Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Efficacy and Safety of Detachable Microneedle Patch Containing Triamcinolone Acetonide in the Treatment of Inflammatory Acne
Authors Thantaviriya S, Kamanamool N, Sansureerungsikul T, Udompataikul M, Wanichwecharungruang S, Rojhirunsakool S
Received 6 March 2023
Accepted for publication 17 May 2023
Published 5 June 2023 Volume 2023:16 Pages 1431—1441
DOI https://doi.org/10.2147/CCID.S411378
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Soraya Thantaviriya,1 Nanticha Kamanamool,2 Titiporn Sansureerungsikul,3 Montree Udompataikul,1 Supason Wanichwecharungruang,3 Salinee Rojhirunsakool1
1Department of Dermatology, Faculty of Medicine, Srinakharinwirot University, Bangkok, Thailand; 2Department of Preventive and Social Medicine, Faculty of Medicine, Srinakharinwirot University, Bangkok, Thailand; 3Department of Chemistry, Faculty of Science, Chulalongkorn University, Bangkok, Thailand
Correspondence: Salinee Rojhirunsakool, Department of Dermatology, Faculty of Medicine, Srinakharinwirot University, 114 Sukhumvit 23, Wattana District, Bangkok, 10110, Thailand, Tel +66894159665, Email [email protected]
Background: Detachable microneedles (DMNs) are dissolvable microneedles that detach from the base during administration. The use of DMNs-containing steroids for acne has never been investigated.
Methods: Thirty-five patients with facial inflammatory acne were evaluated for acne treatment efficacy and safety of DMNs and DMNs containing triamcinolone acetonide (TA) via a 28-day randomized, double-blind, controlled trial. Four inflammatory acne lesions were selected from each participant and randomly treated with a single application of 700 μm DMNs containing 262.02 ± 15.62 μg TA (700DMNTA), 1000 μm DMNs containing 160.00 ± 34.92 μg TA (1000DMNTA), 700 μm DMN without TA (700DMN), and a control. Efficacy was measured by assessing physical grading, diameter, volume, erythema index, and melanin index. Safety was evaluated by assessing reports of adverse effects from patients and physicians.
Results: All three treatment groups achieved resolution of inflammatory acne significantly faster than the control group, with median times for resolution of 4.6, 5.25, 6.7, and 8.1 days in the 1000DMNTA, 700DMNTA, 700DMN, and control, respectively. When compared to the control group, the diameters and post-acne erythema of inflammatory acne were significantly reduced in the treatment groups. The 1000DMNTA decreased acne size and erythema more than other treatments. DMNTA also tended to decrease acne size and erythema more than DMN with no TA, but there was no statistically significant difference. All participants preferred DMN over conventional intralesional steroid injection due to less pain and self-application. No adverse effect was observed.
Conclusion: DMNTA is a safe, effective alternative treatment for inflammatory acne and significantly reduces post-acne erythema.
Keywords: acne vulgaris, microneedle drug delivery, intralesional steroid, steroid injection, acne adjunctive treatment
Introduction
Acne is one of the most common skin diseases worldwide affecting quality of life.1 It mostly occurs during adolescence and can persist into adulthood with life-time prevalence of about 85%.1,2 Inflammatory acne is painful, uncomfortable, and unsightly; therefore, people seek a fast and effective treatment to accelerate the healing of these inflammatory lesions. Topical and oral medications are first-line treatments for acne.3–6 Unfortunately, these treatments are not effective in accelerating the resolution of inflammatory lesions once they occur. Intralesional steroid injection (ILS) has been commonly and widely used to treat inflammatory acne for many years.7,8 It is recommended as an adjunctive treatment for large cysts and nodules when systemic medications may not always be effective. Another popular usage of ILS is for inflammatory acne, which effectively reduces inflammation and accelerates resolution of inflammatory lesions.7 It is a way to directly access the lesion and cause dramatic flattening of most inflammatory acne.8 However, it must be performed by medical personnel and is less accepted by patients due to pain and needle phobia. Furthermore, ILS is an operator-dependent procedure that needs skilled personnel to deliver effective treatment, and side effects such as skin atrophy, hypopigmentation, and infection can occur after treatment.7–9
Various topical or transdermal delivery systems have been investigated for improving drug permeation through the skin.10 The stratum corneum, which generally allows penetration of only small (400 Da) and lipophilic molecules, is the major barrier to transdermal drug delivery.10,11 ILS, which uses a hypodermic needle, can bypass the stratum corneum and directly deposit the drug into the upper and deep dermis, where inflammatory acne lesions occur. Many drug delivery methods can enhance drug’s penetration through the stratum corneum, such as topical enhancers and transdermal patches, however, they cannot deliver drugs directly to the lesion in the dermis.
