Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Efficacy and Safety of Remdesivir in Hospitalized Pediatric COVID-19: A Retrospective Case-Controlled Study
Authors Khalil A , Mohamed A, Hassan M, Magboul S, Ali H, Elmasoudi AS, Ellithy K, Qusad M, Alhothi A, Al Maslamani E, Al Amri M, Soliman A
Received 14 September 2023
Accepted for publication 13 November 2023
Published 23 November 2023 Volume 2023:19 Pages 949—958
DOI https://doi.org/10.2147/TCRM.S432565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Ahmed Khalil,1 Asmaa Mohamed,1 Manasik Hassan,2 Samar Magboul,2 Hossamaldein Ali,1 Ahmed Salah Elmasoudi,1 Khaled Ellithy,3 Mohammad Qusad,2 Abdulla Alhothi,2 Eman Al Maslamani,4 Mohammed Al Amri,5 Ashraf Soliman5
1Section of Pediatric Clinical Pharmacy, Pharmacy Department, Hamad General Hospital, Doha, Qatar; 2Section of Academic General Pediatrics, Department of Pediatrics, Hamad General Hospital, Doha, Qatar; 3Section of Pediatric Intensive Care Unit, Department of Pediatrics, Hamad General Hospital, Doha, Qatar; 4Section of Infectious Diseases, Department of Pediatrics, Sidra Medicine, Doha, Qatar; 5Department of Pediatrics, Hamad General Hospital, Doha, Qatar
Correspondence: Ahmed Khalil, Hamad General Hospital (HGH), Hamad Medical Corporation (HMC), Doha, 3050, Qatar, Tel +974 55078679, Email [email protected]
Introduction: While most children experience mild coronavirus disease 2019 (COVID-19) infections, a minority of cases progress to severe or critical illness. This study aimed to assess the efficacy and safety of Remdesivir (RDV) therapy in children with moderate to severe COVID-19, enhancing clinical decision-making and expanding our understanding of antiviral treatments for pediatric patients.
Methods: The study included 60 patients, 38 receiving RDV treatment and 22 serving as the control group. Data was collected retrospectively from January 2021 to January 2022 through electronic hospital records.
Results: Regarding the main clinical symptoms reported, most patients experienced Upper Respiratory Tract Infections (93.3%), indicating respiratory involvement. Additional symptoms included Central Nervous System (11.7%) and Gastrointestinal (10.0%). Among the 38 cases in the RDV group included in the study, the adverse effects associated with using RDV: Hypoalbuminemia in 19 cases (50.0%) and anemia in 18 cases (47.4%), making them the most common adverse effects. Only one case in the RDV group experienced non-RDV-related death with a different clinical diagnosis. The results showed that RDV treatment was well-tolerated in pediatric patients, with no significant differences in hospital stay and oxygen treatment compared to the control group with P values (0.2, 0.18), respectively.
Conclusion: The outcomes indicate that Remdesivir may represent a safe and therapeutic choice for children with coronavirus disease 2019 (COVID-19).
