Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Efficacy of negative pressure wound therapy using vacuum-assisted closure combined with photon therapy for management of diabetic foot ulcers
Authors Hu X, Lian W, Zhang X, Yang X, Jiang J, Li M
Received 30 January 2018
Accepted for publication 30 May 2018
Published 25 October 2018 Volume 2018:14 Pages 2113—2118
DOI https://doi.org/10.2147/TCRM.S164161
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang

Xiaoxiao Hu,1,* Weishuai Lian,1,* Xiaojun Zhang,2,* Xue Yang,3,* Jinxia Jiang,4 Maoquan Li1
1Department of Interventional Vascular Surgery, The Tenth People’s Hospital affiliated to Tongji University, Tongji University School of Medicine, Shanghai, 200072, China; 2Department of Interventional Catheter, The Tenth People’s Hospital affiliated to Tongji University, Shanghai, 200072, China; 3Department of Anesthesiology, Eastern Hospital Affiliated to Tongji University, Shanghai, 200120, China; 4Department of Emergency, The Tenth People’s Hospital affiliated to Tongji University, Shanghai, 200072, China
*These authors contributed equally to this work
Background: Diabetes mellitus, one of the most prevalent chronic metabolic diseases, causes many complications. Among the complications, one of the most common chronic complications is diabetic foot ulcers (DFUs).
Objective: This study was conducted to investigate the efficacy of negative pressure wound therapy using vacuum-assisted closure (VAC) combined with photon therapy for the management of DFUs.
Patients and methods: The study included a total of 69 patients with DFUs during the period from January 2014 to December 2015. All patients were diagnosed with DFUs with Wagner’s stage 2 or 3 and were divided into two groups – the VAC group in which patients received only VAC and the combined group in which patients received both VAC and photon therapy. Data on duration of the treatment, pre- and postoperative wound surface areas, dressing changing times, pain conditions assessed using visual analog scale scores, recurrence rate and amputation rate were collected.
Results: Among all patients, 35 patients were divided into the VAC group and 34 patients into the combined group. Areas of foot ulcers for all patients ranged from 5 to 100 cm2. The treatment duration, dressing changing times and the peak value of visual analog scale scores were all significantly lower in the combined group compared with the VAC group (P<0.05). However, the reduced area for wound surface showed no significant difference between the two groups. Both recurrence and amputation rates showed no significant difference between the two groups of patients.
Conclusion: Both VAC and VAC combined with photon therapy were effective and safe in the treatment of DFUs, while the combined therapy might have accelerated wound healing, but did not influence the long-term efficacy.
Keywords: diabetic foot ulcer, vacuum-assisted closure, photon therapy
Introduction
Diabetes mellitus, one of the most prevalent chronic metabolic diseases, has been estimated to affect over 200 million adults worldwide and the incidence is still rising.1,2 Diabetes mellitus can cause a lot of complications, and diabetic patients are more likely to develop complications such as obesity, stroke, coronary heart disease, diabetic retinopathy, diabetic nephropathy and diabetic neuropathy.3–5 Studies show that compared with the cost of treating diabetes, more costs are spent on treating diabetic complications.6
Among the complications, one of the most common chronic complications is diabetic foot ulcers (DFUs), which are disabling and affect about 15% of people with diabetes.7 DFUs are considered to be associated with diabetic neuropathy and peripheral vascular disease and can lead to infection, gangrene and may ultimately lead to amputation.8,9 The treatment of DFUs is considered to be complex, and ulcers can often remain unhealed for months, even years.10 It is estimated that >85% of foot amputations in patients are caused by DFUs.11
Treatment success for DFUs depends on the mechanisms of action of the therapy, ulcer chronicity and patient compliance. Several treatment approaches have been already reported and have certainly improved DFU patients’ conditions, such as advanced moist wound therapy,12 bioengineered tissue or skin substitutes,13 growth factors,14 electric stimulation15 and negative pressure wound therapy (NPWT) using vacuum-assisted closure (VAC) method.16 However, due to the complexity of treatment of DFUs, the medical treatment of DFU remains challenging. NPWT by VAC is a noninvasive system creating a localized controlled negative pressure environment.17 VAC technology uses controlled application of negative pressure to the wound, in which specially designed open-pore foam dressings are cut to the shape of the wound and a vacuum unit gives continuous or intermittent subatmospheric pressure.18
Photon therapy is reported to be widely used in treatment of cancers.19 It was reported that since the mid-20th century, photon therapy has been used as a standard adjuvant treatment for treating tumors.19 Some studies also show that photon therapy is effective in treatment of leg ulcers20 and cutaneous wounds.21 However, few studies have reported the efficacy of photon therapy in DFUs. In the present study, we report the application of VAC combined with photon therapy as the treatment for DFU patients. This study may give more clinical evidence for the application of VAC and photon therapy, as well as improve our understanding of the treatment of DFUs.
