Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Efficacy Of Dual-Task Training With Two Different Priorities Instructional Sets On Gait Parameters In Patients With Chronic Stroke
Authors Sengar S, Raghav D, Verma M, Alghadir AH, Iqbal A
Received 10 December 2018
Accepted for publication 1 September 2019
Published 17 October 2019 Volume 2019:15 Pages 2959—2969
DOI https://doi.org/10.2147/NDT.S197632
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Shilpi Sengar,1 Deepak Raghav,1 Meenakshi Verma,1 Ahmad H Alghadir,2 Amir Iqbal2
1Department of Physiotherapy, Santosh Medical College, Ghaziabad, Uttar Pradesh, India; 2Rehabilitation Research Chair, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia
Correspondence: Amir Iqbal
G95-1, Rehabilitation Research Chair, College of Applied Medical Sciences, King Saud University, P.O. Box.10219, Riyadh 11433, Saudi Arabia
Tel +966 1 4696010
Fax +9661 4693589
Email [email protected]
Purpose: Balance is controlled through a complex process involving sensory, visual, vestibular and cerebral functioning which get affected by various neurological disorders such as in stroke. Various types of exercises are designed to address the imbalance that is developed due to these neurological disorders. This study aimed to compare the efficacy of dual-task training using two different priority instructional sets in improving gait parameters in patients with chronic stroke.
Methods: This study was a randomized, pretest-posttest experimental group design that compared between two different priority instructional sets (fixed versus variable) of the dual-task training. A convenience sample of thirty patients with chronic stroke due to ruptured middle cerebral artery (mean age±SD = 55.76±5.23; range 48–65 years) was recruited and equally allocated into two groups. Group 1 received dual-task training with fixed priority instructional sets and group 2 received dual-task training with variable priority instructional sets. Both groups were trained for a period of 45 mins each session, 3-sessions per week for 4 weeks. The timed 10-m walk test and foot prints on walkway paper were used to assess the gait parameters (walking speed, stride length and step length) before and after the training session.
Results: Within-group analysis revealed a significant improvement (p<0.05) on gait parameters for both the groups. Furthermore, Cohen’s d calculation for the treatment effect size revealed highly larger effect size on gait parameters in group 2 (Cohen’s d>2 SD) than group 1 (Cohen’s d<2 SD) for the all variables.
Conclusion: The dual-task training with variable priority instructional sets (group 2) was more effective than dual-task training with fixed priority instructional sets (group 1) in improving gait parameters such as gait speed, stride length, and step length in patients with chronic stroke. Physiotherapists should spread awareness and use this specific set of exercises (variable priority instructional sets) while performing a dual-task balance training program among patients with chronic stroke.
Keywords: stroke, gait velocity, stride length, step length, dual-task balance training, fixed priority training, variable priority training
Introduction
Balance can be understood as a complex process that involves the reception and integration of sensory inputs, the planning, and execution of a movement to accomplish a targeted goal of upright posture and the capability to maintain the center of gravity (COG) against the base of support (BOS) in a certain sensory condition either with eye open or closed.1–3 Normally, in the standing position, the COG lies slightly forward of the S2-spinal level. The peripheral sensory inputs (vestibular systems, visual, and bilateral somatosensory receptors) contribute to controlling postural balance.1,4 Somatosensory receptors provide information about muscle lengthening-shortening, contraction-relaxation, stretch-stress, tension, pain, temperature, pressure, and joint position.4 Visual receptors contribute to environmental orientation and postural control.3,5 The vestibular system contributes to the maintenance of the static and dynamic balance of the head in relation to the COG or change of BOS.6 This system also contributes directly to postural stability with coordinated antigravity muscular activities.1,2
