Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Efficacy of Electroacupuncture with Sparse-Dense-Wave on Patients Suffered Acute Facial Paralysis
Received 20 January 2023
Accepted for publication 20 June 2023
Published 17 July 2023 Volume 2023:16 Pages 1811—1819
DOI https://doi.org/10.2147/CCID.S405569
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Hao Zhang, Fan Chen
Department of Traditional Chinese Medicine, People’s Hospital of Dongxihu District, Wuhan, Hubei, 430040, People’s Republic of China
Correspondence: Fan Chen, Department of Traditional Chinese Medicine, People’s Hospital of Dongxihu District, No. 48, Jinbei First Road, Jinghe Street, Wuhan, Hubei, 430040, People’s Republic of China, Tel +86 15972944985, Email [email protected]
Objective: To explore the efficacy of electroacupuncture (EA) with sparse-dense wave form on the improvement of facial nerve edema, facial spasm, and repair of nerve injury in patients with acute facial paralysis.
Methods: This study enrolled 100 patients who were treated for acute facial paralysis in People’s Hospital of Dongxihu District from December 2019 to December 2020. They were randomly divided into the control group (continuous wave) and the sparse-dense wave group (sparse-dense wave), following by being intervened by EA with different wave forms. Then the facial disability index (FDI) score, serum levels of immunoglobulin A (IgA), immunoglobulin G (IgG), and immunoglobulin M (IgM) in the two groups were evaluated.
Results: The total effectiveness rate (98.00% and 86.00%, respectively; P < 0.05) and the recovery rate of facial spasm (76.00% and 56.00%, respectively; P< 0.05) in the sparse-dense wave group was both significantly higher than that of the control group. After treatment, the scores of physical functions of patients in both groups increased (P < 0.05), the scores of social/well-being dysfunctions decreased (P < 0.05). Besides, the levels of serum IgA, IgG, and IgM in both groups decreased (P < 0.05), and the serum levels in the sparse-dense wave group were significantly lower than the control group (P < 0.05).
Conclusion: EA intervention with sparse-dense wave form is effective for patients with acute facial paralysis, in that it effectively reduced the occurrence of facial spasm and promoted the improvement of edema and repair of nerve injury.
Keywords: acute phase, electroacupuncture, EA, facial spasm, nerve edema, nerve injury repair, peripheral facial paralysis, sparse-dense wave
Introduction
Peripheral facial paralysis, also known as facial paralysis, is a condition characterized by acute onset of unilateral weakness of facial muscles.1,2 As the most common facial nerve disorder, facial paralysis has annually affected 11.5 to 53.3 per 100,000 persons across multiple populations.3,4 Clinical practice showed that facial paralysis showed no difference in gender and can occurred at any age, with a slightly higher prevalence rate in men after 40 years of age and in women after 20 years of age than that of in other age groups.5 Patients present with numbness and paralysis of the face on the affected side, and may have symptoms such as drooping of corners of the mouth, drooling, and inability to complete actions such as knitting one’s brows and frowning, but without central nervous symptoms such as hemiplegia and confusion.6 The acute onset of this disease is likely to leave sequelae that are difficult to eliminate in case of improper treatment. The etiology of facial neuritis is still not fully elucidated up to now. Various factors such as inflammation,7,8 infection,9,10 and ischemia11 may be the contributors of the incidence of facial neuritis, and viral infection has been considered to the vital the vital factor.
Herein, antiviral treatment and nutritional neurotherapy are mainly used in modern medicine for the treatment of this disease, and acupuncture in traditional Chinese medicine (TCM) is also recognized as effective in treating this condition.12,13 The quantum of stimulation by acupuncture can be controlled. In detail, the waveforms stimulated by electroacupuncture are generally divided into three forms: continuous, intermittent and sparse waves.14 Continuous wave can make muscle tonic contraction by keeping the electroacupuncture instrument output pulse current continuous. Intermittent wave is a type of alternating cycle wave, mainly manifesting as making the muscle tonic contraction for 2s by keeping continuous pulse at intervals of about 2s and then relaxing for 2s. Besides, the dense-sparse wave has features of complexity and repeatability, showing as a continuous output of electrical pulses for 2s and stopping for 2s, then continuous output of electrical pulses for 1 second and stopping for 2s, and following by 2 consecutive outputs for 1 s and stopping for 2s. This process aimed to simulate the smiling expression function of the facial muscles, which could make the muscles to get effective contraction as well as relaxation. However, a query then arises as to whether stimulation with different wave forms have different therapeutic effects on peripheral facial paralysis, and whether EA treatment in the acute stage has therapeutic effects and influences the sequelae in patients.15 Besides, previous report has showed that facial neuritis is associated with an abnormal increase in serum immunoglobulins, suggesting that patients with facial neuritis has abnormal humoral immune function. IgG is the major component of immunoglobulins in serum, accounting for 75% of the total immunoglobulins in serum. The abnormal increase of IgG with a specific affinity for motor neuron endings is an important factor in facial neuritis.16 Herein, in this study, we used EA with sparse-dense wave form to treat patients with acute facial paralysis and observed the effects on improvement of facial nerve edema, facial spasm, repair of nerve injury and serum immunoglobulins.
