Back to Journals » Nature and Science of Sleep » Volume 12
Electroacupuncture versus Sham Acupuncture for Perimenopausal Insomnia: A Randomized Controlled Clinical Trial
Authors Li S, Wang Z, Wu H, Yue H, Yin P, Zhang W, Lao L, Mi Y, Xu S
Received 29 September 2020
Accepted for publication 10 December 2020
Published 22 December 2020 Volume 2020:12 Pages 1201—1213
DOI https://doi.org/10.2147/NSS.S282315
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sarah L Appleton
Shanshan Li,1,* Zhaoqin Wang,2,* Huangan Wu,3,* Hongyu Yue,1 Ping Yin,1 Wei Zhang,4 Lixing Lao,5 Yiqun Mi,1 Shifen Xu1
1Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai 200071, People’s Republic of China; 2Department of Aeronautics and Astronautics, Shanghai Key Laboratory of Acupuncture Mechanism and Acupoint Function, Fudan University, Shanghai 200433, People’s Republic of China; 3Shanghai Research Institute of Acupuncture and Meridian, Shanghai University of Traditional Chinese Medicine, Shanghai 200030, People’s Republic of China; 4Department of Biostatistics, School of Public Health, Fudan University, Shanghai 200032, People’s Republic of China; 5Virginia University of Integrative Medicine, Fairfax, VA 22031, USA
*These authors contributed equally to this work
Correspondence: Shifen Xu; Yiqun Mi
Shanghai Municipal Hospital of Traditional Chinese Medicine, 274 Middle Zhijiang Road, Shanghai 200071, People’s Republic of China
Tel +86 13761931393
; Tel +8618930177567
Email [email protected]; [email protected]
Objective: To evaluate the short- and long-term effects of acupuncture on perimenopausal insomnia (PMI) and quality of life.
Patients and Methods: We designed a semi-standardized, patient-blinded, randomized placebo-controlled trial. A total of 84 patients were recruited, all of whom met the criteria for diagnosis of PMI. Either acupuncture therapy or a noninvasive placebo acupuncture therapy designed to treat insomnia was implemented 18 times over the course of 8 weeks (3 times per week for 4 weeks, twice per week for 2 weeks, once per week for 2 weeks). The primary outcome was the change in Pittsburgh Sleep Quality Index (PSQI) scores from baseline to the end of treatment, week 8. Secondary outcomes included climacteric symptoms and quality of life measured by the Menopause Quality of Life (Men-QoL), Insomnia Severity Index (ISI), Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS), sleep parameters recorded in the actigraphy and adverse events. The PSQI and Men-QoL were assessed at weeks 0, 4, 8, 12 and 20. Other assessments were performed at week 0 and week 8.
Results: The participants were randomly assigned to either acupuncture (n=42) or sham acupuncture (n=42) groups. The mean difference from baseline of PSQI score at the end of treatment between real acupuncture and sham acupuncture group was − 2.38 (95% CI, − 3.46 to − 1.30; P< 0.001). The acupuncture group was associated with significantly lower scores than the sham acupuncture group at week 12 and during the 20-week follow-up visits (all P < 0.001). Acupuncture was also associated with significantly higher quality of life in vasomotor and other physical dimensions (all P < 0.001). At the end of treatment, researchers found a significantly higher total sleep time (TST), sleep efficiency (SE) and lower number of average awakenings (AA) (P =0.007 0.023 and 0.011, respectively) in the acupuncture group than in the sham acupuncture group. No severe adverse events were reported.
Conclusion: The findings suggest that acupuncture may be a safe and effective treatment for PMI and improving quality of sleep in patients with menopause and could have a long-lasting effect.
Trial Registration: Chinese Clinical Trial Registry (ChiCTR); Trial ID: ChiCTR1800018645. URL: http://www.chictr.org.cn/showproj.aspx?proj=31482.
