Back to Journals » Clinical Ophthalmology » Volume 14
Efficacy of Standard and Accelerated (10 Minutes) Corneal Crosslinking in Keratoconus Stabilization
Authors Stock RA , Brustollin G , Mergener RA , Bonamigo EL
Received 14 April 2020
Accepted for publication 9 June 2020
Published 24 June 2020 Volume 2020:14 Pages 1735—1740
DOI https://doi.org/10.2147/OPTH.S258205
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ricardo Alexandre Stock, Gustavo Brustollin, Rafael André Mergener, Elcio Luiz Bonamigo
Medical School of the University of the West of Santa Catarina (Universidade do Oeste de Santa Catarina – UNOESC), Joaçaba Campus, State of Santa Catarina, Brazil
Correspondence: Ricardo Alexandre Stock Email [email protected]
Purpose: To evaluate whether Accelerated CXL for 10 minutes is as effective as standard CXL for 30 minutes for the treatment of progressive keratoconus.
Patients and Methods: Eighty-two eyes of 62 patients with keratometry examinations performed before and 6 months after surgery were studied. A total of 39 eyes underwent standard CXL with UVA irradiation of 3 mW/cm2 for 30 minutes and 32 eyes underwent Accelerated CXL UVA irradiation of 9 mW/cm2 for 10 minutes. The eyes of all patients had corneal thicknesses of at least 450 microns (400 microns after epithelium removal).
Results: The means of the keratometry measurements in the preoperative period for the eyes subjected to standard CXL were 46.27 dioptres (D) on the flat axis (K1) and 48.93 D on the steep axis (K2). Postoperatively, K1 was 46.21 D and K2 was 48.97 D, a difference without statistical significance (p = 0.47 and p = 0.48, respectively). In the Accelerated CXL protocol, the preoperative measurements were 44.55 D and 46.19 D for K1 and K2, respectively. In the postoperative period, K1 was 43.37 D, and K2 was 46.64 D (p = 0.38 and p = 0.27, respectively). In the standard group, the mean maximum keratometry (Kmax) preoperatively was 55.87 D, with no statistical significance (p = 0.29). In the preoperative period, the Kmax of the Accelerated group was 51.15 D, with no statistical significance (p = 0.32).
Conclusion: Based on the keratometry results, the accelerated protocol was as effective as the standard protocol for keratoconus stabilization.
Keywords: corneal diseases, cornea, keratometry, efficacy
Plain Language Summary
Keratoconus is a progressive, non-inflammatory thinning of the cornea that causes the cornea to curve, usually at its centre, into the shape of a cone. Currently, there is only one treatment for disease progression is the corneal crosslinking, which makes the cornea more rigid in order to slow or stop the development of the cone shape. The procedure consists of removing the first layer of the cornea (Epi-off), followed by the instillation of riboflavin, a substance derived from vitamin B12, and the application of ultraviolet A radiation at surgical room. The time of exposure to radiation may vary, and the shortest time without loss of efficacy is desirable, with less complication as possible. We present a study that compares the efficacy of 2 irradiation times: 30 minutes, ie, the standard Dresden protocol, and 10 minutes, ie, the Accelerated protocol. If the efficacy is similar, the Accelerated protocol is more comfortable and potentially causes fewer side effects for the patient.
Introduction
Keratoconus is an ectasia of the cornea that progresses without inflammation but with irregular bilateral astigmatism and visual acuity impairment and had an estimated prevalence of 54.5 per 100,000 inhabitants in 1988.1 A more recent study carried out in the National Patient Register of Denmark, from 1977 to 2015, showed the prevalence of 44 per 100,000 persons.2 However, a multicentre study in Riyad, Saudi Arabia, with patients aged 6 to 21 years, found a prevalence of 4.79% or 1:21 patients.3
In general, keratoconus manifests in early puberty and progresses until the third and fourth decades of life, with progressive thinning and ectatic protrusion of the cornea in the shape of a cone.4 The physiopathology of corneal steepening is still unknown, but it is assumed that repetitive trauma, such as eye scratching, combined with abnormalities in the corneal connective tissue contribute to the progression of the disease.5 ABCD classification is used to stage keratoconus from 0 to IV according to progression based on the posterior and anterior corneal curvature, corneal thickness, best corrected visual acuity and corneal scars.6
Although there have been advances in knowledge, the aetiology of keratoconus has not yet been elucidated. Regarding the genetic aetiology, there seems to be no clear relationship because only approximately 10% of carriers have a positive familial history of the disease.7
Early progressive keratoconus can be corrected with glasses, moderate cases can be corrected with rigid gas permeable (RGP) contact lenses, and more advanced cases can be corrected with lenses with specific designs. If visual acuity is not good, surgical treatment is indicated, such intracorneal ring implantation. In cases of proven progressive disease, corneal crosslinking treatment is indicated.8
For a long time, corneal transplantation was the best solution for advanced keratoconus without the possibility of adaptation to rigid lenses. However, due to the delay in obtaining a compatible cornea for transplantation, treatment was delayed for many patients, impairing their quality of life and that of their families.9
The most recent discovery for the treatment of progressive keratoconus was corneal crosslinking (CXL), which, in biological terms, stimulates the formation of new covalent bonds between the collagen fibres of the cornea, making the cornea more stable; thus, there is a lower tendency for thinning and steepening.5 The indication for corneal crosslinking, regarding keratoconus, is stop the progression of the corneal ectasia or stop the steepening of the cornea.
