Back to Journals » Lung Cancer: Targets and Therapy » Volume 7
Electromagnetic navigation bronchoscopy: clinical utility in the diagnosis of lung cancer
Authors Seijo LM
Received 29 July 2016
Accepted for publication 12 September 2016
Published 12 October 2016 Volume 2016:7 Pages 111—118
DOI https://doi.org/10.2147/LCTT.S98643
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Pan-Chyr Yang
Luis M Seijo
Pulmonary Department, Instituto de Investigación Sanitaria-Fundación Jimenez Díaz-Centro de Investigación Biomedica en Red Enfermedades Respiratorias, Madrid, Spain
Abstract: Electromagnetic navigation bronchoscopy (ENB) is one of several technological advances which have broadened the indications for bronchoscopy in the diagnostic workup of lung cancer. The technique facilitates bronchoscopic sampling of peripheral pulmonary nodules as well as mediastinal lymph nodes, although wide availability and expertise in endobronchial ultrasonography has limited its application in routine clinical practice to the former. ENB in this setting is quite versatile and may be considered an established alternative to more invasive techniques, especially in selected patients with underlying pulmonary disease or comorbidities at high risk for complications from computer topography-guided fine needle aspiration or surgical resection. Nodule sampling may be performed with a variety of instruments, including forceps, cytology brushes, and transbronchial needles. Although samples are generally small, they are often suitable for molecular analysis.
Keywords: lung cancer, ENB, electromagnetic navigation, bronchoscopy, diagnosis, pulmonary nodule
Introduction
Solitary pulmonary nodules (SPNs) are often found incidentally on chest radiographs or computed tomography (CT) scans and are quite common. As many as 150,000 pulmonary nodules are diagnosed every year in the US.1 The advent of lung cancer screening with low-dose CT implies that clinicians will face a virtual avalanche of nodules in need of workup, albeit few of them will merit invasive interventions.2 Management of the SPNs generally depends on the clinical suspicion of cancer. While most small nodules can be followed by imaging alone, those ranging in size between 10 mm and 30 mm in diameter are often considered too large for watchful waiting.
The choice of diagnostic procedure depends on patient preference and practitioner expertise, available resources, as well as local biases. Surgery is often recommended for low- to intermediate-risk patients with a high clinical suspicion of cancer in order to avoid the pitfalls of minimally invasive diagnostic tests.3 Many practitioners feel strongly that opting for immediate surgical resection may be the best choice for many patients with resectable nodules because the negative predictive value of a benign diagnosis obtained by minimally invasive techniques is not acceptable in this setting. However, although surgical mortality is low for patients with SPNs and the procedure is diagnostic for the vast majority of cases, only 55%–68% of surgically resected nodules turn out to be malignant, reflecting the shortcomings of a “straight to surgery” approach.4,5 An aggressive management strategy may lead to many invasive procedures for benign nodules. Furthermore, patients with suspicious nodules are often older and heavy smokers with underlying COPD, cardiovascular disease, or other tobacco-related comorbidities, and surgery in these patients is never straightforward.
CT-guided transthoracic needle aspiration (TTNA) and core needle biopsy are the minimally invasive alternatives to bronchoscopy or surgery. Percutaneous biopsy is the gold standard for the minimally invasive diagnosis of peripheral lesions, and remains the most common approach to the intermediate-sized pulmonary nodule with a diagnostic accuracy of 90%.6 The sensitivity of TTNA for lung cancer is 80%–95% and the specificity is 50%–88%.1 However, diagnostic yields reported by individual studies vary from 62% to 99%.7 The biggest drawback is the risk of pneumothorax, with a recent study of more than 15,000 procedures reporting a 15% pneumothorax rate and a 1% incidence of significant bleeding.8 Several factors including needle and nodule size, a history of smoking, and patient age have been linked to the procedural risk of pneumothorax.9 This risk is 11 times greater if the nodule measures less than 20 mm and increases with an increase in the distance from the nodule to the pleural surface. Another drawback of TTNA, common to all minimally invasive techniques, is a modest negative predictive value which often leads to surgery despite a benign diagnosis.10 As many as 68% of patients undergoing surgery with a benign diagnosis obtained by TTNA have cancer.11
The role of conventional bronchoscopy in lung cancer
Recent advances in endobronchial ultrasonography have catapulted bronchoscopy to its current preeminent role in the diagnosis and staging of patients with advanced lung cancer. Conventional bronchoscopy, however, faces many limitations in the workup of pulmonary nodules. The technique often relies on blind or fluoroscopically guided techniques such as bronchoalveolar lavage and use of cytology brushes, needle aspiration, or forceps in order to biopsy a given nodule. Flexible bronchoscopy is invaluable in the diagnosis of endoscopically visible or diffuse disease, including lymphangitic spread of tumors in the lung, but successful sampling of pulmonary nodules depends on the size and location of the nodule and local expertise. Furthermore, diagnostic bronchoscopes have small caliber working channels, so diagnostic samples are often small. Crush artifacts and the lack of rapid onsite sample evaluation at many centers can also limit the diagnostic yields.
