Back to Journals » International Medical Case Reports Journal » Volume 16
Efficacy of Gefapixant, a P2X3 Antagonist, for Refractory Atopic Cough
Authors Ishiura Y , Nomura S , Ishii Y, Imai K, Sawai Y, Tamaki T , Shimizu T, Miyashita N, Ito T
Received 22 June 2023
Accepted for publication 24 August 2023
Published 4 September 2023 Volume 2023:16 Pages 497—501
DOI https://doi.org/10.2147/IMCRJ.S427098
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yoshihisa Ishiura, Shosaku Nomura, Yuka Ishii, Kai Imai, Yusuke Sawai, Takeshi Tamaki, Toshiki Shimizu, Naoyuki Miyashita, Tomoki Ito
First Department of Internal Medicine, Kansai Medical University, Osaka, Japan
Correspondence: Yoshihisa Ishiura, First Department of Internal Medicine, Kansai Medical University, 10-15 Fumizono-cho, Moriguchi, Osaka, 570-8507, Japan, Tel +81-6-6992-1001, Fax +81-6-6993-9837, Email [email protected]
Abstract: Cough, a frequent symptom encountered in clinical practice, often has a considerable impact on patients’ lives. There is an urgent need to investigate more potent antitussive treatments for chronic refractory cough, particularly atopic cough, which is a major cause of chronic refractory cough in Japan. Previous studies have shown that eosinophilic tracheobronchitis with hypersensitivity to sensory nerve C-fibers is the pathophysiology of atopic cough. Gefapixant is a first-in-class P2X3 antagonist that has recently become available for clinical use in patients with refractory coughs. A 64-year-old female non-smoker presented to our hospital with a complaint of chronic intractable cough due to atopic cough. Addition of gefapixant (90 mg/day) to her previous treatment improved her distressing cough, despite the partial efficacy of many other drugs. The findings of this case demonstrate that P2X3 inhibition is a viable therapeutic option for patients with chronic refractory cough caused by atopic cough. This case report offers valuable information regarding currently available treatment options for refractory chronic refractory cough caused by atopic cough. There remains an urgent need to clarify the disease entities presenting with chronic cough that can be effectively treated by inhibiting P2X3.
Plain Language Summary: There is an urgent need to investigate more potent antitussive treatments for chronic refractory cough, because cough has a considerable impact on patients’ lives. Previous studies have shown that eosinophilic tracheobronchitis with hypersensitivity of sensory nerve C-fibers is the pathophysiology of atopic cough, which is a major cause of chronic cough in Japan. Gefapixant is a first-in-class P2X3 antagonist that has recently become available for clinical use in patients with refractory coughs. Herein, we present the case of a 64-year-old female with a refractory atopic cough. The gefapixant add-on improved her distressing cough, indicating that P2X3 inhibition could be a viable therapeutic option for patients with chronic refractory cough caused by atopic cough.
Keywords: chronic cough, atopic cough, gefapixant, P2X3
Introduction
Cough is one of the most common symptoms seen in general practice and respiratory clinics and can interfere with sleep, work, and social activities. As cough negatively affects a patient’s quality of life, it is important to seek more effective treatments especially if chronically persistent. Chronic cough, defined as a cough lasting for >8 weeks with no overt clinical and radiological evidence of lung disease, is also a common reason for referral to a specialist. European Respiratory Society (ERS) guidelines give rise to phenotypes including asthmatic cough and eosinophilic bronchitis.1 Atopic cough is another clinical phenotype that causes bronchodilator-resistant cough associated with generalized atopy and has been included in Japanese guidelines.2–8 The pathological features of atopic cough include eosinophilic tracheobronchitis without bronchoalveolar lavage eosinophilia (BAL), and the physiological features of atopic cough include cough reflex hypersensitivity without bronchial hyperresponsiveness (BHR) due to hypersensitivity of vagal afferent C-fiber.3–8 Conversely, cough variant asthma appears to be similar to bronchial asthma, with mild BHR and eosinophilic inflammation of central and peripheral airways,9 and a cough that is responsive to bronchodilator therapy.10 Without long-term inhaled corticosteroid therapy, nearly 30% of patients with cough variant asthma will develop typical asthma within a few years.3–8 Nonasthmatic eosinophilic bronchitis (NAEB) is a pathophysiologic disease condition and is used in patients complaining cough but also in asymptomatic eosinophilic patients without cough.3–8 Atopic cough, on the other hand, is an airway disease in which bronchodilators are used to treat chronic dry cough, and eosinophils are not detected in induced sputum or in bronchial mucosa in 10 to 20% of patients.3–8 Atopic cough is considered a major cause of chronic cough in Japan.6 Although approximately 60% of patients with atopic cough respond well to treatment with histamine H1 antagonists, other patients require more potent therapy such as corticosteroids because they have more intense submucosal eosinophilic inflammation of the bronchi.7 As a result, there is a critical unmet clinical need for more potent antitussives for the treatment of refractory atopic cough.4–7 Gefapixant is the first P2X3 antagonist that has recently been approved for use in patients with chronic refractory cough lasting for more than one year.11 However, it remains unknown which disease entities that present with chronic cough can be effectively treated with gefapixant. Herein, we present a patient with atopic cough who was administered gefapixant and exhibited marked improvement in symptomatic cough despite the partial efficacy of many other drugs.