There are some protocols currently available for CXL that differ with respect to the time and intensity of ultraviolet A (UVA) light irradiation. In the Dresden (or standard) protocol, the patient is subjected to UVA irradiation of 3 mW/cm2 for 30 minutes. However, this method can cause progressive flattening, haze and infiltrates.5 Therefore, other protocols are being used, called Accelerated CXL, with shorter durations and irradiation intensities ranging from 9 minutes with 10 mW/cm2 to 15 minutes with 7 mW/cm2, among others, and variable results have been obtained.8
Recent studies have concluded that the results of the standard and accelerated protocols are similar, including in children, although the results may vary considering irradiance, time and age, indicating the need for further studies to confirm the efficacy of the Accelerated protocol.10,11 The objective of this study was to determine whether Accelerated CXL with UVA irradiation of 9 mW/cm2 for 10 minutes is as effective as standard CXL with UVA irradiation of 3 mW/cm2 for 30 minutes in controlling the progression of keratoconus.
Patients and Methods
A retrospective study was conducted with data collected from 82 eyes of 62 patients with a mean age of 22.16 years, 40 men and 22 women, who were subjected to Accelerated CXL and standard CXL. Two groups were established: group 1 included 39 eyes of patients who underwent standard CXL with UVA irradiation of 3 mW/cm2 applied for 30 minutes; group 2 included 32 eyes of patients who underwent Accelerated CXL with UVA irradiation of 9 mW/cm2 for 10 minutes.
The inclusion criteria were patients with progressive keratoconus and a minimal corneal thickness of 450 microns. We included patients who had at least 0.75 D progressive steepening of the anterior corneal surface associated with progressive steepening of the posterior corneal surface, in two consecutive exams at least 6 months apart.11,12
The exclusion criteria were patients with a corneal thickness of less than 450 microns, those previously treated (CXL or ring implant) and those who did not complete the minimum follow-up of 6 months. Keratometry measurements were obtained using a WaveLight Topolyzer topographic system.
A pachymetry map was obtained in the preoperative period via corneal tomography performed with a Scheimpflug camera (Pentacam, Oculus) with the sole aim of determining the minimum treatable thickness of 450 microns. Data and keratometry measurements of patients from both groups were collected preoperatively and at least 6 months after the surgical procedure.
The procedure conducted using the standard CXL protocol is described below:
- Instillation of 1% pilocarpine eye drops 30 minutes before the procedure, twice;
- In the operating room, under aseptic conditions, the patient is laid on her back;
- Administration of topical anaesthesia, such as 1% tetracaine hydrochloride with 0.1% phenylephrine hydrochloride;
- Asepsis of the skin around the eye with iodine antiseptic, twice;
- Application of 5% polyvidone iodine and anaesthetic (1% tetracaine hydrochloride with 0.1% phenylephrine hydrochloride) 5 minutes before and immediately before the procedure;
- Placement of a sterile disposable drape;
- Insertion of a speculum to keep the eye open;
- Delimitation of the central 9.0 mm of the cornea with a circular corneal marker;
- Removal of the central 8 mm of the corneal epithelium by debridement. Verification of the minimal corneal thickness of 400 microns using a portable pachymeter. Application of 400 osmol riboflavin with 1% methylcellulose every 3 minutes for 30 minutes;
- Corneal irradiation with a 370-nm UVA light at an irradiance of 3 mW/cm2 (5.4 J/cm2 surface dose) and a distance of 4.5 cm for 30 minutes, application using an Opto X-link (Opto, Brazil) device;
- During irradiation, 400 osmol riboflavin is applied to the cornea every 5 minutes, adding topical anaesthesia (1% tetracaine hydrochloride with 0.1% phenylephrine hydrochloride) if necessary; and
- At the end of irradiation, a soft contact lens bandage is placed and maintained until complete re-epithelialization.