Major advantages of conventional bronchoscopy in the workup of patients with suspected lung cancer include its excellent safety profile and wide availability. Serious complications are rare and generally do not exceed 1%. In a recent study of more than 20,000 procedures, only three deaths were reported.12 Pneumothorax rates are much lower than those reported following TTNA, often well below 5%, with only a handful of patients requiring chest tube placement.13 That notwithstanding, patients with suspected peripheral lung cancer must undergo transbronchial biopsies, a technique which is responsible for 73% of all serious complications related to the procedure.14
Unfortunately, despite its safety profile, conventional bronchoscopy has a poor diagnostic yield for small peripheral lesions. Nodule size and location are key factors, but since bronchoscopy mandates an endobronchial approach, the relationship of the lesion to the bronchial tree is particularly important. Current American College of Chest Physicians (ACCP) guidelines do not recommend conventional bronchoscopy for the evaluation of small pulmonary nodules unless a bronchus sign is clearly present.15 Since a benign diagnosis is often nonspecific and unreliable, the prevalence of cancer in a given practice setting is also paramount and quite variable. Not surprisingly, reported diagnostic yields range from 18% to 62%.16,17 Large malignant nodules located close to the hilum are more amenable to the conventional bronchoscopic approach.18,19 Yields may improve with the use of fluoroscopy, but lesions <2 cm in diameter are often missed. Furthermore, fluoroscopy is not only cumbersome, but requires specific radiation safety measures and training, more space than is often available in a standard bronchoscopy suite, and prolongs the procedure.
Conventional bronchoscopy may be reserved for the perioperative evaluation of the patient with limited-stage peripheral lung cancer. Spanish thoracic society guidelines recommend conventional bronchoscopy be performed in a selected group of patients with suspicious pulmonary nodules who are good surgical candidates.20 A prospective European study found that preoperative bronchoscopy in this setting has an overall diagnostic yield of 41%, and may contribute to changes in surgical strategy in a significant number of cases.21 However, a recent retrospective study reported that little can be expected from preoperative bronchoscopy as fewer than 8% of the procedures lead to unexpected findings,22 particularly in patients with ground-glass opacities or small non-solid nodules.23
Finally, lung cancer screening poses a new challenge to the conventional bronchoscope, since lung cancers detected in this setting are often less than 2 cm in size. van´t Westeinde et al recently reported yields of flexible bronchoscopy in the evaluation of pulmonary nodules detected in the context of lung cancer screening.24 Mean nodule size in that study did not exceed 15 mm and the overall sensitivity of bronchoscopy was a disappointing 13.5%. More importantly, surgical resection was necessary in 95% of the patients, a strong argument in favor of a “straight to surgery” strategy (Table 1).
Electromagnetic navigation bronchoscopy
Electromagnetic navigation bronchoscopy (ENB) was developed in order to overcome the shortcomings of conventional bronchoscopy in the periphery of the lung. ENB is indicated in the diagnostic workup of peripheral pulmonary nodules and mediastinal adenopathy, although widespread use of endobronchial ultrasound has rendered its use in the central airways anecdotal. The procedure is more time consuming than conventional bronchoscopy, including preprocedural planning and simulation as well as the actual intervention, but probably safer, limiting the risk of pneumothorax and bleeding. Current users of this technology rely on ENB for high-risk patients with small- to intermediate-size nodules as an alternative to surgery or CT-guided TTNA. Contraindications to ENB are similar to those described for conventional bronchoscopy in centers relying on conscious sedation. Some centers perform ENB under general anesthesia and must therefore take this into account when selecting high-risk patients for the procedure.