Microneedles are a transdermal drug delivery method that uses small needles with micron dimensions to pierce the skin and deliver drugs to the target area.10,12 Nowadays, there are different types of microneedles available for drug delivery, including solid, coated, dissolving, hollow, and hydrogel microneedles.10 Recently, detachable dissolvable microneedles, microneedles that can detach from the base and be deposited into the skin during the short application time, have also been introduced.13,14 The detachable dissolvable microneedles can be loaded to deliver drugs into the target area of the skin.
The advantage of DMN is that it can effectively deliver drugs directly to the dermis in a minimally invasive way and potentially be self-administered by the patient. DMN may be a good alternative to ILS for treating inflammatory acne lesions. Therefore, this study aimed to investigate the efficacy and safety of DMN and DMN-containing triamcinolone (TA) (DMNTA) compared to control for the treatment of inflammatory acne lesions and the prevention of post-acne erythema.
Materials and Methods
Study Design
This prospective, randomized, double-blinded, intraindividual, comparative study was conducted from October 2021 to August 2022, and was approved by the Human Research Ethics Committee of Srinakharinwirot University (SWUEC/F-488/2563) and was performed in compliance with the Declaration of Helsinki. The study was performed at the Skin Center, Srinakharinwirot University in accordance with relevant guidelines and regulations. The protocol was registered at Thai Clinical Trials Registry (registration number TCTR20211215006). All participants gave written informed consent before enrollment.
Participants
Participants were eligible if they were 18 years or older with mild to severe facial acne and were required to have at least four facial inflammatory papules or pustules. All participants agreed to participate in the trial and signed the informed consent form. Participants were allowed to continue using their usual routine of cosmetics, sunscreen, drinking the same amount of herbal tea, taking oral antibiotics, and taking oral isotretinoin in order to simulate the real-life scenario of an acne patch for inflammatory lesions. Other spot treatments for acne, concealers, new cosmetics, new cosmeceuticals, and new sunscreens are not allowed. Participants who had comedone extraction, ILS, used herbal supplements, or received any other sorts of facial laser and energy-based device treatments within two weeks of the trial’s start were disqualified. Participants with a history of dermatitis, photodermatitis, or skin infection on their face, and pregnant or lactating women were excluded. Four facial inflammatory acne lesions with similar morphology, height, and diameter were chosen by physicians and randomized to receive different treatments.
Detachable Microneedle Patches
The microneedles in this study (Figure 1) were 7.4×7.4 mm2 circular patches containing an array of 61 needles with a tetragonal pyramidal shape with square bases 700 µm or 1000 µm in height. Three types of DMNs were used in this study: 1) a 700 µm DMN containing 262.02 ± 15.62 µg of TA per patch (700DMNTA); 2) a 1000 µm DMNTA containing 160.00 ± 34.92 µg of TA per patch (1000DMNTA), and 3) a 700 µm DMN without TA (700DMN). Microneedle arrays were prepared via the molding method using sodium hyaluronate and sucrose as composite materials. DMNs contained sodium hyaluronate and sucrose. DMNTAs contain sodium hyaluronate, sucrose, and TA.
Randomization, Allocation, Concealment, and Interventions
A randomized list was generated prior to the intervention period using block randomization from the website randomization.com. The clinic staff who was not involved in recruitment, intervention, or assessment received the list and labeled the different DMN types in accordance with the randomization list before recruitment day. At the first study visit, four facial inflammatory acne lesions were chosen from each patient for intervention. Each lesion was labeled A-D from superior to inferior order or left to right side from the investigator’s perspective and received different microneedle interventions as described or a control as previously assigned through randomization. Microneedle patches (700DMNTA, 1000DMNTA, 700DMN) were randomly applied to three inflammatory acne lesions on the first visit and one was left untreated as a control. All participants cleaned their faces with cleanser (CeraVe Hydrating Facial Cleanser, L’Oreal (Thailand) Co., Ltd., Bangkok, Thailand) provided by the researcher before the application of microneedle patches. After cleaning the tested area with a 70% alcohol pad, the microneedle patch was applied to the selected inflammatory papule in a perpendicular direction. Then the area on top of the patch was rubbed using a saline-soaked pad for two minutes to allow the microneedles to detach and dissolve into the skin.
