Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Efficacy of light therapy on nonseasonal depression among elderly adults: a systematic review and meta-analysis
Authors Chang CH , Liu CY , Chen SJ , Tsai HC
Received 15 July 2018
Accepted for publication 22 October 2018
Published 14 November 2018 Volume 2018:14 Pages 3091—3102
DOI https://doi.org/10.2147/NDT.S180321
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Chun-Hung Chang,1,2 Chieh-Yu Liu,3 Shaw-Ji Chen,4,5 Hsin-Chi Tsai6,7
1Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan; 2Department of Psychiatry & Brain Disease Research Center, China Medical University Hospital, Taichung, Taiwan; 3Biostatistical Consulting Laboratory, Department of Speech Language Pathology and Audiology, National Taipei University of Nursing and Health Sciences, Taipei, Taiwan; 4Department of Psychiatry, Mackay Memorial Hospital Taitung Branch, Taitung, Taiwan; 5Department of Medicine, Mackay Medical College, New Taipei, Taiwan; 6Department of Psychiatry, Tzu-Chi General Hospital, Hualien City, Taiwan; 7Department of Psychiatry, School of Medicine, Tzu-Chi University, Hualien City, Taiwan
Objective: The aim of this study was to examine the effectiveness of light therapy in the treatment of geriatric depression.
Methods: A systematic review and meta-analysis were carried out. Data sources for the literature search were PubMed, Cochrane Collaboration’s Central Register of Controlled Clinical Trials, Cochrane Systematic Reviews, and ClinicalTrials.gov. Controlled trials of light therapy on older patients with nonseasonal depression and depression rating scales were eligible. Studies were pooled using a random-effect model for comparisons with light therapy. We used effect size (ES), which expresses changes in depression severity, in each selected meta-analysis to calculate the standardized mean difference on the basis of Hedges’ adjusted g; positive values indicated that the depression severity improved after light therapy. All results were presented with 95% CIs. Statistical heterogeneity was explored through visual inspection of funnel plots and the I2 statistic. Moderators of effects were explored using meta-regression.
Results: We identified eight trials involving 395 participants that met the inclusion criteria. Light therapy was significantly more effective than comparative treatments, including placebo or dim light, with an ES of 0.422 (95% CI: 0.174–0.709, P=0.001). In addition, six of the eight trials used bright (white) light, resulting in significantly reduced severity of geriatric depression (N=273, ES: 0.460, 95% CI: 0.085–0.836, P=0.016). Furthermore, pale blue light therapy reduced the severity of geriatric depression (N=89, ES: 0.464, 95% CI: 0.046–0.882, P=0.030).
Conclusion: Our results highlighted the significant efficacy of light therapy in the treatment of geriatric depression. Additional well-designed, controlled studies are necessary to adopt standard parameters, adequate group sizes, and randomized assignment to evaluate more thoroughly the efficacy of light therapy for treating geriatric depression.
Keywords: depression, elderly adults, light therapy
Corrigendum for this paper has been published
Introduction
Depressive disorders are characterized by sadness or irritability and are associated with several psychophysiological changes.1 In USA, the lifetime prevalence of depression is 11.9% (major depressive disorder, 10.6%; dysthymia, 1.3%) in elderly adults (age >60 years).2 Older adults with depression have a higher risk of suicide and comorbidities than do older adults without depression.3 Moreover, depression is the leading cause of disability, and the economic burden that it causes increases as the population ages.4 Psychotherapy and antidepressants are the major treatment modalities for depression in elderly adults.5,6 However, psychotherapy is limited by the availability of psychologists or psychiatrists,5,7 and geriatric patients are at a higher risk of experiencing side effects from antidepressants than are other populations.8,9 Therefore, augmented non-pharmacologic treatments have been developed for the treatment of depression in elderly patients.
Light therapy (phototherapy), a non-pharmacologic treatment, uses bright artificial white or colored light. Relevant studies have reported the efficacy of light therapy in the treatment of nonseasonal depression10,11 and bipolar depression.12 However, heterogeneity has been observed in these studies because of variables such as light color, light intensity, duration, and settings. Furthermore, few trials have had a randomized control design. Moreover, the results of trial studies investigating the use of light therapy on elderly adults have been inconclusive. Some studies have reported that light therapy is efficacious,13–15 whereas others have not reported significant differences between the case and control groups.16–18
Therefore, we performed a meta-analysis to evaluate the efficacy of light therapy in the treatment of geriatric depression.