Case Presentation
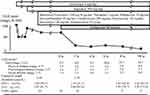
A 64-year-old woman without a history of smoking presented to our hospital with the complaint of chronic non-productive cough lasting for 2 years without wheezing, dyspnea or postnasal drip. No abnormalities were noted on careful auscultatory examination of the lungs. Her peripheral blood eosinophil count, serum immunoglobulin E level, and sputum eosinophil count were 231/μL, 143 IU/mL, and 5%, respectively, suggesting airway eosinophilic inflammation. Chest radiography and computed tomography revealed normal findings, except for a rib fracture due to excessive coughing. Sinus radiography also revealed normal findings. Respiratory function tests revealed a forced expiratory volume in one second (FEV1) of 1.80 L (90.1% of predicted), forced vital capacity (FVC) of 2.01 L (81.7% of predicted), and FEV1/FVC ratio of 0.90, with no bronchial reversibility after bronchodilator inhalation as shown in our previous studies.5,6 Airway hyper-responsiveness was not present, given that provocation with 20 mg/mL methacholine did not change FEV1. The cough threshold for capsaicin inhalation measured by the previously reported method was 0.49 μmol/L, indicating cough reflex hypersensitivity.12 The fractional exhaled nitric oxide (FeNO) was 10 ppb. After 2 weeks of treatment with azelastine, a histamine H1 antagonist, cough severity assessment using a visual analog scale (VAS) score (range, 0–100; higher score = greater severity) showed improvement from 100 mm to 50 mm as in other patients with atopic cough. Based on these findings, a diagnosis of atopic cough was made, although silent postnasal drip syndrome could not be completely ruled out.2–7 After 6 months of follow-up, her cough relapsed, but additional treatment with a Th2 inhibitor, suplatast tosilate, was only partially effective since the VAS improved from 70 mm to 60 mm (Figure 1), which may be related to inability to evade antigen and the existence of multiple causes of cough.13 Other additional treatments with budesonide/formoterol, tiotropium, rabeprazole, dextromethorphan, clarithromycin, amitriptyline, itraconazole, and bakumondo-to were ineffective (Figure 1). Therefore, we decided to administer 90 mg/day (45 mg twice daily) gefapixant, a newly available P2X3 antagonist as an add-on therapy to other treatments.11 After 2 weeks of treatment with gefapixant, the VAS score improved from 70 to 20 mm, and the cough threshold for inhaled capsaicin improved from 0.49 to 1.95 μmol/L. A further cough severity assessment using the Leicester Cough Questionnaire (LCQ) score (range, 3–21; lower score = greater severity)14 started on August 5, 2022, and confirmed improvement from 4.3 to 8.0 (Figure 1). As of April 24, 2023, after 38 weeks of follow-up, her cough had remained stable, with a VAS score of 10 mm and an LCQ score of 14.7, as shown in Figure 1. During this period, there were no abnormal findings in the pulmonary function tests and FeNO values reflecting the results of eosinophilic inflammation in the peripheral airways because the main eosinophilic inflammation occurred in the trachea, as previously reported.2–7 No adverse reactions were observed with gefapixant treatment, including the most frequent adverse reactions and taste problems.11
Discussion
There is an urgent need to seek effective medical treatments for patients with chronic refractory cough because of their profound adverse effects on quality of life and social activities.2–7,11 Kamei et al15 investigated the pathogenic mechanisms of chronic cough and demonstrated the importance of the P2X receptors. Gefapixant is a newly available P2X3 receptor antagonist that has shown efficacy in patients with chronic refractory cough lasting for at least one year.11 However, since chronic cough can be associated with many diseases,6 it remains unknown which disease entities presenting with chronic cough can be effectively treated with gefapixant.
