Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Electrocardiogram Interpretation Competency Among Paramedic Students
Authors Mobrad A
Received 22 July 2020
Accepted for publication 6 August 2020
Published 19 August 2020 Volume 2020:13 Pages 823—828
DOI https://doi.org/10.2147/JMDH.S273132
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdulmajeed Mobrad
Prince Sultan College for EMS, King Saud University, Riyadh, Saudi Arabia
Correspondence: Abdulmajeed Mobrad Email [email protected]
Background: Electrocardiography is an essential emergency tool used in the pre-hospital setting. However, no studies have yet assessed electrocardiogram (ECG) interpretation among emergency medical services (EMS) students in Saudi Arabia. This study aimed to determine the ECG interpretation competency of paramedic students.
Methodology: Cross-sectional, single-center study, a pre-validated, self-administered, two-part questionnaire first created by Coll-Badell et al was used to assess the ECG interpretation competency of paramedic students at Prince Sultan College for Emergency Medical Services (PSCEMS) in King Saud University. Participant data were collected and analyzed to identify factors associated with improved competency.
Results: All students of PSCEMS were included, and 137 of 248 paramedic students completed the questionnaire (55% response rate); 88 students (64.2%) scored > 7.5 points, indicating competency in (ECG) interpretation. Factors such as grade point average (GPA) (> 3.5) and enrollment in cardiology and advanced cardiac life support courses were found to be significantly associated with competency (p< 0.001).
Conclusion: The majority of paramedic students were found to be competent in ECG interpretation. GPA and enrollment in cardiology and advanced cardiac life support courses were significantly associated with improved competency.
Keywords: electrocardiography, paramedic, emergency medical services, advanced cardiac life support, cardiology
Introduction
Electrocardiography is an essential emergency tool used in the pre-hospital setting. If utilized appropriately, it can be used to diagnose or guide the management of a variety of life-threatening conditions.1 Drew et al2 conducted a study to determine the electrocardiography utilization among emergency medical services (EMS) staff in managing patients with acute coronary syndrome (ACS); their results indicated that the increased use of pre-hospital electrocardiography reduced hospital treatment times. However, many studies concluded that there was underutilization of EMS systems by ACS patients.3–5 For those who experienced chest pain, early contact with health systems, particularly through prehospital medical providers, proved to have a beneficial role in revascularization following the cardiac ischemic event.6 Multiple studies found that obtaining a pre-hospital electrocardiogram (ECG) will reduce the door-to-balloon time and lead to faster reperfusion therapy with a lower adjusted risk of mortality among ACS patients.7–9 Moreover, prehospital ECGs were found to have an insignificant effect on transporting time but significant impact on improving patient outcomes.10,11 In addition to their clinical impact, prehospital ECGs were found to be cost-effective.12
However, the competency and knowledge level of the clinician interpreting the ECG is a critical factor. There is a reported lack of comprehensive ECG interpretation content in the curriculum medical education programs.13 Furthermore, O’Brien et al14 evaluated the training and assessment of ECG interpretation skills in the 3rd year internal medicine internship year across institutions and found that the undergraduate curriculum is lacking in terms of basic ECG interpretation competency. In addition, Stopa et al15 evaluated ECG interpretation skills among Polish medical, nursing, and paramedic students and found that the overall score was higher among medical students than nursing and paramedic students. These findings, in addition to other evidence, indicate that the ECG interpretation skills of undergraduate students are not satisfactory.16,17 ECG misinterpretation can lead to inappropriate diagnoses and clinical decisions. However, a limited number of studies have attempted to determine the size of the problem in Saudi Arabia. Alghamdi et al18 conducted a study to assess the frequency of ECG misinterpretation, address the nature of errors, and analyze the determinants of ECG interpretation accuracy among 6th year medical students and interns of Taif University, Taif, Saudi Arabia. They found that the overall performance of medical students and interns was moderate but that ECG interpretation can be improved by self-learning and providing organized educational courses on ECG. However, no studies have yet assessed ECG interpretation among EMS students in Saudi Arabia. Therefore, this study aimed to evaluate and identify the level of ECG interpretation of paramedic students as it related to their Grade Point Average (GPA) and other factors such advanced cardiac life support (ACLS) certification or attending related courses associated with ECG interpretation improvements and competency among EMS students of Prince Sultan Collage for EMS (PSCEMS), King Saud University, Saudi Arabia, Riyadh.
