergency Medical Technicians and Paramedics) arriving at the ED. Although there may be two to four EMS providers on a single crew, all EMS providers were surveyed individually as individual provider practices and knowledge regarding stroke management may differ. All summer volunteers received training on how to administer the survey by the senior author (R.A.). The survey was specifically designed by a multidisciplinary team of authors for this project, and asked EMS providers about methods they use to identify stroke, information they provide for prenotification, how often they prenotify hospital EDs of an incoming suspected stroke patient, barriers to providing prenotification, whether they would like to receive feedback about their stroke patients, how they would like to receive feedback, time window for IV tPA administration, and comprehensive stroke centers in the Northwell Health system. After the survey was completed, EMS providers were provided with a one-page flyer with the correct answers to the survey questions and general information about stroke care and management. The one-page flyer also highlighted the fact that “time is brain”, that prenotification may improve patients’ long-term outcomes, and that the prenotification should include the patient’s last known well time in addition to findings of the Cincinnati Prehospital Stroke Scale assessment.
Data Analysis
Descriptive statistics were used to describe survey responses. Frequencies and proportions were used to describe categorical variables. Responses to open-ended questions were grouped and described using frequencies and proportions.
Results
A total of 301 EMS providers were surveyed; 45.5% were surveyed at North Shore University Hospital, 32.9% at Long Island Jewish Medical Center, 18.6% at Long Island Jewish Forest Hills Hospital, and 3.0% at Lenox Hill Hospital. EMS providers in our sample were affiliated with 25 different EMS agencies; the majority (41.2%) were affiliated with Northwell Health, 29.6% were affiliated with the Fire Department of New York, and 29.2% were affiliated with other EMS agencies (Table 2).
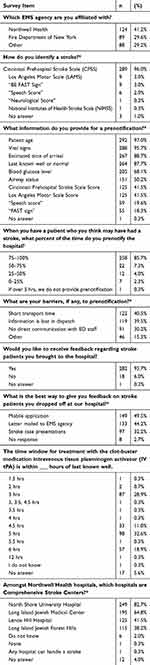 |
Table 2 Summary Of Survey Responses (n = 301) |
As shown in Table 2, the Cincinnati Prehospital Stroke Scale was the most commonly used method to identify stroke (96.0%), but EMS providers also reported using other methods, including the Los Angeles Motor Scale (3.0%), “BE FAST sign” (3.0%), “Speech Score” (2.0%), and “Neurological Score” (0.3%). Only 28.9% and 11.0% of EMS providers correctly reported the time window for IV tPA administration as within 3 hrs and 4.5 hrs of the last known well time, respectively. Most (82.7%) of EMS providers correctly identified the Comprehensive Stroke Center in the Northwell Health system, but three other hospitals were also incorrectly identified as Comprehensive Stroke Centers by many EMS providers.
Many EMS providers (40.5%) cited short transport time as a barrier for providing prenotification. The inability to directly communicate with ED staff (30.2%) and information being lost in dispatch (40.5%) were also common barriers for providing prenotification. The majority of EMS providers (97.0%) reported that they provide the patient’s age, vital signs (95.7%), estimated time of arrival (88.7%), last know well time (88%), and blood glucose level (68.1%) when providing a prenotification.
Almost all EMS providers (93.7%) reported wanting to receive feedback about the stroke patients they transported, and the majority wanted to receive the feedback via a mobile application (49.5%), letter mailed to the EMS agency (44.2%), and stroke case presentations (32.2%).
Discussion
In this quality improvement project, we were able to survey and provide stroke care and management information to over 300 EMS providers affiliated with 25 different EMS agencies. We identified deficits in prehospital stroke care knowledge among EMS providers. Many EMS providers did not know the time window for IV tPA administration, and although over 80% of EMS providers correctly identified the Comprehensive Stroke Center in our health system, other hospitals were also incorrectly identified as a Comprehensive Stroke Center. The only prior survey study of EMS provider knowledge of stroke, we are aware of, is the study by Crocco et al published in 1999.12 This survey of 355 EMS providers in the United States found that most EMS providers were aware of the symptoms of stroke, but were unaware of the time window for IV tPA administration.12 These findings align with our results in that only a minority of EMS providers knew the time window for IV tPA administration. These findings indicate that EMS education regarding prehospital stroke care can be improved. Future work should focus on prehospital stroke care education to address deficits in knowledge. We feel that a rotation in stroke neurology within the paramedic curriculum would be particularly valuable for paramedic students. This rotation would allow them to appreciate the value of EMS providers providing prenotification of an incoming stroke patient and augment their knowledge of emergency stroke care.
We identified barriers to providing prenotification. The most commonly cited barrier to providing prenotification was short transport time. EMS providers may feel that it may not be worth the time and effort it takes to provide a prenotification for a patient with a short transport time, as they may be able to get to the ED quickly. However, regardless of the transport time, a stroke prenotification from EMS mobilizes ED and hospital resources in caring for an acute stroke patient. Therefore, no matter how short the transport time is, we believe that a prenotification should still be provided.
