Back to Journals » Risk Management and Healthcare Policy » Volume 16
Effects of the Novel Coronavirus Pandemic on the Identification and Care of Critically Ill Emergency Patients Not Infected with COVID-19
Authors Zhu MY, Li R, Xu J, She F, Du X, Zhang W
Received 29 August 2023
Accepted for publication 10 November 2023
Published 4 December 2023 Volume 2023:16 Pages 2661—2672
DOI https://doi.org/10.2147/RMHP.S437690
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Ming-Yue Zhu,* Rong Li,* Jie Xu, Fei She, Xin Du, Wei Zhang
Department of Emergency Medicine, the Fourth Medical Center, Chinese PLA General Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wei Zhang, Department of Emergency Medicine, the Fourth Medical Center, Chinese PLA General Hospital, No. 51 Fucheng Road, Haidian District, Beijing, 100048, People’s Republic of China, Tel +86 010-66867373, Email [email protected]
Objective: To clarify variations of diagnosis and treatment in the emergency care of critically ill patients not infected with novel coronavirus (COVID-19) prior to and amidst the COVID-19 pandemic.
Methods: A retrospective cohort study was conducted to compare and analyze the diagnosis and treatment data of critically ill patients with non-COVID-19 infection who were admitted to the emergency department of the Fourth Medical Center of Chinese PLA General Hospital from January 2019 to November 2022. The variations in emergency care of the pandemic were summarized, and the influence of the pandemic on emergency care was assessed.
Results: A total of 6634 critically ill patients with non-COVID-19 infection were included in this study. These patients were elderly, high incidence of chronic diseases, and extended emergency duration during the pandemic. Notably, the proportion of patients requiring intensive care was twofold higher compared to the period before the pandemic. Throughout the pandemic, patients experienced prolonged emergency durations, increased overall costs and daily expenses per patient. Further investigation revealed that elderly patients exhibited worse medical conditions, requiring lengthier emergency treatment and incurring escalated healthcare expenses. However, the presence of pre-existing chronic diseases did not appear to influence disease severity, nor extended emergency durations or heightened healthcare expenditures. Irrespective of the pandemic phase—be it short-term, medium-term, or long-term emergency care—greater healthcare spending was necessary.
Conclusion: There was no difference in the disease spectrum of emergency critical ill patients with non-COVID-19 infection prior to and amidst the COVID-19 pandemic, nor the duration and expenditure in prior chronic illness patients. However, the disease severity and emergency duration have led to an increase in the total cost and economic intensity of emergency care for all patients during the epidemic. Especially, elderly patients required longer emergency duration, greater healthcare spending, and more inpatient medical resources than usual.
Keywords: novel coronavirus epidemic, emergency, elderly
Introduction
The global outbreak of COVID-19, caused by the coronavirus-2019, emerged at the close of 2019, presenting a severe public health crisis for humanity.1 China responded with a strategy involving social measures, targeted identification, and treatment of suspected and confirmed cases to safeguard people’s well-being.2 Managing individuals with COVID-19 required substantial medical resources and efficient diagnostic and treatment services, leading to an increased burden on healthcare expenses.3 Concurrently, routine medical procedures for patients not infected with COVID-19 during the pandemic were influenced by policies and preventive measures.4 The medical landscape underwent substantial changes, with a marked deviation from the pre-pandemic approach. Examining how patients were managed throughout the pandemic is crucial for assessing shortcomings and guiding post-pandemic improvements in healthcare. Our hospital, as a facility specializing in non-COVID-19 cases, continued regular medical operations from late 2019 to November 2022. To comprehend the impact of the pandemic on critically ill patients not infected with non-COVID-19 and requiring urgent care, we collected diagnostic and treatment data of such patients who were admitted in our hospital between January 2019 and November 2022. A comparative analysis was performed between the period before the COVID-19 outbreak (entirety of 2019) and the pandemic phase (January 2020 to November 2022) to discern differences.
Materials and Methods
Research Material
We consistently gathered diagnostic and therapeutic information of severely ill patients who underwent medical care at the emergency ward of the Fourth Medical Center within the Chinese PLA General Hospital. The data collection spanned from January 2019 to November 2022, encompassing 2164 emergency medical visits during 2019 alone, and an overall count of 4470 emergency visits from January 2020 to November 2022.