Materials and Methods
Design, Setting, and Enrollment
A cross-sectional descriptive design was used to determine the level of ECG interpretation among paramedic students at PSCEMS and identify the characteristics of high achievers in this skill via an online standardized research questionnaire. EMS students were enrolled from PSCEMS, King Saud University, Saudi Arabia, Riyadh. The PSCEMS Baccalaureate degree is 4 years; a cardiology course is provided at the beginning of the 2nd year, and the 4th year exclusively comprises an internship with no didactic or laboratory experience.
Convenience sampling was utilized to select the participants. All paramedic students and interns in PSCEMS were allowed an equal chance of inclusion in this study, and participation was voluntary. This study was approved by the institutional review board of King Saud University Medical City, and written informed consent was obtained from all participants. This study adhered to the principles of the Declaration of Helsinki 2013.
Assessment of ECG Interpretation Competency
A standardized research questionnaire created by Coll-Badell et al19 was used. This was a two-part questionnaire; the first part pertained to the profile of the respondents, such as age, grade point average (GPA), year of higher education and history of enrollment in extracurricular courses such as advanced cardiac life support (ACLS) or any other courses related to ECG and these courses’ mode of delivery. The second part comprised a 12-item survey (ten clinical questions and two theoretical questions) aiming to measure the level of competency of the respondents in ECG interpretation. Furthermore, Coll-Badell et al19 stated that a minimum score of 7.5 was needed to attain competence in ECG interpretation. The respondents who received a score of <7.5 failed the ECG competency evaluation. It was proven to be a valid and reliable instrument by the original authors, and it has also been used by other researchers; hence, there is no need to validate it further. Permission to reuse the questionnaire was cordially asked before the study was conducted.
Data Collection and Analysis
The data were gathered via direct, official emails from all 248 PSCEMS students. The responses of each individual and group of respondents were tallied and analyzed. The data regarding respondents’ profiles were gathered and converted into simple frequency counts, percentages, and means. Multiple regression analysis was used to determine the relationship between the profiles of the respondents and their level of competency in ECG interpretation.
Results
The questionnaire was sent to 248 students via their university email; 139 students responded for a response rate of 56%. Two forms were excluded because they were not completed. The average age of respondents was 21.5 years. In terms of the number of students in each academic year, 29 (21.2%) were in 1st year, 34 (24.8%) were in 2nd year, 34 (24.8%) were in 3rd year, and 40 (29.2%) were in their internship year. The mean overall competency score was 7.29 with a wide range from 0 to 12 and the mode was 8. A total of 88 (64.2%) of the respondents scored >7.5 points, indicating competency in ECG interpretation. The most common question that students answered incorrectly was regarding the pathological Q wave; only 30 (22%) students answered it correctly. In addition to that, 81 (59%) students were not able to identify ventricular extra-systole in patients with known digitalis overdose.
Table 1 presents the study level, mean age for each group, and percentage of each group that achieved competency in ECG interpretation.
 |
Table 1 Competency Score per Level |
The 1st year students performed significantly more poorly than the remaining students in terms of the overall score (Tables 1 and 2). This was potentially because the 1st year students had not yet completed the cardiology course. However, despite the fact that the 3rd year and internship students had been exposed to a greater number of patients than had the 2nd year students, there was no significant difference among these groups regarding their competency in ECG interpretation.
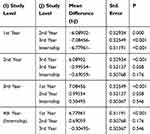 |
Table 2 Group Differences According to Study Level |
As indicated in Table 3, GPA was found to be predictive of competency in ECG interpretation; a GPA of >3.5/5 was positively associated with competency (p<0.001).
 |
Table 3 Group Differences According to GPA |
As demonstrated in Table 4, enrollment in extracurricular courses such as advanced cardiac life support (ACLS) or any other courses related to ECG was significantly associated with ECG interpretation competency.
 |
Table 4 Relationship Between Enrollment in Extracurricular Courses and Overall Score |
Finally, as indicated in Table 5, there was no significant difference in the number of points obtained in relation to the time since the last course, mode of the course delivery (in-class vs online), or length of the course.