The inability to directly communicate with ED staff and consequently, having information being lost in communication were also cited as barriers to providing prenotification. In our region, prenotifications are provided to hospital EDs via EMS dispatch (EMS providers provide the prenotification to EMS dispatch and EMS dispatch relays the information to the hospital ED); there is no direct communication between EMS providers and ED staff. It is possible for EMS dispatch to misinterpret or mishear information from EMS providers and thus, provide the hospital ED with misinformation. Further, since there is no direct communication between the ED staff and EMS providers, it is not possible for ED staff to ask EMS providers clarifying questions or ask for more information. Therefore, EMS systems that follow a similar process should reexamine their prenotification processes. The communication between EMS providers and ED staff could be improved by eliminating the need to go through EMS dispatch to provide prenotifications. The direct communication between EMS providers and ED staff would reduce miscommunication.
Due to the nature of prehospital care, most EMS providers do not know about the final diagnoses and outcomes of their patients. Not surprisingly, 93.7% of the EMS providers we surveyed wanted to receive feedback on their patients and they would prefer to receive feedback via a mobile application. The study by Choi et al found that hospital provision of feedback to EMS was associated with improved compliance with prehospital stroke protocols and documentation.13 Therefore, hospitals and EMS systems should implement methods of providing EMS providers with feedback about stroke patients.
Many EMS providers reported using the Cincinnati Prehospital Stroke Scale to screen for potential stroke (96.0%), which is the prehospital stroke screening tool taught to EMS providers in New York State. However, a few EMS providers also reported using unfamiliar tools, including the “Speech Score” (2.0%) and “Neurological Score” (0.3%).
In addition to assessing EMS providers’ knowledge of prehospital stroke care in this quality improvement project, we also provided EMS providers with information related to stroke care and management. A prior study found that a brief educational training for EMS providers resulted in improvements in EMS provider knowledge of prehospital stroke screening tools and triage protocols.14 We hope that the information we provided via the informational flyers is valuable to EMS providers; however, we do not have longitudinal data regarding the influence of these informational flyers on prehospital stroke care. We do not know whether this short-term informational initiative will increase the number of EMS prenotifications.
Limitations
There are a few limitations of this project to acknowledge. First, this quality improvement project was conducted at four hospitals within the same health system in one geographic region and thus, our results may not be generalizable to EMS systems in other regions. Although we surveyed EMS providers affiliated with numerous EMS agencies, EMS providers from other regions and states may have unique experiences and challenges. One may wonder whether the wide variety of responses to our survey questions may be due to a complex EMS system comprising many ambulance services with various affiliations. While it is true that there are numerous EMS agencies in New York State, this complexity is not unique to New York State; most states in the United States have numerous EMS agencies with various affiliations. Second, we were only able to administer the survey during the daytime. EMS providers who work overnight shifts have different levels of knowledge, experiences, and may encounter unique barriers to providing prenotification.
Conclusions
We identified deficits in prehospital stroke care knowledge among EMS providers, including the time window for IV tPA administration and comprehensive stroke centers in our health system. Short transport time, inability to communicate with ED staff directly, and information being lost in dispatch were cited as barriers to providing prenotification. Most EMS providers desire real-time feedback regarding their patients via a mobile application.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation. 2015;131(4):e29–e322. doi:10.1161/CIR.0000000000000152
2. Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke. 2011;42(7):1952–1955. doi:10.1161/STROKEAHA.110.612358
3. Miller DJ, Simpson JR, Silver B. Safety of thrombolysis in acute ischemic stroke: a review of complications, risk factors, and newer technologies. Neurohospitalist. 2011;1(3):138–147. doi:10.1177/1941875211408731
4. Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology. 2001;56(8):1015–1020. doi:10.1212/WNL.56.8.1015
5. Deng YZ, Reeves MJ, Jacobs BS, et al. IV tissue plasminogen activator use in acute stroke: experience from a statewide registry. Neurology. 2006;66(3):306–312. doi:10.1212/01.wnl.0000196478.77152.fc
6. Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;7:Cd000213.
7. Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004;33(2):116–121. doi:10.1093/ageing/afh064
8. Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–1935. doi:10.1016/S0140-6736(14)60584-5
9. Puolakka T, Kuisma M, Lankimaki S, et al. Cutting the prehospital on-scene time of stroke thrombolysis in Helsinki: a prospective interventional study. Stroke. 2016;47(12):3038–3040. doi:10.1161/STROKEAHA.116.014531
10. Abboud ME, Band R, Jia J, et al. Recognition of stroke by EMS is associated with improvement in emergency department quality measures. Prehosp Emerg Care. 2016;20(6):729–736.
11. Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5(4):514–522. doi:10.1161/CIRCOUTCOMES.112.965210
12. Crocco TJ, Kothari RU, Sayre MR, Liu T. A nationwide prehospital stroke survey. Prehosp Emerg Care. 1999;3(3):201–206. doi:10.1080/10903129908958937
13. Choi B, Tsai D, McGillivray CG, Amedee C, Sarafin JA, Silver B. Hospital-directed feedback to emergency medical services improves prehospital performance. Stroke. 2014;45(7):2137–2140. doi:10.1161/STROKEAHA.114.005679
14. DiBiasio EL, Jayaraman MV, Oliver L, et al. Emergency medical systems education may improve knowledge of pre-hospital stroke triage protocols. J Neurointerv Surg. 2018. doi:10.1136/neurintsurg-2018-014108
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
