Back to Journals » Clinical Ophthalmology » Volume 14
Efficiency of Operating Room Processes for Elective Cataract Surgeries Done by Residents in a National University Hospital
Authors Umali MIN , Castillo TR
Received 19 August 2020
Accepted for publication 6 October 2020
Published 28 October 2020 Volume 2020:14 Pages 3527—3533
DOI https://doi.org/10.2147/OPTH.S277550
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Maria Isabel N Umali, Teresita R Castillo
Department of Ophthalmology and Visual Sciences, University of the Philippines Manila, Philippine General Hospital, Manila, Philippines
Correspondence: Maria Isabel N Umali
Asian Eye Institute, 8/F Phinma Plaza, Hidalgo Drive, Rockwell, Makati City 1200, Philippines
Tel +63 917 539 0045
Email [email protected]
Purpose: Operating room processes must be efficient to boost profitability and minimize cost while retaining surgical care quality. This study aims to assess operating room efficiency for resident-performed elective phacoemulsification surgeries done under local anesthesia by measuring different key performance indicators and comparing this with international benchmark data.
Patients and Methods: This is a prospective cross-sectional study done in the Department of Ophthalmology of the Philippine General Hospital, the National University Hospital. The operating room milestones were noted and recorded by a single third-party observer in randomly selected operating rooms from April to June 2019.
Results: Fifty-six phacoemulsification cases in randomly selected rooms fulfilling both inclusion and exclusion criteria were observed. None of the cases started on or before the scheduled 6:30 a.m. cutting time, with an average of 34 (SD 8.53) minutes late. Entry lag was above the median, while exit lag and turnover time were above the 95th percentile compared to benchmarking data. Segment analysis also showed an increased entry lag (35.11% vs 21.5%), significantly higher than benchmarks (t: 10.99, df: 55, p< 0.01). Comparison with proposed targets in other studies also showed an increased time for entry lag.
Conclusion: This study determined that entry lag is the performance indicator that should be addressed to improve efficiency. A multidisciplinary approach and group goal-setting are needed to implement changes in the operating room.
Keywords: phacoemulsification, health services administration, benchmarking, observational study
Introduction
The operating room (OR) is a vital asset in any tertiary hospital, as it contributes to more than two-thirds of total hospital revenue.1–3 At the same time, 40% of the hospital’s expenses, including both human resources and operating costs, come from the operating room.2–7 From this point of view, operating rooms are responsible for the most significant percentage of income and expenditure.2,4 Thus, the different processes happening in the OR must be efficient to boost profitability and minimize cost, while retaining the quality of surgical care.
In the surgical setting, efficiency is defined by time. Efficiency requires maximizing the use of time by reducing wasted and unused time and increasing output for a set level of input.8–11 Many factors influence how time is used in the operating room, such as surgical scheduling accuracy, starting on time, minimizing procedure time variation, turnover time, inter-operative delays, among others.12–15 These parameters can be taken through direct observation or a previous recording of the different processes, such as a review of records or closed-circuit television.16
Locally, two studies on the efficiency of operating room services have been done. The first study is a cross-sectional survey of operating rooms in the Department of Surgery of the Philippine General Hospital. Results showed that 3.9% of cases started on or before the scheduled start time, while 49.7% started more than one hour late. Additionally, delays were most apparent during patient entry until the start of anesthesia, especially for first cases.9 In another study done in the Department of Obstetrics and Gynecology, processes were compared before and during the OR complex renovation. Results showed no improvement in efficiency parameters even after having revised policies. Likewise, surgeons could cope with patient load despite a limited number of rooms by extension of operating hours.17
There has been no prior study on operating room efficiency for ophthalmologic cases in the country, more specifically those focusing on phacoemulsification, which is the most common surgery done by ophthalmologists. This study aims to describe operating room efficiency for this surgery using different key performance indicators and compare this with international benchmark data. Results can then be used as baseline data for future interventions.
Methods
This is a prospective observational study done in the Operating Room Complex of the Department of Ophthalmology and Visual Sciences of the Philippine General Hospital, the country’s largest public tertiary training institution. Since residents perform most of the cases and the scheduling of attending-performed surgeries is inconsistent, this study focused on the efficiency of processes only for resident-performed surgeries.