Materials and Methods
Basic Information
We conducted a prospective study on 100 patients with acute facial paralysis who were treated in People’s Hospital of Dongxihu District from December 2019 to December 2020. Using a random number table, we divided the cases included in the study into the control group (treated with EA with continuous wave form) and the sparse-dense wave group (treated with EA with sparse-dense wave form). There were 50 cases in the control group, consisting of 26 males and 24 females, with an average age of (47.33 ± 9.29) years and the average duration of disease was (7.04 ± 2.85) d. There were 50 cases in the sparse-dense wave group, consisting of 27 males and 23 females, with an average age of (48.06 ± 9.53) years and the average duration of disease was (7.17 ± 2.78) d. This study was reviewed and approved by the Medical Ethics Committee of our hospital.
Diagnostic Criteria
Western Medicine Diagnostic Criteria
We referred to the diagnostic criteria of Neurology Diagnostics.17 ① There is a history of fatigue, cold, or viral infection before onset of disease. ② Acute onset of peripheral facial paralysis symptoms on one side of the face, such as weakness of facial muscles, lessened wrinkling of the forehead, impaired eyelid closure, flattened nasolabial fold, eyebrow ptosis, drooping of the corner of the mouth, deviation of the mouth to the healthy side when showing teeth, etc. The damage to the nerves controlling the facial muscles is between the tympanic cord and the stapedial nerve in the facial nerve canal (Bell’s facial paralysis). In this condition, patients may have clinical symptoms such as facial paralysis, loss of first two-thirds of the tongue’s sense of taste, dysfunction in salivary gland secretion, and hyperacusis. The localized diagnosis was made for the damaged geniculate ganglion and the involvement of great superficial petrosal (Hunt’s facial paralysis). In this syndrome, patients present with facial paralysis, loss of first two-thirds of the tongue’s sense of taste, dysfunction of salivary gland secretion, loss of lacrimal gland secretion, and pain in concha auriculae and the mastoid area. Herpes may also occur in the pinna and external auditory canal, and the symptoms peak within hours or days. ③ No other cranial nerve damage and signs of brainstem long-tract involvement. ④ Neuroelectrophysiological examination shows complete or partial damage of facial nerve.
TCM Diagnostic Criteria
In TCM, peripheral facial paralysis is explained with reference to the syndrome differentiation criteria of external attack due to wind-cold as per the Criteria for Evaluation and Therapeutic Effect of Peripheral Neuroparalysis in the Integrated Chinese and Western Medicine adopted by the Neurological Professional Committee of the Chinese Association of Integrative Medicine in 2007.18 Symptoms include sudden facial distortion, tightness and contracture of the face, stiffness and restlessness, or blinking with tears, aversion to wind and no sweat, or pain behind the ear. The symptoms are mostly caused by catching cold and blowing wind, and the tongue is pale red with thin and white coating, and the pulse is floating, tight or slow.
Staging
The acute phase lasts 1 to 15 days after onset, the recovery phase is between 16 days to 6 months after onset, and the sequelae phase is 6 months after onset.
Inclusion Criteria
① The patient is diagnosed as having acute peripheral facial paralysis as per the above-mentioned diagnostic criteria of Chinese and Western medicine, and the syndrome differentiation type in Chinese medicine is wind-cold invasion syndrome. ② The patient has unilateral onset of facial nerve weakness. ③ The age of the patient is between 18 and 60 years. ④ This is the first onset. ⑤ The patient has no contraindications for acupuncture treatment and is cooperative. ⑥ The patient gave signed informed consent for the study.