Efficacy Assessments
The primary outcome was time to resolution by physician grading, which was measured by a blinded dermatologist. Physician grading of inflammatory papules (Table 1) was described in 3 grades with 2 representing visible and palpable, 1 representing invisible but palpable, and 0 representing invisible and non-palpable. The time of resolution was determined when the lesion reached grade 0. Other efficacy outcomes consisted of acne diameter measured in millimeters by physicians using a Vernier caliper (ABSOLUTE Digimatic Caliper 500, Mitutoyo Corporation, Kanagawa, Japan). At each visit, the outcomes were measured with the same room and lighting conditions. All outcomes were measured at baseline and days 2, 3, 7, 14, and 28 of treatment.
 |
Table 1 Physician Grading |
Additionally, we evaluated the effect of DMN on post-acne erythema and hyperpigmentation. Erythema (a* value of CIEL*a*b*) and melanin index (L* value) were evaluated using a DSM III Colorimeter (Cortex Technology, Hadsund, Denmark) at baseline and 28 days of treatment. Patient and physician satisfaction were assessed at day 7 of treatment using a visual analog scale. Moreover, participants who had received ILS for treatment of inflammatory acne previously were asked for their preference.
Safety Assessments
Adverse events including skin irritation, pain, pruritus, skin infection, bruising, skin atrophy, skin hypopigmentation, and hyperpigmentation were recorded at each visit via clinical observation by physician and participant reports.
Statistical Analysis
To estimate the sample size, we assumed the median survival time on control treatment was equal to 6.3 days15 and treatment groups were 3 days with a type I error rate (alpha) of 5% and a type II error of 20% (power of 80%). The accrual time during which patients were recruited was 30 days and additional follow-up time after the end of recruitment was 28 days. A sample size of 29 patients was required (29 patients for each group), with 95% confidence and 80% power. The sample size was calculated using the Power and Sample Size Calculation (PS) program. With a dropout rate of 20%, a sample of 35 patients had to be recruited (35 patients in each group). Baseline characteristics of patients were described by treatment group using mean ± SD or median (interquartile range) for the continuous data and frequency and percentage for the categorical data. All patients were included in the analyses (intention-to-treat analysis). For continuous outcomes (such as diameter, volume, erythema index, and melanin index), multilevel data analysis (mixed linear model) was used to compare the difference between groups and the difference between baseline and days 2, 3, 7, 14, and 28. Resolution of acne was defined by invisible and non-palpable acne (physician grade 0). The estimated median time and rate of acne resolution were extracted from the Kaplan–Meier method in all groups. A p-value <0.05 was considered as statistically significant. Statistical analyses were performed with STATA version 14 (StataCorp, Texas, USA).
Results
Participant Demographic Data and Treatment History
Thirty-five participants with facial acne between 18 and 38 years with Fitzpatrick skin type III and IV were enrolled in this study. Two participants were missing at day 28 due to follow-up loss and COVID-19 infection (Figure 2). Twenty-seven participants were female (77.14%), and eight participants were male (22.86%). Most participants presented with mild to moderate acne, including 45.71% with mild acne, 48.57% with moderate acne, and 5.71% with severe acne. Acne types included 42.86% comedone, 91.43% papulopustular, and 2.86% nodulocystic acne. There were 94.29% of participants who had received prior acne treatment and 88.57% of patients had received ILS previously. Demographic data and treatment history are listed in Table 2.
 |
Table 2 Participant Demographic Data and Treatment History |
 |
Figure 2 CONSORT diagram. Screening, enrollment, and follow-up of study participants. |
Time to Resolution of Inflammatory Acne
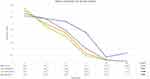
The primary outcome in this study was time to resolution of inflammatory acne by physician grading (Table 1). Table 3 demonstrates the number of participants who achieved resolution at each visit. In the 700DMNTA and 1000DMNTA groups, participants started to achieve resolution at day 2, while 700DMNTA and control groups started at day 3. Statistically significant differences were observed among the four groups at day 2, 3, and 7 of treatment with p-values of <0.001, 0.042, and 0.013, respectively (Table 3). The Kaplan–Meier curve showed all three groups had shorter resolution times than the control (Figure 3). The median time to resolution was 4.6, 5.25, 6.7, and 8.1 days in the 1000DMNTA, 700DMNTA, 700DMN, and control, respectively, from the Kaplan–Meier curve (Figure 3). At day 14 and 28, not all inflammatory lesions were resolved; however, all three-treatment groups demonstrated higher resolution of acne lesions than the control group despite lacking statistical significance (Table 3).