Keywords: acupuncture, perimenopausal insomnia, randomized controlled trial
Introduction
Perimenopause is the transitional period before and after menopause, during which the biological and endocrine changes occur in women. Patients report higher incidences of bothersome symptoms during this period, including vasomotor symptoms, insomnia and depression.1–3 Perimenopausal insomnia (PMI) significantly impairs women’s quality of life, with a prevalence and morbidity rate of 35–50% during menopause.4,5 PMI is characterized by having difficulty with falling night asleep and/or early morning awakening. Insomnia is more severe and longer lasting in perimenopausal women than in non-menopausal women.6,7 Therefore, management of PMI is challenging and requires an innovative and safe alternative approach. Hormone replacement therapy (HRT) and cognitive behavioral therapy (CBT) are the most effective therapies for PMI.8–10 However, some patients are reluctant to use HRT due to the adverse effects, such as cardiovascular disease11 and cancer.12 Cognitive behavioral therapy for insomnia (CBT-I) has strong evidence to improve the quality of sleep and no adverse effects.13,14 However, CTB-I is rarely used in Chinese patients due to the high costs and lack of experienced providers. Consequently, a safe, effective and feasible treatment, without adverse effects is needed. The Cochrane meta-analysis,15 published in 2012 found that acupuncture used as an adjunct to other treatment was shown to be clinically effective for insomnia. There have been several randomized controlled studies in the past that found that acupuncture is relatively effective for the treatment of primary insomnia16,17 and depression-related insomnia.18–20 Patients with PMI often show interest in acupuncture,21,22 a safe and commonly used complementary therapy. Several trials have demonstrated the positive effects of acupuncture on insomnia in perimenopausal women.23–26 However, currently there is a lack of well-designed clinical trials to explore the effects of acupuncture on PMI.21,22 Although several previously published pilot studies24,25 have assessed the effects of acupuncture on PMI, these results lacked any follow-up to investigate the long-term effect of acupuncture in PMI. Facing the limitations of clinical trial, there is need for a high-quality, strictly conducted clinical trial to confirm the effectiveness and safety of acupuncture for PMI.
For those reasons, we have conducted a randomized, placebo-controlled trial to investigate the effect of acupuncture compared to a noninvasive sham control for short- and long-term benefits in perimenopausal women with insomnia.
Patients and Methods
The full protocol of this trial has been previously published.27 A 2-parallel-group, block randomized, blinded (except acupuncturists), sham-controlled trial design was used. All participants signed informed consent at the time of enrollment. The trial was conducted in accordance with the Declaration of Helsinki. The Ethics Committee of Shanghai Municipal Hospital of Traditional Chinese Medicine approved the study protocol (2018SHL-KY-09) and was published on May 2019. Our trial followed the Consolidated Standards of Reporting Trials (CONSORT) and acupuncture reporting guidelines, Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).
Participants
Participants were recruited at Shanghai Municipal Hospital of Traditional Chinese Medicine from October 2018 to December 2019 through the outpatient clinic, advertisements on the hospital-based Wechat and posters. The trial focused on perimenopausal women experiencing insomnia. Participants received either acupuncture or sham acupuncture treatment.
Inclusion criteria were as follows: diagnosis met ICSD-3 (International Classification of Sleep Disorders) criteria;28 age 45 to 60 years old; amenorrhea for at least 6 months; insomnia lasting at least 3 months; a total score higher than 5 on Pittsburgh Sleep Quality Index (PSQI);29 TCM differentiation types (kidney Yin deficiency and kidney Yang deficiency); willingness to participate and be randomly assigned to 1 of the groups; signed informed consent.
Exclusion criteria were as follows: ongoing hormone replacement therapy and/or antidepressant drugs; induced amenorrhea due to surgery; any serious physical disease; insomnia caused by other external factors; a score greater than 15 on PSQI; use of hypnotic medication, except Estazolam; received acupuncture treatment for climacteric syndrome in the last 6 months; participated in any other clinical trial in the last 6 months; not capable of understanding the trial or providing responses for the outcome measurements.
Randomization and Blinding
The random allocation lists were generated by an independent statistician (WZ) using SAS 9.4. The participants who met the criteria were randomly assigned to either acupuncture or sham acupuncture. The random allocation details were concealed in opaque envelopes. The acupuncturist opened the envelopes once participants had finished all baseline assessments at the time of the 1st acupuncture treatment.
Only the acupuncturists knew the treatment allocation. Participants and other relevant researchers (the principal investigator (PI), data analysts, outcome assessors, and statisticians) were kept blinded to the group allocation.
Interventions
A semi-standardized acupuncture protocol for PMI was developed by senior researchers (LXL and HGW) and practiced acupuncturists, according to textbook protocol,30 literature reviews31,32 and our previous study conclusions.17,18 Participants in each group were offered 18 sessions of real or sham treatments over the course of 8 weeks (3 times per week for 4 weeks, twice per week for 2 weeks, once per week for 2 weeks). The details about interventions have been published in our protocol in 2019. Patients were placed in separate quiet spaces lying in a supine position and received 30-minute treatments based on the diagnosed TCM (Traditional Chinese Medicine) syndrome.
