Back to Journals » OncoTargets and Therapy » Volume 9
Efficacy and safety of ultrasound-guided continuous hyperthermic intraperitoneal perfusion chemotherapy for the treatment of malignant ascites: a midterm study of 36 patients
Authors Wu Y, Pan M, Cui S, Ba M, Chen Z, Ruan Q
Received 27 March 2015
Accepted for publication 28 May 2015
Published 20 January 2016 Volume 2016:9 Pages 403—407
DOI https://doi.org/10.2147/OTT.S85564
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jianmin Xu
Yinbing Wu,1,2 Mingxin Pan,1 Shuzhong Cui,2 Mingchen Ba,2 Zulong Chen,2 Qiang Ruan2
1Second Department of Hepatobiliary Surgery, Zhujiang Hospital, Southern Medical University, 2Treatment Center of Body Cavitary Thermo-Perfusion, Cancer Hospital of Guangzhou Medical University, Guangzhou Medical University, Guangzhou, People’s Republic of China
Background: This study aimed to evaluate the efficacy and safety of ultrasound-guided continuous hyperthermic intraperitoneal perfusion chemotherapy (CHIPC) for the treatment of malignant ascites (MA).
Methods: Between July 2011 and June 2013, 36 MA patients were prospectively and consecutively hospitalized for three cycles of elective CHIPC under ultrasound guidance, maintained at a constant flow rate of 400–600 mL/min normal saline containing 5-fluorouracil plus mitomycin or carboplatin and at a constant temperature of 43°C±0.2°C, for 90 minutes. Main outcome measures were ascites resolution, Karnofsky performance status (KPS), and serum tumor biomarkers at 2 weeks after the last cycle of CHIPC. All the patients underwent uneventful CHIPC as scheduled, and vital signs remained stable over CHIPC.
Results: At 2 weeks after the last cycle of CHIPC, MA completely and partially resolved in 26 (72.2%) patients and eight (22.2%) patients, respectively; mean KPS score increased from pretreatment 61±9 to posttreatment 76±9 (P<0.001), and serum carcinoembryonic antigen and carbohydrate antigens 12-5 and 19-9 significantly decreased (all P<0.01).
Conclusion: The current study indicated that ultrasound-guided CHIPC is an effective and safe palliative treatment modality for MA with respect to MA resolution, patient’s general well-being, and systemic disease control. The long-term benefit of CHIPC on overall survival remains to be investigated in MA patients.
Keywords: continuous hyperthermic intraperitoneal perfusion chemotherapy, malignant ascites, peritoneal carcinomatosis, ultrasound guidance, safety profile
Introduction
As a common complication of late-stage carcinomatosis, malignant ascites (MA) mainly results from metastasis, recurrence, or progression of intra- or extraperitoneal cancer, such as gastric, ovarian, and osteosarcoma.1 MA patients normally have an unfavorable survival and a compromised quality of life (QoL) due to complicating abdominal distension or pain, dyspnea, malnutrition, and sepsis.2 Surgical resection is thought to be unsuitable for these patients, while conventional palliative treatment modalities, such as conservative medical treatment, abdominocentesis, and systemic chemotherapy, show a minimal effect on the improvement of MA patients’ survival and QoL.3
Continuous hyperthermic intraperitoneal perfusion chemotherapy (CHIPC) is advantageous over hyperthermic intraperitoneal chemotherapy, which is also a newly emerging palliative treatment modality incorporating hyperthermia therapy and local chemotherapy for peritoneal carcinomatosis.4 CHIPC is normally performed using laparotomy or laparoscopy, at the risk of surgical morbidities, although the latter technique is believed to be less invasive.5,6 The previous study also indicates that there are less effects of CHIPC on the overall survival.5,6 In this study, we used ultrasound-guided abdominocentesis for catheter placement in CHIPC. The primary objective of the present work was to evaluate efficacy and safety of CHIPC with respect to body temperature change, ascites resolution, Karnofsky performance status (KPS), and serum tumor biomarkers.