Atopic cough is an important clinical entity as a common cause of chronic cough that lasts for years; however, the presence of some refractory cases remains an important clinical problem.3–7 It is likely that atopic cough differs from “eosinophilic bronchitis without asthma”, with cough hypersensitivity, normal bronchial responsiveness to inhaled methacholine and normal FeNO levels as shown in our previous studies.4–8,16 We previously showed that suplatast tosilate, an orally active Th2 cytokine inhibitor, is an effective therapeutic option for atopic cough;13 however, more potent therapies are still required because their efficacy can be insufficient. It has been shown that atopic cough is caused by hypersensitivity of sensory nerve C-fibers of the central airways.3–7 Gefapixant, an antagonist of the P2X3 receptor, can reduce the cough response by inactivating sensory nerve transmission of the action potential generated after the receptor stimulus including sensory nerve C-fibers.11 Therefore, we consider that gefapixant may be theoretically suitable for the patients with atopic cough and administered gefapixant to patients with chronic severe and refractory cough with lower LCQ scores and higher VAS scores caused by atopic cough. The favorable outcome of this case demonstrates that P2X3 inhibition is a viable therapeutic option for patients with chronic refractory atopic cough.
However, this case report had several limitations, since gefapixant did not completely relieve cough. As complete clinical relief was not achieved, some patients could eventually benefit from other add-on therapies, such as P2X4 antagonists, as suggested by Kamei et al.15 Second limitation is that the dose 10 mg/day of rabeprazole given to this patient was too low for cough due to reflux.17 We have to consider the possibility that the refractory chronic cough is induced by the other unidentified causes in addition to refractory atopic cough. Another limitation is that the assessment of capsaicin cough sensitivity has only been performed in a limited number of facilities and is not commonly conducted in general practice. We hope the test to measure capsaicin cough sensitivity to be used more widely in many clinics to detect patients who may benefit from gefapixent.
In summary, we have presented the first case of marked successful treatment with gefapixant, a newly available P2X3 antagonist, in a patient with refractory atopic cough, despite the partial efficacy of many other drugs. The findings of this case provide valuable information because currently available treatment options for refractory atopic cough are insufficient. There remains an urgent need to clarify the disease entities presenting with chronic cough that can be effectively treated by inhibiting P2X3.
Abbreviations
BAL, bronchoalveolar lavage eosinophilia; BHR, bronchial hyperresponsiveness; NAEB, nonasthmatic eosinophilic ERS, European Respiratory Society; FeNO, fractional exhaled nitric oxide; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; LCQ, Leicester Cough Questionnaire; VAS, visual analog scale.
Ethical Approval
Institutional approval is not required for publication, so written informed consent was obtained from the patient regarding the publication of details.
Acknowledgment
The authors thank Alison Sherwin, PhD, and Edanz (https://jp.edanz.com/ac) for editing the draft of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by a grant form “Private University Research Branding Project on intractable immune and allergic diseases” from Kansai Medical University.
Disclosure
All authors declare that they have no conflicts of interest.
References
1. Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1):1901136. PMID: 31515408. doi:10.1183/13993003.01136-2019
2. Mukae H, Kaneko T, Obase Y, et al. The Japanese respiratory society guidelines for the management of cough and sputum (digest edition). Respir Investig. 2021;59(3):270–290. PMID: 33642231. doi:10.1016/j.resinv.2021.01.007
3. Fujimura M, Niimi A, Naito K, et al. Guidelines for Diagnosis and Treatment of Prolonged and Chronic Cough for Cough Specialists. Kanazawa: Japan Cough Society. Maeda Syoten; 2021:27–31. In Japanese.
