Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Efficacy and Safety of Resilient Hyaluronic Acid Fillers Injected with a Cannula: A Randomized, Evaluator-Blinded, Split-Face Controlled Study
Authors Beer K, Biesman B, Cox SE, Smith S , Picault L, Trevidic P
Received 23 December 2022
Accepted for publication 4 March 2023
Published 6 April 2023 Volume 2023:16 Pages 959—972
DOI https://doi.org/10.2147/CCID.S402315
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Anne-Claire Fougerousse
Kenneth Beer,1 Brian Biesman,2 Sue Ellen Cox,3 Stacy Smith,4 Laura Picault,5 Patrick Trevidic6
1Beer Dermatology, West Palm Beach, FL, USA; 2Private Practice, Nashville, TN, USA; 3Aesthetic Solutions, Chapel Hill, NC, USA; 4California Dermatology & Clinical Research Institute, Encinitas, CA, USA; 5Teoxane Clinical Development Department, Genève, Switzerland; 6Expert 2 Expert, Paris, France
Correspondence: Patrick Trevidic, Expert 2 Expert, 7 Rue de Sontay, Paris, 75116, France, Tel +33 145 016 415, Fax +33 145 008 981, Email [email protected]
Purpose: Cannulas are increasingly used for injecting hyaluronic acid fillers, as they are thought to improve patient comfort safety and treatment tolerability. This study aimed to demonstrate the non-inferiority of a Resilient Hyaluronic Acid 4 (RHA 4) filler injected with a cannula versus a needle for the treatment of moderate to severe nasolabial folds (NLF).
Patients and Methods: A total of 50 subjects were included in a randomized, evaluator-blinded, split-face trial. The NLF were injected with RHA 4 using a cannula on one side of the face and using a needle on the other side on Day 0. A touch-up could be performed 4 weeks later. The subjects were followed up for 12 weeks after the last injection, ie, injection on Day 0 or touch-up. Efficacy was evaluated using a Wrinkle Severity Rating Scale (WSRS), the Global Aesthetic Improvement Scale (GAIS), and patient-reported outcomes. Safety assessments included the injection-site pain, common treatment reactions (CTRs), and adverse events (AEs).
Results: Twelve weeks after the last injection, the efficacy of the cannula treatment was found to be non-inferior to that of the needle treatment, based on the WSRS score improvements. The other study endpoints showed the equivalent efficacy and safety of the two methods. No serious or unexpected AEs were reported.
Conclusion: RHA 4 may be effectively and safely injected into the NLF using a cannula or a needle, provided it is administrated by a trained practitioner.
Keywords: cosmetic techniques, hyaluronic acid, injections, nasolabial fold, treatment outcome
Corrigendum for this paper has been published.
Introduction
The emergence of nasolabial folds (NLF) is an early sign of aging and a frequent concern of patients desiring aesthetic procedures.1 Since the advent of dermal filling procedures, NLF have been widely treated along with an increasing number of other facial signs of aging.2,3
Although NLF injections are very common in clinical practice, the area presents anatomical specificities making the procedure technically complex.4–6 Briefly, the NLF represents the anatomical border between the cheek, with its generous layer of subcutaneous fat, and the lip, where the skin directly adheres to the orbicularis oris muscle with very little intervening fat.6 Musculodermal insertions of the lip elevator muscles underneath the NLF bring further complexity to the tissue layers’ arrangement.6–9
The NLF has been labelled one of the facial “danger zones”, on the grounds of its association with vascular complications.10,11 This may be partially explained by the disproportionately large number of procedures in this region in routine practice. However, the complex vascular network underneath the NLF clearly plays a role, particularly in the upper third of the fold. The facial artery (FA) runs subcutaneously in the whole NLF but is even more superficial in the upper third of the fold, and it can anastomose with branches of the infraorbital artery (IOA).12–14
In addition to an in-depth knowledge of the anatomy and the adoption of appropriate techniques,15 the use of cannula is seen by many practitioners as an additional safety precaution.15,16 A growing number of practitioners tend to favor the use of cannulas over needles for certain procedures, on the grounds that they enhance injection ease, patient comfort, and safety. While several controlled clinical studies provide support for this,17–20 other trials have only been able to demonstrate an equivalent safety profile for the cannula and needle treatments.21–23 It has been hypothesized that the use of round-tipped cannulas (particularly large diameters, ie, 25G or less) instead of sharp needles may minimize the risk of vascular injury and intravascular injection. Although the current evidence for this is somewhat contradictory,24,25 it is believed that the cannula’s rounded end is less likely to lacerate vessels than a sharp needle, and that cannulas with a larger diameter would require stronger injection forces to penetrate an arterial wall.26,27
In this study, we assessed the investigational device TEOSYAL RHA® 4 (RHA 4, Teoxane S.A., Geneva, Switzerland) which belongs to a range of four Resilient Hyaluronic Acid (RHA) fillers. These fillers are manufactured using Preserved Network Technology, which ensures minimal modification of the hyaluronic acid (HA) chains in the final gels (2–4%).28 There is mild HA crosslinking, which results in rheological properties that are particularly well adapted for treating areas with dynamic facial movements. RHA 4 provides a suitable balance between the filler strength, which provides support and volume to deep folds and depressed areas, and the capacity to stretch, which allows it to accompany facial movements during muscle contraction (eg, during smiling).29 Several randomized controlled trials (RCTs) have demonstrated the clinical efficacy and safety of RHA dermal fillers (RHA 2, RHA 3, and RHA 4) injected with a needle, for treating moderate to severe NLFs.30–33
The aim of this study was to provide clinical evidence for non-inferior efficacy and safety of RHA 4 when injected with a cannula for treating moderate to severe NLF, compared with injections performed with a needle.