Keywords: COVID-19, remdesivir, RDV, efficacy, safety, SARS-CoV-2
Introduction
The pathogenic agent SARS-CoV-2, belonging to the novel coronavirus 2 family, exerts its predominant effects on the respiratory tract, eliciting the onset of a complex and potentially life-threatening condition known as severe acute respiratory syndrome.1 The disease exhibits a spectrum of clinical presentations, from mild and asymptomatic manifestations to severe cases characterized by hypoxemia, ultimately culminating in respiratory failure and mortality.2 However, in the case of children, COVID-19 disease predominantly presents in a mild form and can often be managed with supportive care alone. Only a small proportion of children experience severe or critical illness, necessitating assisted ventilation and admission to the intensive care unit during the infection.3
In the quest for treating coronavirus disease 2019 (COVID-19) effectively, the main focus lies in utilizing extensively studied randomized trials and well-established medications.4–8 Antivirals with inhibitory effects on protease and nucleotide or nucleoside analogs targeting viral RNA synthesis have been repurposed for the management of coronavirus disease 2019 (COVID-19).9–16 Among these agents, nucleoside analogs, particularly Remdesivir, stand out as a highly potent antiviral option to combat the coronavirus disease 2019 (COVID-19). It serves as a nucleoside analog prodrug, effectively inhibiting viral RNA polymerases and leading to delayed chain termination in viral RNA replication.17,18 Notably, it has demonstrated both in vitro and in vivo efficacy against SARS-CoV-2.19 In recent times, Remdesivir (RDV) has shown encouraging outcomes, establishing itself as a promising antiviral for potential COVID-19 treatment. Preliminary data from China indicated that RDV did not demonstrate clinical benefits in adults treated with the drug.20 In the months following the pandemic outbreak, recent evidence has surfaced, showcasing the efficacy of the Remdesivir in expediting clinical recovery time in adults with COVID-19. Conversely, various studies have highlighted the ineffectiveness of hydroxychloroquine and lopinavir-ritonavir.21–25 As a consequence of this data, the US Food and Drug Administration granted an emergency use authorization (EUA) for Remdesivir, while the previously issued EUA for hydroxychloroquine was rescinded.26–29 Recent outcomes from clinical trials, involving over 1000 adult participants, have revealed a reduced time to recovery when utilizing RDV compared to placebo.21 Remdesivir has been granted emergency approval for COVID-19 treatment. However, Remdesivir demonstrates limited efficacy in patients with COVID-19 who have already progressed to mechanical ventilation. In a broader context of hospitalized COVID-19 patients, it exhibits a modest impact on reducing mortality rates, the necessity for ventilatory support, or both. Notably, the clinical utility of remdesivir remains inconclusive for individuals admitted to the hospital for COVID-19 who have exhibited symptoms for more than seven days and require supplemental oxygen. Moreover, the therapeutic regimens involving remdesivir, Hydroxychloroquine, lopinavir, and interferon show minimal to negligible influence on the outcomes of hospitalized COVID-19 patients; this is evidenced by their limited impact on overall mortality, the initiation of mechanical ventilation, and the duration of hospitalization.30–32
Remdesivir presents several noteworthy considerations that impact its clinical utility as an antiviral agent. First, hepatic disposition: Originally designed for hepatitis C treatment, remdesivir’s liver-focused nature may not align well with COVID-19’s primary site of infection, the lungs. Secondly, limited administration options: Remdesivir’s short half-life and rapid clearance necessitate intravenous use in hospitals, limiting its applications. Buccal administration remains a potential avenue but faces challenges. Thirdly, overemphasis on preclinical data: Relying solely on low EC50 values from in vitro studies may not accurately reflect the drug’s clinical effectiveness. Finally, long-term safety profile: The non-uniform distribution of remdesivir raises concerns about drug accumulation, potential toxicity, and the development of drug resistance.33 Remdesivir functions as a substrate for the organic anion transporting polypeptides OATP1B1, OATP1B3, and the P-glycoprotein (P-gp) transporters. It also interacts with multiple cytochrome P450 (CYP450) enzymes, notably CYP2C8, CYP2D6, and CYP3A4, and exhibits inhibitory characteristics in vitro settings. Importantly, there is an absence of compelling evidence showcasing CYP induction by remdesivir and its metabolites in vivo. However, considering its mode of administration and rapid clearance from the body, the potential for remdesivir to induce clinically significant drug-drug interactions (DDIs) appears constrained.34,35 Nonetheless, the necessity for further clinical investigations and studies persists, aimed at assessing its interaction with the cytochrome P450 system and thereby elucidating the prospective drug-drug interactions associated with remdesivir.