 |
Table 3 Number of Lesions That Achieved Resolution Each Follow-Up Day |
Diameter of Inflammatory Acne, Erythema, and Melanin Index
The diameter of inflammatory acne, measured by Vernier calipers, was significantly decreased in the three treatment groups (700DMNTA, 1000DMNTA, 700DMN) compared to the control group (p-values 0.001, <0.001 and 0.020, respectively; Figure 4). Erythema and melanin index were assessed by Colorimeter at day 1 and 28 to evaluate post-acne erythema and hyperpigmentation after inflammatory acne resolved. There was a significant difference in erythema in the three treatment groups compared to the control group (p-value of 0.004 in 700DMNTA, 0.003 in 1000DMNTA and <0.001 in 700DMN group; Figure 5). The melanin index at day 28 was worse compared to day 1 in all groups although not statistically different (Figure 5). The mean patient satisfaction by visual analog scale for 700DMNTA, 1000DMNTA, 700DMN, and the control were 9, 8.88, 8.52, and 7.44, respectively, while the corresponding values of physician satisfaction were 8.85, 8.94, 7.64, and 6.32, respectively. Both patient (p < 0.001 in 1000DMNTA and 700DMNTA, p = 0.001 in 700DMN) and physician satisfaction (p < 0.001 in all three treatments) were significantly higher than the control group. Regarding patient treatment preference, every participant who had experienced ILS for acne lesions preferred the use of microneedle patches over conventional needles. Clinical photographs of a representative case are shown in Figures 6 and 7.
Safety Outcome
We also evaluated side effects including irritation, dermatitis, pain, infection, bruising, skin atrophy, hyperpigmentation, and hypopigmentation. There were no reported side effects in this study.
Discussion
In our practice, ILS is often requested by patients with inflammatory papules because of its effectiveness in dramatically flattening inflammatory lesions within 48–72 hours,7–9 but there are very few studies that explore this treatment. In this study, we investigated the efficacy of DMN as a drug delivery method as an alternative to ILS. Our study is the first to evaluate the safety and efficacy of microneedle patches containing TA in the treatment of inflammatory acne. This study revealed that DMNs were effective in reducing the size and post-acne redness of inflammatory acne. Our primary outcome, median time to resolution of acne, showed a faster time to resolution in all three treatment groups compared to the control. Participants started to achieve resolution at day 2 of treatment in the 700DMNTA and 1000DMNTA groups, similar to that of ILS. All three DMN treatments showed significantly faster times to resolution of inflammatory acne compared to the control. The survival curve (Figure 3) shows that given 1000DMNTA, 700DMNTA, and 700DMN, the median time to resolution was 4.6 days, 5.25 days, and 6.7 days, respectively. The timeframes are quicker than the median time to resolution of 8.1 days for the control.
Facial skin thickness manifested in variable ranges: epidermis (110–135µm) and dermis (1600–2500 µm).16,17 The depth of 90% adnexal structures which were previously reported are about 386–1321µm.17 Acne is a skin disease of pilosebaceous units that involves both sebaceous glands and hair follicles. Hence, we selected the depth of DMNs at 700µm and 1000µm to target the inflammatory pilosebaceous units.
In DMN treatments containing TA, 1000DMNTA tended to be more effective than 700DMNTA, despite 1000DMNTA having a lower amount of TA (160 µg/patch vs 262 µg/patch in 700DMNTA). Therefore, this emphasizes that a low dose of TA is enough for the treatment of inflammatory papules. This is consistent with the findings of Levine and Rasmussen8 who conducted a study to determine the lowest intralesional TA and betamethasone dose for cystic acne treatment. The study reported that TA at a concentration of 0.63, 1.25, and 2.5 mg/mL had similar efficacy as intralesional injections for cystic acne. Moreover, in clinical practice, where a TA concentration of 2.5 mg/mL is usually administered in small injection amounts (approximately 0.05 mL), the amount of TA injected in each lesion is about 125 µg. Therefore, from our findings, when using DMN as a drug delivery system, a TA dose of 160 µg/patch or lower is suggested. However, the depth of the microneedle might be a more important factor in delivering drugs into inflammatory lesions that rise and swell.