Certain conditions, diseases, or syndromes may lead to a deficit in balance abilities, such as the loss of midline orientation because of the inability to integrate visual, vestibular, and somatosensory responses or vertigo due to unequal firing from opposite sides of the vestibular system.3,7 Balance abilities are also influenced by other systems; for instance, attention deficits that reduce a person’s cognizance of environmental hazards and opportunities interfere with anticipatory postural control.8 Injuries to these systems (attention, cognition, and memory) may critically affect the optimal balance function in hemiplegic and head-injured patients.1 In addition, significant deterioration in the function of the sensory system, reduction in muscle strength/volume/mass, alteration in the motor unit, and postural abnormalities are all risk factors for an impairment in the balance mechanism with the aging, and are responsible for postural instability, falls, and even death.5,9,10
Falls among older adults are a considerable public health issue, as well as a potential reason for injury and even death.11 They annually affect approximately 33% and 50% of elderly people aged older than 65 years and 80 years, respectively.10,12 The neurological disorders, diseases, and syndromes that arise due to aging interfere with the gait pattern, walking speed, and gait stability.13 Footwear and obesity have been identified as risk factors for postural instability and mobility impairments, respectively, and are thus involved in accidental falls among older adults.14,15
Stroke patients face frequent falls while walking because of their physical environment, loss of balance ability, functional impairments and restriction in activities and participation realm; however, the falls reduce as the balance function of the body-system improves.16 Many systematic reviews and meta-analyses have examined walking and balance ability in stroke patients and reported the efficacy of specific exercise programs, such as aerobic (endurance), strengthening (muscle strength), stretching (flexibility), mobility (range of motion), sensory (single/combination), and vestibular training combined with dual-task training (walking, postural control, and falls).17–20
A dual-task training program is superior to a single-task training program and plays an important role in improving the postural control that aids in improving gait speed and balance abilities among older adults.21,22 Dual-task is defined as the ability to accomplish two or more cognitive and motor activities simultaneously while maintaining postural control.23 In addition, the dual-task paradigm is the primary approach used to assess and establish the interaction between cognitive processes and motor performance.22,23 An obvious instruction regarding attentional focus plays an important role in contributing to the rate of learning and the retention of the dual-task training effect.22 Dual-task including both motor and cognitive training brought a significant improvement in balance abilities and gait speed among patients with chronic stroke.24 However, in our knowledge, none of the studies examined the efficacy of dual-task training with either fixed or variable priority instructional sets on gait speed and other gait parameters such as stride and step length among patients with chronic stroke. Therefore, this study needed to assess the gait parameters in patients with chronic stroke.
This study aimed to investigate whether dual-task training with variable priority instructional sets is more effective than that with fixed priority instructional sets in improving gait parameters in patients with chronic stroke.
Materials And Methods
Study Design
This study based on pretest-posttest experimental group design.
Ethical Approval
This study followed the ethical standards for human research and obtained an ethical clearance from the ethics sub-committee of King Saud University (ID: RRC-2017-005). A written informed consent was obtained from each participant, and this study was conducted in accordance with the declaration of Helsinki. Furthermore, this study got registered on ClinicalTrials.gov Protocol Registration and Results System (ID: NCT03752788).
Sampling
Convenience sampling method was used to collect the sample. The G*Power 3.1.9.4 used to calculate the effective sample size was based on our pilot study. A priori paired t-test (matched pairs) indicated that an effective sample size of 28 was required to achieve a statistical power of 80% (0.80) to detect the training effect size (0.569) at the 0.05 level of significance. The difference between two means and standard deviation were 1.2 and 1 respectively.