Limited data on children are accessible, given that the majority of clinical trials have concentrated on adults.21,31,36–41 Due to well-established physiological differences between adults and children, any drug that proves effective in treating adults might not be appropriate for pediatric use. Furthermore, there is currently a lack of information on the pediatric pharmacokinetics of RDV exposure.42 Nevertheless, in cases of severe COVID-19 in children, RDV usage is advised, as it stands as a novel antiviral drug demonstrating some efficacy in the clinical trials.21,43 Recent reports have indicated that young infants and children with preexisting medical conditions are at an elevated risk of experiencing severe illness and mortality.44,45 COVID-19 infection has been correlated with multisystem inflammatory syndrome in children, as well as cardiac dysfunction.46,47 In light of the swiftly growing body of evidence concerning the most effective antiviral therapy for COVID-19, it is essential to note that there is still a lack of pediatric-specific data in this area. Therefore, data on the utilization of RDV in the pediatric population is crucial, particularly due to its current prescription for critically ill children. With this background, this retrospective cohort study aims to evaluate the efficacy and safety of RDV in shortening the time to clinical recovery in moderate to severe pediatric cases with COVID-19. This study holds significant importance and can positively impact understanding of the role of Remdesivir in pediatrics. Currently, a limited amount of data is available in the literature regarding its use in pediatric populations. Thus, this study will be the first of its kind in Qatar and the Middle East, investigating the efficacy and safety of Remdesivir, specifically in the pediatric population. The findings can serve as valuable guidance for clinical decision-making and make a significant contribution to the existing knowledge on antiviral therapies for pediatric COVID-19 patients.
Methods
Study Design
This retrospective descriptive study was exclusively conducted at Hamad Medical Corporation in the State of Qatar, focusing on data from a single institution. The study focused on pediatric patients below the age of 14 years who were hospitalized with moderate to severe COVID-19 and required oxygen support in most of them; the study period spanned from January 1, 2021, to January 30, 2022. A total of 60 patients were included in the study, with 38 patients receiving treatment with Remdesivir (RDV group) and 22 patients not receiving Remdesivir treatment (control group). The study followed the principles outlined in the “Declaration of Helsinki” and adhered to Good Clinical Practice guidelines. All research activities followed the relevant laws and regulations the Ministry of Public Health in Qatar set. The study protocol underwent a comprehensive review and received approval from the local Ethics Committee, specifically the Medical Research Committee (MRC), before initiation. As the study followed a retrospective approach, a waiver of informed consent was obtained from the research committee. Information regarding patient characteristics, treatment modalities, and clinical outcomes was gathered using a pre-established data collection template, securely stored within a designated, restricted-access cabinet, with sole access granted to the primary investigator (PI). Subsequently, the information was anonymized and maintained with confidentiality by entering it into an Excel spreadsheet, utilizing serial numbers exclusively, on a laptop solely accessible to the PI to conduct statistical analyses.
Inclusion and Exclusion Criteria
An investigative review study based on chart analysis was conducted on all hospitalized pediatric patients admitted to HMC pediatric COVID facilities, including the general floor and the pediatric intensive care unit. The study included patients who met the following inclusion criteria: (a) SARS-CoV-2 PCR positive (b) hospitalized pediatric patients below the age of 14 years with confirmed COVID-19 and a moderate to severe course of the disease (new or increased supplemental oxygen requirement); While decisions were made following an individualized risk/benefit assessment, in certain instances, patients were admitted due to concerns related to extrapulmonary manifestations of COVID-19 infection, severe comorbidities, or radiographic findings. (c) Normal kidney function, indicated by an estimated glomerular filtration rate (eGFR) exceeding 30 mL/min/1.73m2; (d) Alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels within the normal range. (AST) within the normal range and (e) No other antivirals used for SARS-CoV-2.
Exclusion criteria include: (a) SARS-CoV-2 PCR positive cases with mild severity of illness (b) Acute or chronic kidney diseases with an eGFR < 30 mL/min/1.73m2; and (c) Liver diseases with ALT ≥ 5 times the upper limit of normal at baseline. Following meticulous application of inclusion and exclusion criteria, a total of 60 cases were selected for the final study.
Data Collection
For all pediatric cases, comprehensive clinical and laboratory data were retrospectively collected by reviewing the patients’ electronic hospital medical records (Cerner).
