Back to Journals » Drug Design, Development and Therapy » Volume 18
Efficacy of Intravenous Administration of Esketamine in Preventing and Treating Rebound Pain After Thoracic Paravertebral Nerve Block: A Prospective Randomized, Double-Blind, Placebo-Controlled Trial
Authors Zeng X , Zhang X, Jiang W, Zhou X
Received 18 November 2023
Accepted for publication 3 February 2024
Published 17 February 2024 Volume 2024:18 Pages 463—473
DOI https://doi.org/10.2147/DDDT.S448336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Xu Zeng,1,2 Xianjie Zhang,2 Wencai Jiang,2,* Xinyu Zhou1,*
1Department of Anaesthesiology, Chengdu Medical College, Chengdu, People’s Republic of China; 2Department of Anesthesiology, People’s Hospital of Deyang City, Deyang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xianjie Zhang, Department of Anesthesiology, People’s Hospital of Deyang City, Deyang, People’s Republic of China, Email [email protected]
Purpose: Investigating the efficacy of intraoperative fractionated intravenous esketamine in the prevention of rebound pain after cessation of thoracic paravertebral nerve blockade.
Methods: One hundred and twenty patients who underwent elective thoracoscopic lobectomy were selected for the study and were randomly divided into two groups, the esketamine group was given 0.5 mg/kg and 0.3 mg/kg of esketamine at the induction of anaesthesia and 30 minutes before the end of the operation, respectively, and the control group was given an equal amount of saline. The incidence of rebound pain (RP) 7 days after surgery and postoperative recovery were compared between the two groups.
Results: The NRS pain scores at 24 and 48 hours postoperatively in the esketamine group were significantly lower than those in the control group (P < 0.05). The incidence of postoperative rebound pain was significantly lower in the esketamine group than in the control group (P < 0.05). The consumption of sufentanil was less in the esketamine group in the postoperative 48 hours (P < 0.05). Postoperative recovery was compared between the two groups and the difference was not statistically significant.
Conclusion: Intravenous esketamine reduces postoperative pain scores, decreases the incidence of rebound pain after cessation of thoracic paravertebral block, and reduces opioid consumption.
Keywords: esketamine, rebound pain, paravertebral nerve block, postoperative pain
Introduction
Video-assisted thoracic surgery (VATS) is less invasive than open thoracotomy, and patients recover faster and with less pain postoperatively, but some studies have reported moderate to severe postoperative pain in nearly 40% of patients, even with VATS.1 TPVB is one of the recommended methods for postoperative pain management in thoracic surgery guidelines. It can provide effective analgesia in the short term after surgery, but there may be an exacerbation of pain known as RP when the block effect wears off.2 Existing studies indicate that the incidence of rebound pain after the regression of peripheral nerve block is approximately 30%-45%.2 Rebound pain is considered an important health problem as it inhibits the activity of several systems such as respiratory, digestive and urinary, interferes with the patient’s postoperative recovery, prolongs hospital stay, further leads to wastage of healthcare resources and reduces the overall effectiveness of regional anaesthesia.3
The presence of exacerbated endogenous excitatory processes, such as enhanced N-methyl-D-aspartate (NMDA) receptor activation, contributes to postoperative hyperalgesia caused by local tissue injury. Ketamine is a non-selective inhibitor of NMDA receptors, exhibiting analgesic, anti-hyperalgesic, and anti-inflammatory properties. As the R-enantiomer of ketamine, esketamine has twice the affinity for both opioid receptors and NMDA receptors compared to ketamine. It possesses stronger analgesic and sedative effects and can reduce acute opioid tolerance, as well as exert a certain inhibitory effect on hyperalgesia and central sensitization.4 A number of studies have used esketamine for postoperative analgesia and have shown that esketamine achieves the desired analgesic effect: in a randomised, double-blind, controlled study of 68 patients undergoing bariatric surgery and receiving either intravenous esketamine or placebo, intraoperative use of low-dose esketamine significantly reduced the patients’ acute postoperative pain.5 In a study of the efficacy of low-dose esketamine in combination with sufentanil for postoperative analgesia after caesarean section in women with gestational diabetes mellitus, the addition of low-dose esketamine significantly reduced postoperative sufentanil dosage and was effective in lowering postoperative pain scores in women with gestational diabetes mellitus, as compared with the control group.6 However, in a prospective randomised controlled study by Touil et al on intraoperative ketamine for the prevention of severe rebound pain after cessation of peripheral nerve block, ketamine did not reduce the incidence or intensity of rebound pain after peripheral nerve block.7 There are fewer studies on ketamine or esketamine for the treatment of rebound pain, and some of the ideas in the existing studies are contradictory or poorly elucidated; therefore, more prospective studies are needed to explore whether esketamine can reduce the incidence of rebound pain after regional blockade in order to provide new evidence to support individualised pain management.The aim of this study is to investigate the efficacy of incremental intravenous administration of low-dose esketamine during surgery in preventing and treating rebound pain after the cessation of paravertebral nerve block. Additionally, this study aims to evaluate the impact of esketamine on short-term recovery quality in patients, which can contribute as a reference for developing perioperative analgesic strategies that promote patient rehabilitation.