Materials and Methods
Trial Design and Ethical Considerations
This study was a randomized, evaluator-blinded, within-subject, multicenter, prospective clinical trial.
The trial was conducted in accordance with the International Conference on Harmonization (ICH) Good Clinical Practice (GCP) guidelines, the Code of Federal Regulations, and the Declaration of Helsinki. The study received approval from an institutional review board and was registered on ClinicalTrials.gov (NCT04754646). Informed consent was obtained from all subjects prior to the study procedures.
Each site obtained written approval from Veritas IRB, a US DHHS registered Independent Ethics Committee (#IRB00003814, #IRB00005916, #IRB00005917), which acted as the Central IRB for this study.
Study Population
The target population was adults aged 22 years or older, with bilateral NLF of moderate or severe intensity based on the Wrinkle Severity Rating Scale (WSRS),34 and identical NLF WSRS grades on both sides (inclusion criteria). The subjects who agreed to participate were injected with RHA 4 into the NLF at the baseline visit (Day 0). On one side of the face, the injection was performed using a 25G x 2-inch cannula; on the other side, a 27G x ½-inch needle was used. The side injected first and the injecting device (needle or cannula) were randomized.
Study Product, Study Product Administration, and Subject Follow-Up
TEOSYAL RHA® 4 (RHA 4, Teoxane S.A., Geneva, Switzerland) is an FDA-approved device. RHA 4 is a dermal filler composed of 23 mg/mL, high molecular-weight, 1,4-butanediol diglycidyl ether (BDDE)-crosslinked HA, and 0.3% lidocaine hydrochloride, in a physiological phosphate buffer (pH 7.3). It is used to fill deep wrinkles and folds in thick skin, such as moderate to severe NLFs. The participants were injected with RHA 4 bilaterally on Day 0, and there was an optional touch-up at Week 4, which was administered according to the subject’s initial treatment assignment (ie, the side of the needle/cannula injections remained the same). The subjects were followed for 12 weeks after the last injection (ie, initial or touch-up injection). By convention, the follow-up visit will be referred to as Week 12 from this point.
Supplemental pre-injection and post-injection pain control was prohibited to avoid interference with assessments of pain at the injection site, which were recorded up to 60 minutes after the injection.
Injection Technique and Evaluation of Ease of Injection
The choice of the injection technique (ie, retrograde or anterograde linear threading, cross-hatching, fanning, multiple puncture) was left to the discretion of the treating investigator (TI). The product was injected into the deep dermis/superficial subcutaneous tissue. Extreme caution was taken when injecting the upper part of the NLF, staying superficial enough to avoid the FA territory. The injections were performed slowly and at low pressure, irrespective of the treated side and chosen technique. Gentle massage of the injection site using the fingers was permitted to help smooth the product into place. The TIs were asked to evaluate the ease of injection for each side using a 5-point scale ranging from “1 – very difficult” to “5 – very easy”.
Study Endpoints and Variables
The primary efficacy endpoint was the change in the NLF WSRS scores, as assessed by a Blinded Live Evaluator (BLE) at Week 12, using Teoxane’s photo-validated scale. This scale has previously been shown to yield scores that are repeatable and reproducible (weighted kappa scores for intrarater and interrater agreement all >0.6; unpublished validation data).
The secondary efficacy endpoints were the NLF WSRS scores given by the TI, and the Global Aesthetic Improvement Scale (GAIS) scores given by the TI and BLE. In addition, the subjects completed the NLF domain of FACE-Q, a validated patient-reported outcome measure,35–37 and they assessed their own improvement using the GAIS and rated their satisfaction regarding the treatment.
Pain at the injection-site was assessed by the subjects for each side of the face immediately after the treatment, and at 5-, 30-, and 60-minutes post-injection on a 100-mm visual analog scale (VAS). Following each treatment visit (Day 0 or optional touch-up injection at Week 4), the subjects recorded the nature, severity, and duration of any local injection site reactions in a common treatment reactions (CTRs) diary. This was continued for a total of 28 days. Any CTR that persisted until day 28 was automatically considered to be an adverse event (AE). A periodic safety evaluation was carried out, which included review of the CTR and AE as well as on-site assessments of the subjects’ vision (Snellen visual acuity, confrontational visual field test, ocular motility) at Day 0 (pre- and post-injection), Week 4 (pre- and post-touch-up injection), and the subsequent follow-up visits.