Statistical Analysis
Descriptive statistics provide a concise summary of continuous and quantitative variables, while Categorical data were represented as frequency counts (N) and percentages (%). All statistical analyses were performed using the Statistical Package for the Social Sciences, version 25.0. Subgroup analysis explored the relationship between clinical and demographic factors and clinical outcomes. Patients with missing data for a particular variable were excluded from calculations and analyses. A significance level of p<0.05 was considered statistically significant.
Results
Baseline Demographics and Clinical Characteristics
The demographic and clinical profiles of the patients were compared between the RDV and control groups and are presented in (Table 1). Most patients fell within the age range of 5 to 14 years, accounting for 41.7% of the total sample. This was followed by patients aged 1–5 years, 2 months to 1 year, and <2 months, comprising (28.3%, 16.7%, and 13.3%, respectively). The study population consisted of more males (56.7%) than females (43.3%).
 |
Table 1 Demographic Characteristics |
Comorbidities
The most prevalent underlying medical condition among the patients was related to the Central Nervous System, accounting for (33.3%) of the cases. Other notable conditions included cardiac (21.7%), pulmonary (13.3%), and genetic (10.0%) conditions. The presence of oncology and immunology conditions was relatively low (1.7% each). Regarding the main clinical symptoms reported, most patients experienced Upper Respiratory Tract Infections (93.3%), indicating respiratory involvement. Additional symptoms included Central Nervous System manifestations (11.7%) and Gastrointestinal symptoms (10.0%). In terms of respiratory support, a significant proportion of patients (75.0%) received non-invasive respiratory support, while a smaller percentage required invasive support (15.0%). A small group of patients (10.0%) did not require respiratory support (off O2).
Many patients (88.3%) did not necessitate inotropic support, indicating stable cardiac function. However, a minority of cases (11.7%) required inotropic support, signifying compromised cardiac function. Furthermore, the majority of patients (86.7%) did not encounter any reported clinical complications. Nonetheless, a small proportion of cases were associated with Central Nervous System complications (6.7%), while an even smaller percentage exhibited cardiac complications (1.7%). Within the patient cohort, a total of three deaths occurred, accounting for (5.0%) of the cases. It is important to note that one case in the RDV group resulted in a non-RDV-related death, and all three deaths had distinct clinical diagnoses. The first patient had lobar holoprosencephaly, global developmental delay (GDD), seizure disorder, acute respiratory distress syndrome (ARDS), and multiorgan failure. The second patient had ARDS and pulmonary hemorrhage. The third patient had cardiomyopathy with poor cardiac function. The RDV and control groups did not exhibit a significant difference in terms of the duration of hospital stay and weaning from oxygen treatment (Table 2).
 |
Table 2 Comparison of Hospital Stay and Oxygen Support Duration in RDV and Control Groups |
In adherence to local and international protocols, Dexamethasone, a corticosteroid known for its anti-inflammatory properties, was administered to the majority of COVID pneumonia cases, with (81.6%) of patients receiving this therapy in the current study. Additionally, as part of their primary treatment, (34.2%) of patients were prescribed Enoxaparin, while (21.1%) received Ceftriaxone, an antibiotic. Less frequently used therapies encompassed Anakinra, IVIG, Tocilizumab, Methylprednisolone, and Azithromycin, with frequencies ranging from (2.6% to 10.5%.) Anakinra, Tocilizumab, and Methylprednisolone are immunosuppressive or anti-inflammatory drugs that may be employed in specific cases to manage severe immune responses. IVIG is a treatment that provides antibodies to enhance the immune system. Azithromycin, an antibiotic, may have been prescribed to address atypical bacterial infections (Table 3). The clinical characteristics of the study population are summarized in (Table 4). There were no significant differences in clinical characteristics between the RDV and control groups, p>0.05.