ENB is based on a Global Positioning System-like framework, but instead of using a satellite signal, it employs an electromagnetic field in order to pinpoint the precise location of a steerable probe inside the patient’s chest wall. The ENB system consists of four basic components: the aforementioned electromagnetic field and steerable probe, also known as the locatable guide, an extended working channel (EWC), and licensed software. The procedure may be performed under conscious sedation or general anesthesia, but seldom in a fully conscious patient because constant motion, rapid breathing, and coughing can preclude adequate navigation and/or sampling, while the length of the procedure will otherwise put patient tolerance to the test. We generally perform ENB under conscious sedation with a combination of midazolam and fentanyl at Fundación Jiménez Díaz University Hospital.
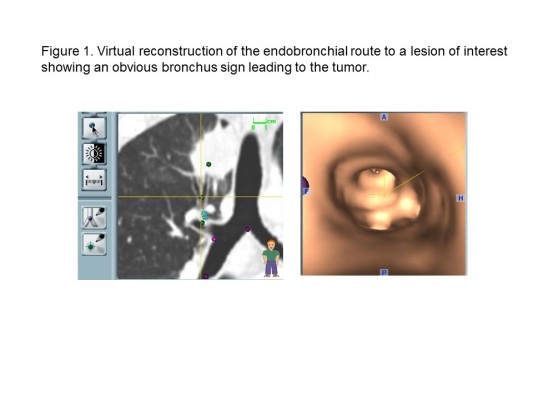
Procedure planning
All ENB procedures require careful planning. Data from a recent chest CT scan with specific slice thickness and intervals are saved on a disc and introduced in the planning software module of a laptop computer. During planning, the software generates a virtual bronchoscopic reconstruction of the patient’s airways and axial, coronal, and sagittal images of the patient’s chest which the operator must navigate in order to generate a number of reference points and targets. Once planning is complete, a file containing all necessary information is saved on a USB stick which is then inserted in the bronchoscopy suite’s hardware in order to download its contents and perform the ENB procedure. Virtual reference points selected during planning will be registered either manually or automatically during ENB by advancing the steerable probe (Figure 1). Generally, well-known reference points such as the main and lobar carinas are chosen and although the risk of pneumothorax is quite low, usually only targets in one lung are selected for a given procedure. Mediastinal lymph nodes may also be selected, and these may be located on either side of the mediastinum.
Planning allows for the operator to study the airways leading to a given target and advance through them in a virtual simulation in order to prepare for the procedure. The planning software may be used even if the procedure is planned as a conventional bronchoscopy, since the cost of ENB should discourage its use when a lesion is accessible using standard techniques.
ENB procedure
The ENB procedure, including topical airway anesthesia and conscious sedation, begins as a routine bronchoscopy. Careful monitoring of vital signs, telemetry, and oxygen saturation is of paramount importance. Since the operator’s attention will be devoted almost entirely to navigation, it is imperative that one or more assistants be in charge of patient monitoring and sample processing during ENB. The ENB procedure begins following routine airway inspection by inserting the steerable probe through the EWC of the bronchoscope. The EWC is a small flexible catheter which can reach the periphery of the lung and is designed to accommodate the steerable probe and sampling instruments. We generally wait to deploy the probe until a conventional inspection is complete, because patient tolerance of the procedure can be gauged in this way and incidental findings may alter procedure objectives. Furthermore, once the probe is connected to the hardware, it is permanently assigned to the patient in the room and cannot be cleaned or reused, so making sure the patient will tolerate the procedure is just common sense.
Once the steerable probe is inserted and advanced, registration begins. While current software upgrades rely on automatic registration, which is accomplished by advancing the steerable probe gently past preselected virtual reference points, manual registration remains an option. The latter alerts the operator to the so-called divergence error, also known as average fiducial target registration error (AFTRE), which estimates the divergence between virtual and actual targets and registration points. AFTREs of 4 mm are considered optimal, although ENB can be performed irrespective of the AFTRE, as long as the potential for missing the target is taken into account. Although automatic registration does not provide an estimate of registration error, the ENB software will not allow the procedure to continue unless the AFTRE is low enough for ENB to be performed safely and accurately.