Methods
Search strategy and inclusion criteria
Two independent authors (Shaw-Ji Chen and Chun-Hung Chang) conducted a systematic article search and used the PubMed database at the National Library of Medicine, Cochrane Collaboration’s Central Register of Controlled Clinical Trials, Cochrane Systematic Reviews, and the ClinicalTrials.gov website (https://ClinicalTrials.gov). Professor Hsin-Chi Tsai made the final inclusion decision of cases that were inconsistently selected. We used the keywords “(Phototherapy OR light therapy) AND (depress* OR mood) AND (old OR elders OR geriatric)” to search for all relevant articles on the PubMed and ClinicalTrials.gov websites until July 14, 2018.
Randomized controlled trials (RCTs) or comparative experimental trials were included. However, we excluded 1) case reports, 2) nonclinical trials, 3) studies not performed on human subjects, and 4) studies including patients with seasonal affective disorder. Additionally, trials that were not associated with the application of light therapy for the treatment of nonseasonal depression were excluded. We retrieved all studies comprising at least two treatment arms (ie, light therapy treatment and placebo or dim light treatment) that were written in English and contained the aforementioned keywords. The titles and abstracts of these articles were then screened by Chun-Hung Chang and Shaw-Ji Chen to determine their eligibility for inclusion in the meta-analysis. Agreement through consensus was performed in cases of disagreement regarding eligibility. In addition, we researched the reference articles listed in the review studies. Figure 1 depicts the screening and search protocols.
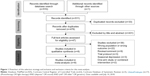  | Figure 1 Flowchart of the selection strategy and inclusion and exclusion criteria for this meta-analysis. |
Data extraction and quality assessment
The primary outcome of these studies was the severity of depression in elderly adults, as assessed by the Geriatric Depression Scale (GDS),19,20 or the Hamilton Depression (HAM-D) rating scale,21 or Beck’s Depression Inventory (BDI).22 We extracted as many clinical variables, including first author, year, sample size, number and type of treatment arms, participant characteristics, details of the light therapy treatment, and comparative arm regimens. Furthermore, we attempted to contact the authors to acquire the original data if they were not available in the articles. Because GDS scores were the most frequently used in the included studies, we used them first to assess the severity of depression in elderly patients; if GDS scores were not available, we used the HAM-D rating scale.
Two reviewers independently evaluated the methodological quality of the included trials using the Jadad scoring system and Newcastle–Ottawa Quality Assessment Scale for the RCTs and comparative experimental trials, respectively.23,24 The Jadad scale evaluates three items using a scale that ranges from 0 to 5 points. Specifically, the methodology of the RCTs was evaluated on the basis of three components: randomization (two points), blinding (two points), and an account of all patients (one point). Thus, the scores ranged from 0 to 5, with a higher score indicating higher methodological quality. By contrast, the comparative trials were evaluated on the basis of nine items across three categories: participant selection (four items), comparability (four items), and exposure (three items). The studies received a maximum of one point for each of the items in the selection and exposure domains, and a maximum of two points for those in the comparability domain. The corresponding author helped to resolve discrepancies between the scores assigned by the two reviewers.
Data synthesis and analysis
We used effect size (ES), which expresses changes in depression severity, in each selected meta-analysis to calculate the standardized mean difference on the basis of Hedges’ adjusted g; negative values indicated that the depression severity decreased after light therapy.25 In addition, we used a random-effects model to pool the individual ESs.26 Thereafter, we performed a meta-analysis using the Comprehensive Meta-Analysis software package (version 3; Biostat, Englewood, NJ, USA). Two-tailed P-values of <0.05 were considered statistically significant. Between-trial heterogeneity was determined using I2 tests, and values of >50% were considered to exhibit considerable heterogeneity. Additionally, a sensitivity analysis was performed to ensure that no single study over-influenced the analysis by excluding each individual study and reanalyzing the overall effect on the remaining studies. Finally, funnel plots and Egger’s test were used to examine potential publication bias. We followed the guidelines of PRISMA to report our findings.27
Results
Article search and characteristics of included patients
We retrieved 47 articles after the initial screening; 22 were excluded because they included the wrong population (not older patients with nonseasonal depression) or the wrong outcome (without depression measure).28–48 In addition, one article was excluded because it was only indexed in the Cochrane Central Register of Controlled Trials. We also excluded nine review articles,36,49–55 three trial protocols,13,56,57 and three studies of seasonal depression.58–60 We excluded two studies with one-arm or combined intervention61 (one article was only indexed in the Cochrane Central Register of Controlled Trials).