In the Accelerated CXL protocol, the same surgical technique was performed but with the irradiance increased from 3 mW/cm2 to 9 mW/cm2 (5.4 J/cm2 surface dose) and the time of UVA irradiation decreased from 30 minutes to 10 minutes.
The principles of the Declaration of Helsinki were followed, and approval was obtained from the Research Ethics Committee of University of the West of Santa Catarina (Universidade do Oeste de Santa Catarina – UNOESC) under number 2,684,055. Patient consent to review their medical records was not necessary because the confidentiality of patient data was guaranteed.
Results
The keratometry measurements performed before surgery for the group subjected to standard CXL (group 1) were 46.27 dioptres (D) (± 4.30 D standard deviation (SD)) in the flat axis (K1) and 48.93 D (± 4.8 D SD) in the steep axis (K2). In the postoperative period, K1 and K2 were 46.21 D (± 4.89 D SD) and 48.97 D (± 5.59 D SD), respectively; these differences were not statistically significant (p = 0.47 and p = 0.48, respectively).
For the Accelerated protocol (group 2), the keratometry measurements obtained before surgery were 44.55 D (± 2.91 D SD) in K1 and 46.19 D (± 3.43 D SD) in K2. In the postoperative period, K1 and K2 were 43.37 D (± 2.50 D SD) and 46.64 D (± 3.21 D SD), and the differences were not statistical significant (p = 0.38 and p = 0.27, respectively).
In the preoperative period, the mean maximum keratometry (Kmax) in the standard group (group 1) was 55.87 D (± 7.85 D SD) and 56.69 D (± 8.55 D SD). This difference was not statistically significant (p = 0.29). For the Accelerated group, in the preoperative period, the mean Kmax (group 2) was 51.15 D (± 5.36 D SD), and in the postoperative period, the mean Kmax was 51.66 D (± 5.54 D SD), with no statistically significant difference (p = 0.32). The results are shown in Table 1.
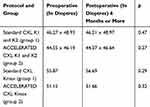 |
Table 1 Keratometry Measurements of the Eyes Subjected to the 2 Protocols |
Discussion
The main objective of corneal CXL is to stabilize the progression of keratoconus by stopping the progressive steepening and thinning of the cornea. Thus, an excellent parameter for determining treatment efficacy is keratometry measurements obtained with Placido rings to determine the topography, providing a more accurate reading of corneal topography compared to that determined via tomographic methods that simulate corneal topography measurements. For this reason, we prefer these measurements over Scheimpflug tomography. In our study, a Pentacam camera was used only to obtain a preoperative pachymetry map.
Because of the frequent side effects associated with the standard technique, new protocols are needed.5 Line of sight loss, haze and progressive flattening are already well defined in research studies. Thus, we opted to adhere to pre- and postoperative keratometry measurements without studying other effects.
The keratometry measurements of the flat axis and steep axis were reduced after surgery in the group subjected to standard CXL (Table 1). These differences were not statistically significant (p = 0.47 and p = 0.48, respectively). The mean Kmax also decreased after surgery in this group, but the difference was not statistically significant (p = 0.29). These findings confirm the efficacy of the standard protocol for maintaining disease stability during the follow-up period in the patients included in our study.
One study showed that the standard protocol with a 12-month follow-up after surgery resulted in a statistically significant Kmax reduction from 49.19 to 46.96 D (p < 0.05).12 A similar result was obtained in another study that used the standard CXL protocol with 3 mW/cm2 for 30 minutes, obtaining a statistically significant reduction in Kmax (p = 0.003).13 The present study obtained a smaller, statistically nonsignificant reduction, ranging from 55.87 D to 56.69 D (p = 0.29), with standard CXL. However, using the Dresden protocol, the curvature of the cornea stabilized, and keratoconus progression stopped.
In the long term, standard CXL provides good results and reduces the Kmax. Using standard CXL, Iqbal et al14 reduced keratoconus, with the Kmax varying from 51.95 to 50.19 (p = 0.0001) over a period of 5 years. In a study by Ghanem et al,15 also with standard CXL, the reduction in Kmax after 2 years was statistically significant (p < 0.001). In our study, stabilization occurred, but the results were not statistically significant, perhaps due to the shorter follow-up period (6 months). The results obtained by Madeira et al10 were also statistically not significant over a follow-up period of 12 months.