Statistical Analysis
The primary objective of the study was to demonstrate the statistical non-inferiority of RHA 4 injected with a cannula versus RHA 4 injected with a needle to treat NLFs. This was evaluated by the change in NLF WSRS scores given by the BLE at Week 12.
The non-inferiority margin was set at 0.5 (a 1-point difference on the scale being considered clinically significant). Therefore, expressing the difference between treated sides as the mean of change from baseline in RHA 4 injected with needle minus change from baseline in RHA 4 injected with cannula, a one-sided 97.5% confidence limit of <0.5 was required to conclude non-inferiority.
The confidence intervals (CIs) were calculated using a one-sided paired t-test; if the normality assumption was not met, as determined by a Shapiro–Wilk test, a normalizing data transformation was applied, and the CIs were calculated and then back-transformed prior to the non-inferiority assessment.
The statistical tests for the secondary endpoints were all performed at the same significance level (α) of 0.05. The categorical and continuous variables were analyzed using two-sided parametric or non-parametric tests for paired data, as appropriate.
The percentage of subjects who responded to the treatment at each visit was determined from the number achieving a 1-grade improvement or more on the NLF WSRS compared to baseline.
The per-protocol (PP), intention-to-treat (ITT), and safety (SAFT) populations were defined for the statistical analyses. The PP population consisted of subjects who had completed 12 weeks of treatment follow-up without any major protocol deviation. The ITT population included all subjects who had received at least one treatment with the RHA 4 filler in compliance with their treatment protocol allocation. The evaluation of the primary endpoint was performed using the PP population, while the secondary efficacy endpoints were all evaluated using the ITT population. Safety analyses were performed using the SAFT population, which included all subjects who had received at least one treatment with the RHA 4 filler.
Results
Study Population
A total of 50 subjects with bilateral NLF of moderate or severe intensity (WSRS) were enrolled at four study sites in the United States. These subjects made up the ITT and SAFT populations. Four of these subjects were excluded from the PP population either due to a randomization error at the touch-up visit (Week 4, N = 1) or because the last visit (Week 12) took place outside of the permitted time window (N = 3).
The mean age of the ITT population was 55.8 years (standard deviation, SD: 8.2; range: 42–77). The subjects were primarily female (98.0%) and White (78.0%). All six Fitzpatrick Skin Types (FST) were represented; 12 (24.0%) subjects had FST IV to VI (Table 1).
 |
Table 1 Subject Demographics |
Injection Volume and Technique
On Day 0, the mean total (bilateral) injection volume of RHA 4 was 2.77 mL (SD: 0.87), with no statistically significant difference between the treated sides (p = 0.1792). Twenty subjects (40.0%) received a touch-up treatment (at Week 4) on their cannula-treated side and 17 subjects (34.0%) received a touch-up treatment on their needle-treated side. The mean total touch-up volume of RHA was 1.31 mL (SD: 0.73), with no statistically significant difference between the treated sides (p = 0.9427). The overall unilateral injection volume (initial + touch-up) did not differ significantly between the treated sides (p = 0.2669), with 1.71 mL (SD: 0.64) for the cannula-treated side and 1.67 mL (SD: 0.63) for the needle-treated side (Table 2).
 |
Table 2 Injection Volumes |
The TIs used and combined various injection techniques. Linear threading “alone” was the most frequent method for the initial injections, being performed for 26 (52.0%) of the cannula and 13 (26.0%) of the needle treatments. The remaining cannula injections were performed using the fan-like technique “alone” or combined with linear threading, while the remaining needle treatments were performed with the fan-like technique, crosshatching, and/or multiple puncture techniques, which were sometimes combined with linear threading. The TIs rated the injections as “easy” or “very easy” in 98.0% of the NLFs, regardless of the injection method (p = 0.2101). However, there were slightly more “very easy” versus “easy” answers for the cannula-treated side (Figure 1).
 |
Figure 1 Ease of injection of RHA 4 into the nasolabial fold with a cannula or a needle, according to the treating investigator. |
Primary Efficacy Endpoint
In the PP population, the RHA 4 injected with a cannula was shown to be statistically non-inferior to the RHA 4 injected with a needle for treating moderate to severe NLF, based on the WSRS scores given by the BLE at Week 12. Compared to baseline, the mean change [95% CI] in NLF severity was −1.61 [−1.82, −1.40] on the cannula-treated side, and −1.65 [−1.86, −1.44] on the needle-treated side, giving a difference of 0.04 (<0.5, the non-inferiority margin).