Data collection was done from April to June 2019 by a single third-party observer using a standard time-taking device. The observer was an ophthalmology trainee who was not an employee of the hospital. Since there was only one observer, but multiple operating rooms with simultaneous ongoing cases, randomly selected rooms with consecutive cases were directly observed. Only elective adult phacoemulsification surgeries done under topical anesthesia and performed by residents were included. Cases that were emergencies, done by staff surgeons or had pediatric patients, were excluded. Different operating room milestones were observed and recorded for each operation (Table 1). Demographic data, including age and gender, were also collected. Residents operate on ‘service patients’ who are mostly indigent and are covered by the national health insurance. The specific socioeconomic characteristics of the patients are not within the scope of the study.
 |
Table 1 Operating Room Milestones Observed in This Study and Their Corresponding Definitions9,15 |
Although phacoemulsification surgeries were observed, this study focused more on the peri-operative and operating room milestones affecting efficiency, not the surgery itself. Thus, the different surgery segments such as capsulorhexis, phacoemulsification, irrigation and aspiration, and others were not noted. Instead, only the total operative time, as observed in the lid retractors’ placement and removal, was recorded. Instead of other microsurgical procedures, this particular action was used as the milestone marker, since this could be seen grossly by the study observer.
Data and Statistical Analysis
Data collected were entered into an electronic spreadsheet file (Excel 2016). From the milestones obtained, the different key performance indicators were determined (Table 2). A schematic for the different parameters is shown in Figure 1. Further analysis was done using Stata 13. Benchmarking was done through comparison with published target values,11,18 with the assumption that benchmarking data were normally distributed, where the median resembles the mean, the one-sample test of means was performed to compare current with said data. The significance level for all sets of analyses was set at a p-value of less than 0.05 using two-tailed comparisons.
 |
Table 2 Efficiency Parameters That Were Calculated from the Operating Room Milestones with Their Corresponding Equations and Definitions9,15,18 |
 |
Figure 1 Schematic of the different operating room milestones and key performance parameters. |
Ethical Considerations
Ethics approval was obtained from the institution’s review board, the University of the Philippines, Manila, Research Ethics Board (UPMREB). A waiver of informed consent was requested and granted by the Board since this is an operational study that sought to represent operating room processes mathematically. Likewise, no patient identifiers were collected, and no direct interventions were done. Patients gave informed consent for their respective surgeries. This study received a grant from the Philippine General Hospital Expanded Health Research Office and was conducted according to the Declaration of Helsinki.
Results
Fifty-six phacoemulsification cases fulfilling the inclusion and exclusion criteria were observed from April to June 2019. Mean age was 63 (SD 9.81), with ages ranging from 33 to 78 years old. There were 27 (48.21%) and 29 (51.79%) males and females undergoing phacoemulsification, respectively. There was no single case that started on or before the scheduled start time of 6:30 a.m. Phacoemulsification surgeries started an average of 34 (SD 8.53) minutes late.
Comparison with benchmark data18 showed that entry lag was above median, while exit lag and turnover time were above the 95th percentile of benchmark data (Table 3). Segment analysis showed a significant difference in values for both entry and exit lags compared to published benchmarks specific for cataract surgery (Table 4 and Figure 2).18 Likewise, comparing study results with another study’s proposed targets11 showed that entry lag was increased by as much as seven minutes, while exit lag and turnover time were low, similar to the benchmark comparisons done previously. Furthermore, the operating time for phacoemulsification was also higher, 42.9 minutes vs. 30 minutes set as target in the study.11
 |
Table 3 Key Performance Indicators Obtained for This Study and Compared with Internationally Published Proposed Targets and Benchmark Data11,18 |
 |
Table 4 In-Room Segment Analysis Containing Equation for Data Source, Results (in Percent) and Comparison to Benchmark Data Specific for Cataract Surgeries18 |
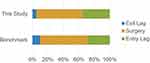 |
Figure 2 Segment analysis showing percentage of time spent for entry lag, the operation, and exit lag. Results of this study are compared with benchmarks for cataract surgery. |
Discussion
Current Practice
The operating room complex of the Department of Ophthalmology is located in another building, separate from the main hospital. The complex is exclusive for ophthalmologic cases only and has its own set of nurses and staff. Because of its isolated environment, the operating room procedures can be more easily observed and attributed to the Department, unlike other departments such as surgery, orthopedics, and otolaryngology, which all share their operating rooms.