Acupuncture
Patients received treatment consisting of 10 acupuncture points, 8 main fixed points plus 2 additional points selected by researchers based on the patient’s syndrome differentiation. The main points include Baihui (GV20), shenting (GV24), yintang (GV29), qihai (CV6), guanyuan (CV4) and bilateral anmian (EX-HN22), sanyinjiao (SP6), and shenmen (HT7). Additional points include mingmen (GV4) and shenshu (BL23) for kidney yang deficiency and taiXi (KI3) and fuliu (KI7) for kidney yin deficiency. Sterile and disposable (0.25 × 40 mm and 0.30 × 40 mm in length; Jia Jian, China) needles were inserted into the skin to the depth of 10–30 mm and manipulated manually (manipulation technique included lifting, thrusting, and rotating) until the patient reported needling sensations (Deqi sensation). GV20 and GV29 were connected to a G6805–2 Multi-Purpose Health Device (Huayi Company), using continuous wave type, frequency at 2.5 HZ, and intensity of 4–5 mA. Needles were retained for 30 min before removal. Conversation between acupuncturists and patients was minimal to avoid nonspecific treatment effects.
Sham Acupuncture
Participants in the sham acupuncture group received Streitberger Placebo needle,33 a non-invasive placebo device. The needle shortens into itself once it touches the skin giving the visual impression of insertion into the skin. Both acupuncture group and sham acupuncture group used the base device. Although the blunt needle tip could generate weak effects,34,35 there are significant differences between acupuncture and sham acupuncture.36 The placebo needle has also been successfully used by our research team in a previous study.17,18 The acupoints were the same as used for the acupuncture group, but without insertion. AG6805–2 Multi-Purpose Health Device was connected to the GV20 and GV29, without electrical pulse. Needles were retained for 30 min before removal. Participants in both groups received 18 treatments over the course of 8 weeks.
Others Concurrent Treatments
We discouraged participants from starting new cointerventions for insomnia during the study period. However, participants already receiving Estazolam (1–2mg) treatment continued use for the intervention period. Participants were told that they had equal odds of receiving real or “placebo” treatment and were free to withdraw from the study at any time. Acupuncturists (SSL and ZQW) were trained professionally for administering this treatment.
Standardization of the Intervention
The treatment was provided at Shanghai Municipal Hospital of Traditional Chinese Medicine. The acupuncturists obtained bachelor’s degrees in TCM, had at least 3 years of clinical experience prior to this study, and are registered practitioners of TCM. All relevant researchers were trained according to the protocol to ensure the quality of this study.
Outcomes Measurements
The primary outcome was the change in the Pittsburgh Sleep Quality Index (PSQI) between the baseline and the end of treatment (week 8) results.15 The PSQI is a self-rating questionnaire resulting in a global score between 0 and 21, which consists of 7 sub-scores (sleep quality, sleep onset latency, sleep duration, sleep efficiency, sleep disturbances, daytime dysfunction and use of sleep medication).37 A PSQI global score >5 indicates a poor quality of sleep.29 PSQI were assessed before random assignment (baseline), during the treatment (week 4), at the end of treatment (week 8; primary time point), and during follow-up visits (week 12 and week 20).
Secondary outcomes were climacteric symptoms and quality of life measured by the Menopause Quality of Life (Men-QoL)38,39 scales at week 4, week 8 and at the post-treatment follow-up visits at week 12 and week 20; the sleep parameters recorded in the Actigraphy (included TST: total sleep time; SE: sleep efficacy; SA: sleep awakenings; AA: average awakening; WASO: wake after sleep onset) at week 8; sleep disturbance measured by Insomnia Severity Index (ISI)40 at week 8; and anxiety and depression measured by Self-Rating Anxiety Scale (SAS)41 and Self-Rating Depression Scale (SDS)41,42 at week 8. At the end of treatment, participants were asked to assess which treatment they received (acupuncture group, simulated acupuncture treatment group, unsure).43
Any adverse events (AE) likely to be related to the acupuncture treatment were recorded. All AE were reported on the case report form (CRF) by independent assessors (HYY and PY).
Statistical Analysis
The sample size calculation was based on the change of PSQI scores. A systematic review15 shows that at least a 2.70-point difference in PSQI scores between acupuncture and sham acupuncture has clinical significance. We expected that acupuncture would outperform the sham acupuncture by 3 points (80% power, 5% significance level, and 2-sided test). Considering a dropout rate of 20%, a total of 84 participants were recruited.
An intention-to-treat approach44 was used and all randomly assigned participants were analyzed. Continuous variables were described as mean (SD) or median (p25, p75) and categorical variables were described as frequency and percentage. For baseline characteristics, continuous variables were examined by independent sample t-test or Wilcoxon rank-sum test, and categorical variables were compared by chi-square test, Fisher’s exact test or CMH chi-square test as appropriate.