Patients and methods
Patients
The study protocol was approved by the Institutional Review Board at the Cancer Hospital of Guangzhou Medical University in accordance with the latest version of the Declaration of Helsinki. Between July 2011 and June 2013, 36 MA patients were prospectively and consecutively screened for eligibility for elective CHIPC. The inclusion criteria were as follows: aged 18–75 years; diagnosed with MA confirmed on a combination of medical imaging examination, endoscopy, ascites cytology, and serum oncology; with an unresectable primary disease; with an ascites volume between 2,000 mL and 6,000 mL (the optimal range for the inclusive volume according to the preexperiments, data not shown); with a normal serum dihydropyrimidine dehydrogenase; and with a compensated cardiopulmonary or hepatorenal function reserve. The exclusion criteria were as follows: having received radical or palliative abdominal resection with 1-month time; with serious wasting or morbid obesity; with complicating serious cardiopulmonary or hepatorenal insufficiency or coagulopathy; expected to survive <4 weeks; or rejecting to participate in this study. All the above excluded criteria, such as wasting, morbid obesity, and serious comorbidity, were defined according to the diagnosis criteria of the Zhujiang Hospital, Southern Medical University, Zhujiang, People’s Republic of China. For the predicted survival definition, we have used a predictive model in the preliminary study (data not shown).
Before participating in this study, all the patients gave their informed consent and approved this study in writing.
Methods
All CHIPC procedures were performed by an assigned oncologic team led by the corresponding author, including resident oncologists, anesthesiologists, radiologists, clinical pathologists, oncological nurses, and research technicians. The patient was placed supine or semisupine, and conventional abdominal ultrasound scan was performed to locate the puncture sites in the left/right, upper/lower quadrants. Under general anesthesia with endotracheal intubation or epidural anesthesia, the abdominal skin was prepared, disinfected, and draped as routine before abdominocentesis, with the inflow catheters placed in the left and right upper quadrants and the outflow catheters in bilateral lower quadrants, respectively. The perfusion catheters were connected to a BR-TRG-I CHIPC system (Guangzhou Bright Medical Technology Co., Ltd, Guangzhou, People’s Republic of China) with a ±5% flow rate precision, ±0.15°C temperature control, and automatic cooling function, approved by China Food and Drug Administration (license number 2009-3260924), and also equipped with temperature sensors for continuous monitoring of perfusate and body temperature over CHIPC.7 The perfusion solution consisted of 3,500–6,000 mL normal saline and 1,500 mg 5-fluorouracil, and the perfusion was maintained at a constant temperature of 43°C±0.2°C and at a flow rate of 400–600 mL/min for 90 minutes. The first cycle of CHIPC was done in the operating room, while the next two cycles were given in the ward using the same protocol, after the patient was intramuscularly premedicated with 25 mg promethazine and 75 mg pethidine, at an interval of 1 week. In the last cycle of CHIPC, 80 mg carboplatin was added into the perfusate for malignant gastrointestinal stromal tumors (GISTs) and ovarian cancers, while 10 mg mitomycin was added for liver, gastric, colon, and pancreatic cancers. Intravenous systemic chemotherapy was initiated 6 weeks after CHIPC as indicated. Main outcome measures were ascites resolution, KPS, and serum carcinoembryonic antigen (CEA) as well as carbohydrate antigens 12-5 (CA12-5) and 19-9 (CA19-9) 2 weeks after the last cycle of CHIPC. Resolution of ascites was defined as follows: complete response, ≥75% resolution of ascites maintaining >4 weeks; partial response, 50%-75% resolution of ascites maintaining >4 weeks; and no response, <50% resolution or recurrence of ascites.8
Statistical analysis
The statistical software package SPSS 17.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. All continuous data were expressed as mean ± standard deviation, and the means were compared using the paired Student’s t-test. A two-tailed P<0.05 was considered to be statistically significant.
Results and discussion
Overall, 36 patients, including 16 men and 20 women, at a median age of 49 years (35–73 years) and with a KPS score of 40-70 were studied. The disease history was 7 days to 5 months (mean, 1.1 months) to the time of diagnosis. The underlying primary disease was gastric cancer (n=12), ovarian cancer (n=12), colon cancer (n=8), pancreatic cancer (n=2), postoperative hepatocellular carcinoma (n=1), and postoperative malignant GIST (n=1).