The complex opens at 6:00 a.m., with 6:30 a.m. designated as the start time for cases. Patients are already received by 6:00 a.m. and they are prepared for surgery and wheeled into their respective operating rooms. The cut-off for elective surgeries is 11:45 a.m., after which emergency cases are prioritized. Elective cases which have not started by this time are deferred. The patients are sent home and rescheduled for surgery on another date. Thus, having efficient peri-operative processes is important to decrease canceled cases due to cut-off.
Once patients are brought inside the operating room, they are checked by the nurses and attached to oxygen support and monitoring devices. Patient prepping and scrubbing are done by the first- or second-year residents and can only be done inside the respective operating rooms. The previous case has to be wheeled out first before the next patient’s scrubbing can be done. This study observed the flow of processes in consecutive cases of phacoemulsification surgeries scheduled in a single room.
Benchmarking
To the authors’ knowledge, there has been no prior study exploring operating room efficiency for ophthalmologic surgeries in the country, specifically for phacoemulsification. There are also no guidelines and targets for peri-operative efficiency parameters set by the local ophthalmology society. Likewise, there are no operating room targets set by the Department yet. Thus, for this study’s purposes, the key performance indicators were compared with published benchmarks from the OR Benchmarks Collaborative (ORBC), an automated benchmarking service from McKesson Enterprise Intelligence. The ORBC database has 471 subscribers, including acute care hospitals and ambulatory surgical centers in the US, Canada, Saudi Arabia, Australia, and New Zealand.18 It should be noted that this benchmark data did not discriminate between the different types of surgeries, which could have made results of this study falsely high when comparing percentile values. Nonetheless, the most common surgery entered into their database was that of cataract surgery.
Efficiency is measured through the use of different parameters. Most remarkable in the results is that among the 56 operations observed, none started on or before the scheduled “cutting” time of 6:30 a.m. In the study done in the Department of Surgery of the same hospital, only 3.9% of cases started on time, with almost half starting more than an hour late. Furthermore, 54.3% of late starts were caused by the tardiness of surgeons.9 This study is limited because the exact time of arrival of the patients, surgeons, and nurses was not noted since it was not feasible for a single observer to collect them.
Turnaround time (TAT) starts at the first patient’s exit from the operating room until the next patient’s surgery. It comprises three segments: exit lag, turnover time, and entry lag (Figure 1). Results consistently showed that entry lag is the indicator that needed improvement. Entry lag is composed of three time segments, namely, (a) patient entry to room until surgery prep (“patient wait time”), (b) time for surgical preparation and draping (“surgery prep time”), and (c) end of surgery prep until the start of surgery (“surgery lag time”). Thus, decreasing the time spent in these segments can decrease the overall entry lag. Noted general reasons for the delay in this segment included late arrival of pharmacy needs and intraocular lens, sterilization of instruments, and prolonged preparation of other surgical needs and machines.
Segment analysis with data specific for cataract surgery from the same database18 showed an increased preoperative time, accompanied by a proportional decrease in postoperative time, which was consistent with the earlier findings of having a prolonged entry lag (Figure 2). This type of analysis is essential since it shows how much is spent in the surgery itself versus the other procedures surrounding the surgery but not directly contributing to income generation. Having a lower percentage of time spent doing the surgery with increased pre- and postoperative times would characterize an inefficient operating room, while a higher percentage of time spent during the operation would describe an operating room with streamlined processes.
Comparison with International Data
Aside from comparing results with the ORBC database, results were also directly compared to the targets set in another similar study by Kang et al, which, like this study, was done in an urban public tertiary hospital. Their efficiency parameters were also measured during their senior residents’ surgery days performing phacoemulsification using local anesthesia, again very similar to this study. The ideal times they set for each segment were 15 minutes for entry lag, 30 minutes for surgery, 5 minutes for exit lag, and 20 minutes for turnover time.11
Comparing these targets with our results showed increased entry lag, similar to the results of the benchmarking. Operating time was also increased in this study by 13 minutes, which may be due to differences in the residents’ learning curve performing the surgeries. Likewise, the cataract cases scheduled on the intervention days were uncomplicated ones, unlike in this study, wherein there was no exclusion of severe cataract cases.