Secondary Efficacy Endpoints
NLF WSRS Scores and Percentage of Responders (BLE and TI Assessments)
The TIs evaluated each subject’s NLF at all study visits using the WSRS. The scores were found to improve from a mean bilateral NLF severity of 3.3 (SD: 0.5) on Day 0, to 2.1 (SD: 0.7) on the cannula-treated side and 2.0 (SD: 0.7) on the needle-treated side at Week 4 (change from baseline, p = 0.4240) (Figure 2). The mean WSRS scores remained stable on both treated sides up to Week 12, with mean scores at Week 12 of 1.8 (SD: 0.7) and 1.7 (SD: 0.7) for the cannula- and needle-treated sides, respectively (change from baseline, p = 0.3367). No statistically significant difference between treatment groups was noted at any time point (p > 0.1797). The mean differences between the scores at baseline and Week 12 were similar for the two different evaluators (TI; p = 0.3367 and BLE; p = 0.2500), with change from baseline values of −1.5 (SD: 0.6) and −1.6 (SD: 0.7) for the cannula-treated side as assessed by the TI and BLE, respectively. For the needle-treated side, change from the baseline values are −1.6 (SD: 0.7) and −1.6 (SD: 0.7) for the TI and BLE, respectively.
 |
Figure 2 Mean (SD) scores on the 5-point Wrinkle Severity Rating Scale for the nasolabial folds, according to the treating investigator at each visit. |
The percentage of subjects who responded to the treatment was identical for the two treated sides at Week 12 according to the BLE (94.0%) and the TI (98.0%), there was a slight increase between Week 4 and Week 12, possibly due to the optional touch-up injection (Figure 3). No significant difference between treatment groups was noted at any time point (p > 0.5637).
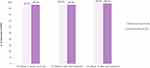 |
Figure 3 Percentage of subjects who responded to the treatment at each visit, based on changes on the Wrinkle Severity Rating Scale as assessed by the treating investigator. |
GAIS (BLE, TI, and Subject Assessments)
At Week 12, all subjects (100.0%) were “improved” (Grade 2) or “much improved” (Grade 1) compared with the baseline, according to the BLE using the GAIS. According to the TIs or the subjects themselves, at least 90.0% of the subjects were “improved” or “much improved”. It was found that the TIs and subjects gave very low grades on the GAIS throughout the study, with no significant difference between the treated sides throughout the follow-up period (p > 0.1250 for all comparisons; Figure 4).
 |
Figure 4 Percentage of subjects rated “improved” or “much improved” on the Global Aesthetic Improvement Scale at each visit by the treating investigator (A) and the subjects (B). |
Subject Satisfaction
The proportion of subjects who were “satisfied” or “very satisfied” with the treatment was high (>90.0%), and this was similar for the two treated sides (p > 0.1875) throughout the study follow-up (Figure 5). At the last study visit, Week 12, only five subjects (10.0%) were not satisfied with their NLF, either on both sides (N = 2, 4.0%) or on one side only (cannula, N = 3, 6.0%).
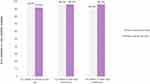 |
Figure 5 Percentage of subjects “satisfied” or “very satisfied” with the study treatment at each visit. |
FACE-Q (Subject-Rated)
The NLF FACE-Q scores on Day 0 (before injection) were similar for the two sides. Equal improvements were seen after the study treatment, with mean scores increasing between Day 0 and Week 12 by 40.7 (SD: 25.61) and 42.3 (SD: 27.93) points for the cannula-treated and needle-treated sides, respectively (p = 0.5625, Figure 6).
 |
Figure 6 Mean (SD) scores on the nasolabial fold domain of FACE-Q at each visit. |
Safety Endpoints
Injection Site Pain
For the initial treatment (Day 0), the subjects rated their pain at the injection site using a 100 mm VAS. The mean rating was at 34.7 mm (SD: 25.9) for the cannula injections and at 41.3 mm (SD: 25.8) for the needle injections. The difference was statistically significant (p = 0.0256), but not clinically meaningful. Pain at the site of injection quickly disappeared after procedure for the two treated sides (Figure 7). Similar trends were noted for the optional touch-up treatment (data not shown). There was no significant difference between the two sides during the injections (p = 0.7451).
 |
Figure 7 Mean (SD) injection site pain during and after the treatment, as indicated on a 100 mm Visual Analogue Scale. |
Common Treatment Reactions
Almost all subjects experienced at least one CTR after the initial treatment, with 48 subjects (96.0%) reporting reactions on the cannula-treated side and 49 (98.0%) reporting reactions on the needle-treated side. The number of subjects who were affected by each separate symptom was consistently lower on the cannula side, reaching statistical significance for bruising (p = 0.0004), lumps and bumps (p = 0.0010), redness (p = 0.0050), itching (p = 0.0348), and pain (p = 0.0389). However, the CTR severity was identical for the two sides, with 95.4% and 94.6% of reactions deemed mild or moderate on the cannula and needle sides, respectively. Furthermore, the subjects did not consider the CTRs that persisted to the last diary day to be “severe.” The CTR duration was also similar for the two sides, with 77.1% and 78.0% of symptoms having resolved by Day 14 for the cannula and needle treatments, respectively. As shown in Table 3, firmness and lumps/bumps were the longest-lasting reactions, regardless of the treatment side.
 |
Table 3 Number and Duration of Common Treatment Reactions (CTRs) Based on the Subjects’ 28-Day Diaries That Started at the Initial Treatment |
Similar trends were noted for the CTRs reported after the optional touch-up injections (data not shown).