Exclusion Criteria
① The patient has cardiovascular and cerebrovascular diseases, malignant tumor, respiratory system diseases, endocrine system diseases, and other diseases that make the patient unsuitable for participation in this study. ② The patient has facial spasm or concomitant epilepsy, Meige’s syndrome or psychogenic hemifacial spasm. ③ The patient has other nervous system diseases. ④ The patient is a pregnant or lactating woman. ⑤ Intolerance to acupuncture treatment.
Methods
Basic Treatment Regimen
The patients in both groups received basic symptomatic treatment, namely, 0.75 mg/d dexamethasone (manufacturer: Guangdong Sancai Shiqi Pharmaceutical Co., Ltd., approval No.: GYZZ H 44024276, specification: 0.75 mg * 100 s) was administered orally for seven days, and the doses were gradually reduced according to the doctor’s advice and the degree of recovery. Patients were prescribed vitamin B1 (manufacturer: Guangdong Hengjian Pharmaceutical Co., Ltd., approval number: GYZZ H44020620, specification: 10 mg*100s, usage and dosage: 10 mg three times a day), vitamin B12 (manufacturer: YunPeng Pharmaceutical Group Co., Ltd., approval number: GYZZ H14023321, specification: 25 ug*100s, usage and dosage: 25 ug each time once a day).
Selection of Needles and Acupoints
Hwato brand acupuncture needles (Suzhou Medical Appliance Factory) with the specifications of 0.3 mm×25 mm and 0.3 mm×40 mm were used for acupuncture, while Greatwall brand KWD-808 pulse electronic therapeutic apparatus (Wujin Greatwall Medical Appliance Co., Ltd.) was used for EA.
The selected acupoints were listed as follows: GB 14 (Yangbai), SI 18 (Quanliao), ST 6 (Jiache), ST 4 (Dicang), ST 2 (Sibai), HN5 (Taiyang), GB 31 (Fengshi, bilateral), LI4 (Hegu, bilateral), and ST 36 (Zusanli, bilateral).
Procedure
The needles and acupoints were routinely disinfected. The 0.3 mm × 25 mm filiform needles were obliquely inserted into GB 14 (Yangbai), ST 2 (Sibai), and HN5 (Taiyang) at a depth of about 0.3 inch, and the 0.3 mm×40 mm filiform needles were perpendicularly inserted into LI4 (Hegu) and SI 18 (Quanliao) at a depth of about 0.8 inch. The perpendicular insertion into SI 18 (Quanliao) was done at a depth of about 0.3 inch, and the horizontal insertion from GB31 (Fengshi) to the opposite side was also performed with the same depth. The ST 6 (Jiache) penetrated 0.75 inch in the direction of ST 4 (Dicang). All the acupuncture needle insertions used the technique of uniform reinforcing-reducing method. After qi arrival, the needles were retained for 30 min. During needle retention, the EA apparatus was switched on, together with a set of electrodes for GB 14 (Yangbai) and HN5 (Taiyang), and a set of electrodes for ST 6 (Jiache) and ST 4 (Dicang), which were connected to the EA apparatus. The waveforms of the control group were selected as continuous wave, with the frequency set at 1 Hz to 2 Hz, and the waveforms of the sparse-dense wave group were selected as sparse-dense wave, with the frequency set at 2 Hz/10Hz. The intensity was adjusted as per the patient’s tolerance. We observed the rhythmic contraction of facial muscles once a day, for 30 minutes each time. One course of treatment consisted of continuous treatment for six days and rest for one day, and both groups of patients were administered four such courses. The patients underwent electromyography (EMG) on the first day after the recovery period and in the sequelae period. During the sequelae period, the patients were followed telephonically for six months to find out the improvement of clinical symptoms such as facial spasm, facial stiffness, and secretion of tears.