Participants
Thirty participants with chronic stroke were recruited for this study from the out-patents department at neuro-rehabilitation center of our university hospital. The baseline characteristics of all the participants including age, height, weight, BMI, side of lesion, onset of stroke, stages of stroke recovery assessed according to Brunnstrom approach and the muscle tone of paretic limb assessed by Ashworth scale and other screening parameters were documented prior to the study. The participants those were a diagnosed case of chronic stroke (due to ruptured middle cerebral artery) made by a neurologist and verified using CT/MRI25 exhibited the age between 45 and 65 years;26 ability to walk 10 m without assistance;22 their stroke onset between 6 and 12 months prior to the study;25 and scored greater than 24 on Mini-Mental State Examination (MMSE)23 in this study. However, those who had neurological conditions other than stroke, uncontrolled hearing or visual and vestibular impairment took more than 15 s on Timed Up & Go (TUG) test, had lower extremity amputation, a case of diagnosed speech-language impairment (not able to respond verbally to auditory stimuli) by a speech-language pathologist, and noticed their concurrent participation in another clinical trial were excluded for this study.25
Procedure
The community living patients with chronic stroke (due to ruptured MCA) called through advertisements in newspaper for the evaluation of the condition of their stroke at the neuro-rehabilitation center of our university hospital. Those who met the inclusion criteria were recruited for this study through a convenience sampling method. These subjects were randomly distributed using online website Randomization.com (https://:www.randomization.com) into groups 1 and 2. Group 1 consisted of 15 patients, who received dual-task balance training with a fixed priority instructional set. Attention was focused on both postural and cognitive tasks throughout this session. Group 2 consisted of 15 patients who received dual-task training with variable priority instructional sets. During the first half of the training session, attention was focused on postural tasks such as step forward, backward and sideway, while during the remaining half of the session, attention was focused on cognitive tasks such as the remembering of words, counting forward (1,4,7,10 …) and backward (… 10,7,4,1) by adding 3 to the digits.27 The schematic presentation of procedures of this study can be understood through Figure 1.
 |
Figure 1 Flow-diagram of procedures (participant selection, allocation into groups and data collection). |
In postural/motor tasks, subjects were instructed to perform the task with a narrow base of support (reduced step-width) on a narrow path marked on the ground. They were instructed to walk forward, backward, step and sideways on that narrow path along with a cognitive task of counting three. In cognitive task, they were instructed to count and add by three to the digits in increasing (1,4,7,10 …) and decreasing (… 10,7,4,1) order while going forward and coming back to the original point, respectively. They were also instructed to walk with narrow base of support, step, sideways, backward avoiding the obstacles (holding a basket) with a cognitive task to remember the words.23
In the beginning, all the participants received a traditional intervention including slow sustained stretching (hold time 10 s/stretch, 10-repetitions/session) and active range of motion exercises (10-repetitions/session) to the upper and lower extremities. Later on, they received a dual-task balance training sessions of 45 mins per day, 3 times a week for 4 weeks, so as to complete 10–12 hrs of training in order to improve the balance performance.23 This included 12 repetitions in each session for 30 mins. Excluding the initial 3 repetitions (no cognitive task), the rest 9 repetitions were performed under dual-task conditions.25
The mini-mental state examination (MMSE) scale was used as a screening tool to determine any impaired cognition that would affect the ability of the participant to follow instructions.27 All the patients performed the timed 10-m walk test comfortably with their own preferred pace before and after the training sessions (12 sessions).28 Subjects ambulated 9.2 m (30 feet) on a paper walk-way with ink patches on their foot, which left behind a foot print record. Ambulation time for 6.1 m (20 feet) was recorded with a stopwatch. The first and last 1.5 m (5 ft.) of the walk were not used. We obtained footprints on paper walkway to measure stride length and step length.29 The stride length is the actual distance between the two successive placement of the same foot.29 The step length is the distance by which the named foot (either right or left) moves forward in front of the other one.29,30
The MMSE concentrates only on the cognitive facets of the brain functions. It includes eleven questions to assess general cognitive ability, such as orientation to date, day, season and year; registration (immediate recall); attention and calculation; ability to recall of 3-words and dialect. Its total score ranges between 0 and 30. A score of 24 or below on the MMSE indicates decreased cognitive ability (e.g. dementia), however greater or equal to 25 on MMSE is an indicative of preserved cognitive ability. This test has shown good test-retest reliability with the same (r = 0.887) or different (r = 0.827) examiners.31
The timed 10-m walk test evaluates gait speed in patients with chronic stroke with high inter-rater reliability results (ICC=0.998) using the Emory Functional Ambulation Profile (E-FAP).32 The timed 10-m walk test measures gait speed (ICC=0.80) over a short distance in the clinic where people are undergoing inpatient rehabilitation after stroke.30
Temporal-distance measure using ink footprint record evaluates step length and stride length.29 Timed Up & Go (TUG) test scores showed excellent reliability (ICC>0.95) and are able to identify the patient’s mobility with respect to healthy elderly subjects, such as the gait parameters (ϱ range=0.620–0.900; p<0.05) and walking endurance (ϱ=−0.960; p<0.01) in subjects with chronic stroke.33 The TUG score correlates with gait speed, balance, functional level, ability to go out, and this score can change over time.