The Accelerated CXL (9 mW/cm2) used in the study by Khairy et al12 showed no significant difference (p = 0.388) in Kmax at a follow-up of approximately 14 months. This result is consistent with the results of our study because a statistically nonsignificant result was obtained using the same curved axis keratometry (Kmax) using the same Accelerated CXL protocol.
All postoperative keratometry measurements (Table 1) in the Accelerated CXL group also decreased during the course of our study. These differences were not significant (p = 0.38 on the flat axis and p = 0.27 on the steep axis). The Kmax also decreased in the postoperative period in the Accelerated CXL group, but this difference was not significant (p = 0.32), thus demonstrating that Accelerated CXL was also effective in maintaining disease stability during the follow-up period of our study. Based on these data, both methods can be considered effective for treating the disease.
In search of alternatives, Mita et al16 used 3 minutes of 30 mW/cm2 UVA irradiation, obtaining satisfactory results regarding keratometry measurements, with the Kmax ranging from 49.95 in the preoperative period to 49.19 after 6 months; this difference was statistically significant (p < 0.05). In the present study, with Accelerated CXL for 10 minutes with 9 mWcm2 UVA irradiation, there was a reduction in the Kmax from 55.87 to 56.69, without statistical significance.
In the study by Alnawaiseh et al,17 an accelerated CXL protocol involving 18 mW/cm2 UVA irradiation for 5 minutes interrupted keratoconus progression at 21.7 months of follow-up after surgery, with a statistically significant reduction in Kmax (p = 0.018). The present study (Accelerated CXL) used a 10-minute protocol with 9 mW/cm2 UVA irradiation and obtained topographic stabilization or reduced the Kmax, but the difference was not significant.
According to Lang et al,18 standard CXL (3 mW/cm2 for 30 minutes), performed in 35 eyes of 26 patients with a 12-month follow-up, achieved stabilization in 97.1% of the patients based on Kmax, demonstrating that the procedure effectively stabilized the curvature of the cornea.16 In turn, the Accelerated protocol (9 mW/cm2 for 10 minutes) obtained a corneal stability index of 93.10%. Analysing the results from protocols used in the study by Lang et al18 and in our study, we can conclude that both stabilized or reduced the keratometry values and that this parameter is adequate for demonstrating the efficacy of the Accelerated and standard protocols.
A study conducted by Nicula et al11 concluded that after a 4-year follow-up, standard CXL reduced K1 from 47.41 D to 45.36 D (p = 0.004) and K2 from 51.98 D to 50.21 D (p = 0.0078), thus significantly contributing to the stabilization of keratoconus. In the Accelerated CXL protocol with 9 mW/cm2 UVA irradiation for 10 minutes, there was also a reduction in K1 values, which decreased from 46.97 D to 44.96 D (p = 0.0048), and in K2 values, which decreased from 50.55 D to 48.75 D (p = 0.0287).
The Accelerated CXL procedure is relatively new in ophthalmology. Therefore, a greater number of studies must be performed including biomechanical aspects, with a longer follow-up time because safety, speed and comfort for patients are essential requirements in the path towards a standardized procedure to stop keratoconus progression, minimizing complications.15,19
Conclusions
The results of this study allow concluding that according to the keratometry measurements obtained in the 6-month period, Accelerated CXL for 10 minutes is as effective as standard CXL for keratoconus stabilization in this period with our patients. Complications associated with standard CXL, such as corneal haze, progressive flattening and the presence of infiltrates justify the search for alternative methods to reduce the negative effects of the procedure and thus benefit future patients. The main limitation of our study is the follow-up time. Studies with a greater number of patients and longer observation times are necessary to confirm the efficacy of Accelerated CXL and decrease the side effects of standard CXL.
Abbreviations
CXL, crosslinking; Accelerated CXL, accelerated crosslinking for 10 minutes; K1, flat axis keratometry; K2, steep axis keratometry; Kmax, mean maximum keratometry; Kmin, mean minimum keratometry; UVA, ultraviolet A.
Data Sharing Statement
Data are available upon reasonable request to the corresponding author.