Evaluation of Efficacy
The efficacy of EA in the two groups before treatment and after the follow-up was evaluated with reference to scoring criteria and efficacy evaluation criteria as per the peripheral nerve paralysis of integrated traditional Chinese and western medicine evaluation and efficacy criteria.7 Scoring criteria were as follows: The symptoms were evaluated based on 10 actions such as raising the forehead lift, frowning, closing eyes, nose shrug, muscle strength in the affected side, nasolabial folds, cheek bulge, showing teeth, whistling, and lowering the lower lip, with a score of 10.0 points if normal. According to the degree of impairment compared with the healthy side, the patients were scored as 7.5, 5.0, 2.5, and 0.0 points, with a functional score of 100.0. The higher the total score, the better was the therapeutic effect. Grade I was for 100 points, which indicated normal; Grade II was for 75–100 points, which indicated mild dysfunction; Grade III was for 50–75 points, indicating moderate dysfunction; Grade IV was for 25–50 points, indicating severe dysfunction; Grade V was for 0–25 points, indicating very severe dysfunction; Grade VI was for 0 points, indicating complete paralysis. Efficacy criteria were as follows: ① Recovery: The bilateral forehead wrinkles and nasolabial folds were symmetrical again and frowning and closure of eyes were normal. Additionally, there was no air leakage from the corner of the mouth during cheek bulge, no food residue between the teeth and cheeks during eating, and no distortion at the corners of the mouth during talking and laughing. The facial expression was normal, with full functional score. ② Marked improvement: The bilateral frontal wrinkles and nasolabial groove were basically symmetrical, the eye closure was not completely tight, the frowning was slightly weak, zygomatic muscle strength was about grade IV of unarmed muscle strength, no air leakage was noticed during cheek bulge, no food residue was seen between the teeth and cheek during eating, and the angle of mouth was slightly asymmetric during laughing, with the functional score > 75 points. ③ Improvement: The symptoms improved after treatment, that is, the patient with grade IV–VI moved to grade III, with the functional score of 50–74 points. ④ Ineffectiveness: After treatment, the symptoms remained above grade IV and the functional score was < 50 points. Total effectiveness rate = (Recovery + Marked improvement + Improvement)/total cases *100%.
The patients in both groups were evaluated for facial spasm before treatment and after treatment during follow-up. We referred to Cohen’s evaluation criteria for the classification of recovery in facial spasms.19 ① Recovery: The patient has no facial or eyelid traction symptoms; ② Improvement: The clinical symptoms of the patient are markedly relieved, and the facial and eyelid tic symptoms are less frequent; ③ Ineffectiveness: There is no significant improvement in various clinical symptoms and signs of the patient.
Observation Indicators
① EMG was performed on the patients before treatment (T0), on the first day of recovery (T1), and on the first day of sequelae (T2). We measured the latency time of facial nerve F wave movement, amplitude of induced CMAP, and facial nerve conduction velocity. Recording electrodes were connected to the lower surface of orbital orbicularis muscle, stimulating electrodes were connected to the fossa of styloid process, reference electrodes were connected to the back 1 cm from the tip of the brow of outer canthus, and grounding electrodes were connected to the wrist. The band-pass was set at 2 Hz to 10 Hz, stimulation time was 0.1 ms, the quantum of stimulation was gradually increased until the waveform was stable, stable response waveforms were recorded and facial nerve conduction velocity was determined. ② The facial neuromuscular dysfunction of the two groups of patients was evaluated before treatment and after follow-up with reference to the face disability index (FDI).20 The FDI scale consists of two subscales and 10 questions. The first subscale refers to physical function, and consists of five questions. Each question is divided into four grades and scored 2, 3, 4, and 5 points, respectively. The higher the score, the more serious the corresponding dysfunction. The second subscale refers to social/well-being function, and consists of five questions. Each question is divided into six grades and scored 1, 2, 3, 4, 5, and 6 points, respectively. The higher the score, the milder the corresponding dysfunction. ③ Fasting venous blood from patients in both groups was drawn early in the morning before and after treatment, and centrifuged and the serum was separated. The levels of immunoglobulin A (IgA), immunoglobulin G (IgG), and immunoglobulin M (IgM) in the serum of patients were detected using automatic chemiluminescence immunoassay analyzer.
Statistical Analysis
Statistical data in this study were processed and analyzed using SPSS 23.0 software. Intergroup independent sample t-test and intra-group paired sample t-test were used for measurement data that met the normal distribution and homogeneity of variance, and non-parametric test was used for non-compliance. The counting data was tested using χ2; Rank sum test was used for data grade. P < 0.05 was considered statistically significant.
Results
Basic Information
Statistical testing confirmed that there was no difference in basic aspects such as gender, age, and duration of disease between the two groups (P > 0.05), indicating that the groups were feasible for comparison.
Comparison of Efficacy in Terms of Improvement in Facial Paralysis Between the Two Groups
As shown in Table 1, the total effectiveness rate of 98.00% in the sparse-dense waveform group was significantly higher than the 86.00% in the control group (P < 0.05), and the difference was statistically significant.