The final quantitative analysis included 395 participants from eight trials.13–18,62,63 We followed the PRISMA guidelines, and the search process is displayed in Figure 1. Table 1 presents a summary of the study characteristics. The average number of subjects was 49.38±28.61 (range: 10–89), and the average treatment duration of these trials was 18.25±13.57 days (range: 2–35 days). The average age of the participants was 71.63±5.63 years. Studies were conducted in North America (n=3), East Asia (n=2), and Europe (n=3).
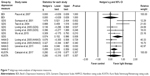
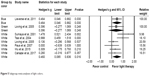
Meta-analyses of pre- and post-light therapy
The positive ES results indicated that the severity of depression significantly improved after light therapy. Specifically, the overall ES of light therapy vs comparative therapies to mitigate depression severity was 0.442 (95% CI: 0.174–0.709, P=0.001; Figure 2). Moreover, heterogeneity was observed within these studies (Q=12.899, df=7, I2=45.731%, P=0.075) and publication bias was detected using the Egger’s test (t=1.115, df=6, two-tailed P=0.307; Figure 3).
  | Figure 2 Meta-analysis of studies comparing depression severity before and after light therapy in elderly adults. |
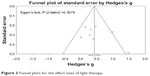  | Figure 3 Funnel plots for the effect sizes of light therapy. |
Meta-regression analyses of light therapy
We noted that female sex and mean age were positively correlated with the effects of light therapy (female sex, slope =0.2242, 95% CI: −2.0430 to 2.4915; mean age, slope =0.0380, 95% CI: −0.131 to 0.0892). However, these findings did not reach significance (P=0.8463 and 0.1450, respectively). Moreover, meta-regression revealed no significant association between the changes in depression severity after light therapy and intensity of light therapy in lux or in intervention duration in days (P=0.3095 and 0.9693, respectively; Figure 4).
  | Figure 4 Meta-regression of the effects of (A) female sex, (B) mean age, (C) treatment duration in days, and (D) light intensity in lux. |
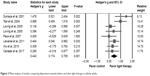
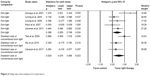
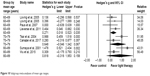
Subgroup analyses of different light colors
No conclusive evidence was presented in the reviewed studies to support the effects of different light colors on geriatric depression; therefore, we conducted a subgroup meta-analysis of the studies that used different light colors. We found that both bright-light therapy (N=273, ES: 0.460, 95% CI: 0.085–0.836, P=0.016) and pale blue light therapy (N=89, ES: 0.464, 95% CI: 0.046–0.882, P=0.030) resulted in significant reductions in the severity of geriatric depression, whereas green light’s effect was nonsignificant (N=33, ES: 0.396, 95% CI: −0.277 to 1.069, P=0.248; Figure 5).
  | Figure 5 Subgroup meta-analyses of light colors. |
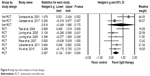
Subgroup analyses of comparators
Trials employing standard care or conventional room light as a comparator had higher ESs. Five trials13,15–17,63 used dim light as comparator and the ES was 0.388 (95% CI: 0.029–0.748, P=0.034). Three14,18,62 trials used standard care as comparator and the ES was 0.529 (95% CI: 0.074–0.984, P=0.023; Figure 6).
  | Figure 6 Subgroup meta-analyses of comparators. |
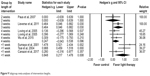
Subgroup analyses of depression measures
Four primary depression measures – GDS, HAM-D, BDI, and Kurz-Skala Stimmung/Aktivierung rating scale64 – were used in these trials. Two studies reported both GDS and HAM-D scores.16,17 Five14–18 of the eight trials used GDS as a primary measure and had significant ESs: 0.574 (95% CI: 0.152–0.996, P=0.008; Figure 7). Three studies reported changes in HAM-D scores and the combined ES was 0.285 (95% CI: 0.01–0.0559, P=0.042).13,16,17
Subgroup analyses of study designs
Six13,14,16–18,63 of the eight trials employed an RCT design and had significant ESs: 0.387 (95% CI: 0.124–0.651, P=0.004), whereas two trials15,18 did not use an RCT design and showed nonsignificant ESs: 0.818 (95% CI: −0.349 to 1.985, P=0.170; Figure 8).