 |
Table 5 Differences in Score Due to Timing, Delivery, and Length of Course |
Discussion
This study aimed to evaluate ECG interpretation competency among EMS students using the two-part questionnaire developed by Coll-Badell et al. The questionnaire was previously demonstrated to be a valid and reliable instrument by the original authors, which was later confirmed by other researchers.19 Overall, our current sample of paramedic students demonstrated acceptable competency in ECG interpretation. Sixty-four percent (64%) of the students obtained scores of >7.5 Further, after completing their 1st year and the cardiology course during their 2nd year, there was a significant improvement; 22 of the 2nd year students (65%) achieved competency in ECG interpretation (i.e. achieved a score of 7.5, compared to only 4% seen among 1st year students). Although this study supports the findings of previous similar studies, this is the first study to evaluate paramedic student competency in ECG interpretation. Our current findings are indicative of an acceptable level of competency in ECG interpretation among these paramedic students. This finding concurs with that of Werner et al,20 which demonstrated that 54% of EMS nurses in western Sweden were competent in ECG interpretation. Our result is also in line with that of Whitbread et al,21 who reported that paramedics could reliably recognize pathological change on an ECG. This study demonstrated that the competency of ECG interpretation varied among the paramedic students who participated in this study, primarily according to their level of education and GPA. Once the students had completed the formal cardiology course at the beginning of their 2nd year, their competency in ECG interpretation improved. Interestingly, no further significant improvement was observed with academic progression. These findings reinforce those of Nik Azlan and Muhamad.22 Moreover, the ACLS course and other related extracurricular courses were found to play a major role in improving student competency. This finding reinforces the importance of a dedicated undergraduate cardiology course for paramedics, along with specialized courses such as ACLS and other related extracurricular courses. Utilizing distance learning for such courses seems to be equal to in-class learning in terms of achieving an acceptable level of competency in ECG interpretation.
There are some limitations to this study. First, this was a single-center study, and therefore, selection bias cannot be excluded. Further, as the questionnaire was completed via email, it was impossible to ensure that the students did not share answers. Furthermore, these results do not reflect the students’ competency in ECG interpretation during real-world stressful emergencies or medical scenarios and therefore the findings cannot be generalized to a provider level and future studies should include assessments of professional Saudi paramedics. The retention of ECG interpretation knowledge might be affected after their graduation, so continuous education in this skill is warranted as they are recently completed formal ECG training but are not yet practicing independently. Finally, this study confirmed the existing opportunity to improve patient outcome as obtaining a pre-hospital electrocardiogram (ECG) will lower adjusted risk of mortality among ACS patients, that might be achieved as relying more on pre-hospital ECG that done by paramedics in the field.
Conclusions
This is the first study to evaluate paramedic student competency in ECG interpretation. The majority of our paramedic students demonstrated acceptable competency in ECG interpretation. GPA and enrollment in cardiology were significantly associated with improved competency. ACLS courses and other related extracurricular courses were found to play a major role in improving student competency. Future studies should include professional Saudi paramedics and methods on how to retain ECG interpretation knowledge should also be examined.
Acknowledgments
The author is thankful to the Deanship of Scientific Research, King Saud University and Prince Sultan College for Emergency Medical Services’ Research center for supporting him in this research.
Disclosure
The author declares no conflicts of interest in this work.
References
1. Ajam T, Mehdirad A. Electrocardiography. [Cited 3 April 2020]. Available from: https://emedicine.medscape.com/article/1894014-overview#a6.