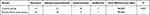 |
Table 1 Comparison of Efficacy in Terms of Improvement in Facial Paralysis Between the Two Groups (n = 50) |
Comparison of Efficacy in Terms of Improvement in Facial Spasm Between the Two Groups
As shown in Table 2, the total effectiveness rate of 98.00% in the sparse-dense group was not significantly different than the 94.00% in the control group (P > 0.05), while the recovery rate of 76.00% in the sparse-dense group was significantly higher than the 56.00% in the control group (P < 0.05), and the difference was statistically significant.
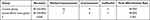 |
Table 2 Comparison of Efficacy in Terms of Improvement in Facial Spasm Between the Two Groups (n = 50) |
Changes of EMG in the Two Groups
As shown in Table 3, there was no significant difference in F-wave duration, F-wave amplitude, and nerve conduction velocity of the affected side between the two groups at T0 (P > 0.05). At T1 and T2, the F-wave duration and F-wave amplitude of the sparse-dense wave group were significantly lower than those of the control group (P < 0.05), and the nerve conduction velocity of the affected side was significantly higher than that of the control group (P < 0.05), with statistical significance.
 |
Table 3 Changes in EMG of Patients in Both Groups ( |
Changes in FDI Scores of Patients in the Two Groups
As shown in Table 4, there was no difference in the physical function scores and social/well-being dysfunction scores of FDI between the two groups before treatment (P > 0.05), but the physical function scores of the two groups increased after treatment (P < 0.05), and the social/well-being dysfunction scores decreased (P < 0.05). Compared with the control group, the change of scores in the sparse-dense wave group was more obvious (P < 0.05), and the difference was statistically significant.
 |
Table 4 Changes in FDI Scores of Patients in Both Groups (Points, |
Changes of Serum Immunoglobulin in the Two Groups
As shown in Table 5, serum IgA, IgG, and IgM levels in patients between the two groups had no difference before treatment (P > 0.05), while serum IgA, IgG, and IgM content in patients of the two groups reduced after treatment (P < 0.05) and those in the sparse-dense wave group were significantly lower than those in the control group (P < 0.05), and the difference was statistically significant.
 |
Table 5 Changes in Serum Immunoglobulin Levels in Both Groups ( |
Discussion
Peripheral facial paralysis, as a disease with sudden onset, manifests as muscle paralysis affecting facial expression including the frontalis muscle, which makes it difficult to perform facial movements such as knitting one’s brows and frowning. Additionally, patients have symptoms such as incomplete eye closure, drooping at the corners of the mouth, and air leakage during cheek bulge, affecting the self-image and psychological state of patients.21 Viral infection and wind-cold-dampness are considered key causes of facial neuritis.22 Patients have pathological changes such as facial edema and demyelination in the early stage, and hence, antiviral drugs and B vitamins are sometimes used as part of the treatment plan in early stages of this disease to relieve the extent of neural edema and promote nerve repair.
Epidemiological survey data estimates that at least 3.35 million people in China suffer from this disease every year.23 The disease can occur at any age, most commonly between 20 to 50 years, and is slightly more common in men.5 Inadequate rest, fatigue, high blood glucose, infection of the upper respiratory tract, and heavy drinking are factors that can reduce immunity, which in turn induces the occurrence of peripheral facial paralysis.
According to the theory of TCM, peripheral facial paralysis is classified in the category of “oblique mouth and eyes”.24 It is believed that the deficiency of vital qi and empty venation, as well as the invasion of pathogenic factors of wind-cold and wind-heat into the facial Yangming and Shaoyang meridians and collaterals will result in the loss of nourishment in meridians, blockage of meridian qi, and relaxation of muscle and fascia. Therefore, the principle of treatment is to disperse wind and pathogenic factors, and regulate qi and blood.25 The courses of facial meridians and collaterals are complex. The pathological change in the facial nerve can lead to inflammatory edema and pain, which can be relieved by dredging meridians and collaterals and harmonizing qi and blood by stimulating acupoints (ST 4, GB 14 and ST 2) closely related to facial nerve.