  | Figure 8 Subgroup meta-analyses of study designs. |
Subgroup analyses of intervention lengths
In these eight trials, the length of the intervention was from <1 to 4 weeks. Three studies14,15,62 adopted <1 week intervention and showed significant ESs: 0.848 (95% CI: 0.217–1.478, P=0.008), whereas trials with longer interventions did not show significant ESs (Figure 9).
  | Figure 9 Subgroup meta-analyses of intervention lengths. |
Subgroup analyses of mean age ranges
In these eight trials, the mean age range was from 60 to 80 years. Four studies13,16,17,63 with a mean age range of 60–69 years showed significant ESs: 0.271 (95% CI: 0.018–0.523, P=0.035), whereas other studies with higher mean ages did not show significant ESs (Figure 10).
  | Figure 10 Subgroup meta-analyses of mean age ranges. |
Adverse effects
No significant adverse reactions were observed in either the intervention group or control group. Moreover, no incidents of mania or hypomania during the light treatment or follow-up were reported in the eight trials.
Sensitivity analysis
In the meta-analysis of light therapy’s overall effects on geriatric depression, the conclusion remained significant when any single study was removed.
Discussion
This meta-analysis investigated the efficacy of light therapy for the treatment of nonseasonal depression in elderly adults. The main results were that 1) depression severity significantly decreased after light therapy (ES: 0.442, 95% CI: 0.174–0.709, P=0.001), 2) the treatment effects of white and pale blue light were significant, and 3) no manic shifting occurred in elderly adults who received light therapy in the eight trials.
Our study had several merits compared with a previous meta-analytic study.49 In our study, we enrolled more trials and patients compared with the previous meta-analytic article. We included eight trials and 395 participants, whereas these numbers in the earlier study49 were 6 and 359, respectively. Moreover, we used meta-regression first to evaluate the effect on geriatric depression between light therapy and clinical variables. In addition, we first reported the potential factors including age groups and long-term effects.
Our findings were in agreement with relevant reviews regarding the efficacy of light therapy in the treatment of nonseasonal depression in adults10,11 and bipolar depression.12 However, these reviews did not address the general elderly population with depression. Three trials indicated that depression scores differed significantly between experimental and control groups,13–15 whereas two trials did not.16,18 Both Loving et al and Wu et al reported an improvement in their participants’ depression after light therapy, although the differences between the experimental and control groups were not significant. In the present meta-analysis, we found that the severity of depression among elderly adults significantly decreased after light therapy; however, two of the examined trials did not indicate a significant difference between their experimental and control groups. One possible cause for this inconsistency is the time of treatment, because as studies have suggested, phototherapy in the morning can result in a higher treatment response through circadian resynchronization.10,11,65 In the study by Loving et al, only 13 of 41 patients received light therapy in the morning.
Different light colors may have different effects on geriatric depression. Five trials used bright (white) light,14–16,18,62 one trial used bright (pale blue) light,13 and one used green light.17 Both white light and blue colors exhibited efficacy for the treatment of depression. Furthermore, studies have indicated that blue light affects mood and cognitive function more than other colors because it is mediated through melanopsin.65,66 We suggest that further well-designed studies using blue light and a large sample size should be conducted to test the efficacy of blue light therapy in the treatment of geriatric depression.