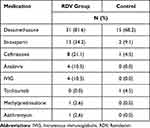 |
Table 3 Other Medication During the COVID-19 Course |
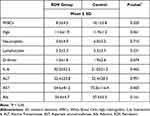 |
Table 4 Comparison of Clinical Characteristics by RDV and Control Groups |
Among the 38 patients in the RDV group included in this study as presented in (Table 5), The Data concerning adverse effects related to the administration of Remdesivir were documented. Hypoalbuminemia was the most common adverse effect, observed in 19 cases (50%), followed by Anemia in 18 cases (47.4%), High ALT in 13 cases (34.2%), Hypokalemia in 9 cases (23.7%), and Thrombocytopenia, elevated AST, and PT in 8 cases each (21.1%). Additionally, Vomiting was reported in only 3 cases (7.9%).
 |
Table 5 Adverse Effects Related to the Remdesivir |
Discussion
This retrospective cohort study involving pediatric population under the age of 14 years provides evidence regarding the efficacy and safety profile of Remdesivir, along with other drugs, in hospitalized patients with moderate to severe COVID-19 and those who required oxygen support. In comparison to other drugs, the treatment with RDV was well tolerated. Out of the 38 patients treated with RDV, one case succumbed to the illness as it progressed. A more extensive case series involving children diagnosed with COVID-19 in the USA and Europe during the early phase of the outbreak revealed that younger age and pre-existing medical conditions were associated with worse clinical outcomes and similar patients aged 1–5 years (28.3%), 2 months to 1 year (16.7%) and <2 months (13.3%), 5 to 14 (41.7%) were observed in our cohort.31,34,38 The study population consisted of more males (56.7%) than females (43.3%).
Moreover, RDV patients exhibited a lower rate of hospitalization. In the initial stages of illness, when the virus actively multiplies in the host’s tissue, Remdesivir has demonstrated promising potential as a treatment option.48 Nevertheless, in our cohort, patients received RDV treatment courses within 5 to 10 after the onset of symptoms, as noted in the study.21 For children with a positive SARS-CoV-2 PCR test conducted within the previous 3–4 days, the current recommendations suggest intravenous administration of RDV for a duration of 3–5 days.48 In our study, we adhered to these existing indications for using RDV in our study population.
In this study, 5 (13.2%) patients receiving RDV required inotropic support, and these findings were like the study by Goldman et al.49 It is important to highlight that (86.8%) of the patients receiving RDV did not experience any complications.
In this study, children undergoing RDV treatment encountered temporary adverse effects during the treatment course, which subsequently normalized upon discharge. These effects included hypoalbuminemia, anemia, thrombocytopenia, hypokalemia, Elevated levels of transaminases in the bloodstream (liver enzymes), high prothrombin time (PT), and vomiting. Notably, our findings align with previous reports on this subject.50,51 These results imply that RDV may have a potential beneficial effect in mitigating complications and specific laboratory abnormalities when administered to pediatric patients with COVID-19.
According to our data, treatment with RDV may have played a role in preventing the progression to more severe respiratory disease, evident from the lower proportion of serious adverse events related to respiratory failure and a reduced incidence of new oxygen requirements, additionally, a lower proportion of children required higher levels of respiratory support during the study. Our findings align with the research conducted by Beigel et al, where RDV was superior with evidence of lower respiratory infection compared to placebo.21 Clinical trials and research efforts have primarily concentrated on adult care during the current pandemic.21,42 However, pediatricians must ensure optimal care for particularly vulnerable children, even in challenging circumstances. Unfortunately, there is a need for more data regarding the efficacy, safety, tolerability, and pharmacokinetics of Remdesivir in the pediatric population under 12 years old.21 Nevertheless, in patients where COVID-19 is severe, RDV should be considered for this specific population.43 The availability of randomized controlled trials (RCTs) concerning pediatric patients for COVID-19 treatments is limited due to ethical concerns about severe presentations in children. Evaluating the risks and benefits carefully is crucial for this vulnerable population. Despite challenges, it is crucial to carefully evaluate the risks and benefits of treatment options for vulnerable pediatric populations. Tailored evidence is necessary to minimize morbidity and mortality and ensure the optimal care of children with COVID-19. The strengths of this retrospective study lie in its ability to provide valuable insights into the efficacy and safety of Remdesivir in children with COVID-19, along with comprehensive data collection encompassing demographic information, clinical findings, and laboratory investigations. However, the study’s limitations include the small sample size of the RDV-treated cohort, limiting generalizability, and the absence of a randomized control group, which further restricts the establishment of causal relationships, the study’s reliance on data from a single institution, and the retrospective design. Continued research efforts are needed to provide more robust evidence for effective and safe treatments in this specific population.