Many studies have pointed out both controllable and uncontrollable factors and strategies that can be adopted to improve efficiency in the operating room.11,19–21 In a multilevel study comparing the process of cataract surgery in Belgium, process flow was negatively influenced by the severity of the cataract and presence of particular cause variation. On the other hand, the flow was enhanced with topical anesthesia (instead of peribulbar, retrobulbar or general analgesia), surgeons’ experience, use of specialized scrub nurses, and eye clinic design.20 In another study comparing the effect of group goal and group performance theories on operating room efficiency for resident performed surgeries; a multi-professional ophthalmologic surgical team set publicly stated goals and strategies to achieve the target times they set for each segment. At the end of the intervention, they could decrease overall case time from 55 to 46 minutes, allowing for 13 cases in a ten-hour workday.11
Moreover, in a time and motion study of 140 operations across 18 theatre sessions, extreme variability in the number of cases performed, and patient flow efficiency between different institutions was observed.19 In this study, the average time to complete one case was 19.97 minutes. They also found a significant association between the duration of one operation with the number of allied health professionals (AHPs), leading the authors to conclude that supporting the surgeon with sufficient AHPs could improve operational efficiency significantly.19
Application to Local Setting
Computing the total cycle length using the mean data obtained from this study gives four cases that can be done in the five hours allotted for elective surgeries at our institution. However, if cases start at the scheduled time of 6:30 a.m. and entry lag is decreased while maintaining the mean operating time, a total of seven cases can be performed. A change as small as this may be significant since, in an unpublished study by the authors, the total waiting time for cataract surgery at our institution is 80 days. Thus, increasing the number of surgeries that can be done per room will decrease patient waiting time for surgery. Proposed interventions to address this include sterilization of instruments and retrieval of pharmacy needs the day before, attendance checks for surgeons, consecutive cases with the same laterality, and group goal and target time setting.
Strengths and Limitations
Ophthalmologic surgeries, especially that of phacoemulsification cataract surgery, are different from other types of surgeries in that they are shorter, usually only use topical anesthesia, and can be done in quick succession. Thus, the effects of operating room efficiency are more apparent in these types of operations. At present, no other studies examining operating room efficiency in ophthalmology are available in the country. This study was also done with a single third-party observer to eliminate potential bias and differences in observations and data recording.
On the other hand, this study results may have a Hawthorne Effect since the doctors and staff know that such a study is being done. The exact start of recorded observations included in the study was unannounced to minimize this bias. Additionally, the surgeons and nurses did not know which exact rooms were included in the day’s data recording. There was also no contact nor intervention by the third-party observer throughout the study period. Lastly, this study was limited in that only a few cases were observed over a short period. Nevertheless, results were able to pinpoint which specific efficiency parameter needed the most improvement.
Conclusion
This time and motion study determined that entry lag is the performance indicator that should be addressed to improve efficiency because it was consistently increased compared to both benchmark and published targets. Further studies measuring other crucial performance parameters such as preadmission screening, surgical time-out, and primetime utilization, may be done. Likewise, interventional studies, particularly those targeting entry lag, may be initiated to increase operating room efficiency in the Department. Communication with other members of the surgical team and hospital staff, along with group goal-setting, may pave the way for better utilization and delivery of hospital services.
Acknowledgments
Authors would like to thank Alvin Duke R. Sy, RN for help in statistical analysis.
Disclosure
Maria Isabel N Umali reports grants from the Philippine General Hospital Expanded Health Research Office, during the conduct of the study. The authors report no other potential conflicts of interest in this work.