Materials and Methods
Study Design and Patient Enrollment
The research was approved by the Ethics Committee of Deyang People’s Hospital (2023–04-012-H01) and registered with the Chinese Clinical Trial Registry (ChiCTR2300069099). The clinical trial followed the Declaration of Helsinki, the Good Clinical Practice (GCP) for Drug Clinical Trials issued by the State Drug Administration (SDA) and other relevant regulations. Written informed consent was obtained from all participants. We recruited patients scheduled to undergo thoracoscopic lobectomy between March 2023 and July 2023.The inclusion criteria were as follows: both genders, aged 18 to 65 years, BMI 18.5 to 28 kg/m2, ASA classification I to III. Exclusion criteria included: (1) patients with known allergies to the active ingredients of the drug being studied; (2) Patients at serious risk of increased intracranial pressure; (3) uncontrolled or untreated hypertension (resting systolic/diastolic blood pressure exceeding 180/100mmHg); (4) untreated or insufficiently treated hyperthyroidism; (5) patients requiring other surgeries during the study period or experiencing complications that would affect the study evaluation during or after surgery; (6) patients unwilling to participate after being informed about the study; (7) Post-operative planned admission to intensive care unit (ICU) for further treatment of patients; (8) patients with a history of severe psychiatric disorders or currently experiencing severe psychiatric disorders; (9) patients with congestive heart failure, a history of severe angina, or unstable angina or myocardial infarction within the past six months; (10) Prior to inclusion in the study, each patient will be tested on their ability to perform the Numeric Pain Scale Assessment (NRS), Patient Controlled Analgesia (PCA) pump operation, answer the telephone, and comprehend the Neuropathic Pain Syndrome Inventory (NPSI), and those who are unable to comprehend the relevant operations will be excluded from the study; (11) pregnant or lactating women; (12) individuals who had participated in other clinical trials within the past three months; (13) patients with positive preoperative Central Sensitization Inventory (CSI), Pain Catastrophizing Scale (PCS), and Douleur Neuropathique 4 (DN4) neuropathic pain scale assessments. Drop-out criteria included conversion to open thoracotomy during surgery, postoperative ICU admission for further treatment, occurrence of severe adverse reactions during or after surgery, and patient or family withdrawal from the study.
Randomization and Blinding
Before the study, a research assistant who was not involved in the study used a computer-generated random number table to randomly allocate participants into two groups in a 1:1 ratio. The group assignments were concealed using sequentially labeled, opaque sealed envelopes. Prior to anesthesia, an envelope was opened by another research assistant who was not involved in the experiment. The intervention drug, either esketamine or an equal volume of normal saline, was prepared according to the group assignment and delivered to the attending anesthesiologist. Throughout the data collection process, all patients, nurses, surgeons, and researchers responsible for data collection, follow-up, and statistical analysis were unaware of group assignments.
Interventions
The patients were randomly divided into two groups: the esketamine group and the control group. In the esketamine group, a bolus of esketamine 0.5mg/kg was administered intravenously during anesthesia induction, followed by another bolus of esketamine 0.3mg/kg half an hour before the end of the surgery. In the control group, an equal volume of normal saline was administered during anesthesia induction and half an hour before the end of the surgery, matching the dosage of the esketamine group.