Once registration is complete, the EWC and the probe are simultaneously guided through the airways following a computer-generated pathway complete with individual way points. Advancing the probe can also be a trial and error process in which the operator relies on virtual sagittal, coronal, and axial views together with a screen indicating the distance to the target and an icon representing the probe’s position. The ENB hardware relies on the selected reference points and information from three external sensors placed on the patient’s chest wall in order to triangulate the location of the steerable probe and make recommendations regarding navigation to the selected target(s). The appropriate turns are made using a hand-held, telescopic device and an EWC with a curved tip catheter design similar to those used in coronary angiography procedures. Feedback from the software is constant and in real time, including information regarding the probe’s pitch, roll, and direction. Once the target is reached, the EWC is fixed in place and the probe removed in order to begin sampling (Figure 2).
The ENB EWC is large enough to accommodate most conventional sampling instruments, including forceps, cytology brushes, and needles. A protocolized sampling procedure was routinely followed in performing catheter aspiration first, followed by forceps biopsies, brushing and/or needle sampling, and finally a mini-lavage using the EWC and a 10 mL aliquot of sterile saline. Needle aspiration can be challenging in some locations because of the resistance met by the needle as it negotiates the turns made by the EWC en route to a given target. However, the advantage of the needle is evident, as it can penetrate the airway and reach beyond it in order to sample a nodule which does not invade the bronchi in its vicinity.
Since the information provided by the software is only reliable insofar as it was obtained from static images, any significant change in the position of the target and/or registration points resulting from coughing, rapid breathing, or a pneumothorax may lead to misinformation regarding the probe’s location and therefore limit diagnostic yield. Breathing can be a challenge when a lesion is close to the diaphragm or fissures leading to constant target excursion and uncertainty regarding the exact location of the probe, since the ENB’s software cannot account for respiratory movement. It is common practice to check the sampling site by periodically reintroducing the probe in order to verify that the EWC has not been displaced or that a sudden unexpected inconsistency in the probe’s location has taken place. The latter can be an ominous warning that a pneumothorax has occurred and may be a reason to terminate the procedure, especially if the patient complains of chest discomfort.
ENB in lung cancer
Current ACCP guidelines recommend ENB for lesions which are hard to reach with the conventional bronchoscope in order to avoid unnecessary invasive tests if the equipment and expertise are available.7 Cost is an issue with ENB because the locatable guide and EWC are single-use only, and start-up costs are considerable. A recent cost-analysis study comparing ENB with TTNA found that ENB increased average costs by US$3,719 per patient.25 However, ENB is safer, avoiding chest tube placement in 6% of patients and minimizing other complications such as major bleeding and respiratory failure.25 The major advantage of ultrasound-guided bronchoscopy is that the ultrasound probe can be reused (Table 1).
ENB yields are highly dependent on the presence of a bronchus sign as evidenced by a landmark prospective study.26 The bronchus sign is more common in malignancies which tend to be spiculated and larger than benign nodules (>30 mm).27,28 A positive bronchus sign has also been found to be a strong predictor of diagnostic success for ultrasound-guided bronchoscopic sampling of peripheral lung nodules.29 Nodule location and size may also be important for ENB success.30–32
ENB is a safe procedure. The risk of pneumothorax is very low and chest tube placement is rare. A recent meta-analysis of more than 1,000 procedures found that ENB caused only 32 pneumothoraces and less than 20 patients required chest tube placement.33 Pneumothorax following TTNA is almost 10 times more common. Other complications such as major bleeding, arrhythmias, and death have not been reported or are exceedingly rare. Unfortunately, safety comes at a cost, since malignancy cannot be entirely excluded due to the low negative predictive value of the procedure (52.1%).33 The latter remains low when a benign diagnosis such as chronic or granulomatous inflammation is obtained mirroring the accrued experience with other minimally invasive diagnostic techniques such as TTNA. This shortcoming of ENB is clinically relevant precisely because ENB is often challenged to rule out cancer in a high-risk patient with a suspicious nodule (Figure 3).