Materials
A chair with arm rests and 46cm seat height, stopwatch, shoe box (height – 10 cm; width – 19 cm; length – 33 cm), clear and plane surface of l0m in length, marker, 4 steps with hand railing, measuring tape, sticky tape, pencil, paper, ink, and basket were used to assist in assessing the outcomes in this study.
Statistical Analysis
Statistical analysis was done by using SPSS ver.21 (SPSS, Chicago, IL, USA). The Kolmogorov–Smirnov test of normality confirmed that the sample distribution matches the characteristics of a normal distribution (D=0.129; p=0.654). Further, Levene’s test of homogeneity of variance verified. Therefore, a parametric Student’s t-test (un-paired t-test) was applied to compare between and within the groups for all variables. Further, Cohen’s d test was applied to measure the training effect-size within the group. The level of significance was set at p<0.05.
Results
The present study compares the effect of dual-task training with two different priority instructional sets (Fixed and Variable Priority) on gait parameters in patients with chronic stroke.
The ages of group 1 and group 2 ranged from 48 to 64 years and 48 to 65 years, respectively, with a mean (± SD) of 55.93 ± 4.93 years and 55.60 ± 5.53 years, respectively. Furthermore, side of lesion (left/right), the percentage distributions of male and female subjects with their BMI scores, the average scores of MMSE, TUG and E-FAP in group 1 and group 2 are described in Table 1.
 |
Table 1 Demographic Characteristics (Mean ± SD) Of Both The Groups |
The subjects of two groups were matched by age and gender, thus comparable and these may also not influence the study outcome measures (effect of trainings on comfortable preferred walking speed, maximal walking speed, step length, and stride length) (p< 0.05). Interpreting Cohen’s d treatment effect size as d < 0.2 Small effect – mean difference is <0.2 standard deviation; d < 0.2–0.5 Medium effect – mean difference is 0.2–0.5 standard deviation; d > 0.5–1.0 Large effect – mean difference is 0.8–1.0 standard deviation; d>1 Highly Large effect – mean difference is >1.0 standard deviation.
Outcome Measures
Effect On Comfortable Preferred Walking Speed
Table 2 shows that the mean scores of timed 10-m walk test with comfortable preferred walking speed in both groups improved significantly (p<0.05) after the training. Further, the treatment effect size (Cohen’s d test) was found higher in group 2 (d=2.422) than in group 1 (d=0.805). In addition, pretest and posttest mean differences between the groups can be understood in Figure 2.
 |
Table 2 Pretest-Posttest Comparison Of Timed 10-M Walk Test With Comfortable Preferred And Maximal Walking Speed (m/s) Within Each Group |
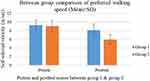 |
Figure 2 Pretest and posttest comparison of mean-preferred walking speed (m/s) between the groups (p<0.001; Cohen’s d=1.702 standard deviation). |
Effect On Maximal Walking Speed
Table 3 shows that the mean scores of timed 10-m walk test with maximal walking speed in both groups improved significantly (p<0.05) after training. Further, the treatment effect size (Cohen’s d test) was found higher in group 2 (d=2.357) than in group 1 (d=0.838). In addition, pretest and posttest mean differences between the groups can be understood in Figure 3.
 |
Table 3 Pretest-Posttest Comparison of Step Length and Stride Length within Each Group (n=15) |
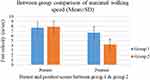 |
Figure 3 Pretest and posttest comparison of mean maximal walking speed (m/s) between the groups (p<0.001; Cohen’s d=2.0745 standard deviation). |
Effect On Step Length
Table 4 shows that the mean step length in both groups improved (p<0.05) after training. Further, the treatment effect size (Cohen’s d test) was higher in group 2 (d=3.977) than in group 1 (d=1.628). In addition, pretest and posttest mean differences between the groups can be understood in Figure 4.