Adverse Events
From the time of informed consent until the last study visit, the TI recorded 106 treatment-related AEs (TRAEs), which were experienced by 31 (62.0%) subjects. Ninety-nine (93.4%) of the TRAEs were identified using the subjects’ CTR diaries. The frequency of TRAEs was similar for the cannula and needle treatments, as shown by CI overlapping. For the cannula injection, 23 (46.0%) subjects experienced 54 TRAEs, while for the needle injection, 29 (58.0%) subjects experienced 64 events (Table 4). Most of the TRAEs were related to the administration site and were mostly induration or mass at the injection-site. Headaches (nine events) were experienced by six subjects (12.0%). The eight TRAEs that persisted until the end of the study (affecting three subjects, 6.0%) were mild in intensity and resolved within 4 weeks following the end of the study (confirmed by the subjects). Three AEs of Special Interest (AESIs) were reported, which were all related to visual disturbances; these were of mild severity, and none related to the study treatment, as confirmed by the TI, study medical monitor, and/or ophthalmologist. There were no nodular complications or vascular compromise events. No serious, unexpected, or late-onset TRAEs were reported.
 |
Table 4 Treatment-Related Adverse Events (TRAEs) According to the Technique Used and Overall |
Discussion
This study was the first randomized, split-face controlled trial to compare the efficacy and safety of cannula versus needle injections of the dynamic filler RHA 4 into the NLF. With a medium-sized cohort including all FST, it complements clinical evidence previously obtained in 15-month and 18-month studies in supporting the safety and durability of RHA 4.31,32
Compared with other dermal fillers of the RHA range, RHA 4 has the highest degree of HA modification (4%) and is intended to be injected into the deepest plane (deep dermis to subcutis).
Our results showed that the efficacy of the RHA 4 NLF treatment was similar for the cannula- and needle-treated sides, based on the WSRS scores given by BLEs. Twelve weeks after the last RHA 4 injection, 94.0% of the subjects were found to have responded to the treatment, as determined by the NLF WSRS scores given by the BLEs. This result was identical for the two injection methods. The secondary efficacy endpoints included both clinician- and patient-reported outcomes, and they all revealed similar treatment benefits for the two injection methods.
The cannula-treated NLF had lower rates of CTRs at the injection site, particularly for bruising, lumps and bumps, redness, itching, and pain. However, this did not translate into significant differences in the rate of TRAEs between the two sides. As almost all the TRAEs were identified using the subject diaries, this implies that the high CTR rate on the needle-injected side relates to mild and transient reactions.
Several previous studies have reported similar findings to those obtained in our study for NLF and other signs of aging. Specifically, it has previously been found that round-tipped cannulas have a comparable efficacy and safety profile to needle injections, and that there is a slight improvement in the injection site pain and local reactions, which indicates that the tissue trauma is less extensive. In two previous split-face controlled studies for NLF treatments, patients were found to experience less pain, edema, redness, and bruising on the cannula-injected side compared with the needle-injected side, and the difference was most marked during the first days following the injection.17,19 In another clinical trial that evaluated cheek augmentation using a volumizing HA filler, several injection site reactions were also found to be less frequent on the cannula-treated side, namely pain, lumps and bumps, and bruising; however, the severity of the side effects was similar for the two treated sides.20 In contrast to these studies, a recent multicenter RCT investigated the treatment of infraorbital hollowing using HA and observed the opposite pattern, with higher rates of local reactions on the cannula-treated side.21
Importantly, no SAEs occurred after any of the injections in our study, and there were no events related to vascular occlusion. Although vascular compromise remains rare considering the number of dermal filling procedures performed each year, the consequences can be dramatic and – in the most serious cases –may lead to temporary or permanent blindness.10 The introduction of cannulas was believed to minimize the risk of intravascular injection, as the blunt tip is thought to push the arteries and veins aside as it passes through the tissue. This theory is partially supported by a recent retrospective study which interviewed 370 US dermatologists, taking note of the vascular occlusion events encountered in their routine practice. Statistical analyses revealed a significantly higher rate of occlusion events with needles than with cannulas (p < 0.001).38 However, other studies, including clinical case reports and cadaveric studies, indicate that the safety profile of cannulas should not be overestimated.39 For instance, two recent cadaveric studies showed that the force required for smaller Gauge cannulas (ie, 27G or thinner) to penetrate an arterial wall was similar for needles of a corresponding size. This indicates that higher Gauges should be used whenever possible.26,27 Furthermore, a recent review of 28 cases of blindness related to HA embolism and referred to the same clinic revealed that most of the patients had been injected with a cannula.24
Given that the evidence for the superior safety of cannulas is somewhat contradictory, practitioners should be encouraged to adopt safety precautions that go beyond the simple use of a cannula. This includes an in-depth knowledge of the anatomy, slow injection techniques, and awareness of the clinical signs that indicate vascular compromise (eg, skin blanching, mottled discoloration, and/or pain). It has also been noted that cannula techniques, like any other, require a learning curve. The rate of SAEs occurring during dermal filling procedures is markedly lower for physicians with several years of experience, regardless of needle or cannula use.38 For some practitioners, cannula injections may be seen as an “advanced” technique, yet the higher “ease of injection” scores obtained in the present study show that this technique is easier to use than a needle injection.