Patients and methods
Patients
The present retrospective study included a total of 69 patients with DFUs who were admitted to our hospital during the period from January 2014 to December 2015. All patients were diagnosed with DFUs with Wagner’s stage 2 or 3.22 Areas of foot ulcers for all patients ranged from 5 to 100 cm2 on calcaneal, dorsal or plantar after debridement. For all patients, traditional methods such as advanced moist wound therapy dressing were used for >2 months and were not effective. Patients with the following characteristics were excluded: 1) patients with other vascular lesions or dermatosis such as active Charcot arthropathy; 2) patients with severe diabetic complications such as diabetic nephropathy or diabetic cardiovascular diseases; and 3) patients with cancers and other severe systemic diseases such as collagen vascular disease or systemic infection. All patients were divided into two groups according to the treatments they received: the VAC group in which patients received only VAC and the combined group in which patients received both VAC and photon therapy. Informed written consents were obtained from all patients. The present study was approved by the ethics committee of the Tenth People’s Hospital affiliated to Tongji University.
For both groups of patients, conventional therapy and surgical debridement were applied including glucose control, surgical debridement to remove necrotic tissues and postoperative washing with 1.5% hydrogen peroxide solution, physiological saline ten times diluted Anerdian III skin disinfectant and 0.9% saline, and infection control using appropriate antibiotics if necessary. For NPWT using VAC, a negative pressure system provided by KCI company (San Antonio, TX, USA) was used. Sterile polyurethane foam dressing was designed according to the shape of ulcers and was covered with adhesive drape to create an airtight seal. Continuous negative pressure ranging from 80 to 125 mmHg was maintained. After debridement, the wound surface was washed with 0.9% saline for 3–5 days. The growth of granulation and the condition of wound were examined every day; dressing change and flaps or skin grafts were considered if necessary. The treatment was continued until ulcer closure.
For the combined group, except for the same VAC strategy, Carnation-11 photon therapeutic apparatus (Lifotronic, Shenzhen, China) was used to provide irradiation with a central wavelength of 640±10 nm and an optical power density of 230 mW/cm2. The irradiation was performed five times every day, which lasted for 10 minutes each time. The treatment was continued until ulcer closure.
For both the groups, nursing management strategies were performed including mental intervention to relax the patients; monitoring patients’ conditions such as blood circulation, skin color, temperature, swelling, limb sensation and movement; monitoring the drainage tube to ensure its function; and monitoring the dressing condition.
Data collection
For all patients, demographic data such as age, gender and the course of disease were collected. Clinical outcomes such as DFU stage, duration of the treatment, pre- and postoperative wound surface areas, dressing changing times, pain conditions assessed using visual analog scale scores, recurrence rate and amputation rate were also collected and analyzed. The pictures of the wound surface were taken using a digital camera, and measurement of the wound surface was performed with ImageJ software. All patients were followed up for 1 year after admission.
Statistical analysis
The measurement data were expressed as median (range). Comparison between two groups was performed using the Mann–Whitney U test. Categorical variables were analyzed using chi-squared test or Fisher’s exact test. P-value <0.05 was considered to be statistically significant. All calculations were made using SPSS 18.0.
Results
Basic clinical information of all patients
A total of 69 DFU patients were included in this retrospective study. Forty-one patients were male and 28 patients were female, with a median age range of 60 (51–69). Among all patients, 35 patients formed the VAC group with a male:female ratio of 20:15 and a median age range of 61 (51–69) and 34 patients formed the combined group with a male:female ratio of 21:13 and a median age of 60 (52~68). Areas of foot ulcers for all patients ranged from 5 to 100 cm2. As shown in Table 1, age, gender, course of disease, DFU stage and preoperative wound surface area showed no significant difference between the two groups of patients.
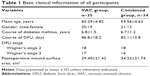  | Table 1 Basic clinical information of all participants |
Comparison of clinical outcomes between the two groups of patients
As shown in Table 2, clinical outcomes including duration of the treatment, pre- and postoperative wound surface areas, dressing changing times and pain conditions were analyzed and compared between the two groups. Results showed that the treatment duration, dressing changing times and the peak value of visual analog scale scores were all significantly lower in the combined group compared to the VAC group (P<0.05). However, the reduced area for wound surface showed no significant difference between the two groups, suggesting that the combined therapy might have accelerated wound healing, but did not influence the long-term efficacy.