The differences in group outcome measures of Actigraphy, ISI, SAS and SDS were evaluated by covariance analysis, and PSQI and Men-QoL were assessed by the linear mixed effects model with the interaction of visit and group. We assessed the success of blinding by using the Bang Blinding Index.45 All statistical analyses were performed using SAS software (version 9.4), and P values less than 0.05 were considered significant.
Results
Figure 1 shows 106 participants were screened. Of the 22 participants who were excluded, 5 declined to participate and 17 were not postmenopausal or in the menopausal transition, did not meet the inclusion criteria, or were using HT drugs. Of the 84 eligible participants enrolled and randomly assigned 42 participants were allocated to the acupuncture group and 42 participants to the sham acupuncture group. In the acupuncture group 2 women dropped out due to personal reasons. In the control group, 1 woman dropped out due to personal reasons. At the end of treatment, 40 participants in the acupuncture group and 41 participants in the sham acupuncture group had completed treatment. The missing data were imputed by LOCF method (Last observation carried forward).
 |
Figure 1 Study flow diagram. |
Sociodemographic and clinical characteristics, risk factors for insomnia, and baseline outcomes were similar between the 2 groups (Table 1). A majority of participants had obtained a secondary school degree and were employed. The participants’ mean age was 52.5 years, the duration of insomnia was 39.7 months and very few of them had received Estazolam therapy for insomnia. On the Expectancy Questionnaire (administered before the first treatment), most women indicated that they believed their PMI would be improved by acupuncture.
 |
Table 1 Baseline Characteristics of Participants, by Group |
On the primary outcome, the linear mixed effects model showed a significant interaction of visit and group (P< 0.001). The intention-to-treat (ITT) analyses at the end of treatment (week 8) showed a mean change from baseline in PSQI of −3.76 and −1.38 in the acupuncture and sham acupuncture group, with an estimated difference of −2.38 (95% CI, −3.46 to −1.30; P <0.001; Table 2; Figure 2). At week 4, there was no statistically significant difference between acupuncture group and sham acupuncture group: −0.95 (95% CI, −2.03 to 0.13; P =0.084). At 12-week and 20-week follow-up visits, there were statistically significant differences in the PSQI score between the 2 groups −3.55 (95% CI, −4.63 to −2.47; P <0.001) and −3.64 (95% CI, −4.72 to −2.56; P <0.001), respectively. Effectively, the acupuncture group reported lower post treatment PSQI scores than the sham acupuncture group. The acupuncture group showed a greater reduction in PSQI score compared with the sham acupuncture group (−3.76 vs −1.38; P <0.001). Table 3 shows the 7 components of PSQI. The aspects of Sleep Duration, Sleep Quality, Sleep Disturbance and Habitual Sleep Efficiency showed the significant difference between 2 groups.
 |
Table 2 Changes from Baseline of PSQI and Men-QoL Outcomes at the End of Treatment (8-Week) and the 12-Week and the 20-Week Follow-Up Visits by Group |
 |
Table 3 Seven Components of PSQI Changes from Baseline to the End of Treatment (8-Week) and the 12-Week and the 20-Week Follow-Up Visits by Group |
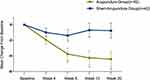 |
Figure 2 Adjusted mean (95% CI) change from baseline in PSQI scores. Note: *P<0.05 vs sham acupuncture group. |
Similar results were observed for Men-QoL dimensions (Table 2). The acupuncture group reported lower scores than sham acupuncture group in Men-QoL vasomotor and physical domains at week 8 during the final treatment report, and at weeks 12 and 20 during follow-up visits: −1.22 (95% CI, −1.70 to −0.75; P <0.001), −1.27 (95% CI, −1.72 to −0.82; P <0.001), −1.35 (95% CI, −1.76 to −0.94; P <0.001) and −0.69 (95% CI, −1.09 to −0.30; P <0.001), −0.08 (95% CI, −1.12 to −0.849; P <0.001), −0.85 (95% CI, −1.18 to −0.53; P <0.001). Of note, at week 4, there were no statistically significant differences between the acupuncture group and the sham acupuncture group: −0.43 (95% CI, −0.89 to 0.03; P=0.066) and −0.40 (95% CI, −0.75 to 0.06; P=0.021). For psychosocial and sexual dimensions scores, there were no significant differences between groups at any time points (P > 0.05).