2. Drew BJ, Sommargren CE, Schindler DM, Benedict K, Zegre-Hemsey J, Glancy JP. A simple strategy improves prehospital electrocardiogram utilization and hospital treatment for patients with acute coronary syndrome (from the ST SMART Study). Am J Cardiol. 2011;107:347–352. doi:10.1016/j.amjcard.2010.09.027
3. Rebeiz A, Sasso R, Bachir R, Mneimneh Z, Jabbour R, El Sayed M. Emergency medical services utilization and outcomes of patients with ST-elevation myocardial infarction in Lebanon. J Emerg Med. 2018;55:827–835. doi:10.1016/j.jemermed.2018.09.016
4. Ho AF, Loy EY, Pek PP, et al. Emergency medical services utilization among patients with ST-segment elevation myocardial infarction: observations from the Singapore myocardial infarction registry. Prehosp Emerg Care. 2016;20:454–461. doi:10.3109/10903127.2015.1128032
5. Trimmel H, Bayer T, Schreiber W, Voelckel WG, Fiedler L. Emergency management of patients with ST-segment elevation myocardial infarction in Eastern Austria: a descriptive quality control study. Scand J Trauma Resusc Emerg Med. 2018;26:38. doi:10.1186/s13049-018-0504-3
6. Scholz KH, Hilgers R, Ahlersmann D, et al. Contact-to-balloon time and door-to-balloon time after initiation of a formalized data feedback in patients with acute ST-elevation myocardial infarction. Am J Cardiol. 2008;101:46–52. doi:10.1016/j.amjcard.2007.07.078
7. Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) registry. J Am Coll Cardiol. 2009;53:161–166. doi:10.1016/j.jacc.2008.09.030
8. Mumma BE, Kontos MC, Peng SA, Diercks DB. Association between prehospital ECG use and patient home distance from the PCI center on total reperfusion time in STEMI patients: a retrospective analysis from the NCDR®. Am Heart J. 2014;167:915. doi:10.1016/j.ahj.2014.03.014
9. Khot UN, Johnson ML, Ramsey C, et al. Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation. 2007;116:67–76. doi:10.1161/CIRCULATIONAHA.106.677401
10. Patel M, Dunford JV, Aguilar S, et al. Pre-hospital electrocardiography by emergency medical personnel: effects on scene and transport times for chest pain and ST-segment elevation myocardial infarction patients. J Am Coll Cardiol. 2012;60:806–811. doi:10.1016/j.jacc.2012.03.071
11. Kahlon TS, Barn K, Akram MM, et al. Impact of pre-hospital electrocardiograms on time to treatment and one year outcome in a rural regional ST-segment elevation myocardial infarction network. Catheter Cardiovasc Interv. 2017;89:245–251. doi:10.1002/ccd.26567
12. Garvey JL, MacLeod BA, Sopko G, Hand MM. Pre-hospital 12-lead electrocardiography programs: a call for implementation by emergency medical services systems providing advanced life support - National Heart Attack Alert Program (NHAAP) Coordinating Committee; National Heart, Lung, and Blood Institute (NHLBI); National Institutes of Health. J Am Coll Cardiol. 2006;47:485–491. doi:10.1016/j.jacc.2005.08.072
13. Antiperovitch P, Zareba W, Steinberg JS, et al. Proposed in-training electrocardiogram interpretation competencies for undergraduate and postgraduate trainees. J Hosp Med. 2018;13:185–193. doi:10.12788/jhm.2876
14. O’Brien KE, Cannarozzi ML, Torre DM, Mechaber AJ, Durning SJ. Training and assessment of ECG interpretation skills: results from the 2005 CDIM survey. Teach Learn Med. 2009;21:111–115. doi:10.1080/10401330902791255
15. Stopa M, Sevenathan H, Bogusławski M, Pałasz I. Assessment of ECG interpretation skills among polish medical students, nursing, emergency medicine and english division medical students. Porto Biomed J. 2017;2:231.
16. Matthias AT, Indrakumar J. Competency of final year medical students in ECG Interpretation-an experience of a medical school in South Asia. Asian Stud Med J. 2013;13(6).
17. Jablonver RS, Lundberg E, Zhang Y, Stagnaro-Green A. Competency in electrocardiogram interpretation among graduating medical students. Teach Learn Med. 2014;26:279–284. doi:10.1080/10401334.2014.918882
18. Alghamdi SAA, Almuntashiri AHA, Aljuaeed MSA, Mohamed MA. Electrocardiography misreading among sixth-year medical students and interns in Taif University. Int J Community Med Public Health. 2018;5:4225. doi:10.18203/2394-6040.ijcmph20183958
19. Coll-Badell M, Jiménez-Herrera MF, Llaurado-Serra M. Emergency nurse competence in electrocardiographic interpretation in Spain: a cross-sectional study. J Emerg Nurs. 2017;43:560–570. doi:10.1016/j.jen.2017.06.001
20. Werner K, Kander K, Axelsson C. Electrocardiogram interpretation skills among ambulance nurses. Eur J Cardiovasc Nurs. 2014;1–7.
21. Whitbread M, Leah V, Bell T, Coats TJ. Recognition of ST elevation by paramedics. Emerg Med J. 2002;19:66–67. doi:10.1136/emj.19.1.66
22. Nikazlan NM, Muhamad SZ. Confidence level and knowledge of pre-hospital thrombolysis therapy of paramedic in prehospital care: a survey. Med Health J. 2019;14:34–43. doi:10.17576/MH.2019.1401.03
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