4. Fujimura M, Ogawa H, Yasui M, Matsuda T. Eosinophilic tracheobronchitis and airway cough hypersensitivity in chronic non-productive cough. Clin Exp Allergy. 2000;30(1):41–47. PMID: 10606929. doi:10.1046/j.1365-2222.00698.x
5. Fujimura M, Ohkura N, Abo M, et al. Exhaled nitric oxide levels in patients with atopic cough and cough variant asthma. Respirology. 2008;13(3):359–364. PMID: 18399857. doi:10.1111/j.1440-1843.2008.01273.x
6. Fujimura M, Abo M, Ogawa H, et al. Importance of atopic cough, cough variant asthma and sinobronchial syndrome as causes of chronic cough in the Hokuriku area of Japan. Respirology. 2005;10(2):201–207. PMID: 15823186. doi:10.1111/j.1440-1843.00686.x
7. Fujimura M, Nishi K, Ohka T, Yasui M, Kasahara K. Bronchial biopsy and sequential bronchoalveolar lavage in atopic cough: in view of the effect of histamine H1-receptor antagonists. Allergology Int. 2000;49(2):135–142. doi:10.1046/j.1440-1592.2000.00171.x
8. Fujimura M, Sakamoto S, Matsuda T. Bronchodilator-resistive cough in atopic patients: bronchial reversibility and hyperresponsiveness.. Intern Med. 1992;31(4):447–452. PMID: 1352997. doi:10.2169/internalmedicine.31
9. Niimi A, Amitani R, Suzuki K, Tanaka E, Murayama T, Kuze F. Eosinophilic inflammation in cough variant asthma. Eur Respir J. 1998;11(5):1064–1069. doi:10.1183/09031936.98.11051064
10. Corrao WM, Braman SS, Irwin RS. Chronic cough as the sole presenting manifestation of bronchial asthma. N Engl J Med. 1979;300(12):633–637. doi:10.1056/NEJM197903223001201
11. McGarvey LP, Birring SS, Morice AH, et al.; COUGH-1 and COUGH-2 Investigators. Efficacy and safety of gefapixant, a P2X3 receptor antagonist, in refractory chronic cough and unexplained chronic cough (COUGH-1 and COUGH-2): results from two double-blind, randomised, parallel-group, placebo-controlled, Phase 3 trials. Lancet. 2022;399(10328):909–923. doi:10.1016/S0140-6736(21)02348-5
12. Ishiura Y, Fujimura M, Yamamoto H, Ishiguro T, Ohkura N, Myou S. COX-2 inhibition attenuates cough reflex sensitivity to inhaled capsaicin in patients with asthma. J Investig Allergol Clin Immunol. 2009;19(5):370–374. PMID: 19862936.
13. Ishiura Y, Fujimura M, Yamamoto H, et al. Effect of an orally active Th2 cytokine inhibitor, suplatast tosilate, on atopic cough. Arzneimittelforschung. 2008;58(6):297–302. PMID: 18677972. doi:10.1055/s-0031-1296510
14. Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax. 2003;58(4):339–343. doi:10.1136/thorax.58.4.339
15. Kamei J, Takahashi Y, Yoshikawa Y, Saitoh A. Involvement of P2X receptor subtypes in ATP-induced enhancement of the cough reflex sensitivity. Eur J Pharmacol. 2005;528(1–3):158–161. PMID: 16321375. doi:10.1016/j.ejphar.2005.10.030
16. Villalobos-Violan V, Betancor D, Mahíllo-Fernández I, Sastre J. Nonasthmatic eosinophilic bronchitis and asthma Analysis of Biomarkers. J Investig Allergol Clin Immunol. 2022;32(3):216–217. PMID: 34661536. doi:10.18176/jiaci.0738
17. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline: guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):27–56. PMID: 34807007. doi:10.14309/ajg.0000000000001538
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.