In the subgroup analyses of depression measures, five trials14–18 used GDS as a primary measure and had larger effects than those13,16,17 that used HAM-D (ES: 0.515 vs 0.285). However, heterogeneity was observed within the studies that adopted GDS (Q=10.685, df=4, I2=62.566, P=0.030), whereas no significant heterogeneity was observed within the studies reporting HAM-D (Q=1.616, df=2, I2=0.000, P=0.446). Our findings showed that studies with GDS had larger z-scores than those with HAM-D (2.667 vs 2.035) and suggest that the depression measures were a potential factor in influencing treatment effects. GDS is a self-rated measure, whereas HAM-D is clinician rated. Different rating methods may result in different evaluations of depression severity. The HAM-D rating scale and clinician-rated Montgomery–Åsberg Rating Scale67 are primary outcome measures for clinical trials of psychopharmacological treatment of depression.68,69
In the subgroup analysis of intervention length, we found that the effect of light therapy compared with control treatment reached statistical significance at <1 week (ES: 0.848, 95% CI: 0.217–1.478, P=0.008). A relevant meta-analysis found that 2-week intervention periods were effective for improving depression.49 The treatment effect did not increase with the intervention length. Moreover, among these eight trials, Canazei et al62 were the first to report immediate psychophysiological effects of single, short-room light exposure in mildly depressed geriatric inpatients during a short cognitive stimulation session and when resting. Virk et al70 used a single, short, bright-light exposure of 10,000 lux in the morning in untreated patients with seasonal affective disorder and found that briefly administering light was clinically effective within 20 minutes and that improvements of mood even occurred after the first bright-light exposure. Recent studies have shown that acute light can directly affect mood and learning without producing major disruptions in circadian rhythms and sleep.65 A functional imaging study of 17 healthy volunteers reported that 40-second periods of blue or green ambient light increased responses to emotional stimuli in the voice area of the temporal cortex and in the hippocampus.66 When we conducted a sensitivity test to exclude Canazei’s study, the ES remained statically significant (ES: 0.464, 95% CI: 0.164–0.772, P=0.003). Therefore, the study conducted by Canazei et al did not affect the overall treatment ES. Further studies with short-term interventions will facilitate understanding of the underlying immediate effects.
Furthermore, we investigated potential factors such as mean age and long-term effects after stopping phototherapy. We found that light therapy on patients with a mean age of 60–69 years reached statistical significance (ES: 0.271, 95% CI: 0.018–0.523, P=0.035), whereas patients of older age groups did not (Figure 11). Lam reported that younger age is a predictor of response to light therapy for winter depression.71 In addition, we observed that two of the eight trials reported 3-month follow-ups after stopping light therapy.16,17 The ES was 0.449 (95% CI: 0.081–0.816, P=0.017). No significant heterogeneity was observed within these studies (Q=0.729, df=1, I2=0.000, P=0.393; Figure 12); however, this was because only two studies were analyzed for long-term effect. Thus, further trials with long-term evaluation at ≥6 months are required.
  | Figure 11 Subgroup meta-analyses of effects at 3-month follow-up after stopping light therapy. |
  | Figure 12 Funnel plots for effect size of subgroup meta-analysis on (A) white light, (B) standard care, (C) GDS, (D) <1 week. |
Heterogeneity and publication bias
Because significant heterogeneity (>50%) of the included studies in the subgroup analysis (at least three trials) was found for white color (I2=61.063%), standard care (I2=54.020%), GDS (I2=62.566%), and intervention length of <1 week (I2=62.486%), sensitivity analyses were performed. For white color, the effect remained significantly positive; only when the study of Tsai et al14 was removed did the effect become nonsignificant (ES: 0.322, 95% CI: −0.028 to 0.671, P=0.072). For standard care, when any one of the three studies14,18,62 was removed, the effect became nonsignificant (P=0.059, 0.120, and 0.067). In the subgroup meta-analysis of GDS, the conclusion remained significant when removing any single study. For an intervention length of <1 week, when the studies by Sumaya et al15 and Tsai et al14 were removed, the effect changed to nonsignificant (P=0.067 and 0.170, respectively). Results of the Egger’s test suggested no significant publication biases in the subgroup meta-analysis on white color, standard care, GDS, intervention length of <1 week (white light: P=0.28125; standard care: P=0.98627; GDS: P=0.17994; intervention length of <1 week: P=0.67980). Figure 12 displays the funnel plots.
No incidents of mania, hypomania, or severe adverse effects during light treatment were reported in these eight trials. In the study by Loving et al, one participant (receiving bright-light treatment) who dropped out died in the hospital because of late-stage emphysema 3 months after leaving the study.16 In the study by Lieverse et al, adverse effect profiles did not differ between two groups, and the most common adverse effect was headache.13 The absence of side effects in this study could be a result of the short duration and limited exposure to light therapy. Further studies should include extended treatment trials to assess side effects associated with the prolonged use of light therapy.
Limitations
Our study had some limitations. First, most of the studies included in the meta-analysis lacked a well-designed control group, and possible bias may have resulted from the placebo effect. In our study, six trials used an RCT design and meta-analyses showed significant ESs, whereas the other two non-RCTs did not. Second, because details were lacking regarding combined treatments, including antidepressants or psychotherapy, we could not exclude the possibility of biased outcomes. Third, in the subgroup meta-analysis of different colors of light therapy, the number of studies included in each subgroup was small. However, light therapy is a noninvasive and safe non-pharmacological treatment for geriatric populations. Additional well-designed trials should be conducted to determine the standard settings for improving the response of elderly adults with depression to light therapy.