The limitations of this study include the fact that there was only one male participant (2.0%) and only three subjects (6.0%) with very dark skin (FST VI). This imbalance in the sex and skin types of the participants is a common pitfall in dermal filler trials, particularly those focusing on wrinkles and folds. This can be at least partially attributed to wrinkles appearing later in life in darker-skinned individuals and being of less concern to men, who tend to focus on other aspects of facial aging.40,41 Nevertheless, no significant differences in the safety outcomes were found between subjects with lighter (I–III) and darker (IV–VI) skin phototypes in this study. Also, the study population reflected the diversity of those who usually seek NLF treatment.
Altogether, the results of this study provide robust clinical evidence that RHA 4 performs equally well when injected into the NLF with a cannula or a needle, and that both procedures are safe and well tolerated.
Conclusion
This prospective, multicenter, blinded-evaluator, split-face controlled study of 50 subjects showed that RHA 4 was equally effective and safe for the correction of dynamic wrinkles and folds when injected with a needle and when injected with a cannula.
This study confirms and complements existing evidence of the efficacy and safety of RHA 4 for treating NLF and should reassure physicians that both cannula and needle injections can be used. Both approaches have been shown to provide equivalent treatment efficacy and are expected to be safe and well tolerated when administered by a trained practitioner with an in-depth knowledge of facial anatomy.
Data Sharing Statement
The data that support the findings of this study will be openly available under aggregated format in ClinicalTrials.gov at www.clinicaltrial.gov, reference number NCT04754646. The participants of this study did not give written consent for their individual data to be shared publicly; thus, due to the sensitive nature of the research, supporting individual participant data are not available. The authors confirm that the data supporting the findings of this study are available within the article, and that no additional information or documentation will be shared.
Ethics Approval and Informed Consent
This study was a randomized, evaluator-blinded, within-subject, multicenter, prospective clinical trial.
The trial was conducted in accordance with the International Conference on Harmonization (ICH) Good Clinical Practice (GCP) guidelines, the Code of Federal Regulations, and the Declaration of Helsinki. The study received approval from an institutional review board and was registered on ClinicalTrials.gov (NCT04754646). Informed consent was obtained from all subjects prior to the study procedures. Each site obtained written approval from Veritas IRB, a US DHHS registered Independent Ethics Committee (#IRB00003814, #IRB00005916, #IRB00005917), which acted as the Central IRB for this study.
Consent for Publication
All the authors agree to the publication of the manuscript.
Author Contributions
All the authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Materials and funding for this study were provided by Teoxane SA.
Disclosure
Drs. Beer, Biesman, Cox, and Smith were clinical investigators for this study and received research grants for their involvement. Mrs Picault and Dr. Trevidic have financial relationship with Teoxane SA (Geneva, Switzerland) as clinical project coordinator, chief scientific officer, respectively. Dr Brian Biesman reports grants, personal fees from Allergan, grants, personal fees from Cytrellis, grants, personal fees from ENDO, grants, personal fees from Galderma, grants, personal fees from L’Oreal, personal fees from Lumenis, grants from Merz, grants, personal fees from Pulse, grants, personal fees from Raziel, grants, personal fees from Revance, grants, personal fees from Revision, personal fees from Revelle, personal fees from RVL, grants, personal fees from Solta, grants from Soliton, grants from Teoxane, grants from ZO Skin, outside the submitted work. Dr Sue Ellen Cox reports research grant from Teoxane, during the conduct of the study; grants, personal fees from Allergan, grants, personal fees from Galderma, grants, personal fees from Croma/Hugel, outside the submitted work.
Dr Stacy Smith reports fair market value fees for service as medical monitor from Teoxane, during the conduct of the study; medical monitor fees from Evolus, grants from Sofregen, outside the submitted work. Dr Patrick Trevidic reports personal fees from Teoxane, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Treating Nasolabial Folds [press release]; 2015. Available from: aestheticsjournal.com.