The performance of ENB is clearly inferior to the gold standard of surgical resection. ENB’s pooled sensitivity for malignancy has been reported as 71% and accuracy for malignancy does not exceed 80%.33 Direct comparison of ENB with conventional or alternative navigational techniques is limited to a single trial assessing the yield of ENB compared to radial ultrasound probes.30 In that randomized trial, diagnostic yields of 59%, 69%, and 87.5% were reported for ENB, radial ultrasound probe, and the combination of both techniques, respectively. The combined procedure was statistically superior to either ENB or radial probe ultrasound as stand-alone interventions. Trials comparing conventional bronchoscopy with ultrasound probe-guided sampling of peripheral pulmonary nodules have shown the latter to be more sensitive, even for small lesions.34,35 Probe location and lesion size determine diagnostic yields with this technique, which faces many of the limitations ENB grapples with.36,37 A recent meta-analysis found that ultrasound-guided bronchoscopy has a pooled sensitivity and specificity of 73% and 100%, respectively, for the detection of lung cancer in peripheral nodules.38 The procedure is as safe as ENB with pneumothorax rates as low as 1%.34
ENB yields may improve using general anesthesia and rapid onsite evaluation.33,39 Better ENB yields have also been reported in recent studies suggesting that learning curves may have underestimated outcomes, although results from a multicenter registry found disappointing results with ENB in the diagnosis of peripheral lesions.40,41
Finally, it should be noted that ENB’s applications in lung cancer go beyond diagnosis. The procedure has been used for the accurate placement of fiducial markers in order to facilitate stereotactic radiation therapy treatments in selected patients with lung cancer.42 It has also been employed as a guide for endoscopic brachytherapy treatment of peripheral lesions in inoperable patients,43 and may be useful in order to mark small pulmonary nodules earmarked for resection using pleural dye.44 Furthermore, ENB has been shown to be an effective means of obtaining tissue samples for molecular analysis, including EGFR mutations and EML4-ALK translocations in lung tumors, proving its versatility and clinical value.45 Novel applications include placement of ablation probes in a target tumor and guidance of endobronchial ablation catheters for the minimally invasive treatment of lung cancer.46,47
Conclusion
The clinical utility of ENB in the diagnosis of lung cancer is well established, although it continues to be the subject of ongoing clinical studies. Patient and target selection continue to be the key variables influencing ENB yields and outcomes. Future applications of ENB in lung cancer go beyond diagnostics, with ongoing studies investigating its role in therapeutics, either as an aid to radiation therapy or as a guide for novel ablation catheters. Alternative guided bronchoscopic techniques such as ultrasound-guided bronchoscopy currently compete with ENB, although they face many of its shortcomings with the possible exception of cost and availability.
Disclosure
LS served as a paid consultant for Covidien, owner of Superdimension in 2013. The author reports no other conflicts of interest in this work.
References
Ost D, Fein AM, Feinsilver SH. Clinical practice. The solitary pulmonary nodule. N Engl J Med. 2003;348(25):2535–2542. | ||
The National Lung Screening Trial Research Team. Reduced lung cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. | ||
Gambhir SS, Shepherd JE, Shah BD, et al. Analytical decision model for the cost-effective management of solitary pulmonary nodules. J Clin Oncol. 1998;16(6):2113–2125. | ||
Bernard A. Resection of pulmonary nodules using video-assisted thoracic surgery. The Thorax Group. Ann Thorac Surg. 1996;61(1):202–204. | ||
Congregado Loscertales M, Girón Arjona JC, Jiménez Merchán R, et al. Usefulness of video-assisted thoracoscopy for the diagnosis of solitary pulmonary nodules. Arch Bronconeumol. 2002;38(9):415–420. | ||
Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer: summary of published evidence. Chest. 2003;123(Suppl 1):115S–128S. | ||
Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5):e142S–e165S. | ||
Weiner RS, Schwartz LM, Woloshin S, Welch HG. Population-based risk for complications after transthoracic needle biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med. 2011;155(3):137–144. | ||
Covey AM, Gandhi R, Brody LA, Getrajdman G, Thaler HT, Brown KT. Factors associated with pneumothorax and pneumothorax requiring treatment after percutaneous lung biopsy in 443 consecutive patients. J Vasc Interv Radiol. 2004;15(5):479–483. | ||
Zarbo RJ, Fenoglio-Preiser CM. Interinstitutional database for comparison of performance in lung fine-needle aspiration cytology. A College of American Pathologists Q-Probe Study of 5264 cases with histologic correlation. Arch Pathol Lab Med. 1992;116(5):463–470. | ||
Mitruka S1, Landreneau RJ, Mack MJ, et al. Diagnosing the indeterminate pulmonary nodule: percutaneous biopsy versus thoracoscopy. Surgery. 1995;118(4):676–684. | ||
Jin F, Mu D, Chu D, Fu E, Xie Y, Liu T. Severe complications of bronchoscopy. Respiration. 2008;76(4):429–433. | ||
Huang CT, Ruan SY, Liao WY, et al. Risk factors of pneumothorax after endobronchial ultrasound-guided transbronchial biopsy for peripheral lung lesions. PLoS One. 2012;7(11):e49125. | ||
Reinoso MA, Lechin A, Varon J, Wade L. Complications from flexible bronchoscopy in a training program. J Bronchology Interv Pulmonol. 1996;3:177–181. | ||
Rivera MP, Mehta AC; American College of Chest Physicians. Initial diagnosis of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(Suppl 3):131S–148S. | ||
Torrington KC, Kern JD. The utility of fiberoptic bronchoscopy in the evaluation of the solitary pulmonary nodule. Chest. 1993;104(4):1021–1024. | ||
Stringfield JT, Markowitz DJ, Bentz RR, Welch MH, Weg JG. The effect of tumor size and location on diagnosis by fiberoptic bronchoscopy. Chest. 1977;72(4):474–476. | ||
Chechani V. Bronchoscopic diagnosis of solitary pulmonary nodules and lung masses in the absence of endobronchial abnormality. Chest. 1996;109(3):620–625. | ||
Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest. 2000;117(4):1049–1054. | ||
Álvarez CJ, Bastarrika G, Disdier C, et al. Manejo del nódulo pulmonar solitario [Guideline on management of solitary pulmonary nodule]. Arch Bronconeumol. 2014;50:285–293. Spanish. | ||
Schwarz C, Schonfeld N, Bittner RC, et al. Value of flexible bronchoscopy in the pre-operative work-up of solitary pulmonary nodules. Eur Respir J. 2013;41(1):177–182. | ||
Zhang Y, Zhang Y, Chen S, et al. Is bronchoscopy necessary in the preoperative workup of a solitary pulmonary nodule? J Thorac Cardiovasc Surg. 2015;150(1):36–40. | ||
Jhun BW, Um SW, Suh GY, et al. Preoperative flexible bronchoscopy in patients with persistent ground-glass nodule. PLoS One. 2015;10(3):e0121250. | ||
van ’t Westeinde SC, Horeweg N, Vernhout RM, et al. The role of conventional bronchoscopy in the workup of suspicious CT scan screen-detected pulmonary nodules. Chest. 2012;142(2):377–384. | ||
Dale CR, Madtes DK, Fan VS, Gorden JA, Veenstra DL. Navigational bronchoscopy with biopsy versus computed tomography-guided biopsy for the diagnosis of a solitary pulmonary nodule: a cost-consequences analysis. J Bronchology Interv Pulmonol. 2012;19(4):294–303. | ||
Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a bronchus sign on CT imaging: results from a prospective study. Chest. 2010;138(6):1316–1321. | ||
Bilaçeroglu S, Kumcuoglu Z, Alper H, et al. CT bronchus sign-guided bronchoscopic multiple diagnostic procedures in carcinomatous solitary pulmonary nodules and masses. Respiration. 1998;65(1):49–55. | ||
Haro Estarriol M, Rubio Goday M, Vizcaya Sánchez M, Baldó Padró X, Casamitjá Sot MT, Sebastian Quetglás F. Biopsia pulmonar broncoscópica con fluoroscopia en lesiones pulmonares localizadas. Estudio de 164 casos [Bronchoscopic lung biopsy with fluoroscopy to study 164 localized pulmonary lesions]. Arch Bronconeumol. 2004;40:483–488. Spanish. | ||