In our study, the 700DMN, which did not contain TA, also improved inflammatory acne. This is likely because microneedles that puncture the lesion subsequently help the drainage of pus or other contents from the lesion. Therefore, a shortened resolution time of the inflammatory papules and pustules was observed.
Interestingly, all DMN treatments can significantly reduce post-acne erythema when compared to no treatment. Post-acne erythema is a common sequelae of acne after inflammatory lesions, causing psychological distress and frustration in many patients.18–20 In this study, we observed the positive effect of DMN on post-acne erythema. Even 700DMN that does not contain steroids demonstrated efficacy in decreasing post-acne erythema. This effect may be explained by DMN, which hastens the time of resolution and results in a shorter inflammatory duration and less erythema in the area. We do not believe that this result was due to the prolonged effect of steroids since we only applied a single application of DMN in our study. Nevertheless, post-inflammatory hyperpigmentation represented by the melanin index was not significantly different after DMN treatment at day 28. This is possibly because the post-acne erythema was still more prominent than hyperpigmentation during that follow-up period. Therefore, the effect of DMN on post-inflammatory hyperpigmentation cannot yet be determined, and further studies with longer follow-ups should be performed to explore this issue.
Regarding safety, both higher (262 µg/patch) and lower (160 µg/patch) TA doses had no adverse effects. The major concerns of administering DMN containing steroids directly to the skin are atrophy and hypopigmentation. These side effects did not occur from treatment day until the end of the follow-up period of 1 month, which is within the period that atrophy and hypopigmentation usually occur in our experience after ILS (3–4 weeks after ILS). Therefore, a single application of DMN containing TA with a dose of up to 262 µg/patch is safe for acne treatment.
Another major advantage of using DMN instead of ILS is the self-application of the patch, which does not require skilled medical personnel to be present. In our study, we asked for the preference between DMN and ILS in participants who had experienced ILS for the treatment of inflammatory acne previously. All patients preferred the use of microneedle patches over conventional needles for the treatment of inflammatory acne because it was less painful and could be self-applied.
Limitations of this study include that the frequency of follow-up in the first week was limited due to the restrictions caused by the COVID-19 pandemic policy. Additionally, most inflammatory lesions in this study were inflammatory papules and pustules since it is difficult to identify participants with four similar nodules or cystic lesions at a single time period. For further study, the frequency of follow-up should be increased in the first week after treatment and a longer follow-up period may allow for the detection of unexpected side effects of DMN. In addition, the lowest effective concentration of DMN containing TA and multiple repeated applications of DMN can be explored for safety and efficacy. Finally, randomized controlled trial comparing DMN containing TA and ILS is recommended to compare the efficacy of these two treatments for inflammatory acne.
Conclusion
DMNTA is effective in accelerating the resolution of inflammatory acne and reducing post-acne erythema. It is safe and no adverse effects were reported; thus, it could be considered an alternative treatment for inflammatory acne.
Data Sharing Statement
The data of this study are available on request from the corresponding author, SR. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Ethics Approval
This study was approved by the Human Research Ethics Committee of Srinakharinwirot University (SWUEC/F-488/2563) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Funding
This work was supported by the Faculty of Medicine and HRH Princess Maha Chakri Sirindhorn Medical Center, Srinakharinwirot University under grant number 159/2565.
Disclosure
Professor Supason Wanichwecharungruang reports a patent PCT/TH2019/000031 licensed to Mineed technology. The authors report no other conflicts of interest in this work.