 |
Table 4 Comparison of Pretest and Posttest Step Length (mean ± SD, N=15) within the Group |
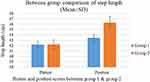 |
Figure 4 Pretest and posttest comparison of mean step length between the groups (p<0.001; Cohen’s d=3.044 standard deviation). |
Effect On Stride Length
Table 5 shows that the mean stride length in both groups improved significantly (p<0.05) after training. Further, the treatment effect size (Cohen’s d test) was higher in group 2 (d=3.159) than in group 1 (d=1.628). Moreover, pretest and posttest mean differences between the groups can be understood in Figure 5.
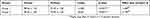 |
Table 5 Comparison Of Pretest And Posttest Stride Length (Mean ± SD, N=15) Within The Group |
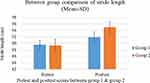 |
Figure 5 Pretest and posttest comparison of mean stride length between the groups (p>0.001; Cohen’s d=1.871). |
Discussion
This study aimed to analyze the effect of a dual-task training program with instructional sets with two different priorities on gait parameters in patients with chronic stroke. This study revealed that it is achievable to implement individualized dual-task training in combination with traditional interventions, including different cognitive tasks in patients with chronic stroke. This study also showed that the patients with chronic stroke adhered to the instructional sets of attention focus and also learned to comply with either variable or fixed priority instructions. The results of this study are consistent with those of other studies that revealed the importance of attention resources used in dual-task training and prepared the background for the use of strategic plan to train the balance.23,27
In our study, the participants of the group 2, who focused on variable priority instruction sets, learned and retained the task faster than the participants of group 1, who focused on dual-task training with fixed priority instructional sets. It could be understud by previously published study which revealed that after training, the processing demands of participants were needed to accomplish the task less when their attention was shifted between two tasks as similar in dual-task training with variable priority instruction group.27 In addition, previous study reported that the optimization of interaction among visual, somatosensory, and vestibular systems results in balance improvement in adults of 65 years of age and older. Interestingly, the same study also proved that the deteriorating balance function could be reversed with the help of balance training.34 Another study suggested that the incorporation of both motor and cognitive tasks as dual-task training brings a significant improvement on balance and daily living abilities among patients with stroke.35
The data support our experimental hypothesis that dual-task training with variable priority instructional sets is more effective than that with fixed priority instructional sets in improving gait parameters in patients with chronic stroke. The results of the inter-group comparison after 4-weeks post-training sessions revealed the progress for both groups 1 and 2. Group 2, those trained with variable priority instructional sets, reported more improvement than group 1, those trained with fixed priority instructional sets in gait velocity, step length, and stride length of the patients with chronic stroke. Evidence supports that the temporal motor parameters improved when subjected to external auditory cues while walking and pointed out the auditory paced stimulation as a novel and inexpensive tool that brought the improvement in gait parameters and gait rehabilitation in patients with Parkinson’s disease.27 That is why we chose a rhythmic auditory tone discrimination as an important component in our study protocol.27
Task-coordination skills are developed by practicing the two tasks together, rather than practicing a single task at onetime.21 Dual-task performance is improved through the efficacious integration and coordination between two tasks while practicing dual-task training.22 Though, individual-task performance gets automatized upon practicing only one task (single-task training) at onetime.28 Notably, the results of a previous study revealed that the effect of dual-task training on dual-task performance was retained until the 12-week follow-up among the participants who received dual-task training with variable priority instructions. However, the effect of single task-training on individual-task performance was maintained till the 12-week follow-up among the participants of both groups who received dual-task training with fixed and variable priority instructions, respectively.23
Our result points towards the role and importance of the instructions/commands while performing balance control training under dual-task settings. Similarly, one study reported that the participants of dual-task training with variable priority instructions had benefited more over the participants of dual-task training with fixed priority instructions and found their participants learned to coordinate among two tasks as well.22 Although after completion of their training sessions, the processing demand needs less to perform the task when participants were subjected to shift their attention between two tasks as recommended in dual-task training with variable priority instructions sets. This could be why the training effect enabled one group of participants who received variablepriority instructions to learn the task faster than the other group of participants who received fixedpriority instructions at 2 weeks of training and retain the effects of training for a longer duration of 3 months.22