The results of actigraphy assessments are reported in Table 4. After treatment, there were a significantly higher TST (405.64 ± 61.19 vs 372.39 ± 47.84; P =0.007) and SE (81.14 ± 7.89 vs 76.61 ± 9.28; P =0.023) in the acupuncture group than in the sham acupuncture group. There were significantly lower instances of AA (4.19 ± 1.59 vs 5.35 ± 2.45; P =0.011) in the acupuncture group than the sham acupuncture group. However, no significant differences in the SA and WASO were noted between the 2 groups (P > 0.05). Table 5 shows the estimated means and SD between the 2 groups for secondary outcomes of insomnia severity, anxiety, and depression. At the end of treatment (week 8), ISI and SAS scores were significantly lower in the acupuncture group than the sham acupuncture group (8.86 ± 3.88 vs 12.50±5.15; P <0.001) (44.98 ± 3.85 vs 48.10 ± 6.04; P =0.007). There were 9 women in the acupuncture group and 10 women in the sham acupuncture group that used Estazolam for insomnia at baseline (Table 6). However, after treatment, 3 women in the acupuncture group stopped taking Estazolam and 1 woman in the sham acupuncture group began Estazolam therapy.
 |
Table 4 Actigraphy Assessments at Baseline and the End of Treatment (Week 8) by Group |
 |
Table 5 ISI, SAS and SDS Outcomes at Baseline and the End of Treatment (Week 8) by Group |
 |
Table 6 Use of Estazolam for Insomnia, by Group, n (%) |
Based on the results of the Bang Blinding Index (Table 7), blinding was successful in the sham acupuncture group, but more participants in the acupuncture group correctly guessed their group placement. Adverse events are reported in Table 8. There were 2 women (1 bleeding and 1 pain) in the acupuncture group and 1 woman (pain) in the sham acupuncture group who reported adverse events. All adverse events were mild and all participants continued on to finish the trial.
 |
Table 7 Results of the Blinding, by Group |
 |
Table 8 Adverse Events, by Group, n (%) |
Discussion
Previous studies have focused on the effect of acupuncture on vasomotor symptoms rather than insomnia. For PMI, there are 2 trials that reported the benefits of acupuncture and moxibustion, but the sample size used in these studies are small.25,46 Avis26 and Borud23 et al demonstrated that acupuncture could improve the PSQI score and prolong the night sleep time in patients with PMI. However, the patients enrolled in these studies were mainly postmenopausal women with vasomotor symptoms rather than insomnia. A previously published study reported that acupuncture can relieve the severity of insomnia over a short period of time.24 Our trial is the first study focus on the acupuncture for PMI in short- and long-term improvement of sleep quality.
In our semi-standardized, patient-blinded, randomized, sham-controlled trial, the results showed that the 8-week course of electroacupuncture was more effective than sham acupuncture for patients with PMI. Through analyzing 7 components of PSQI, our data suggest that electroacupuncture may also affect sleep quality in the following ways: prolonged Sleep Duration, improved Sleep Quality, fewer Sleep Disturbances and increased Habitual Sleep Efficiency. All these effects were again observed during the 20-week follow-up. This means electroacupuncture not only provided short-term relief but also long-term relief lasting up to 3 months post treatment. While the Sleep Latency reduced at week 12 and week 20, Use of Sleep Medication and Daytime Dysfunction showed no significant change in this trial. The wActiSleep-BT wireless sleep monitor showed the same outcomes in Sleep Efficacy and Total Sleep Time, and the reported Average Awakening reduced as well. The outcomes of PSQI and wActiSleep-BT wireless sleep monitor all proved the efficacy of electroacupuncture treatment for PMI compared with sham acupuncture group. Patients in electroacupuncture group also had improvements in some menopausal symptoms (vasomotor and physical domains) and anxiety. In addition, there were no severe adverse events during the trial. Our findings are consistent with the short-term efficacy studies of acupuncture for perimenopausal insomnia. However, our study also shows electroacupuncture treatment may improve the quality of sleep for perimenopausal insomnia patients for up to 3 months. This is strong evidence that other similar studies have not mentioned, indicating that electroacupuncture plays an important role in the management of perimenopausal insomnia in clinical practice. Furthermore, we found no evidence of an advantage of electroacupuncture over sham acupuncture on depression and the Men-QoL (psychosocial and sexual domains).