Anesthesia Management
The patients underwent a standard fasting period of 8 hours for food and 2 hours for fluids before the surgery. Thirty minutes prior to surgery, a peripheral intravenous line was established in the upper limb in the anesthesia preparation room, and standard monitoring (non-invasive blood pressure, electrocardiogram, and pulse oximetry) was applied. TPVB was performed in the lateral decubitus position, targeting the space 2cm near the lower border of the fourth thoracic vertebra. The area was sterilized with iodine and under ultrasound guidance, a needle was inserted in a plane-oblique approach to the paravertebral space. After confirming the needle tip position and observing bloodless aspiration, 15mL of 0.25% ropivacaine was slowly injected, resulting in a visualized pleural displacement. Skin temperature was measured every 5 minutes for 30 minutes after the injection of the local anesthetic. Needle puncture and cold sensation were assessed in each nerve distribution area. If an increase in skin temperature and reduced sensation were observed within the 30-minute timeframe, the block was considered successful. After a 30-minute observation period without adverse reactions, the patient was transferred to the operating room where routine monitoring such as non-invasive blood pressure, electrocardiogram, and pulse oximetry were applied. Under local anesthesia, radial artery cannulation was performed under ultrasound guidance for continuous blood pressure monitoring. Anesthetic induction included the administration of midazolam 0.05mg/kg, etomidate 0.3mg/kg, sufentanil 0.5μg/kg, and rocuronium bromide 0.6mg/kg. Tracheal intubation was performed 3 minutes later, followed by fiberoptic bronchoscopy to confirm the appropriate positioning of the tube. Mechanical ventilation parameters were set as follows: respiratory rate (RR) of 12–20 breaths per minute, tidal volume (VT) of 4–6mL/kg, inspiratory-to-expiratory ratio (I:E) of 1:1.5, and FiO2 of 29%. Anesthetic maintenance included propofol infusion at 4–12 mg/(kg.h), remifentanil infusion at 0.1–0.3 μg/(kg.min), with additional rocuronium bromide and sufentanil administered as needed to maintain bispectral index (BIS) values between 40 and 60. Thirty minutes prior to the end of the surgery, 30mg of ketorolac was administered intravenously. After surgery, patient-controlled intravenous analgesia with sufentanil (1μg /mL) was initiated, with a background infusion rate of 2mL/h and a single-demand dose of 2mL, with a lockout time of 15 minutes. If the patients in the PACU reported a NRS score equal to or greater than 4, the PCIA pump was pressed by the anesthesia nurse. If the NRS score remained equal to or greater than 4 for three consecutive PCIA demands, rescue analgesia was administered, either with a 5mg intravenous dose of dexmedetomidine or a 100mg intravenous drip of tramadol. In case of moderate to severe nausea and vomiting after surgery, a 4mg intravenous dose of ondansetron was administered for rescue. If relief was not achieved, a repeat dose of 4mg ondansetron could be given, with a maximum total dose of 8mg. The Pain Manager System (version V1.2.0.2.1.0) was utilized to collect data regarding PCIA device usage.
Data Collection and Result Evaluation
In this study, the baseline data of patients were recorded, including age, gender, height, weight, BMI, ASA classification, and surgical site. The NRS was used to assess the preoperative pain intensity of patients. The CSI was used to evaluate the primary physical and somatic symptoms associated with central sensitization. The PCS was used to assess negative emotions related to pain, such as rumination, magnification, and helplessness. The DN4 neuropathic pain questionnaire was used to evaluate the presence of neuropathic lesions at the surgical site. Patients were assessed for quality of short-term postoperative recovery using the BPI.