Conclusion
In conclusion, our findings of this study provide evidence that Remdesivir treatment is well tolerated in children below the age of 14 years. The data suggest that RDV may be a viable treatment option for pediatric population with COVID-19 infection.
Data Sharing Statement
Upon reasonable request, the primary author will provide the raw data supporting the conclusions of this article.
Ethics Statement
The study was conducted in accordance with the principles of the Declaration of Helsinki, Good Clinical Practice (GCP), and in compliance with the laws and regulations of the Ministry of Public Health (MOPH) in Qatar. The study received approval from the Institutional Review Board (IRB) committee in Medical Research Center (MRC), Doha, Qatar, with the number (MRC-01-22-090).
Acknowledgment
We stand in solidarity with those who are currently battling or have experienced illness due to COVID-19 infection, as well as their families and the healthcare professionals bravely confronting this pandemic on the front lines.
Author Contributions
All authors made a significant contribution to the work reported whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This article’s publication was funded by the Medical Research Center (MRC) of Hamad Medical Corporation (HMC).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang Z, Yang L. The therapeutic potential of natural dietary flavonoids against SARS-CoV-2 infection. Nutrients. 2023;15(15):3443. doi:10.3390/nu15153443
2. McIntosh K, Hirsch MS, Bogorodskaya M. COVID-19: clinical features; 2023.
3. Manti S, Licari A, Montagna L, et al. SARS-CoV-2 infection in pediatric population. Acta Biomed. 2020;91(11–S):e2020003. doi:10.23750/abm.v91i11-S.10298
4. Shakoor H, Feehan J, Al Dhaheri AS, et al. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: could they help against COVID-19? Maturitas. 2021;143:1–9. doi:10.1016/j.maturitas.2020.08.003
5. Michienzi SM, Badowski ME. Can vitamins and/or supplements provide hope against coronavirus? Drugs Context. 2020;9:1–29. doi:10.7573/dic.2020-5-7
6. Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J Infect Public Health. 2020;13(10):1373–1380. doi:10.1016/j.jiph.2020.06.021
7. Naghipour S, Ghodousi M, Rahsepar S, Elyasi S. Repurposing of well-known medications as antivirals: hydroxychloroquine and chloroquine – from HIV-1 infection to COVID-19. Expert Rev Anti Infect Ther. 2020;18(11):1119–1133. doi:10.1080/14787210.2020.1792291
8. Pawar AY. Combating devastating COVID-19 by drug repurposing. Int J Antimicrob Agents. 2020;56(2):105984. doi:10.1016/j.ijantimicag.2020.105984
9. Wang J. Fast identification of possible drug treatment of Coronavirus Disease-19 (COVID-19) through Computational Drug Repurposing Study. J Chem Inf Model. 2020;60(6):3277–3286. doi:10.1021/acs.jcim.0c00179
10. McKee DL, Sternberg A, Stange U, Laufer S, Naujokat C. Candidate drugs against SARS-CoV-2 and COVID-19. Pharmacol Res. 2020;157:104859. doi:10.1016/j.phrs.2020.104859
11. Hall DC, Ji HF. A search for medications to treat COVID-19 via in silico molecular docking models of the SARS-CoV-2 spike glycoprotein and 3CL protease. Travel Med Infect Dis. 2020;35:101646. doi:10.1016/j.tmaid.2020.101646
12. Zhu Z, Lu Z, Xu T, et al. Arbidol monotherapy is superior to lopinavir/ritonavir in treating COVID-19. J Infect. 2020;81(1):e21–e23. doi:10.1016/j.jinf.2020.03.060
13. Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi:10.1038/s41422-020-0282-0