Conclusion
Our results indicated that light therapy is effective for treating geriatric depression and that white and blue light are both effective. Further well-designed controlled trials are necessary to determine standard parameters, adequate group sizes, and randomized assignment to evaluate the effectiveness of phototherapy for treating depression in elderly adults.
Acknowledgment
This work was supported by grants from China Medical University Hospital (DMR-107-201) and the Ministry of Health and Welfare, Taiwan (MOHW107-TDU-B-212-123004).
Author contributions
Chun-Hung Chang proposed the research ideas, performed the statistical analysis, processed the database, and drafted the initial manuscript. Shaw-Ji Chen and Chieh-Yu Liu searched the database, provided expert opinions, and reviewed the final submitted manuscript. Hsin-Chi Tsai was in charge of this study, critically reviewed the draft of the manuscript, and approved the final submitted version of the manuscript. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Belmaker RH, Agam G. Major depressive disorder. N Engl J Med. 2008;358(1):55–68. | ||
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. | ||
McCall WV. Late life depression. Psychiatr Clin North Am. 2013;36(4):xi. | ||
Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64(12):1465–1475. | ||
Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–1970. | ||
Lackamp J, Schlachet R, Sajatovic M. Assessment and management of major depressive disorder in older adults. Psychiatr Danub. 2016;28(Suppl 1):95–98. | ||
Frederick JT, Steinman LE, Prohaska T, et al. Community-based treatment of late life depression an expert panel-informed literature review. Am J Prev Med. 2007;33(3):222–249. | ||
Frank C. Pharmacologic treatment of depression in the elderly. Can Fam Physician. 2014;60(2):121–126. | ||
Pitychoutis PM, Kokras N, Sanoudou D, Dalla C, Papadopoulou-Daifoti Z. Pharmacogenetic considerations for late life depression therapy. Expert Opin Drug Metab Toxicol. 2013;9(8):989–999. | ||
Penders TM, Stanciu CN, Schoemann AM, Ninan PT, Bloch R, Saeed SA. Bright Light Therapy as Augmentation of Pharmacotherapy for Treatment of Depression: A Systematic Review and Meta-Analysis. Prim Care Companion CNS Disord. 2016;18(5):1–8. | ||
Perera S, Eisen R, Bhatt M, et al. Light therapy for non-seasonal depression: systematic review and meta-analysis. BJPsych Open. 2016;2(2):116–126. | ||
Tseng PT, Chen YW, Tu KY, et al. Light therapy in the treatment of patients with bipolar depression: A meta-analytic study. Eur Neuropsychopharmacol. 2016;26(6):1037–1047. | ||
Lieverse R, Nielen MM, Veltman DJ, et al. Bright light in elderly subjects with nonseasonal major depressive disorder: a double blind randomised clinical trial using early morning bright blue light comparing dim red light treatment. Trials. 2008;9:48. | ||
Tsai YF, Wong TK, Juang YY, Tsai HH. The effects of light therapy on depressed elders. Int J Geriatr Psychiatry. 2004;19(6):545–548. | ||
Sumaya IC, Rienzi BM, Deegan JF, Moss DE. Bright light treatment decreases depression in institutionalized older adults: a placebo-controlled crossover study. J Gerontol A Biol Sci Med Sci. 2001;56(6):M356–M360. | ||
Loving RT, Kripke DF, Elliott JA, Knickerbocker NC, Grandner MA. Bright light treatment of depression for older adults [ISRCTN55452501]. BMC Psychiatry. 2005;5:41. | ||
Loving RT, Kripke DF, Knickerbocker NC, Grandner MA. Bright green light treatment of depression for older adults [ISRCTN69400161]. BMC Psychiatry. 2005;5:42. | ||
Wu MC, Sung HC, Lee WL, Smith GD. The effects of light therapy on depression and sleep disruption in older adults in a long-term care facility. Int J Nurs Pract. 2015;21(5):653–659. | ||
Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. | ||
Lu CH, Liu CY, Yu S. Depressive disorders among the Chinese elderly in a suburban community. Public Health Nurs. 1998;15(3):196–200. | ||