Previously, many studies have reported the beneficial effects of dual-task training over single-task training on balance in older adults and highlighted the significance of balance-related instructional sets on learning.27 According to the task-integration hypothesis, practicing two tasks together allows participants to develop task co-ordination skills.23 Dual-task training has been used as it suggests that the sensory-motor processing essential for motor control requires attention resources.27
Schwenk et al studied the effect of a specific dual-task training in geriatric patients with mild-to-moderate dementia and revealed that it is effective in increasing dual-task performance while walking.36 Verghese et al conducted a study to examine the effect of cognitive remediation on gait in sedentary seniors and suggested that cognition remediation improves mobility in older adults.37 McCulloch et al concluded that patients with Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis have difficulty in performing dual tasks.34 Furthermore, few researchers supported the efficacious effect of dual-task training on non-balance concerning tasks and comparative importance of instructional sets on learning ability.38
In our study, balance control was affected in diverse ways when the participants underwent different instructional sets under dual-task training. We even demonstrated an improvement in functional balance tasks with variable priority instructions following 4 weeks of dual-task training. Increased in the ability to allocate attention (e.g. dual-task processing skills) that resulted in the improvement of dual-task performance for a new and untrained stimuli, this skill can be recognized to other dualtasks those are indirectly trained. Therefore, definite instructions towards attention focus should be integrated when the therapists determine to train balance under dual-task conditions.23
As per the task-coordination and management hypothesis, it is very crucial to coordinate and manage multiple tasks during a dual-task performance, especially in older adults as this ability reduces with age. These factors/outcomes of aging recommend that dual-task training with instructional sets for balance control should be considered for patients with chronic stroke. Variablepriority instructional sets had an efficacious effect even on a novel (untrained) dual task.
The results of this study revealed that the improvement achieved in the balance component was greater in group 2 who received dual-task training with variable priority instructional set than in group 1 who received dual-task training with fixed priority instructional set in patients with chronic stroke, which is consistent with other studies.23,35,38
This study examined the feasibility of our training approaches and to validate that patients with chronic stroke could, in fact, adhere to instructional sets. It will also help in giving some concrete information about the effectiveness of instructional sets either with variable or fixed priority in improving the gait parameters of the patients with chronic stroke. Since the study fulfilled the demand of required sample size (n>28) to be effective, the results of this study might be useful to generalize among the physiotherapists while considering the treatment of balance impairment in patients with chronic stroke and community-dwelling older adults except significant neurological and musculoskeletal condition exhibiting cognitive decline.
Our study had few limitations despite its strength. The study had a short duration of intervention and did not assess the training affect at follow up; increasing the training duration and assessing the training effect at follow up might bring more improvement in the outcome measure and establish the long-term effect of the training interventions. Further, our study was not double-blinded that might affect the results of the study. In addition, we used a rhythmic auditory tone task during the training session in our study that influences the preferable walking speed in people, as certainly in patients with Parkinson’s disease. However, we didn’t assess separately its influence on the comfortable preferred walking speed of the participants in our study.
Conclusion
This study hypothesized that dual-task training with variable priority instructional sets may be more effective than that with fixed priority instructional in improving gait parameters in patients with chronic stroke. The hypothesis was validated, and it was observed that dual-task training with variable priority instructional sets is more effective in improving gait parameters such as gait speed, stride length, and step length in patients with chronic stroke.
Relevance To Clinical Practice
The instructional sets (variable/fixed priority) were a crucial contributing factor to the improvement in dual-task performance. The variable priority instructional set presented benefits over the fixed priority instructional set in terms of learning rate and longer retention time for the skills obtained during training.
Physiotherapists should spread awareness and also add this specific set of exercise (variable priority instructional set) into their treatment’s interventions while treating the patients with chronic stroke.