EA therapy combines ancient acupuncture therapy with modern science. The filiform needles are connected to an EA apparatus and inserted into corresponding acupoints, so that the meridians and collaterals are dredged through the double stimulation of acupuncture and the current on the acupoints.26 After EA treatment, the peripheral nerves usually exhibit slower facial muscle spasms, slightly enlarged nerve endings, and increased number of mitochondria in the body, thus accelerating the repair of peripheral nerves.27 EA sparse-dense wave form refers to the wave with alternating sparse wave and dense wave output. It is believed in TCM that EA with sparse-dense wave form can strengthen blood and lymphatic circulation and guide muscle contraction and relaxation, thereby relieving facial pain in patients. The therapeutic effect is most marked in the acute stage of peripheral facial paralysis.28
EA with sparse-dense wave form can promote blood circulation and increase blood flow in the face, assist in the absorption of edema and nutrition metabolism of the facial nerve, and accelerate the repair of facial nerve damage. It is applied on the affected side of HN5 (Taiyang), SI 18 (Quanliao), ST 4 (Dicang), ST 6 (Jiache), GB 31 (Fengchi, bilateral), LI4 (Hegu, bilateral), and ST 36 (Zusanli, bilateral), and all the acupoints are used in coordination to dredge the Yangming meridians and achieve the effect of dispelling wind.29 Chen et al30 studied 70 patients with acute peripheral facial paralysis and found that using EA sparse-dense wave auxiliary intervention could lead to better recovery of facial nerve function, reduce pain, and improve the therapeutic effect. Our current study found that the total effectiveness rate of 98.00% in the sparse-dense wave group was significantly higher than the 86.00% in the control group, and the recovery rate of facial spasm of 76.00% in the sparse-dense wave group was significantly higher than the 56.00% in the control group, indicating that EA intervention with sparse-dense wave form could improve the therapeutic effect and the recovery rate of facial spasm in patients with acute facial paralysis. This may be due to the fact that EA stimulated the regeneration of damaged facial nerves by promoting the recovery of axoplasmic flow after nerve transection while increasing facial blood flow and reducing muscle glycogen decomposition, thereby slowing muscle atrophy and relieving facial nerve palsy in the early stage of onset. The time duration and amplitude of F wave in the sparse-dense wave group were significantly lower than those in the control group at T1 and T2, and the nerve conduction velocity on the affected side was significantly higher than that in the control group, suggesting that the EA intervention with sparse-dense wave form could promote the repair of nerve injury on the affected side.
Clinical facial nerve electrophysiological examination, including facial EA, facial nerve EMG, and other aspects, are expressed in terms of the common amplitude and latency of nerve fibers in response to electrical stimulation.31 After treatment, the scores of physical function and social/well-being dysfunction increased and decreased, respectively, in both the groups. Compared with the control group, the change of scores in the sparse-dense wave group was more obvious, indicating that EA with sparse-dense wave form could improve facial muscle function, physical function, and social/well-being. After treatment, the serum IgA, IgG, and IgM levels in patients in the two groups decreased, and those in the sparse-dense group were significantly lower than those in the control group, confirming that the immune system played an important role in the body’s inflammatory response among these patients. Immunoglobulins such as IgA, IgM, and IgG can cooperate with phagocytes to exert immune protection for a long time and can also activate the complement system to protect the body, while reducing repeated attacks of the disease, and improving the treatment effect.
In conclusion, EA intervention with sparse-dense wave form shows good therapeutic effect in patients with acute facial paralysis, in that it could effectively reduce the degree of facial spasm and reduce the inflammatory response of the body, thereby promoting the improvement of neural edema and repair of nerve injury, while further improving facial muscle function.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
We confirm that we have read the Editorial Policy pages. This study was conducted with approval from the Ethics Committee of People’s Hospital of Dongxihu District.(Approval date: 2018.2.28). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
Wuhan Municipal Health and Family Planning Commission Scientific research project, Youth Project (project name: Clinical Efficacy of Electroacupuncture Dilatational Wave Treatment of Acute-Stage Facial Paralysis No: WZ18Q15).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Yu Z, Shen M, Shang W, Wu J, Xuan L, Khalaf OI. Timing of acupuncture treatment in peripheral facial paralysis: a systematic review and meta-analysis. Comput Math Methods Med. 2021;2021:4221955. PMID: 34956397; PMCID: PMC8694981. doi:10.1155/2021/4221955
2. Wang F, Li Q, Yu Q, Liang J, Xu Y, Chen G. The efficacy and safety of acupoint catgut embedding for peripheral facial paralysis: a protocol for systematic review and meta analysis. Medicine. 2021;100(46):e27680. PMID: 34797292; PMCID: PMC8601333. doi:10.1097/MD.0000000000027680
3. Monini S, Lazzarino AI, Iacolucci C, et al. Epidemiology of Bell’s palsy in an Italian Health District: incidence and case–control study. Acta Otorhinolaryngol Ital. 2010;30(4):198. PMID: 21253285; PMCID: PMC3008145.