References
1. Wisuthsarewong W, Nitiyarom R, Kanchanapenkul D, Arunkajohnask S, Limphoka P, Boonchai W. Acne beliefs, treatment-seeking behaviors, information media usage, and impact on daily living activities of Thai acne patients. J Cosmet Dermatol. 2020;19(5):1191–1195. doi:10.1111/jocd.13132
2. Tan AU, Schlosser BJ, Paller AS. A review of diagnosis and treatment of acne in adult female patients. Int J Womens Dermatol. 2018;4(2):56–71. doi:10.1016/j.ijwd.2017.10.006
3. Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945–73 e33. doi:10.1016/j.jaad.2015.12.037
4. Thiboutot DM, Dreno B, Abanmi A, et al. Practical management of acne for clinicians: an international consensus from the Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2018;78(2 Suppl):S1–S23 e1. doi:10.1016/j.jaad.2017.09.078
5. Hauk L. Acne Vulgaris: treatment guidelines from the AAD. Am Fam Physician. 2017;95(11):740–741.
6. Goh CL, Abad-Casintahan F, Aw DC, et al. South-East Asia study alliance guidelines on the management of acne vulgaris in South-East Asian patients. J Dermatol. 2015;42(10):945–953. doi:10.1111/1346-8138.12993
7. National Guideline Alliance (UK) (NICE Guideline, No 198). Intralesional corticosteroids for the treatment of individual acne vulgaris lesions: acne vulgaris: management: evidence review K; 2021.
8. Levine RM, Rasmussen JE. Intralesional corticosteroids in the treatment of nodulocystic acne. Arch Dermatol. 1983;119(6):480–481. doi:10.1001/archderm.1983.01650300034012
9. Gallagher T, Taliercio M, Nia JK, Hashim PW, Zeichner JA. Dermatologist use of intralesional triamcinolone in the treatment of acne. J Clin Aesthet Dermatol. 2020;13(12):41–43.
10. Waghule T, Singhvi G, Dubey SK, et al. Microneedles: a smart approach and increasing potential for transdermal drug delivery system. Biomed Pharmacother. 2019;109:1249–1258. doi:10.1016/j.biopha.2018.10.078
11. Park JH, Allen MG, Prausnitz MR. Biodegradable polymer microneedles: fabrication, mechanics and transdermal drug delivery. J Control Release. 2005;104(1):51–66. doi:10.1016/j.jconrel.2005.02.002
12. Henry S, McAllister DV, Allen MG, Prausnitz MR. Microfabricated microneedles: a novel approach to transdermal drug delivery. J Pharm Sci. 1998;87(8):922–925. doi:10.1021/js980042
13. Sawutdeechaikul P, Kanokrungsee S, Sahaspot T, et al. Detachable dissolvable microneedles: intra-epidermal and intradermal diffusion, effect on skin surface, and application in hyperpigmentation treatment. Sci Rep. 2021;11(1):24114. doi:10.1038/s41598-021-03503-5
14. Toprangkobsin P, Banlunara W, Limcharoen B, et al. Delivery and diffusion of retinal in dermis and epidermis through the combination of prodrug nanoparticles and detachable dissolvable microneedles. Drug Deliv Transl Res. 2022;12(11):2751–2761. doi:10.1007/s13346-022-01136-3
15. Bruce S, Conrad C, Peterson R, et al. Significant efficacy and safety of low level intermittent heat in patients with mild to moderate Acne; 2008:3–9. Available from: http://www.myzenoeurope.com/doc/zenowhite.pdf.
16. Wang S, Yu RX, Fan W, et al. Detection of skin thickness and density in healthy Chinese people by using high-frequency ultrasound. Skin Res Technol. 2022. doi:10.1111/srt.13219
17. Sasaki GH, Travis HM, Tucker B. Fractional CO2 laser resurfacing of photoaged facial and non-facial skin: histologic and clinical results and side effects. J Cosmet Laser Ther. 2009;11(4):190–201. doi:10.3109/14764170903356465
18. Kalantari Y, Dadkhahfar S, Etesami I. Post-acne erythema treatment: a systematic review of the literature. J Cosmet Dermatol. 2022;21(4):1379–1392. doi:10.1111/jocd.14804
19. Chalermsuwiwattanakan N, Rojhirunsakool S, Kamanamool N, Kanokrungsee S, Udompataikul M. The comparative study of efficacy between 1064-nm long-pulsed Nd:YAG laser and 595-nm pulsed dye laser for the treatment of acne vulgaris. J Cosmet Dermatol. 2021;20(7):2108–2115. doi:10.1111/jocd.13832
20. Agamia N, El-Nagdy S, El-Ariny A. A split face comparative study using a novel triple combination therapy for the treatment of persistent post acne erythema. Dermatol Ther. 2022;35(4):e15327. doi:10.1111/dth.15327
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.