The primary outcome indicator was average NRS) pain scores at 6 hours, 12 hours, 24 hours, 48 hours, 72 hours, 4 days, and 7 days after surgery. The NRS pain scores ranged from 0 to 10, with 0 indicating no pain, 1–3 indicating mild pain, 4–6 indicating moderate pain, and 7–10 indicating severe pain. The secondary outcome measures included the incidence of rebound pain within 7 days after surgery, the consumption of sufentanil via patient-controlled analgesia pump in the first 48 hours after surgery, extubation time (time from the end of surgery to removal of the endotracheal tube), duration of stay in the post-anesthesia care unit, incidence of adverse events within 48 hours after surgery, length of hospital stay, and 7-day postoperative BPI score. Rebound pain was defined as severe pain at the surgical site occurring after the transversus abdominis plane block had worn off, with an NRS score ≥7. Adverse events within 48 hours after surgery mainly included nausea, vomiting, hallucination, delirium, and nightmares. The BPI assessment was conducted through telephone follow-up on the 7th day after surgery to evaluate the patients’ short-term recovery quality. Adverse events were closely monitored throughout the study, and appropriate actions were taken when necessary.
Statistical Analysis
Using the PASS 15.0 software, sample size calculation was performed. According to the relevant literature8 and our preliminary experiment, we expected that the mean postoperative pain score in the control group would be 3.9±1.62 points, and the mean postoperative pain score in the esketamine group could be decreased by 0.9 points, set α=0.05, 1-β=0.8, and calculated the sample size of 52 cases in each group, and taking into account the loss of visit rate of about 10%, the final A minimum of 58 cases in each group was required, totalling a minimum of 116 study subjects included.
Data analysis was performed using SPSS 25.0 statistical software. The normality of the data was visually assessed using histograms and verified using the Shapiro–Wilk test. NRS scores at different postoperative time intervals were repeated measures and analysed using generalised estimating equations (GEE). A generalised estimating equation was constructed using group and different time as the main variables, age and gender as covariates, NRS scores as the dependent variable, and the autocorrelation AR (1) was chosen for the structure of the working correlation matrix. Normally distributed quantitative data were presented as mean ± standard deviation, and between-group comparisons were conducted using independent samples t-test. Non-normally distributed quantitative data were presented as median (M) and interquartile range (IQR), and between-group comparisons were performed using the Mann–Whitney U-test. Data from repeated measurements were analyzed using generalized estimating equation. Qualitative data were presented as percentages (%), and between-group comparisons were carried out using the chi-square test or Fisher’s exact test. All statistical tests were two-way, and a difference of P ≤ 0.05 was considered statistically significant.
Results
A total of 132 patients were recruited and evaluated for the study, of whom 12 were excluded (5 with poor preoperative blood pressure control, 4 who refused to participate, 1 who was scheduled to be transferred to the ICU for postoperative treatment, 1 who had a positive preoperative CSI, and 1 who had an allergy), resulting in a total of 120 subjects entered into the intentional analysis (Figure 1).
 |
Figure 1 Trial Diagram. |
The demographics of the patients are shown in Table 1. There were no statistically significant differences in the baseline data between the two groups, including patient age, sex ratio, BMI, ASA classification, surgical site, concurrent illnesses, CSI scores, DN4 scores, and PCS scores.
 |
Table 1 Demographic Characteristics of the Participants |
Pain Scores and Rebound Pain
Figure 2 shows the mean pain experienced by patients in both groups at different time points of the study. At baseline (preoperative) the mean NRS pain scores were similar in both groups (esketamine group versus control group: 1.1±0.5 versus 1.1±0.6, P value=0.867), and similarly at 6 hours, 12 hours, 72 hours, 4 days, and 7 days postoperatively the mean NRS pain scores were similar in both groups. However, there was a significant difference in the mean pain scores between the two groups at 24 hours (2.5±1.5 versus 3.3±1.8, P value=0.009) postoperatively and 48 hour (2.5±1.0 versus 3.4±2.1, P value=0.003) postoperatively. Figure 2 shows an upward trend in mean pain scores for each group at 48 hours postoperatively compared with baseline, and these changes were significant (P < 0.05) at 24–48 hours postoperatively. From day 3 onwards, the patients’ pain scores showed a downward trend, and by day 7, they had largely returned to preoperative pain levels. The incidence of rebound pain at 7 days postoperatively was significantly lower in the esketamine group compared with the control group (8.3% versus 33.3%, P=0.001).