4. Rogalska E, Skowronek-Bala B, Swierczynska A, et al. Bell’s palsy in malopolska’s children in 2010–2014 years. Przegl Lek. 2016;73(3):170–173. PMID: 27349048.
5. Huang P, Liu M. 神经科专病中医临床诊治 [Clinical Diagnosis and Treatment of Neurological Diseases in Traditional Chinese Medicine]. Beijing: People’s Medical Publishing House; 2005. Chinese.
6. Sun Z, Ma T, Huang X, et al. 大秦艽汤联合针刺治疗急性周围性面瘫疗效及对面神经肌电图的影响 [Efficacy of Gentiana macrophylla decoction combined with acupuncture on acute peripheral facial paralysis and its effect on facial nerve EMG]. J Emerg Trad Chin Med. 2021;30(5):877–879. Chinese. doi:10.3969/j.issn.1004-745X.2021.05.035
7. Atan D, Ikincioğulları A, Köseoğlu S, et al. New predictive parameters of Bell’s palsy: neutrophil to lymphocyte ratio and platelet to lymphocyte ratio. Balkan Med J. 2015;32(2):167–170. PMID: 26167340; PMCID: PMC4432696. doi:10.5152/balkanmedj.2.015.15456
8. Kum RO, Yurtsever kum N, Ozcan M, et al. Elevated neutrophil-to-lymphocyte ratio in Bell’s palsy and its correlation with facial nerve enhancement on MRI. Otolaryngol Head Neck Surg. 2015;152(1):130–135. PMID: 25347990. doi:10.1177/0194599814555841
9. Abdel-Aziz M, Azab NA, Khalifa B, et al. The association of Varicella zoster virus reactivation with Bell’s palsy in children. Int J Pediatr Otorhinolaryngol. 2015;79(3):328–331. PMID: 25599860. doi:10.1016/j.ijporl.2014.12.010
10. Zandian A, Osiro S, Hudson R, et al. The neurologist’s dilemma: a comprehensive clinical review of Bell’s palsy, with emphasis on current management trends. Med Sci Monit. 2014;20:83–90. PMID: 24441932; PMCID: PMC3907546. doi:10.12659/MSM.889876
11. Grewal DS. Bell’s palsy-tertiary ischemia: an etiological factor in residual facial palsy. Indian J Otolaryngol Head Neck Surg. 2018;70(3):374–379. PMID: 30211092; PMCID: PMC6127045. doi:10.1007/s12070-018-1381-9
12. Wang W, Chen Y, Li Z, et al. 针刺结合手法治疗急性期周围性面瘫的疗效观察 [The curative effect of acupuncture combined with technique in acute peripheral facial paralysis]. J Emerg Trad Chin Med. 2021;30(9):1638–1640. Chinese. doi:10.3969/j.issn.1004-745X.2021.09.035
13. Yovitania V, Fu QH, Pei J, Zhou H. Neuroprotective effect of electroacupuncture against acute ischemic stroke via PI3K-Akt-mTOR pathway-mediated autophagy. World J Tradit Chin Med. 2022;8(3):339–349. doi:10.4103/2311-8571.333712
14. Liu L, Zhu Y, Li Q, et al. 不同波型电针治疗周围性面瘫的疗效比较与安全性评价 [Comparison of efficacy and the safety evaluation of electroacupuncture with different waveforms for peripheral facial paralysis patients]. Chin Acupunct Moxibus. 2012;32(07):587–590. Chinese. doi:10.13703/j.0255-2930.2012.07.005
15. Xu X, Pan J, Chen J, et al. 透刺法联合麦粒灸治疗周围性难治性面瘫的临床观察 [Clinical observation of penetrating method and wheat moxibustion in the treatment of peripheral refractory facial paralysis]. J Guangzhou Univ Tradit Chin Med. 2022;39(3):569–574. Chinese.
16. Lu L, Liang J, Xie X. 电针治疗面瘫的护理体会 [Nursing experience of electroacupuncture treatment of facial paralysis]. Pract J Clin Med. 2008;15:32–33. Chinese.
17. Chen S. 神经疾病诊断学 [Neurological Disease Diagnostics]. Vol. 24. Shanghai Science and Technology Press; 2006:233–235. Chinese.