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–296. | ||
Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. | ||
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Hedges LV, Olkin I. Statistical Methods for Meta-analysis. San Diego, CA: Academic Press; 1985. | ||
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. | ||
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. | ||
van Marum RJ. [Symptomatic treatment in patients with dementia: light, but not melatonin, is probably worthwhile]. Ned Tijdschr Geneeskd. 2008;152(43):2322–2324. Dutch. | ||
Onega LL, Pierce TW, Epperly L. Bright Light Therapy to Treat Depression in Individuals with Mild/Moderate or Severe Dementia. Issues Ment Health Nurs. 2018;39(5):370–373. | ||
Barry HC. Light Therapy Improves Behavioral Disturbances, Sleep, Depression in Older Patients with Cognitive Impairment. Am Fam Physician. 2018;97(4):Online. | ||
Düzgün G, Durmaz Akyol A. Effect of Natural Sunlight on Sleep Problems and Sleep Quality of the Elderly Staying in the Nursing Home. Holist Nurs Pract. 2017;31(5):295–302. | ||
Hopkins S, Morgan PL, Schlangen LJM, Williams P, Skene DJ, Middleton B. Blue-Enriched Lighting for Older People Living in Care Homes: Effect on Activity, Actigraphic Sleep, Mood and Alertness. Curr Alzheimer Res. 2017;14(10):1053–1062. | ||
Figueiro MG, Hunter CM, Higgins P, et al. Tailored Lighting Intervention for Persons with Dementia and Caregivers Living at Home. Sleep Health. 2015;1(4):322–330. | ||
Figueiro MG, Plitnick BA, Lok A, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527–1537. | ||
Loprinzi PD. Objectively measured light and moderate-to-vigorous physical activity is associated with lower depression levels among older US adults. Aging Ment Health. 2013;17(7):801–805. | ||
Hanford N, Figueiro M. Light therapy and Alzheimer’s disease and related dementia: past, present, and future. J Alzheimers Dis. 2013;33(4):913–922. | ||
Friedman L, Spira AP, Hernandez B, et al. Brief morning light treatment for sleep/wake disturbances in older memory-impaired individuals and their caregivers. Sleep Med. 2012;13(5):546–549. | ||
Royer M, Ballentine NH, Eslinger PJ, et al. Light therapy for seniors in long term care. J Am Med Dir Assoc. 2012;13(2):100–102. | ||
Roecklein KA, Schumacher JA, Miller MA, Ernecoff NC. Cognitive and behavioral predictors of light therapy use. PLoS One. 2012;7(6):e39275. | ||
Vandewalle G, Hébert M, Beaulieu C, et al. Abnormal hypothalamic response to light in seasonal affective disorder. Biol Psychiatry. 2011;70(10):954–961. | ||
Burns A, Allen H, Tomenson B, Duignan D, Byrne J. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr. 2009;21(4):711–721. | ||
Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA. 2008;299(22):2642–2655. | ||
Dowling GA, Graf CL, Hubbard EM, Luxenberg JS. Light treatment for neuropsychiatric behaviors in Alzheimer’s disease. West J Nurs Res. 2007;29(8):961–975. | ||
Hickman SE, Barrick AL, Williams CS, et al. The effect of ambient bright light therapy on depressive symptoms in persons with dementia. J Am Geriatr Soc. 2007;55(11):1817–1824. | ||
Kaida K, Takahashi M, Otsuka Y. A short nap and natural bright light exposure improve positive mood status. Ind Health. 2007;45(2):301–308. | ||
Grandner MA, Kripke DF, Langer RD. Light exposure is related to social and emotional functioning and to quality of life in older women. Psychiatry Res. 2006;143(1):35–42. | ||
Schindler SD, Graf A, Fischer P, Tölk A, Kasper S. Paranoid delusions and hallucinations and bright light therapy in Alzheimer’s disease. Int J Geriatr Psychiatry. 2002;17(11):1071–1072. | ||
Ash JB, Piazza E, Anderson JL. Light therapy in the clinical management of an eating-disordered adolescent with winter exacerbation. Int J Eat Disord. 1998;23(1):93–97. | ||
Zhao X, Ma J, Wu S, Chi I, Bai Z. Light therapy for older patients with non-seasonal depression: A systematic review and meta-analysis. J Affect Disord. 2018;232:291–299. | ||