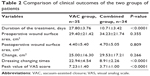  | Table 2 Comparison of clinical outcomes of the two groups of patients |
Comparison of recurrence and amputation rates between the two groups of patients
Lastly, we compared the recurrence and amputation rates between the two groups of patients. Thirty patients in the VAC group and 30 patients in the combined group recovered well with no recurrence (Figure 1). Both recurrence and amputation rates showed no significant difference between the two groups of patients (Table 3), indicating both the treatments had similar safety.
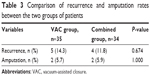  | Table 3 Comparison of recurrence and amputation rates between the two groups of patients |
Discussion
Due to the complexity involved in the treatment of DFUs, ulcers can often remain unhealed for a long time and, thus, place burden on the health care resources due to prolonged hospitalization, rehabilitation and home nursing care treatment.23 Moreover, once a DFU has developed, the development of wound progression may ultimately lead to amputation, which will greatly damage the health and life of the patients. At present, most of the clinical treatment strategies are not thought to be efficient enough to guarantee adequate DFU healing, which propels all medical researchers to develop new treatment approaches. It was reported that the NPWT using VAC is more effective than traditional advanced moist wound therapy, with significant improvements in wound volume and healing rates as well as much more treatment costs. Although the clinical effectiveness of VAC therapy is well established, few studies have focused on the efficacy of photon therapy for the management of DFUs. In the present study, we, for the first time, reported the efficacy of VAC combined with photon therapy in the treatment of DFUs.
Our study demonstrated that both VAC and VAC combined with photon therapy were effective in the treatment of DFUs, while the combined therapy might have accelerated wound healing, but did not influence the long-term efficacy. Gupta et al demonstrated that photon therapy was effective in the treatment of leg ulcers.20 In an animal study, Leite et al showed that photon therapy could promote healing of cutaneous wounds in undernourished rats.21 Both these studies showed that photon therapy might be effective in DFUs, and we are the first to demonstrate the efficacy of photon therapy in the treatment of DFUs.
Recurrence and amputation rates for both the methods were similar, indicating that the photon therapy was also safe in the treatment of DFUs. Günal et al studied the efficacy of VAC and GranuFoam Silver dressing in the management of DFUs and found that combined use of VAC and GranuFoam Silver dressing could significantly reduce the recurrence rate of DFUs compared with traditional advanced moist wound therapy.24 Armenio et al demonstrated that combined use of bioengineered tissue and VAC could also significantly reduce both recurrence and amputation rates of DFUs, compared with the standard method based on surgical debridement, moist dressing, off-load and autologous skin grafts.25 In the present study, we found that combined use of VAC and photon therapy had similar recurrence and amputation rates compared with only VAC. This difference might be due to different control groups and comparisons, but could still demonstrate the safety and efficacy of the combined treatment strategy.
Conclusion
In conclusion, we conducted a retrospective study to compare the efficacy of VAC and VAC combined with photon therapy for the management of DFUs. Results showed that both VAC and VAC combined with photon therapy were effective and safe in the treatment of DFUs, while the combined therapy might have accelerated wound healing, but did not influence the long-term efficacy. This study may give more clinical evidence for the application of VAC and photon therapy, as well as improve our understanding of the treatment of DFUs.
Acknowledgments
This work was supported by the project (The Mechanism of LncRNA-MALAT1 Regulating Endothelial Progenitor Cells Biological Function in Diabetic Angiopathies) No 81671793 and the Fundamental Research Funds for the Central Universities (No 22120170092).
Disclosure
The authors report no conflicts of interest in this work.