18. Yang W, Wu F, Zhang M. 周围性面神经麻痹的中西医结合评定及疗效标准(草案) [Evaluation and efficacy criteria of integrated traditional Chinese and western medicine in peripheral facial nerve palsy]. Chin Med Assoc. 2006;3(9):786–787. Chinese. Chinese. doi:10.3969/j.issn.1672-1349.2005.09.018
19. Ma H, Li J, Yu F. Visual analysis of CiteSpace knowledge map of acupuncture and moxibustion in treating peripheral facial paralysis. J Clin Acupunct Moxibus. 2021;37(6):57–62. doi:10.19917/j.cnki.1005-0779.021119
20. Bei B, Zhong W, Lao J. Clinical observation on electric acupuncture combined with needle warming moxibustion on peripheral facial paralysis by yin and yang meridians of both lower limbs. J Emerg Trad Chin Med. 2020;29(3):453–455. doi:10.3969/j.issn.1004-745X.2020.03.020
21. Di Y, Xun J, Zhou J. 小续命汤加减治疗周围性面瘫急性期(风寒袭络证)的疗效观察 [Observation on the curative effect of XiaoXumingtang on acute phase of peripheral facial paralysis (Wind cold attack collateral syndrome)]. J Emerg Trad Chin Med. 2022;31(6):1074–1076. Chinese.
22. Ye Y, Yang Y, Zhu L, et al. 隔牵正散灸联合挂针法治疗急性期周围性面瘫(风寒证)的临床研究 [Clinical study on the treatment of acute peripheral facial paralysis (Wind cold syndrome) by Geqianzheng powder Moxibustion combined with hanging needle method]. J Emerg Trad Chin Med. 2020;29(2):305–308. Chinese.
23. Long H, Feng S, Li B, et al. 半刺法配合透灸法治疗周围性面瘫急性期(风寒证)的临床观察 [Clinical observation of half acupuncture combined with thorough moxibustion in the treatment of acute phase of peripheral facial Paralysis (wind chill syndrome)]. J Emerg Trad Chin Med. 2020;29(10):1829–1831. Chinese. doi:10.3969/j.issn.1004-745X.2020.10.038
24. Yan M, Zeng J, Lin S, et al. Clinical observation on the treatment of acute peripheral facial paralysis with semi-acupuncture of filiform fire needle combined with yifeng acupoint ultrasonic induction of traditional Chinese medicine. J Emerg Trad Chin Med. 2022;31(4):626–629.
25. Li L, Li Z, Wang Y, et al. 蜂针经穴散刺法结合针刺治疗恢复期周围性面瘫临床研究 [Clinical study on bee needle acupuncture for convalescent peripheral facial paralysis]. J Clin Acupunct Moxibus. 2022;38(2):17–20. Chinese.
26. Li W, Li G, Guo X, et al. Rules of acupoints selection of electro-acupuncture in treating acute peripheral facial paralysis based on complex network. J Clin Acupunct Moxibus. 2020;36(10):48–52.
27. Gao C, Zhuang J, Zhang F. 常规针刺配合浅针法对急性期周围性面瘫患者疼痛,面动脉血流动力学及面部肌电图的影响 [Effects of conventional acupuncture combined with shallow acupuncture on pain, facial arterial blood flow dynamics and facial electromyography in patients with acute peripheral facial paralysis]. J Emerg Trad Chin Med. 2022;31(4):690–693. Chinese.
28. Zeng W, Yu X. 悬挂针联合麦粒灸治疗急性期周围性面瘫的临床观察 [Clinical observation of hanging needle combined with wheat moxibustion in the treatment of acute peripheral facial paralysis]. J Emerg Trad Chin Med. 2022;31(6):1040–1042. Chinese.
29. Xu M, Lu S, Yang S. Effects of acupuncture combined with chaihu guizhi decoction on clinical efficiency and facial function recovery in Bell’s facial paralysis patients of acute wind-cold type. J Emerg Trad Chin Med. 2020;29(8):1391–1394. doi:10.3969/j.issn.1004-745X.2020.08.021
30. Chen F, Chen Q, Zhang H. 电针疏密波辅助治疗周围性面瘫急性期临床观察 [Clinical observation of electro-acupuncture and densification wave assisted treatment of acute peripheral facial paralysis]. J Emerg Trad Chin Med. 2022;31(5):878–881. Chinese.
31. Wu X, Dong G, Mu S, et al. 周围性面瘫患者针灸治疗前后面部表情肌弹性与面神经功能评分的相关性 [Correlation between facial expression muscle elasticity and facial nerve function score in patients with peripheral facial paralysis before and after acupuncture treatment]. J Clin Ultrasound Med. 2022;24(5):363–367. Chinese.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