References
1. Pham DN, Klinkert A. Surgical case scheduling as a generalized job shop scheduling problem. Eur J Oper Res. 2008;185(3):1011–1025. doi:10.1016/j.ejor.2006.03.059
2. Gür Ş, Eren T. Application of operational research techniques in operating room scheduling problems: literature overview. J Healthc Eng. 2018;2018:1–15. doi:10.1155/2018/5341394
3. Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233. doi:10.1001/jamasurg.2017.6233
4. Sartini M, Spagnolo AM, Panatto D, Perdelli F, Cristina ML. Improving environmental quality in an operating room: clinical outcomes and economic implications. J Prev Med Hyg. 2013;54(2):75. doi:10.15167/2421-4248/jpmh2013.54.2.376
5. Ahmadi E, Masel DT, Metcalf AY, Schuller K. Inventory management of surgical supplies and sterile instruments in hospitals: a literature review. Health Syst. 2019;8(2):134–151. doi:10.1080/20476965.2018.1496875
6. Pourmohammadi K, Hatam N, Shojaei P, Bastani P. A comprehensive map of the evidence on the performance evaluation indicators of public hospitals: a scoping study and best fit framework synthesis. Cost Eff Resour Alloc. 2018;16(1). doi:10.1186/s12962-018-0166-z
7. Macario A, Vitez TS, Dunn B, McDonald T. Where are the costs in peri-operative care?: analysis of hospital costs and charges for inpatient surgical care. Anesthesiology. 1995;83(6):1138–1144. doi:10.1097/00000542-199512000-00002
8. Fixler T, Wright JG. Identification and use of operating room efficiency indicators: the problem of definition. Can J Surg. 2013;56(4):224–226. doi:10.1503/cjs.020712
9. Lapitan MCM, Buckley BS, Abalajon DD, Cruz PLO, Raymundo MEM. Efficiency status of the elective non-cardiac surgery operating rooms of the department of surgery of the philippine general hospital. Acta Med Philipp. 2013;47(4):30–35.
10. Mpyet CD. An audit of the use of ophthalmic theatre time. J Community Eye Health. 2002;15(44):62.
11. Kang JM, Padmanabhan SP, Schallhorn J, Parikh N, Ramanathan S. Improved utilization of operating room time for trainee cataract surgery in a public hospital setting. J Cataract Refract Surg. 2018;44(2):186–189. doi:10.1016/j.jcrs.2017.11.014
12. Balzer C, Raackow D, Hahnenkamp K, Flessa S, Meissner K. Timeliness of operating room case planning and time utilization: influence of first and to-follow cases. Front Med. 2017;4. doi:10.3389/fmed.2017.00049.
13. Gottschalk MB, Hinds RM, Muppavarapu RC, et al. Factors affecting hand surgeon operating room turnover time. Hand. 2016;11(4):489–494. doi:10.1177/1558944715620795
14. Wiyartanti L, Lim CH, Park MW, Kim JK, Kwon GH, Kim L. Resilience in the surgical scheduling to support adaptive scheduling system. Int J Environ Res Public Health. 2020;17(10):3511. doi:10.3390/ijerph17103511
15. Boggs SD, Tsai MH, Urman RD. The Association of Anesthesia Clinical Directors (AACD) glossary of times used for scheduling and monitoring of diagnostic and therapeutic procedures. J Med Syst. 2018;42(9). doi:10.1007/s10916-018-1022-6
16. Jones LK, Jennings BM, Goelz RM, Haythorn KW, Zivot JB, de Waal FBM. An ethogram to quantify operating room behavior. Ann Behav Med. 2016;50(4):487–496. doi:10.1007/s12160-016-9773-0
17. De GBGS, Llave CL Impact of revised management policies on the efficiency of gynecologic operating room processes in a tertiary training hospital *. 2016.
18. Foster T. Data for benchmarking your OR’s performance. OR Manager. 2012;28(1):13–16.
19. Roberts HW, Myerscough J, Borsci S, Ni M, O’Brart DPS. Time and motion studies of national health service cataract theatre lists to determine strategies to improve efficiency. Br J Ophthalmol. 2018;102(9):1259–1267. doi:10.1136/bjophthalmol-2017-310452
20. De Regge M, Gemmel P, Duyck P, Claerhout I. A multilevel analysis of factors influencing the flow efficiency of the cataract surgery process in hospitals. Acta Ophthalmol. 2016;94(1):31–40. doi:10.1111/aos.12819
21. Pittner AC, Sullivan BR. Resident surgeon efficiency in femtosecond laser-assisted cataract surgery. Clin Ophthalmol. 2017;Volume 11:291–297. doi:10.2147/OPTH.S128626
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