2. Stefura T, Kacprzyk A, Dros J, et al. Tissue fillers for the nasolabial fold area: a systematic review and meta-analysis of randomized clinical trials. Aesthetic Plast Surg. 2021;45(5):2300–2316. doi:10.1007/s00266-021-02439-5
3. Bass LS. Injectable filler techniques for facial rejuvenation, volumization, and augmentation. Facial Plast Surg Clin North Am. 2015;23(4):479–488. doi:10.1016/j.fsc.2015.07.004
4. Jitaree B, Phumyoo T, Uruwan S, Jiirasutat N, Pratoomthai B, Tansatit T. Clinical implications of the arterial supplies and their anastomotic territories in the nasolabial region for avoiding arterial complications during soft tissue filler injection. Clin Anat. 2021;34(4):581–589. doi:10.1002/ca.23617
5. Pilsl U, Anderhuber F. The External Nose: the nasal arteries and their course in relation to the nasolabial fold and groove. Plast Reconstr Surg. 2016;138(5):830e–835e. doi:10.1097/PRS.0000000000002626
6. Barton FE, Gyimesi IM. Anatomy of the nasolabial fold. Plast Reconstr Surg. 1997;100(5):1276–1280. doi:10.1097/00006534-199710000-00032
7. Kwon H-J OJ, Cho T-H, Choi Y-J, Yang HM. The nasolabial fold: a micro–computed tomography study. Plast Reconstr Surg. 2020;145(1):71–79. doi:10.1097/PRS.0000000000006328
8. Beer GM, Manestar M, Mihic-Probst D. The causes of the nasolabial crease: a histomorphological study. Clinical Anatomy. 2013;26(2):196–203. doi:10.1002/ca.22100
9. Pessa JE, Brown F. Independent effect of various facial mimetic muscles on the nasolabial fold. Aesthetic Plast Surg. 1992;16(2):167–171. doi:10.1007/BF00450609
10. Beleznay K, Carruthers JDA, Humphrey S, Carruthers A, Jones D. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39(6):662–674.
11. Scheuer JF, Sieber DA, Pezeshk RA, Gassman AA, Campbell CF, Rohrich RJ. 3rd, Sieber DA, Pezeshk RA, Gassman AA, Campbell CF, Rohrich RJ. Facial danger zones: techniques to maximize safety during soft-tissue filler injections. Plast Reconstr Surg. 2017;139(5):1103–1108. doi:10.1097/PRS.0000000000003309
12. Lee JG, Yang HM, Choi YJ, et al. Facial arterial depth and relationship with the facial musculature layer. Plast Reconstr Surg. 2015;135(2):437–444. doi:10.1097/PRS.0000000000000991
13. Scheuer JF. Anatomy of the facial danger zones: maximizing safety during soft-tissue filler injections. Plast Reconstr Surg. 2017;139(1):50e–58e.
14. Kim HS, Lee KL, Gil YC, Hu KS, Tansatit T, Kim HJ. Topographic anatomy of the infraorbital artery and Its clinical implications for nasolabial fold augmentation. Plast Reconstr Surg. 2018;142(3):273e–280e. doi:10.1097/PRS.0000000000004704
15. Jones DH, Fitzgerald R, Cox SE, et al. Preventing and treating adverse events of injectable fillers: evidence-based recommendations from the American Society for Dermatologic Surgery Multidisciplinary Task Force. Dermatol Surg. 2021;47(2):214–226. doi:10.1097/DSS.0000000000002921
16. Sundaram H, Weinkle S, Pozner J, Dewandre L. Blunt-tipped microcannulas for the injection of soft tissue fillers: a consensus panel assessment and recommendations. J Drugs Dermatol. 2012;11(8):s33–39.
17. Hexsel D, Soirefmann M, Porto MD, Siega C, Schilling-Souza J, Brum C. Double-blind, randomized, controlled clinical trial to compare safety and efficacy of a metallic cannula with that of a standard needle for soft tissue augmentation of the nasolabial folds. Dermatol Surg. 2012;38(2):207–214. doi:10.1111/j.1524-4725.2011.02195.x
18. Fulton J, Caperton C, Weinkle S, Dewandre L. Filler injections with the blunt-tip microcannula. J Drugs Dermatol. 2012;11(9):1098–1103.
19. Beer KR. Safety and effectiveness of injection of calcium hydroxylapatite via blunt cannula compared to injection by needle for correction of nasolabial folds. J Cosmet Dermatol. 2014;13(4):288–296. doi:10.1111/jocd.12115
20. Jones D, Palm M, Cox SE, McDermott M, Sartor M, Chawla S. Safety and effectiveness of hyaluronic acid filler, VYC-20L, via cannula for cheek augmentation: a randomized, single-blind, controlled study. Dermatol Surg. 2021;47(12):1590–1594. doi:10.1097/DSS.0000000000003246
21. Fabi S, Zoumalan C, Fagien S, Yoelin S, Sartor M, Chawla S. A prospective, multicenter, single-blind, randomized, controlled study of VYC-15L, a hyaluronic acid filler, in adults for correction of infraorbital hollowing. Aesthet Surg J. 2021;41(11):NP1675–NP1685. doi:10.1093/asj/sjab308
22. Gubanova EI, Starovatova PA. A prospective, comparative, evaluator-blind clinical study investigating efficacy and safety of two injection techniques with Radiesse(®) for the correction of skin changes in aging hands. J Cutan Aesthet Surg. 2015;8(3):147–152. doi:10.4103/0974-2077.167271
23. Chopra R, Graivier M, Fabi S, Nestor M, Meuse P, Mashburn J. A multi-center, open-label, prospective study of cannula injection of small-particle hyaluronic acid plus lidocaine (SPHAL) for lip augmentation. J Drugs Dermatol. 2018;17(1):10–16.