Holvast F, Massoudi B, Oude Voshaar RC, Verhaak PFM. Non-pharmacological treatment for depressed older patients in primary care: A systematic review and meta-analysis. PLoS One. 2017;12(9):e0184666. | ||
Stephenson KM, Schroder CM, Bertschy G, Bourgin P. Complex interaction of circadian and non-circadian effects of light on mood: shedding new light on an old story. Sleep Med Rev. 2012;16(5):445–454. | ||
Sloane PD, Figueiro M, Cohen L. Light as Therapy for Sleep Disorders and Depression in Older Adults. Clin Geriatr. 2008;16(3):25–31. | ||
Terman M. Evolving applications of light therapy. Sleep Med Rev. 2007;11(6):497–507. | ||
Montgomery P, Dennis J. Bright light therapy for sleep problems in adults aged 60+. Cochrane Database Syst Rev. 2002;(2):CD003403. | ||
Dijk DJ, Boulos Z, Eastman CI, Lewy AJ, Campbell SS, Terman M. Light treatment for sleep disorders: consensus report. II. Basic properties of circadian physiology and sleep regulation. J Biol Rhythms. 1995;10(2):113–125. | ||
Most EI, Scheltens P, van Someren EJ. Prevention of depression and sleep disturbances in elderly with memory-problems by activation of the biological clock with light – a randomized clinical trial. Trials. 2010;11:19. | ||
Huang SY, Sung HC, Su HF. Effectiveness of bright light therapy on depressive symptoms in older adults with non-seasonal depression: a systematic review protocol. JBI Database System Rev Implement Rep. 2016;14(7):37–44. | ||
Moscovici L. Bright light therapy for seasonal affective disorder in Israel (latitude 32.6 degrees N): a single case placebo-controlled study. Acta Psychiatr Scand. 2006;114(3):216–218. | ||
Magnusson A. Light therapy to treat winter depression in adolescents in Iceland. J Psychiatry Neurosci. 1998;23(2):118–122. | ||
Webb M, Jarrett D. Response to phototherapy of an elderly patient with seasonal affective disorder. Am J Psychiatry. 1988;145(12):1607–1608. | ||
Leggett AN, Conroy DA, Blow FC, Kales HC. Bright Light as a Preventive Intervention for Depression in Late-Life: A Pilot Study on Feasibility, Acceptability, and Symptom Improvement. Am J Geriatr Psychiatry. 2018;26(5):598–602. | ||
Canazei M, Pohl W, Bauernhofer K, et al. Psychophysiological Effects of a Single, Short, and Moderately Bright Room Light Exposure on Mildly Depressed Geriatric Inpatients: A Pilot Study. Gerontology. 2017;63(4):308–317. | ||
Paus S, Schmitz-Hübsch T, Wüllner U, Vogel A, Klockgether T, Abele M. Bright light therapy in Parkinson’s disease: a pilot study. Mov Disord. 2007;22(10):1495–1498. | ||
Wendt G, Binz U, Müller AA. KUSTA (Kurz-Skala Stimmung/Aktivierung): a daily self-rating scale for depressive patients. Pharmacopsychiatry. 1985;18(1):118–122. | ||
Legates TA, Fernandez DC, Hattar S. Light as a central modulator of circadian rhythms, sleep and affect. Nat Rev Neurosci. 2014;15(7):443–454. | ||
Vandewalle G, Schwartz S, Grandjean D, et al. Spectral quality of light modulates emotional brain responses in humans. Proc Natl Acad Sci U S A. 2010;107(45):19549–19554. | ||
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. | ||
Khan A, Khan SR, Shankles EB, Polissar NL. Relative sensitivity of the Montgomery-Asberg Depression Rating Scale, the Hamilton Depression rating scale and the Clinical Global Impressions rating scale in antidepressant clinical trials. Int Clin Psychopharmacol. 2002;17(6):281–285. | ||
Carmody TJ, Rush AJ, Bernstein I, et al. The Montgomery Asberg and the Hamilton ratings of depression: a comparison of measures. Eur Neuropsychopharmacol. 2006;16(8):601–611. | ||
Virk G, Reeves G, Rosenthal NE, Sher L, Postolache TT. Short exposure to light treatment improves depression scores in patients with seasonal affective disorder: A brief report. Int J Disabil Hum Dev. 2009;8(3):283–286. | ||
Lam RW. Morning light therapy for winter depression: predictors of response. Acta Psychiatr Scand. 1994;89(2):97–101. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.