Inclusion Criteria
- Patients classified as critically ill who fulfilled the emergency treatment criteria and treatment guidelines.5
- Individuals aged above 14 years. A parent or legal guardian of patients under 18 years of age provided informed consent.
- As the diagnosis and treatment approach for extremely elderly patients during emergency procedures exhibited significant variations, patients aged ≤ 95 years were included.
Exclusion Criteria
- Absence of emergency medical records.
- Insufficient diagnostic information.
- Lack of emergency nursing records and associated treatment documentation.
- Patients who exited the emergency treatment area without initiating treatment subsequent to the initial evaluation of their condition.
Research Methods
Retrospective methods were used to gather demographic, diagnostic, and treatment information of the selected patients. This included details such as gender, age when diagnosed, specific disease type, prior chronic illness history, duration of diagnosis and treatment, status post emergency care, overall patient expenditure, and daily patient spending. Notably, the emergency conditions were categorized into 10 groups based on criteria such as respiratory issues, nervous system disorders, circulatory system problems, digestive system ailments, urinary system malfunctions, endocrine and metabolic dysfunctions, injuries, poisonings, infections, fever, malignant tumors, and other complications. A chronic ailment was defined as having one or more of the subsequent conditions: hypertension, coronary heart disease, diabetes, chronic obstructive pneumonia, bronchial asthma, aftermath of a cerebrovascular accident, Alzheimer’s disease, and Parkinson’s disease. The objective was to assess how the pandemic affected the diagnosis and treatment of critically ill emergency patients by comparing 2019 patient data with pandemic-phase data. To explore the influence of age on diagnosis and treatment, ages were grouped into 8 categories spanning 10 years each. Patient status post emergency care was categorized as “discharged”, “general ward admission”, “intensive care unit admission”, and “death”, providing a measure of disease severity. The severity levels were defined as “low-risk”, “medium-risk”, “high-risk”, and “death”, denoted by numbers 1 to 4. The majority of emergency cases underwent treatment, which was usually of short duration. To evaluate the connection between treatment duration and healthcare spending, six time frames were used: short-term (1–4 days), medium-term (about a week, 5–9 days), and long-term (10 days and more).
Statistical Methods
The data concerning diagnosis and treatment prior to the pandemic served as a baseline. A comparison and analysis were conducted on the disparities in the diagnosis and treatment data for critically ill patients in emergency situations during the pandemic. Furthermore, the impact of population informatics data on diagnosis and treatment was explored. Statistical analysis was carried out using SPSS 20.0 software. The data on age when diagnosed, duration of diagnosis and treatment, overall patient expenditure, and daily patient spending conform to a normal distribution underwent t-test. Chi-square test was used for data on gender and prior chronic illness history. Rank-sum test was used to the data on status post emergency care and specific disease type. To elucidate the interplay of various factors, multivariate analysis of variance was employed. A significance level of p < 0.05 was adopted for statistical inference.
Results
Comparison of Data Before and During the Pandemic
Comparing the data for emergency care prior to and during the pandemic reveals that there were no statistically significant differences between the two periods concerning gender (p = 0.087) and the type of disease (p = 0.124). However, substantial disparities were observed in terms of age, presence of chronic medical conditions, duration of diagnosis and treatment, status post emergency care, total expenses per patient, and daily expenses per patient (Table 1). Notably, during the pandemic, critically ill emergency patients were generally the elderly, with a higher prevalence of patients having a history of chronic diseases. Additionally, there was a decline in the number of patients being discharged after emergency treatment (with discharge rates dropping from 54.48% to 39.57% during the pandemic). Conversely, there was an increase in the proportion of patients being hospitalized, particularly a marked rise in critically ill patients (ICU admissions increased from 13.64% before the pandemic to 21.25% during the pandemic). The healthcare expenses exhibited an escalation both in terms of time and financial intensity. The aforementioned findings indicated that during the pandemic, younger patients tended to go back home after receiving emergency medical treatment, while elderly patients with pre-existing chronic conditions required more extended medical care. Throughout the pandemic timeframe, irrespective of patient age or chronic ailment history, critically ill individuals not infected with COVID-19 displayed graver conditions, necessitating prolonged emergency assessment and treatment periods. This led to an escalation in healthcare costs per patient and overall health expenditure intensity. Patient age and chronic ailment history serve as fundamental factors that likely influence emergency medical processes. For instance, advanced patient age correlates with extended diagnosis and treatment durations, potentially consuming more medical resources. Moreover, a possible association exists between chronic ailment history and age; notably, patients with chronic conditions in this study had a significantly higher average age (73.68 years old) compared to those without chronic conditions (average age of 53.43 years old), denoted by a statistical significance (p < 0.01). The impact of patient age, chronic ailment history, and disease severity on the duration of emergency care, status post emergency care, and medical expenditure requires further examination.