It still remains unclear how electroacupuncture alleviates PMI. Acupuncture is believed to have a positive effect on restoring a normal sleep-wake cycle. It was shown that acupuncture improved sleep efficiency and total sleep time, reduced the number of awakenings after sleep, and reduced the length of the first stage (first stage of what?).24 Physiological hyperexcitability during insomnia was reflected in the degree of hyperactivity of sympathetic nerves (SNS) and hypothalamus-pituitary-adrenal axis (HPA). Evidence suggests that acupuncture reduces rostral ventrolateral medulla (RVLM)’s oxidative stress and regulates sympathetic excitability, where the sympathetic nervous control center is located.47 Meanwhile, electroacupuncture might regulate hypothalamus pituitary adrenal axis hyperactivity by changing the micro RNA expression.48 Additionally, imaging studies have shown that the glucose metabolic rates of the thalamus, anterior cingulate cortex and medial prefrontal cortex in insomnia patients are higher than those of healthy people, which leads to greater productivity and heat generation in insomnia.49 Electroacupuncture at KI3 attenuates glucose metabolism in the hypothalamus and hypothalamus.50 This might reduce sympathetic stimulation, which affects sleep status. For PMI patients, lower estradiol and higher luteinizing hormone levels are significantly involved. Acupuncture can improve levels of estradiol, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) which stabilizes sex hormones,51 having the same effect as a hormone replacement.
Some limitations of this trial should be highlighted. The use of actigraphy monitors were not defined (1 to 3 nights) due to the limited supply. We hoped this variation could be addressed by randomization (occurred in both groups) and data averaging. Secondly, this study did not pay attention to changes in female estrogen levels because most patients were unwilling to take blood tests. Thirdly, we included patients with the most common syndromes of kidney-yin deficiency and kidney-yang deficiency pattern in order to reach a satisfactory internal consistency of the participants. In the future, we will design more rigorous studies to prove the effectiveness of acupuncture in the treatment of PMI with broader applications.
Conclusion
The findings suggest that electroacupuncture may be a safe and effective treatment for PMI and improving quality of sleep in patients with menopause and has long lasting effects.
Abbreviations
PMI, perimenopausal insomnia; PSQI, Pittsburgh Sleep Quality Index; Men-QoL, Menopause Quality of Life; ISI, Insomnia Severity Index; SAS, Self-Rating Anxiety Scale; SDS, Self-Rating Depression Scale; TST, total sleep time; SE, sleep efficiency; AA, average awakenings; ChiCTR, Chinese Clinical Trial Registry; HRT, hormone replacement therapy; SSRIs, selective serotonin reuptake inhibitors; ICSD-3, International Classification of Sleep Disorders; PI, principal investigator; AE, adverse events; CRF, case report form; LOCF, Last observation carried forward; ITT, intention-to-treat; SNS, sympathetic nerves; HPA, hypothalamus-pituitary-adrenal axis; RVLM, reduced rostral ventrolateral medulla; FSH, follicle-stimulating hormone; LH, luteinizing hormone.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author (Shifen Xu) upon reasonable request. Also, the individual deidentified participant data is available after contacting the corresponding author via email ([email protected]). The data will be available immediately following publication without an end date.
Acknowledgments
The authors thank Prof. Ruiping Wang from Shanghai University of Traditional Chinese Medicine for the statistical guidance; Dr. Jing Chen and Jian Xu from Shanghai Municipal Hospital of Traditional Chinese Medicine for referring proper participants; Prof. Xiao Huang from Department of Neurology and Department of Psychological Medicine, Zhongshan Hospital, Fudan University for providing expert opinions on the treatment protocol; we also thank Dr. Zonya Christine Crossno and Dr. Philippa Hazlewood from the International Education College, Shanghai University of Traditional Chinese Medicine, for editorial support of manuscript, and all other project staff, as well as the trial participants.
Funding
The study was partly supported by grants from the National Natural Science Foundation of China (No 81973943), Shanghai Municipal Health Commission (2019LJ06), and sponsored by grants from Shanghai Committee of Science and Technology, China (No. 18401905200). The funding body has no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Avis NE, Crawford SL, Green R. Vasomotor symptoms across the menopause transition: differences among women. Obstet Gynecol Clin North Am. 2018;45(4):629–640. doi:10.1016/j.ogc.2018.07.005