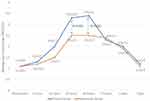 |
Figure 2 Average NRS pain scores. *Difference between average pain scores is significant. NRS=Numerical Rating Scale (0–10 points, 0=no pain and 10=worst pain). |
Opioid Consumption
Consumption of PCIA sufentanil was 50 (48–52) μg and 48 (48–50) μg (P=0.017) at 48 hours postoperatively in the esketamine and control groups, respectively, and the difference was statistically significant.
Adverse Events
Table 2 shows the incidence of adverse events in both groups, which were similar in both groups (esketamine group versus control group: 31.7% versus 30%). There were 19 cases in the esketamine group, including 9 cases of nausea and vomiting, 9 cases of delirium, and 1 case of nightmare. There were 18 cases in the control group, with 7 cases of nausea and vomiting, 9 cases of delirium, 1 case of nightmare and 1 case of hallucination. The severity of adverse events was low, ie, mild, in both groups. Serious adverse events occurred in both groups.
 |
Table 2 Comparison of Intraoperative and Postoperative Conditions |
Other Intraoperative Indicators
The differences in operation time, anaesthesia time, extubation time, PACU stay and postoperative hospital days between the two groups were not statistically significant.
BPI Scores
The BPI pain related parameters for 7 days postoperatively are shown in Table 3. The difference in the scores of the effect of pain on daily life, mood, ability to walk, daily routine, relationship with others, sleep, and interest in life of the patients in the two groups was not statistically significant.
 |
Table 3 BPI Assessment |
Generalised Estimating Equation Analysis
NRS pain scores at different time points are repeated measures information, now we choose to establish generalised estimating equations with group and time as the main variables, age and gender as covariates, and NRS pain scores as dependent variables. From the results of parameter estimation, the differences between different measurement time points, group and age were statistically significant, while the differences between different genders were not statistically significant, as shown in Table 4.
 |
Table 4 Results for Generalised Estimating Equations |
Discussion
The results of this single-centre randomised controlled clinical trial demonstrated that intraoperative fractionated low-dose intravenous esketamine reduced pain scores after cessation of thoracic paravertebral nerve block and significantly reduced the incidence of rebound pain (NRS ≥ 7) from 33.3% to 8.5%.The beneficial effects of intravenous esketamine on rebound pain are believed to contribute to decreased pain scores at 24–48 hours and reduced opioid consumption in the first 48 hours postoperatively. However, no benefit of esketamine on patient recovery was found at the one-week postoperative follow-up.
Postoperative acute pain after thoracic surgery can be extremely severe and may gradually progress into chronic pain. It has been reported that the incidence of chronic pain at 3 and 6 months after thoracic surgery is 57% and 47% respectively, which is the highest among all types of surgeries.9 Despite the introduction of video-assisted thoracic surgery, nearly 16% of patients still experience moderate to severe acute pain within 48 hours after surgery.10 The optimal postoperative pain management strategy for VATS surgery remains uncertain. In existing systematic reviews and guidelines for postoperative pain management in VATS, the use of regional analgesic techniques such as paravertebral nerve block, serratus anterior plane block, and erector spinae plane block is recommended.11,12 However, even after the analgesic effects of nerve blocks wear off, there is still a 30–45% chance of experiencing severe breakthrough pain.2,13,14 Esketamine, a newly marketed intravenous anesthetic in the country, possesses both anesthetic and analgesic effects and is widely used in anesthesia induction and maintenance as well as the management of acute and chronic pain. Previous studies have shown that low-dose intravenous esketamine can alleviate postoperative pain and reduce opioid consumption,15–17 which is consistent with our findings. In previous intraoperative analgesia predominantly based on opioid drugs, the incidence of postoperative complications such as nausea, vomiting, and respiratory depression was relatively high. It is worth noting that our results demonstrate that the combined use of esketamine during surgery significantly reduces the dosage of opioid analgesics while effectively improving postoperative pain relief. We applied the multimodal analgesic concept of Enhanced Recovery After Surgery (ERAS) to postoperative pain management in thoracoscopic surgery, using a combination of low-dose μ-opioid receptor agonists, NMDA receptor antagonists, and NSAIDs. By blocking pain stimuli transmission at different targets in the pain pathway, this approach reduces the dosage-related side effects of opioid drugs while ensuring good analgesic efficacy and promoting patient recovery after surgery. This can provide a reference for the development of more beneficial perioperative analgesic protocols in clinical practice.