Further research is required to recognize the length of training benefits (follow-up) that are sustained among patients with chronic stroke due to ruptured MCA and what surplus approaches (home exercise program) are important to sustain and maximize the benefits of the training. Some other outcome measures could be added/used for balance control during gait cycle, such as the center of mass (COM), center of pressure (COP), and inclination angles (IA) in patients with chronic stroke (ruptured middle cerebral artery). Other gait variables, such as step width, cadence, and rate of response, could be evaluated. Since motor learning is long-term skills acquisition, more specific assessment tools such as retention test or transfer test are needed to understand the training effect (relatively permanent change) on motor learning performance in patients with chronic stroke. Furthermore, a more definite strengthening and proprioception-enhancement study protocol could be integrated with this training method. Additional research is needed to understand the effect on other orthopedic conditions.
Acknowledgment
The authors are grateful to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs.
Author contributions
All authors substantially contributed towards conception and design, analysis and interpretation of data, drafting and critically revising the paper, gave final approval of the version to be published and agreed to be accountable for all aspect of the work.
Data sharing statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Umphred DA. Foundations for clinical practice in neurological rehabilitation. Neurol Rehabil. 2013;1.
2. Błażkiewicz M. Muscle force distribution during forward and backward locomotion. Acta Bioeng Biomech. 2013;15(3):3–9.
3. Gaerlan MG. The Role of Visual, Vestibular, and Somatosensory Systems in Postural Balance. 2010. UNLV Theses, Dissertations, Professional Papers, and Capstones. 357. Available from: https://digitalscholarship.unlv.edu/thesesdissertations/357.
4. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(suppl_2):ii7–ii11. doi:10.1093/ageing/afl077
5. Assländer L, Hettich G, Mergner T. Visual contribution to human standing balance during support surface tilts. Hum Mov Sci. 2015;41:147–164. doi:10.1016/j.humov.2015.02.010
6. Magnusson M. Posture, balance control, movement: involvement in vestibular rehabilitation. Neurophysiol Clin. 2016;46(4–5):238. doi:10.1016/j.neucli.2016.09.006
7. Jeon S-H, Lee S-M, Kim J-H. Therapeutic effects of reaching with forward bending of trunk on postural stability, dynamic balance, and gait in individuals with chronic hemiparetic stroke. J Phys Ther Sci. 2015;27(8):2447–2451. doi:10.1589/jpts.27.2447
8. Abuin-Porras V, Villafañe JH, Jiménez-Antona C, Palacios A, Martínez-Pascual B, Rodríguez-Costa I. Relationship between attention and balance: a dual-task condition study in children. J Exerc Rehabil. 2018;14(3):349. doi:10.12965/jer.1836142.071
9. Abrahamova D, Hlavacka F. Age-related changes of human balance during quiet stance. Physiol Res. 2008;57(6):957.
10. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehab. 2001;82(8):1050–1056. doi:10.1053/apmr.2001.24893
11. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/j.maturitas.2013.02.009
12. Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360(23):2390–2393. doi:10.1056/NEJMp0900963
13. Tinetti ME, Kumar C. The patient who falls:“it’s always a trade-off”. Jama. 2010;303(3):258–266. doi:10.1001/jama.2009.2024
14. Del Porto H, Pechak C, Smith D, Reed-Jones R. Biomechanical effects of obesity on balance. Int J Exerc Sci. 2012;5(4):1.
15. Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. Gerontologist. 2006;46(3):367–376. doi:10.1093/geront/46.3.367
16. Harris JE, Eng JJ, Marigold DS, Tokuno CD, Louis CL. Relationship of balance and mobility to fall incidence in people with chronic stroke. Phys Ther. 2005;85(2):150–158.
17. Teasell RW, Bhogal SK, Foley NC, Speechley MR. Gait retraining post stroke. Top Stroke Rehabil. 2003;10(2):34–65. doi:10.1310/UDXE-MJFF-53V2-EAP0
18. Van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, Van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil. 2004;18(8):833–862. doi:10.1191/0269215504cr843oa
19. Eng JJ. Strength training in individuals with stroke. Physiother Can. 2004;56(4):189. doi:10.2310/6640.2004.00025
20. Sihvonen S. Postural Balance and Aging: Cross-sectional Comparative Studies and a Balance Training Intervention. Jyväskylä University Printing House, University of Jyväskylä; 2004.