All the patients underwent uneventful CHIPC as scheduled and vital signs remained stable over CHIPC (Table 1; all P>0.05). Ascites completely resolved in 26 (72.2%) patients, partially resolved in eight (22.2%) patients, and with no significant response in two (5.6%) patients. Mean KPS score increased from pretreatment 61±9 to posttreatment 76±9 (P<0.001), and serum CEA and CA 12-5 and 19-9 significantly decreased (all P<0.01; Table 2).
During the follow-up at the outpatient clinic visits, the patients complained of no clinically significant adverse events, except for mild abdominal distension or discomfort and transient fever. Follow-up liver and renal function tests showed no clinically significant abnormalities. Grades I and II bone marrow suppression occurred in four (11.1%) patients, and mild gastrointestinal reaction in six (16.7%) patients, all of which resolved after symptomatic treatment. No peritoneal sepsis, bowel adhesion, intestinal obstruction, or puncture site metastasis occurred. All patients were followed-up as scheduled for 2–12 months (median, 7 months), and the survival curve is depicted in Figure 1.
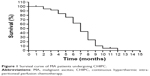  | Figure 1 Survival curve of MA patients undergoing CHIPC. |
MA patients usually exhibit a dismal survival ranging from weeks to months, at 1-year overall survival below 10%.1 Effective elimination or control of ascites may be beneficial for MA patients with respect to improvement of overall survival and QoL.1 CHIPC is a palliative treatment modality that has been well documented for peritoneal carcinomatosis manifesting as refractor or recurrent ascites. Tumor cells are normally sensitive to hyperthermia, which significantly increases cell membrane permeability to drugs. Large-volume hyperthermic perfusate allows adequate exposure of free tumor cells and tumor micrometastases to chemotherapeutic agents in a constant and continuous manner. Moreover, CHIPC is associated with relatively less toxicities as it results from the entry of a significantly lower dose chemotherapeutic agent into the blood stream as compared to systemic chemotherapy. Thus, CHIPC is reported to be advantageous over systemic or intraperitoneal chemotherapy for the treatment of peritoneal carcinomatosis including MA.4–8
In previous reports,4–12 CHIPC was usually performed using laparotomy or laparoscopy, which allowed a direct visualization of intraperitoneal disease and placement of perfusion catheters. However, laparotomy- or laparoscopy-assisted CHIPC may result in some surgical morbidities and require delicate postoperative care. In contrast, ultrasound-guided percutaneous access is a minimally invasive interventional imaging modality for diagnosis, follow-up, and treatment of MA, with a good accuracy, reproducibility, and cost-effectiveness.13,14 Our results showed that ultrasound-guided CHIPC had a good efficacy and safety profile. CHIPC effectively resolved ascites and improved patients’ general well-being in association with the control of systemic disease within a short time as shown by follow-up examination.
Treatment-emergent hyperthermia is a major safety concern over CHIPC,15 aside from puncture- and chemotherapy-associated morbidities, as the parietal and visceral peritonea can efficiently absorb the heat. Increased body temperature may have an adverse impact on the patient’s circulatory, respiratory, neurologic, and metabolic functions. Our results demonstrated that peritoneal perfusion at a constant temperature (43°C±0.2°C) and flow rate (400-600 mL/min) resulted in a clinically insignificant increase in body temperature without significantly altering the patient’s physiologic condition.
There were some limitations in this study. First, the sample size was relatively small; however, to the best of our knowledge, the present work was the largest study evaluating efficacy and safety of ultrasound-guided CHIPC for the treatment of MA. Second, the effect of peritoneal hyperthermia on the patient’s general well-being and tolerability was not fully studied, although the increase of body temperature was <1°C in extent and transient in duration. Finally, the benefit of ultrasound-guided CHIPC remained undetermined in this study with respect to overall survival, while the long-term follow-up study is ongoing in our institute.