Minezawa T, Okamura T, Yatsuya H, et al. Bronchus sign on thin-section computed tomography is a powerful predictive factor for successful transbronchial biopsy using endobronchial ultrasound with a guide sheath for small peripheral lung lesions: a retrospective observational study. BMC Med Imaging. 2015;15:21. | ||
Eberhardt R, Anantham D, Ernst A, Feller-Kopman D, Herth F. Multimodality bronchoscopic diagnosis of peripheral lung lesions: a randomised controlled trial. Am J Respir Crit Care Med. 2007;176(1):36–41. | ||
Jensen KW, Hsia DW, Seijo LM, et al. Multicenter experience with electromagnetic navigation bronchoscopy for the diagnosis of pulmonary nodules. J Bronchology Interv Pulmonol. 2012;19(3):195–199. | ||
Rivera P, Gonzalez J, Rabines A, et al. Predictors of diagnostic yield and complications of electromagnetic navigation bronchoscopy in peripheral pulmonary lesions. ATS International Conference Abstracts. ATS Journal. 2015:abstract 3731. | ||
Gex G, Pralong JA, Combescure C, Seijo L, Rochat T, Soccal PM. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration. 2014;87(2):165–176. | ||
Wang Memoli JS, Nietert PJ, Silvestri GA. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest. 2012;142(2):385–393. | ||
Paone G, Nicastri E, LucantoniG, et al. Endobronchial ultrasound-driven biopsy in the diagnosis of peripheral lung lesions. Chest. 2005;128(5):3551–3557. | ||
Yamada N, Yamazaki K, Kurimoto N, et al. Factors related to diagnostic yield of transbronchial biopsy using endobronchial ultrasonography with a guide sheath in small peripheral pulmonary lesions. Chest. 2007;132(2):603–608. | ||
Huang CT, Ho CC, Tsai YJ, Yang PC. Factors influencing visibility and diagnostic yield of transbronchial biopsy using endobronchial ultrasound in peripheral pulmonary lesions. Respirology. 2009;14(6):859–864. | ||
Steinfort DP, Khor YH, Manser RL, Irving LB. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: systematic review and meta-analysis. Eur Respir J. 2011;37(4):902–910. | ||
Brownback KR, Quijano F, Latham HE, Simpson SQ. Electromagnetic navigational bronchoscopy in the diagnosis of lung lesions. J Bronchology Interv Pulmonol. 2012;19(2):91–97. | ||
Lamprecht B, Porsch P, Wegleitner B, Strasser G, Kaiser B, Studnicka M. Electromagnetic navigation bronchoscopy (ENB): increasing diagnostic yield. Respir Med. 2012;106(5):710–715. | ||
Ost DE, Ernst A, Lei X, et al. Diagnostic yield and complications of bronchoscopy for peripheral lung lesions: results of the AQuIRE registry. Am J Respir Crit Care Med. 2016;193(1):68–77. | ||
Anantham D, Feller-Kopman D, Shanmugham LN, et al. Electromagnetic navigation bronchoscopy-guided fiducial placement for robotic stereotactic radiosurgery of lung tumors: a feasibility study. Chest. 2007;132(3):930–935. | ||
Harms W, Krempien R, Grehn C, Hensley F, Debus J, Becker HD. Electromagnetically navigated brachytherapy as a new treatment option for peripheral pulmonary tumors. Strahlenther Onkol. 2006;182(2):108–111. | ||
Krimsky WS, Minnich DJ, Cattaneo SM, et al. Thoracoscopic detection of occult indeterminate pulmonary nodules using bronchoscopic pleural dye marking. J Community Hosp Intern Med Perspect. 2014;4(1):23084. | ||
Ha D, Choi H, Almeida FA, et al. Histologic and molecular characterization of lung cancer with tissue obtained by electromagnetic navigation bronchoscopy. J Bronchology Interv Pulmonol. 2013;20(1):10–15. | ||
Narsule CK, Sales Dos Santos R, Gupta A, et al. The efficacy of electromagnetic navigation to assist with computed tomography-guided percutaneous thermal ablation of lung tumors. Innovations (Phila). 2012;7(3):187–190. | ||
Eberhardt R, Kahn N, Herth F. ‘Heat and Destroy’: bronchoscopic-guided therapy of peripheral lung lesions. Respiration. 2010;79(4):265–273. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.