14. Elfiky AA. Ribavirin, Remdesivir, Sofosbuvir, Galidesivir, and Tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020;253:117592. doi:10.1016/j.lfs.2020.117592
15. Martinez MA. Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob Agents Chemother. 2020;64(5). doi:10.1128/AAC.00399-20
16. Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):7798):265–269. doi:10.1038/s41586-020-2008-3
17. Yang L, Wang Z. Bench-to-bedside: innovation of small molecule anti-SARS-CoV-2 drugs in China. Eur J Med Chem. 2023;257:115503. doi:10.1016/j.ejmech.2023.115503
18. Blair HA. Remdesivir: a review in COVID-19. Drugs. 2023;83(13):1215–1237. doi:10.1007/s40265-023-01926-0
19. Ko WC, Rolain JM, Lee NY, et al. Arguments in favour of remdesivir for treating SARS-CoV-2 infections. Int J Antimicrob Agents. 2020;55(4):105933. doi:10.1016/j.ijantimicag.2020.105933
20. Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395(10236):1569–1578. doi:10.1016/S0140-6736(20)31022-9
21. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of covid-19 — final report. N Engl J Med. 2020;383(19):1813–1826. doi:10.1056/NEJMoa2007764
22. Linsell L, Bell J. Effect of hydroxychloroquine in hospitalized patients with covid-19. N Engl J Med. 2020;383(21):2030–2040. doi:10.1056/NEJMoa2022926
23. Tang W, Cao Z, Han M, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020:m1849. doi:10.1136/bmj.m1849
24. Cavalcanti AB, Zampieri FG, Rosa RG, et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate covid-19. N Engl J Med. 2020;383(21):2041–2052. doi:10.1056/NEJMoa2019014
25. Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe covid-19. N Engl J Med. 2020;382(19):1787–1799. doi:10.1056/NEJMoa2001282
26. Chan‐Tack K, Sampson M, Earp J, et al. Considerations and challenges in the remdesivir COVID‐19 pediatric development program. J Clin Pharmacol. 2023;63(2):259–265. doi:10.1002/jcph.2158
27. Low M, City F. EUA 046 Gilead remdesivir LOA outpatients (01212022); 2022:1–9
28. FDA. Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine. FDA; 2020.
29. Hegazy SK, Tharwat S, Hassan AH. Clinical study to compare the efficacy and safety of casirivimab & imdevimab, remdesivir, and favipravir in hospitalized COVID-19 patients. J Clin Virol Plus. 2023;3(2):100151. doi:10.1016/j.jcvp.2023.100151
30. WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO solidarity randomised trial and updated meta-analyses [published correction appears in Lancet. 2022 Oct 29;400(10362):1512]. Lancet. 2022;399(10339):1941–1953. doi:10.1016/S0140-6736(22)00519-0
31. Ader F, Bouscambert-Duchamp M, Hites M, et al. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a Phase 3, randomised, controlled, open-label trial. Lancet Infect Dis. 2022;22(2):209–221. doi:10.1016/S1473-3099(21)00485-0
32. Pan H, Peto R; WHO Solidarity Trial Consortium. Repurposed antiviral drugs for covid-19 - interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511. doi:10.1056/NEJMoa2023184
33. Wang Z, Yang L, Song X-Q. Oral GS-441524 derivatives: next-generation inhibitors of SARS‐CoV‐2 RNA‐dependent RNA polymerase. Front Immunol. 2022;13:1015355. doi:10.3389/fimmu.2022.1015355
34. Humeniuk R, Mathias A, Kirby BJ, et al. Pharmacokinetic, pharmacodynamic, and drug-interaction profile of remdesivir, a SARS-CoV-2 replication inhibitor. Clin Pharmacokinet. 2021;60(5):569–583. doi:10.1007/s40262-021-00984-5
35. Yang K. What do we know about remdesivir drug interactions? Clin Transl Sci. 2020;13(5):842–844. doi:10.1111/cts.12815
36. Munoz F, Muller W, Ahmed A, et al. Safety and efficacy of remdesivir in a pediatric covid-19 population. Top Antivir Med. 2021;29(1):237.