24. Zhou SB, Chiang CA, Liu K. False sense of safety: blunt cannulas cause the majority of severe vascular complications in hyaluronic acid injection. Plast Reconstr Surg. 2020;146(2):240e–241e. doi:10.1097/PRS.0000000000007022
25. Tansatit T, Apinuntrum P, Phetudom T. A dark side of the cannula injections: how arterial wall perforations and emboli occur. Aesthetic Plast Surg. 2017;41(1):221–227. doi:10.1007/s00266-016-0725-7
26. Pavicic T, Webb KL, Frank K, Gotkin RH, Tamura B, Cotofana S. Arterial wall penetration forces in needles versus cannulas. Plast Reconstr Surg. 2019;143(3):504e–512e. doi:10.1097/PRS.0000000000005321
27. Ugradar S, Hoenig J. Measurement of the force required by blunt-tipped microcannulas to perforate the facial artery. Ophthalmic Plast Reconstr Surg. 2019;35(5):444–446. doi:10.1097/IOP.0000000000001302
28. Faivre J, Gallet M, Tremblais E, Trevidic P, Bourdon F. Advanced concepts in rheology for the evaluation of hyaluronic acid-based soft tissue fillers. Dermatol Surg. 2021;47(5):e159–e167. doi:10.1097/DSS.0000000000002916
29. Trevidic P, Kaufman-Janette J, Weinkle S, et al. Injection guidelines for treating midface volume deficiency with hyaluronic acid fillers: the ATP approach (anatomy, techniques, products). Aesthet Surg J. 2022;42(8):920–934. doi:10.1093/asj/sjac007
30. Sundaram H, Shamban A, Schlessinger J, et al. Efficacy and safety of a new resilient hyaluronic acid filler in the correction of moderate-to-severe dynamic perioral rhytides: a 52-week prospective, multicenter, controlled, randomized, evaluator-blinded study. Dermatol Surg. 2022;48(1):87–93. doi:10.1097/DSS.0000000000003238
31. Rzany B, Converset-Viethel S, Hartmann M, et al. Efficacy and safety of 3 new resilient hyaluronic acid fillers, crosslinked with decreased BDDE, for the treatment of dynamic wrinkles: results of an 18-month, randomized controlled trial versus already available comparators. Dermatol Surg. 2019;45(10):1304–1314. doi:10.1097/DSS.0000000000001971
32. Kaufman-Janette J, Taylor SC, Cox SE, Weinkle SH, Smith S, Kinney BM. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18(5):1244–1253. doi:10.1111/jocd.13100
33. Monheit G, Kaufman-Janette J, Joseph JH, Shamban A, Dover JS, Smith S. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blinded, and within-subject study. Dermatol Surg. 2020;46(12):1521–1529. doi:10.1097/DSS.0000000000002391
34. Development and validation of a nasolabial fold severity rating scale 2017 PMA P170002. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170002B.pdf.
35. Kappos EA, Temp M, Schaefer DJ, Haug M, Kalbermatten DF, Toth BA. Validating facial aesthetic surgery results with the FACE-Q. Plast Reconstr Surg. 2017;139(4):839–845. doi:10.1097/PRS.0000000000003164
36. Klassen AF, Cano SJ, Schwitzer JA, et al. Development and psychometric validation of the FACE-Q skin, lips, and facial rhytids appearance scales and adverse effects checklists for cosmetic procedures. JAMA Dermatol. 2016;152(4):443–451. doi:10.1001/jamadermatol.2016.0018
37. Klassen AF, Cano SJ, Scott A, Snell L, Pusic AL. Measuring patient-reported outcomes in facial aesthetic patients: development of the FACE-Q. Facial Plast Surg. 2010;26(4):303–309. doi:10.1055/s-0030-1262313
38. Alam MS, Banerjee P. Intravenous cannula as an economical option for canalicular trephine in cases of canalicular obstruction. Ophthalmic Plast Reconstr Surg. 2021;37(3S):S120–S121. doi:10.1097/IOP.0000000000001825
39. Yeh LC, Fabi SG, Welsh K. Arterial penetration with blunt-tipped cannulas using injectables: a false sense of safety? Dermatol Surg. 2017;43(3):464–467. doi:10.1097/DSS.0000000000000929
40. Wang JV, Valiga A, Albornoz CA, Geronemus RG. Comparison of injectable filler locations in men and women: an age-matched case analysis. J Cosmet Dermatol. 2021;20(8):2469–2471. doi:10.1111/jocd.14293
41. Alexis A, Boyd C, Callender V, Downie J, Sangha S. Understanding the female African American facial aesthetic patient. J Drugs Dermatol. 2019;18(9):858–866.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