Conclusion
In conclusion, CHIPC is an effective and safe palliative treatment modality for MA with respect to resolution of ascites, improvement of patient’s general well-being, and control of intraperitoneal disease. Hyperthermia is a major CHIPC-emergent adverse event, while it has insignificant effects on the patient’s cardiopulmonary status due to its mild severity and transient duration. The benefit of CHIPC for overall survival of MA patients, who normally have a dismal prognosis, remains yet to be investigated in further long-term follow-up studies.
Acknowledgments
This work was supported by the grants from Guangdong Province and Hong Kong SAR Breakthrough Funds in Key Areas of Science and Technology (number 2006Z1-E6041) and Guangdong Provincial Science and Technology Program (number 2009A030301013), People’s Republic of China.
Disclosure
The authors report no conflicts of interest in this work.
References
Fushida S, Oyama K, Kinoshita J, et al. VEGF is a target molecule for peritoneal metastasis and malignant ascites in gastric cancer: prognostic significance of VEGF in ascites and efficacy of anti-VEGF monoclonal antibody. Onco Targets Ther. 2013;6:1445–1451. | ||
Tsubamoto H, Takeuchi S, Ito K, et al. Feasibility and efficacy of intraperitoneal docetaxel administration as salvage chemotherapy for malignant gynaecological ascites. J Obstet Gynaecol. 2014;35:69–73. | ||
Akagi T, Inomata M, Etoh T, Yasuda K, Shiraishi N, Kitano S. Laparoscopic versus conventional palliative resection for incurable, symptomatic stage IV colorectal cancer: impact on short-term results. Surg Laparosc Endosc Percutan Tech. 2011;21:184–187. | ||
Al-Shammaa HA, Li Y, Yonemura Y. Current status and future strategies of cytoreductive surgery plus intraperitoneal hyperthermic chemotherapy for peritoneal carcinomatosis. World J Gastroenterol. 2008;14:1159–1166. | ||
Esquivel J, Averbach A, Chua TC. Laparoscopic cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in patients with limited peritoneal surface malignancies: feasibility, morbidity and outcome in an early experience. Ann Surg. 2011;253:764–768. | ||
Passot G, Bakrin N, Isaac S, et al. Postoperative outcomes of laparoscopic vs open cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy for treatment of peritoneal surface malignancies. Eur J Surg Oncol. 2014;40:957–962. | ||
Ba M, Long H, Zhang X, et al. Different sequential approaches of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in treating ovarian cancer with malignant ascites. J Cancer Res Clin Oncol. 2004;140:1497–1506. | ||
Ba MC, Cui SZ, Lin SQ, et al. Chemotherapy with laparoscope-assisted continuous circulatory hyperthermic intraperitoneal perfusion for malignant ascites. World J Gastroenterol. 2010;16:1901–1907. | ||
Graziosi L, Mingrone E, Marino E, Cavazzoni E, Donini A. Analysis of operative morbidity in a single center initial experience with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Tumori. 2014;100:15–20. | ||
Votanopoulos KI, Swords DS, Swett KR, et al. Obesity and peritoneal surface disease: outcomes after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for appendiceal and colon primary tumors. Ann Surg Oncol. 2013;20:3899–3904. | ||
Macrì A, Arcoraci V, Belgrano V, Caldana M. Short-term outcome of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: preliminary analysis of a multicentre study. Anticancer Res. 2014;34:5689–5693. | ||
Huang CQ, Yang XJ, Yu Y. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy improves survival for patients with peritoneal carcinomatosis from colorectal cancer: a phase II study from a Chinese center. PLoS One. 2014;9:e108509. | ||
Cui S, Ba M, Tang Y, et al. B ultrasound-guided hyperthermic intraperitoneal perfusion chemotherapy for the treatment of malignant ascites. Oncol Rep. 2012;28:1325–1331. | ||
Ba MC, Long H, Cui SZ, et al. Multivariate comparison of B-ultrasound guided and laparoscopic continuous circulatory hyperthermic intraperitoneal perfusion chemotherapy for malignant ascites. Surg Endosc. 2013;27:2735–2743. | ||
Yang XJ, Li Y, Yonemura Y. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy to treat gastric cancer with ascites and/or peritoneal carcinomatosis: results from a Chinese center. J Surg Oncol. 2010;101:457–464. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