37. Elsawah HK, Elsokary MA, Abdallah MS, ElShafie AH. Efficacy and safety of remdesivir in hospitalized Covid‐19 patients: systematic review and meta‐analysis including network meta‐analysis. Rev Med Virol. 2021;31(4). doi:10.1002/rmv.2187
38. Wu Z, Han Z, Liu B, Shen N. Remdesivir in treating hospitalized patients with COVID-19: a renewed review of clinical trials. Front Pharmacol. 2022;13. doi:10.3389/fphar.2022.971890
39. Angamo MT, Mohammed MA, Peterson GM. Efficacy and safety of remdesivir in hospitalised COVID-19 patients: a systematic review and meta-analysis. Infection. 2022;50(1):27–41. doi:10.1007/s15010-021-01671-0
40. Seethapathy R, Wang Q, Zhao S, et al. Effect of remdesivir on adverse kidney outcomes in hospitalized patients with COVID-19 and impaired kidney function. PLoS One. 2023;18(2):e0279765. doi:10.1371/journal.pone.0279765
41. Alsowaida YS, Shehadeh F, Kalligeros M, Mylonakis E. Incidence, and potential risk factors for remdesivir-associated bradycardia in hospitalized patients with COVID-19: a retrospective cohort study. Front Pharmacol. 2023;14:1106044. doi:10.3389/fphar.2023.1106044
42. Maharaj AR, Wu H, Hornik CP, et al. Simulated assessment of pharmacokinetically guided dosing for investigational treatments of pediatric patients with coronavirus disease 2019. JAMA Pediatr. 2020;174(10):e202422. doi:10.1001/jamapediatrics.2020.2422
43. Chiotos K, Hayes M, Kimberlin DW, et al. Multicenter interim guidance on use of antivirals for children with coronavirus disease 2019/severe acute respiratory syndrome coronavirus 2. J Pediatric Infect Dis Soc. 2021;10(1):34–48. doi:10.1093/jpids/piaa115
44. Götzinger F, Santiago-García B, Noguera-Julián A, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4(9):653–661. doi:10.1016/S2352-4642(20)30177-2
45. Kim L, Whitaker M, O’Halloran A, et al. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET,14 States, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1081–1088. doi:10.15585/mmwr.mm6932e3
46. Hasan MR, Al Zubaidi K, Diab K, et al. COVID-19 related multisystem inflammatory syndrome in children (MIS-C): a case series from a tertiary care pediatric hospital in Qatar. BMC Pediatr. 2021;21(1):267. doi:10.1186/s12887-021-02743-8
47. Molloy EJ, Nakra N, Gale C, Dimitriades VR, Lakshminrusimha S. Multisystem inflammatory syndrome in children (MIS-C) and neonates (MIS-N) associated with COVID-19: optimizing definition and management. Pediatr Res. 2023;93(6):1499–1508. doi:10.1038/s41390-022-02263-w
48. Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical–therapeutic staging proposal. J Heart Lung Transplant. 2020;39(5):405–407. doi:10.1016/j.healun.2020.03.012
49. Goldman DL, Aldrich ML, Hagmann SHF, et al. Compassionate use of remdesivir in children with severe COVID-19. Pediatrics. 2021;147(5). doi:10.1542/peds.2020-047803
50. La Tessa A, Motisi MA, Marseglia GL, et al. Use of remdesivir in children with covid-19 infection: a quick narrative review. Acta Biomed. 2021;92(3). doi:10.23750/ABM.V92IS7.12396
51. Mohammad Zadeh N, Mashinchi Asl NS, Forouharnejad K, et al. Mechanism and adverse effects of COVID-19 drugs: a basic review. Int J Physiol Pathophysiol Pharmacol. 2021;13(4):102–109.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