This study used esketamine for postoperative analgesia in patients undergoing thoracoscopic lobectomy. Compared to the control group, the incidence of postoperative rebound pain was significantly reduced in the esketamine group. This may be attributed to the non-competitive binding of esketamine to NMDA receptors, inhibiting the activation of glutamate on these receptors, blocking NMDA signal pathway transmission, reducing neuronal excitability, and inhibiting pain hypersensitivity.18 Compared to the control group, the consumption of sufentanil in the esketamine group was significantly reduced at 48 hours postoperatively. Previous studies have shown consistent results that different doses of esketamine, either through single intravenous injection16 or through continuous infusion via analgesic pump during or after surgery,19 can reduce the consumption of opioid analgesics in the first 48 hours postoperatively. This may be due to esketamine’s activation of μ, δ, and k opioid receptors, strengthening the activity of the endogenous antinociceptive system, and reducing opioid tolerance.20 Zhou et al demonstrated that perioperative administration of a single dose of esketamine did not reduce postoperative pain scores after thoracoscopic lung resection.21 However, the results of this study showed that the NRS scores at 24 and 48 hours postoperatively were significantly lower in the esketamine group. The reduction in postoperative pain scores in this study may be attributed to multiple intravenous injections of esketamine during the procedure.
Previous studies have shown that intraoperative use of esketamine can reduce the incidence of postoperative nausea and vomiting in patients undergoing thoracoscopic lung nodule resection.22,23 However, this study found no statistically significant difference in the occurrence of postoperative nausea and vomiting between the two groups, which is consistent with domestic and international studies.19,24,25 Furthermore, a meta-analysis on the use of esketamine for postoperative acute pain also indicated that esketamine does not reduce the incidence of postoperative nausea and vomiting.26 Another consideration when using esketamine during the perioperative period is the occurrence of psychiatric adverse reactions such as hallucinations, nightmares, and delirium. In this study, no occurrence of hallucinations or psychiatric symptoms was observed during the follow-up of both groups of patients. Relevant guidelines27 and meta-analyses26,28 have indicated that the perioperative use of esketamine does not increase adverse central nervous system reactions, suggesting that the use of esketamine at this dosage during the perioperative period is relatively safe. Analyses for other secondary outcomes showed no significant difference in length of stay between the two groups, which is similar to national and international studies.25 The study showed no significant differences in extubation time and PACU stay time between the two groups, indicating that the use of esketamine at the dosage of 0.8mg/kg in this study does not affect postoperative recovery of patients.
It has been found that there are age and gender differences in postoperative pain, and that being young and female are risk factors that increase the risk of postoperative rebound pain.2 The results of the present study differed somewhat from the above studies in that the results of the generalised estimating equations for the postoperative pain scores only found a correlation between group, age, and postoperative pain, but there was no statistically significant correlation between gender and pain. This may be attributed to the sample size issue. The gender ratio between the two groups was similar. Additionally, factors influencing postoperative pain intensity are complex, such as patients’ pain perception, the medical proficiency of doctors, duration of hospital stay, etc.29 Therefore, further collection of samples and more in-depth research are needed in the future to explore these factors.
This study has strengths in that it excluded patients with pre-existing central sensitization and pathological pain by using the CSI, DN4, and PCS questionnaires before surgery, thus avoiding the influence of pre-existing neuropathic pain on the assessment of postoperative pain. However, there are also limitations to this study. Firstly, it is a single-center study with a relatively small sample size. Secondly, it only investigated the effects of a fixed dose of esketamine and did not explore other doses. It is possible that lower doses of esketamine may also be effective with fewer adverse reactions, and further research is needed to explore the optimal dosage of esketamine for reducing rebound pain. Thirdly, the follow-up in this study only lasted for one week after surgery, and there was no long-term follow-up at 3 months, 6 months, or longer, making it difficult to determine whether esketamine can improve patients’ long-term quality of life. Further long-term follow-up is needed in the future.