2. Kravitz HM, Xinhua Z, Bromberger JT, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31(7):979–990.
3. Mulhall S, Andel R, Anstey KJ. Variation in symptoms of depression and anxiety in midlife women by menopausal status. Maturitas. 2018;108:7–12. doi:10.1016/j.maturitas.2017.11.005
4. Prairie BA, Wisniewski SR, Luther J, et al. Symptoms of depressed mood, disturbed sleep, and sexual problems in midlife women: cross-sectional data from the study of Women’s Health Across the Nation. J Womens Health (Larchmt). 2015;24(2):119–126. doi:10.1089/jwh.2014.4798
5. Greenblum CA, Rowe MA, Neff DF, Greenblum JS. Midlife women: symptoms associated with menopausal transition and early postmenopause and quality of life. Menopause. 2013;20(1):22–27. doi:10.1097/gme.0b013e31825a2a91
6. Slopien R, Wichniak A, Pawlak M, Slopien A, Warenik-Szymankiewicz A, Sajdak S. Disturbances of sleep continuity in women during the menopausal transition. Psychiatr Pol. 2015;49(3):615–623. doi:10.12740/PP/33442
7. Tal JZ, Suh SA, Dowdle CL, Nowakowski S. Treatment of insomnia, insomnia symptoms, and obstructive sleep apnea during and after menopause: therapeutic approaches. Curr Psychiatry Rev. 2015;11(1):63–83. doi:10.2174/1573400510666140929194848
8. Antonijevic IA, Stalla GK, Steiger A. Modulation of the sleep electroencephalogram by estrogen replacement in postmenopausal women. Am J Obstet Gynecol. 2000;182(2):277–282. doi:10.1016/S0002-9378(00)70211-0
9. Joffe H, Petrillo L, Viguera A, et al. Eszopiclone improves insomnia and depressive and anxious symptoms in perimenopausal and postmenopausal women with hot flashes: a randomized, double-blinded, placebo-controlled crossover trial. Am J Obstet Gynecol. 2010;202(2):171 e171–171 e111.
10. McCurry SM, Guthrie KA, Morin CM, et al. Telephone-based cognitive behavioral therapy for insomnia in perimenopausal and postmenopausal women with vasomotor symptoms: a MsFLASH randomized clinical trial. JAMA Intern Med. 2016;176(7):913–920. doi:10.1001/jamainternmed.2016.1795
11. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. Revista Médica De Chile. 2018;288(8):321–333.
12. Rennert G, Rennert HS, Pinchev M, Lavie O, Gruber SB. Use of hormone replacement therapy and the risk of colorectal cancer. J Clin Oncol. 2009;27(27):4542–4547. doi:10.1200/JCO.2009.22.0764
13. Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. doi:10.7326/M14-2841
14. Geiger-Brown JM, Rogers VE, Liu W, Ludeman EM, Downton KD, Diaz-Abad M. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. 2015;23:54–67. doi:10.1016/j.smrv.2014.11.007
15. Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database Syst Rev. 2012.
16. Wing-Fai Y, Ka-Fai C, Shi-Ping Z, Tuan-Gee Y, Law ACK. Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep. 2009;32(8):1039–1047. doi:10.1093/sleep/32.8.1039
17. Yin X, Gou M, Xu J, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med. 2017;37:193–200. doi:10.1016/j.sleep.2017.02.012
18. Yin X, Li W, Wu H, et al. Efficacy of electroacupuncture on treating depression-related insomnia: a randomized controlled trial. Nat Sci Sleep. 2020;12:497–508. doi:10.2147/NSS.S253320
19. Chung KF, Yeung WF, Yu YM, et al. Acupuncture for residual insomnia associated with major depressive disorder: a placebo- and sham-controlled, subject- and assessor-blind, randomized trial. J Clin Psychiatry. 2015;76(6):e752–760.
20. Wing-Fai Y. Electroacupuncture for residual insomnia associated with major depressive disorder: a randomized controlled trial. Sleep. 2011;6(34).
21. Mengyang H, Yuqing Z. Meta-analysis of randomized controlled trials of acupuncture in the treatment of menopausal insomnia. J Hainan Med Univ. 2020;1–17.
22. Ning Z, Jing HU, Yan W. Meta-analysis on RCTs of menopause sleep disorders treated by acupuncture therapy. Chin J Info TCM. 2012;19(08):24–26.
23. Borud EK, Alraek T, White A, et al. The acupuncture on hot flushes among menopausal women (ACUFLASH) study, a randomized controlled trial. Menopause. 2009;16(3):484–493. doi:10.1097/gme.0b013e31818c02ad
24. Fu C, Zhao N, Liu Z, et al. Acupuncture improves peri-menopausal insomnia: a randomized controlled trial. Sleep. 2017;40(11). doi:10.1093/sleep/zsx153.
25. Hachul H, Garcia TK, Maciel AL, Yagihara F, Tufik S, Bittencourt L. Acupuncture improves sleep in postmenopause in a randomized, double-blind, placebo-controlled study. Climacteric. 2013;16(1):36–40. doi:10.3109/13697137.2012.698432
26. Avis NE, Coeytaux RR, Levine B, Isom S, Morgan T. Trajectories of response to acupuncture for menopausal vasomotor symptoms: the acupuncture in menopause study. Menopause. 2017;24(2):171–179. doi:10.1097/GME.0000000000000735
27. Li S, Yin P, Yin X, et al. Effect of acupuncture on insomnia in menopausal women: a study protocol for a randomized controlled trial. Trials. 2019;20(1):308. doi:10.1186/s13063-019-3374-8
28. Sateia MJ. International classification of sleep disorders-third edition. Chest. 2014;146(5):1387–1394. doi:10.1378/chest.14-0970
29. Buysse DJ, Iii CFR, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
30. Ji Z, Baixiao ZLL. Acupuncture and Moxibustion (International Standard Library of Chinese Medicine). Beijing: People’s Medical Publishing House; 2014.