References
Diet MJE. Lifestyle, and the Risk of Type 2 Diabetes Mellitus in Women – NEJM. New England Journal of Medicine. 2001;345(11):790–797. | ||
Gr J. Effects of Combination Lipid Therapy in Type 2 Diabetes Mellitus – NEJM. New England Journal of Medicine. 2010;362(17):1563–1574. | ||
Wu T, Xie G, Ni Y, et al. Serum metabolite signatures of type 2 diabetes mellitus complications. J Proteome Res. 2015;14(1):447–456. | ||
Alvarez CA, Lingvay I, Vuylsteke V, Koffarnus RL, Mcguire DK. Cardiovascular Risk in Diabetes Mellitus: Complication of the Disease or of Antihyperglycemic Medications. Clin Pharmacol Ther. 2015;98(2):145–161. | ||
Yigit S, Karakus N, Inanir A. Association of MTHFR gene C677T mutation with diabetic peripheral neuropathy and diabetic retinopathy. Mol Vis. 2013;19(30):1626–1630. | ||
Bao X, Yang C, Fang K, Shi M, Yu G, Hu Y. Hospitalization costs and complications in hospitalized patients with type 2 diabetes mellitus in Beijing, China. J Diabetes. 2017;9(4):405–411. | ||
Alavi A, Sibbald RG, Mayer D, et al. Diabetic foot ulcers. J Am Acad Dermatol. 2014;(1):21(e21–e24). | ||
Chin YF, Liang J, Wang WS, Hsu BR, Huang TT. The role of foot self-care behavior on developing foot ulcers in diabetic patients with peripheral neuropathy: a prospective study. Int J Nurs Stud. 2014;51(12):1568–1574. | ||
Hingorani A, Lamuraglia GM, Henke P, et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;633S(2 Suppl):3S–21S. | ||
Moura LI, Dias AM, Carvalho E, de Sousa HC. Recent advances on the development of wound dressings for diabetic foot ulcer treatment – a review. Acta Biomater. 2013;9(7):7093–7114. | ||
Shojaiefard A, Khorgami Z, Larijani B. Independent risk factors for amputation in diabetic foot. Int J Diabetes Dev Ctries. 2008;28(2):32. | ||
Cychosz CC, Phisitkul P, Belatti DA, Wukich DK. Current Concepts Review: Preventive and Therapeutic Strategies for Diabetic Foot Ulcers. Foot & Ankle International. 2015;37(3):334. | ||
Widgerow AD. Bioengineered skin substitute considerations in the diabetic foot ulcer. Ann Plast Surg. 2014;73(2):239. | ||
Dumantepe M, Fazliogullari O, Seren M, Uyar I, Basar F. Efficacy of intralesional recombinant human epidermal growth factor in chronic diabetic foot ulcers. Growth Factors. 2015;33(2):128–132. | ||
Kwan RL, Cheing GL, Vong SK, Lo SK, Sk L. Electrophysical therapy for managing diabetic foot ulcers: a systematic review. Int Wound J. 2013;10(2):121–131. | ||
Isaac AL, Armstrong DG. Negative pressure wound therapy and other new therapies for diabetic foot ulceration: the current state of play. Med Clin North Am. 2013;97(5):899–909. | ||
Ulusal AE, Sahin MS, Ulusal B, Cakmak G, Tuncay C. Negative pressure wound therapy in patients with diabetic foot. Acta Orthop Traumatol Turc. 2011;45(4):254–260. | ||
Venturi ML, Attinger CE, Mesbahi AN, Hess CL, Graw KS. Mechanisms and clinical applications of the vacuum-assisted closure (VAC) Device: a review. Am J Clin Dermatol. 2005;6(3):185–194. | ||
Simone, II CB, Kramer K, O’Meara WP, et al. Comparison of Predicted Excess Secondary Malignancies Between Proton and Photon Radiation Therapy for Treatment of Stage I Seminoma. International Journal of Radiation Oncology Biology Physics. 2012;82(1):242. | ||
Gupta A, Telfer J, Filonenko N, Salansky N, Sauder D. The use of low-energy photon therapy in the treatment of leg ulcers – a preliminary study. Journal of Dermatological Treatment. 1997;8(2):103–108. | ||
Leite SN, Andrade TA, Masson-Meyers DS, Leite MN, Enwemeka CS, Frade MA. Phototherapy promotes healing of cutaneous wounds in undernourished rats. An Bras Dermatol. 2014;89(6):899–904. | ||
Nagoba BS, Gandhi RC, Wadher BJ, Rao A, Hartalkar AR, Selkar SP. A simple and effective approach for the treatment of diabetic foot ulcers with different Wagner grades. Int Wound J. 2010;7(3):153–158. | ||
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37(3):651–658. | ||
Günal Ö, Tuncel U, Turan A, Barut S, Kostakoglu N. The Use of Vacuum-Assisted Closure and GranuFoam Silver® Dressing in the Management of Diabetic Foot Ulcer. Surg Infect. 2015;16(5):558. | ||
Armenio A, Cutrignelli DA, Nardulli ML, et al. Bio-Engineering tissue and V.A.C. therapy: A new method for the treatment of extensive necrotizing infection in the diabetic foot. Annali Italiani Di Chirurgia. 2017;88:268–274. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