Conclusion
In conclusion, in patients undergoing thoracoscopic lobectomy, fractionated low-dose intravenous administration of esketamine can alleviate postoperative pain scores, decreases the incidence of rebound pain after thoracic paravertebral block cessation, decrease opioid consumption, and does not increase the occurrence of adverse postoperative reactions, which is beneficial to patients’ early postoperative recovery.
Data Sharing Statement
All source data files are available upon request to the correspondence author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17(6):836–844. doi:10.1016/S1470-2045(16)00173-X
2. Jen TTH, Ke JX, Wing KJ, et al. Development and internal validation of a multivariable risk prediction model for severe rebound pain after foot and ankle surgery involving single-shot popliteal sciatic nerve block. Br J Anaesth. 2022;129(1):127–135. doi:10.1016/j.bja.2022.03.030
3. Sunderland S, Yarnold CH, Head SJ, et al. Regional versus general anesthesia and the incidence of unplanned health care resource utilization for postoperative pain after wrist fracture surgery: results from a retrospective quality improvement project. Reg Anesth Pain Med. 2016;41(1):22–27. doi:10.1097/AAP.0000000000000325
4. Li X, Xiang P, Liang J, Deng Y, Du J. Global trends and hotspots in esketamine research: a bibliometric analysis of past and estimation of future trends. Drug Des Devel Ther. 2022;16:1131–1142. doi:10.2147/DDDT.S356284
5. Yang T, Mudabbar MS, Liu B, Xu M, Fu Q. Intraoperative esketamine is effective at reducing acute postoperative pain in bariatric surgery patients: a randomized control trial. Obes Surg. 2023;33(8):2368–2374. doi:10.1007/s11695-023-06676-2
6. Han T, Chen Q, Huang J, et al. Low-dose esketamine with sufentanil for postcesarean analgesia in women with gestational diabetes mellitus: a prospective, randomized, double-blind study. Front Endocrinol. 2023;14:1202734. doi:10.3389/fendo.2023.1202734
7. Touil N, Pavlopoulou A, Barbier O, Libouton X, Lavand’homme P. Evaluation of intraoperative ketamine on the prevention of severe rebound pain upon cessation of peripheral nerve block: a prospective randomised, double-blind, placebo-controlled study. Br J Anaesth. 2022;128(4):734–741. doi:10.1016/j.bja.2021.11.043
8. Lee KH, Kang JH, Oh HS, et al. Intravenous oxycodone versus intravenous morphine in cancer pain: a randomized, open-label, parallel-group, active-control study. Pain Res Manag. 2017;2017:9741729. doi:10.1155/2017/9741729
9. Clephas PRD, Hoeks SE, Singh PM, et al. Prognostic factors for chronic post-surgical pain after lung and pleural surgery: a systematic review with meta-analysis, meta-regression and trial sequential analysis. Anaesthesia. 2023;78(8):1005–1019. doi:10.1111/anae.16009
10. Sun K, Liu D, Chen J, et al. Moderate-severe postoperative pain in patients undergoing video-assisted thoracoscopic surgery: a retrospective study. Sci Rep. 2020;10(1):795. doi:10.1038/s41598-020-57620-8
11. Feray S, Lubach J, Joshi GP, Bonnet F, Van de Velde M; PROSPECT Working Group *of the European Society of Regional Anaesthesia and Pain Therapy. PROSPECT guidelines for video-assisted thoracoscopic surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2022;77(3):311–325. doi:10.1111/anae.15609
12. Spaans LN, Bousema JE, Meijer P, et al. Acute pain management after thoracoscopic lung resection: a systematic review and explorative meta-analysis. Interdiscip Cardiovasc Thorac Surg. 2023;36(1):ivad003. doi:10.1093/icvts/ivad003
13. Woo JH, Lee HJ, Oh HW, Lee JW, Baik HJ, Kim YJ. Perineural dexamethasone reduces rebound pain after ropivacaine single injection interscalene block for arthroscopic shoulder surgery: a randomized controlled trial. Reg Anesth Pain Med. 2021;46(11):965–970. doi:10.1136/rapm-2021-102795