31. Borud E, White A. A review of acupuncture for menopausal problems. Maturitas. 2010;66(2):131–134. doi:10.1016/j.maturitas.2009.12.010
32. Borud E, Grimsgaard S, White A. Menopausal problems and acupuncture. Auton Neurosci. 2010;157(1–2):57–62. doi:10.1016/j.autneu.2010.04.004
33. Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352(9125):364–365. doi:10.1016/S0140-6736(97)10471-8
34. Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006;24(1):13–15. doi:10.1136/aim.24.1.13
35. Lundeberg T, Lund I, Sing A, Naslund J. Is placebo acupuncture what it is intended to be? Evid Based Complement Alternat Med. 2011;2011:932407. doi:10.1093/ecam/nep049
36. Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25(4):1161–1167. doi:10.1016/j.neuroimage.2005.01.016
37. Backhausa J, Junghannsa K, Broocksa A, Riemannb D, Hohagena F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–740. doi:10.1016/S0022-3999(02)00330-6
38. Greene JG. Constructing a standard climacteric scale. Maturitas. 2008;61(1–2):78–84. doi:10.1016/j.maturitas.2008.09.011
39. Lewis JE, Hilditch JR, Wong CJ. Further psychometric property development of the Menopause-Specific Quality of Life questionnaire and development of a modified version, MENQOL-intervention questionnaire. Maturitas. 2005;50(3):209–221. doi:10.1016/j.maturitas.2004.06.015
40. Bastien CH, VallieAres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307.
41. Li RX, Ma M, Xiao XR, Xu Y, Chen XY, Li B. Perimenopausal syndrome and mood disorders in perimenopause: prevalence, severity, relationships, and risk factors. Medicine (Baltimore). 2016;95(32):e4466. doi:10.1097/MD.0000000000004466
42. Zung WK. A self-rating depression scale. Arch Gen Psychiatry. 1965;12(1):63. doi:10.1001/archpsyc.1965.01720310065008
43. Lao L, Bergman S, Hamilton G, Langenberg P, Berman B. Evaluation of acupuncture for pain control after oral surgery: a placebo-controlled trial. Arch Otolaryngol Head Neck Surg. 1999;125(5):567. doi:10.1001/archotol.125.5.567
44. White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials. 2012;9(4):396–407. doi:10.1177/1740774512450098
45. Bang H, Ni L, Davis CE. Assessment of blinding in clinical trials. Control Clin Trials. 2004;25(2):143–156. doi:10.1016/j.cct.2003.10.016
46. Huang MI, Nir Y, Chen B, Schnyer R, Manber R. A randomized controlled pilot study of acupuncture for postmenopausal hot flashes: effect on nocturnal hot flashes and sleep quality. Fertil Steril. 2006;86(3):700–710. doi:10.1016/j.fertnstert.2006.02.100
47. Wang X-R, Yang J-W, Ji C-S, et al. Inhibition of NADPH oxidase–dependent oxidative stress in the rostral ventrolateral medulla mediates the antihypertensive effects of acupuncture in spontaneously hypertensive rats. Hypertension. 2018;71(2):356–365.
48. Zhu J, Chen Z, Meng Z, et al. Electroacupuncture alleviates surgical trauma-induced hypothalamus pituitary adrenal axis hyperactivity via microRNA-142. Front Mol Neurosci. 2017;10:308. doi:10.3389/fnmol.2017.00308
49. Nofzinger EA, Buysse DJ, Germain A, Price JC, Miewald JM, Kupfer DJ. Functional neuroimaging evidence for hyperarousal in insomnia. Am J Psychiatry. 2004;161:2126–2129. doi:10.1176/appi.ajp.161.11.2126
50. Li J, Peng C, Lai D, et al. Changes in cerebral glucose metabolism after acupuncture at KI3 in spontaneously hypertensive rats: a positron emission tomography study. Acupunct Med. 2019;37:107–115. doi:10.1177/0964528419828733
51. Zhu H, Nan S, Suo C, et al. Electro-acupuncture affects the activity of the hypothalamic-pituitary-ovary axis in female rats. Front Physiol. 2019;10:466. doi:10.3389/fphys.2019.00466
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