Ethics
This study was reviewed and approved by the Research Ethics Committee of UNOESC under number 2.684.055.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, provided final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi:10.1016/S0039-6257(97)00119-7
2. Bak-Nielsen S, Ramlau-Hansen CH, Ivarsen A, Plana-Ripoll O, Hjortdal J. Incidence and prevalence of keratoconus in Denmark - an update. Acta Ophthalmol. 2019;97(8):752–755. doi:10.1111/aos.14082
3. Torres Netto EA, Al-Otaibi WM, Hafezi NL, et al. Prevalence of keratoconus in pediatric patients in Riyadh, Saudi Arabia. Br J Ophthalmol. 2018;102(10):1436–1441. doi:10.1136/bjophthalmol-2017-311391
4. Bouheraoua N, Jouve L, El Sanharawi M, et al. Optical coherence tomography and confocal microscopy following three different protocols of corneal collagen-crosslinking in keratoconus. Invest Ophthalmol Vis Sci. 2014;55(11):7601–7609. doi:10.1167/iovs.14-15662
5. Santhiago M. Corneal crosslinking: the standard protocol. Rev Bras Oftalmol. 2017;76(1):43–49. doi:10.5935/0034-7280.20170010
6. Belin MW, Duncan JK. Keratoconus: the ABCD grading system. Klin Monbl Augenheilkd. 2016;233(6):701–707. doi:10.1055/s-0042-100626
7. Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:ID795738. doi:10.1155/2015/795738
8. Horovitz R, Garcia R, Bechara S. Crosslinking: an updated and effective insight. Rev Bras Oftalmol. 2015;74(2):119–123. doi:10.5935/0034-7280.20150027
9. Zeschau A, Balestrin I, Stock R, Bonamigo E. Indications of keratoplasty: a retrospective study in a university hospital. Rev Bras Oftalmol. 2013;72(5):316–320. doi:10.1590/S0034-72802013000500007
10. Madeira C, Vasques A, Beato J, et al. Transepithelial accelerated versus conventional corneal collagen crosslinking in patients with keratoconus: a comparative study. Clin Ophthalmol. 2019;13:445–452. doi:10.2147/OPTH.S189183
11. Nicula CA, Rednik AM, Bulboaca AE, Nicula D. Comparative results between “Epi-Off” conventional and accelerated corneal collagen crosslinking for progressive keratoconus in pediatric patients. Ther Clin Risk Manag. 2019;15:1483–1490. doi:10.2147/TCRM.S224533
12. Khairy HA, Marey HM, Ellakwa AF. Epithelium-on corneal cross-linking treatment of progressive keratoconus: a prospective, consecutive study. Clin Ophthalmol. 2014;8:819–823. doi:10.2147/OPTH.S60453
13. Ng AL, Chan TC, Cheng AC. Conventional versus accelerated corneal collagen cross-linking in the treatment of keratoconus. Clin Exp Ophthalmol. 2016;44(1):8–14. doi:10.1111/ceo.12571
14. Iqbal M, Elmassry A, Badawi AE, Gharieb HM, Said OM. Visual and refractive long-term outcomes following standard cross-linking in progressive keratoconus management. Clin Ophthalmol. 2019;13:2477–2488. doi:10.2147/OPTH.S232954
15. Ghanem RC, Santhiago MR, Berti T, Netto MV, Ghanem VC. Topographic, corneal wavefront, and refractive outcomes 2 years after collagen crosslinking for progressive keratoconus. Cornea. 2014;33(1):43–48. doi:10.1097/ICO.0b013e3182a9fbdf
16. Mita M, Waring GO, Tomita M. High-irradiance accelerated collagen crosslinking for the treatment of keratoconus: six-month results. J Cataract Refract Surg. 2014;40(6):1032–1040. doi:10.1016/j.jcrs.2013.12.014
17. Alnawaiseh M, Rosentreter A, Bohm MR, Eveslage M, Eter N, Zumhagen L. Accelerated (18 mW/cm2) corneal collagen cross-linking for progressive keratoconus. Cornea. 2015;34(11):1427–1431. doi:10.1097/ICO.0000000000000578
18. Lang PZ, Hafezi NL, Khandelwal SS, Torres-Netto EA, Hafezi F, Randleman JB. Comparative functional outcomes after corneal crosslinking using standard, accelerated, and accelerated with higher total fluence protocols. Cornea. 2019;38(4):433–441. doi:10.1097/ICO.0000000000001878
19. Greenstein SA, Fry KL, Bhatt J, Hersh PS. Natural history of corneal haze after collagen crosslinking for keratoconus and corneal ectasia: scheimpflug and biomicroscopic analysis. J Cataract Refract Surg. 2010;36(12):2105–2114. doi:10.1016/j.jcrs.2010.06.067
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