14. Fang J, Shi Y, Du F, et al. The effect of perineural dexamethasone on rebound pain after ropivacaine single-injection nerve block: a randomized controlled trial. BMC Anesthesiol. 2021;21(1):47. doi:10.1186/s12871-021-01267-z
15. Yu L, Zhou Q, Li W, et al. Effects of esketamine combined with ultrasound-guided pectoral nerve block type II on the quality of early postoperative recovery in patients undergoing a modified radical mastectomy for breast cancer: a randomized controlled trial. J Pain Res. 2022;15:3157–3169. doi:10.2147/JPR.S380354
16. Xu LL, Wang C, Deng CM, et al. Efficacy and safety of esketamine for supplemental analgesia during elective cesarean delivery: a randomized clinical trial. JAMA Network Open. 2023;6(4):e239321. doi:10.1001/jamanetworkopen.2023.9321
17. Zhang Y, Cui F, Ma JH, Wang DX. Mini-dose esketamine-dexmedetomidine combination to supplement analgesia for patients after scoliosis correction surgery: a double-blind randomised trial. Br J Anaesth. 2023;131(2):385–396. doi:10.1016/j.bja.2023.05.001
18. Schatzberg AF. Mechanisms of Action of Ketamine and Esketamine. Am J Psychiatry. 2021;178(12):1130. doi:10.1176/appi.ajp.2021.21060653
19. Lei Y, Liu H, Xia F, et al. Effects of esketamine on acute and chronic pain after thoracoscopy pulmonary surgery under general anesthesia: a multicenter-prospective, randomized, double-blind, and controlled trial. Front Med Lausanne. 2021;8:693594. doi:10.3389/fmed.2021.693594
20. Mihaljević S, Pavlović M, Reiner K, Ćaćić M. Therapeutic Mechanisms of Ketamine. Psychiatry Danub. 2020;32(3–4):325–333. doi:10.24869/psyd.2020.325
21. Zhou R, Zhang Y, Tang S, et al. A single preoperative dose of s-ketamine has no beneficial effect on chronic postsurgical pain in patients undergoing video-assisted thoracoscopic surgical lung lesion resection: a prospective randomized controlled study. J Cardiothorac Vasc Anesth. 2023;37(8):1433–1441. doi:10.1053/j.jvca.2023.02.046
22. Long YQ, Wang D, Chen S, et al. Effect of balanced opioid-free anaesthesia on postoperative nausea and vomiting after video-assisted thoracoscopic lung resection: protocol for a randomised controlled trial. BMJ Open. 2022;12(11):e066202. doi:10.1136/bmjopen-2022-066202
23. Yan H, Chen W, Chen Y, et al. Opioid-free versus opioid-based anesthesia on postoperative pain after thoracoscopic surgery: the use of intravenous and epidural esketamine. Anesth Analg. 2023;137(2):399–408. doi:10.1213/ANE.0000000000006547
24. Zhu Y, Li Q, Liu G, et al. Effects of esketamine on postoperative rebound pain in patients undergoing unilateral total knee arthroplasty: a single-center, randomized, double-blind, placebo-controlled trial protocol. Front Neurol. 2023;14:1179673. doi:10.3389/fneur.2023.1179673
25. Massoth C, Schwellenbach J, Saadat-Gilani K, et al. Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy - A randomised controlled trial. J Clin Anesth. 2021;75:110437. doi:10.1016/j.jclinane.2021.110437
26. Wang J, Chen X, Guo J. Comment on ”Perioperative intravenous S-ketamine for acute postoperative pain in adults: a systematic review and meta-analysis”. J Clin Anesth. 2021;75:110490. doi:10.1016/j.jclinane.2021.110490
27. Cohen SP, Bhatia A, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American society of regional anesthesia and pain medicine, the American Academy of pain medicine, and the American society of anesthesiologists. Reg Anesth Pain Med. 2018;43(5):521–546.
28. Brinck EC, Tiippana E, Heesen M, et al. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev. 2018;12(12):CD012033. doi:10.1002/14651858.CD012033.pub4
29. Lin LY, Hung TC, Lai YH. Pain control and related factors in hospitalized patients. Medicine. 2021;100(30):e26768. doi:10.1097/MD.0000000000026768
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