21. Li KZ, Roudaia E, Lussier M, Bherer L, Leroux A, McKinley P. Benefits of cognitive dual-task training on balance performance in healthy older adults. J Gerontol Series A. 2010;65(12):1344–1352. doi:10.1093/gerona/glq151
22. Silsupadol P, Shumway-Cook A, Lugade V, et al. Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Arch Phys Med Rehab. 2009;90(3):381–387. doi:10.1016/j.apmr.2008.09.559
23. Silsupadol P, Siu K-C, Shumway-Cook A, Woollacott MH. Training of balance under single-and dual-task conditions in older adults with balance impairment. Phys Ther. 2006;86(2):269–281.
24. An H-J, Kim J-I, Kim Y-R, et al. The effect of various dual task training methods with gait on the balance and gait of patients with chronic stroke. J Phys Ther Sci. 2014;26(8):1287–1291. doi:10.1589/jpts.26.1287
25. Plummer-D’Amato P, Kyvelidou A, Sternad D, Najafi B, Villalobos RM, Zurakowski D. Training dual-task walking in community-dwelling adults within 1 year of stroke: a protocol for a single-blind randomized controlled trial. BMC Neurol. 2012;12(1):129. doi:10.1186/1471-2377-12-129
26. Chen C-L, Chen H-C, Wong M-K, Tang F-T, Chen R-S. Temporal stride and force analysis of cane-assisted gait in people with hemiplegic stroke. Arch Phys Med Rehab. 2001;82(1):43–48. doi:10.1053/apmr.2001.18060
27. Buragadda S, Alyaemni A, Melam GR, Alghamdi MA. Effect of dualtask training (fixed priority-versus-variable priority) for improving balance in older adults. World Appl Sci J. 2012;20(6):884–888.
28. Silsupadol P, Lugade V, Shumway-Cook A, et al. Training-related changes in dual-task walking performance of elderly persons with balance impairment: a double-blind, randomized controlled trial. Gait Posture. 2009;29(4):634–639. doi:10.1016/j.gaitpost.2009.01.006
29. Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired: reliability and meaningfulness. Phys Ther. 1984;64(1):35–40. doi:10.1093/ptj/64.1.35
30. Fulk GD, Echternach JL. Test-retest reliability and minimal detectable change of gait speed in individuals undergoing rehabilitation after stroke. J Neurol Phys Ther. 2008;32(1):8–13. doi:10.1097/NPT0b013e31816593c0
31. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198.
32. Wolf SL, Catlin PA, Gage K, Gurucharri K, Robertson R, Stephen K. Establishing the reliability and validity of measurements of walking time using the Emory Functional Ambulation Profile. Phys Ther. 1999;79(12):1122–1133.
33. Ng SS, Hui-Chan CW. The timed up & go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch Phys Med Rehab. 2005;86(8):1641–1647. doi:10.1016/j.apmr.2005.01.011
34. McCulloch K. Attention and dual-task conditions: physical therapy implications for individuals with acquired brain injury. J Neurol Phys Ther. 2007;31(3):104–118. doi:10.1097/NPT.0b013e31814a6493
35. Her J-G, Park K-D, Yang Y, et al. Effects of balance training with various dual-task conditions on stroke patients. J Phys Ther Sci. 2011;23(5):713–717. doi:10.1589/jpts.23.713
36. Schwenk M, Zieschang T, Oster P, Hauer K. Dual-task performances can be improved in patients with dementia A randomized controlled trial. Neurology. 2010;74(24):1961–1968. doi:10.1212/WNL.0b013e3181e39696
37. Verghese J, Mahoney J, Ambrose AF, Wang C, Holtzer R. Effect of cognitive remediation on gait in sedentary seniors. J Gerontol Series A. 2010;65(12):1338–1343. doi:10.1093/gerona/glq127
38. Choi JH, Kim BR, Han EY, Kim SM. The effect of dual-task training on balance and cognition in patients with subacute post-stroke. Ann Rehabil Med. 2015;39(1):81–90. doi:10.5535/arm.2015.39.1.81
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