 |
Table 1 Comparison of Emergency Data of Patients with Non-COVID-19 Infection Prior to and Amidst the Pandemic |
Influence of Age and Chronic Disease History on the Status Post Emergency Care
The age category was split into 8 intervals, with each interval representing a span of 10 years. The patient status classification consists of four levels based on the following criteria: “discharge”, “admission to a general ward”, “admission to an intensive care unit”, and “death”. A comparison was conducted between the data from before and during the pandemic across the different age intervals to determine whether any statistical distinctions existed between the two periods (Table 2). Throughout the pandemic phase, patients of all age groups experienced a worsening of their conditions, with individuals aged 35 and above exhibiting a statistically significant difference in the severity of aggravation (p < 0.01). But there was no difference in the severity of the disease of young patients under 35 years old.
 |
Table 2 Comparison of Status Post Emergency Care in Different Age Groups |
The potential connection between a patient’s medical history of chronic illnesses and their status post emergency care was examined using chi-square test (Table 3). The impact of prior chronic illness history on status post emergency care were observed solely among patients who were discharged (p = 0.026) or those admitted to the intensive care unit (p = 0.004). Particularly noteworthy was the marked rise (70% increase) in the percentage of patients with a history of chronic ailments in the intensive care unit.
 |
Table 3 The Impact of Prior Chronic Illness History on Status Post Emergency Care |
The results of a multivariate analysis of variance indicated that age significantly influenced the status post emergency care (p < 0.01). In contrast, the presence of chronic illness history did not have a significant impact on the status post emergency care (p = 0.219). This discrepancy may be attributed to the fact that patients with a history of chronic illnesses generally tended to be older, which indirectly affected their status post emergency care.
Influence of Age, Chronic Disease History, and Disease Severity on the Duration of Emergency Care
Likewise, the contrast in the timeframe of emergency medical care before and during the pandemic was assessed across various age groups. Additionally, the difference in the duration of emergency medical care prior to and during the pandemic was analyzed based on the status post emergency care, considering the disease severity (Table 4). Comparing the pandemic period to the pre-pandemic phase, patients aged 65 and older encountered significantly lengthened emergency care times, whereas those below 25 years old experienced considerably shorter durations (p = 0.023). Furthermore, the duration of emergency treatment for discharged patients during the pandemic was notably lengthier compared to prior to the pandemic (with an average increase of 0.87 days during the pandemic, p < 0.01).
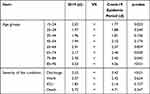 |
Table 4 Impact of Age Groups and Severity of the Condition on Duration of Diagnosis and Treatment |
The duration for emergency care throughout the pandemic was notably prolonged, irrespective of whether patients had a history of chronic conditions (Figure 1). Patients with a history of chronic ailments experienced an average prolongation of approximately 0.43 days in the duration of emergency care (p = 0.003), while patients without such medical history saw an average extension of 0.16 days (p = 0.047).
 |
Figure 1 The impact of prior chronic illness history on duration of diagnosis and treatment prior to and amidst the COVID-19 pandemic. |
A multivariate analysis of variance revealed that the presence of chronic diseases did not impact the duration of emergency treatment (p = 0.275), whereas age and disease severity demonstrated significant effects on emergency care duration (p < 0.01).
Influence of Age, Chronic Disease History, Disease Severity, and Duration of Emergency Care on the Daily Expenditure per Patient
The daily expenses incurred per patient is indicative of the daily expenses associated with the diagnosis and treatment of each patient. This metric provides insight into the daily healthcare expenses borne by patients. Higher daily expense per patient signifies greater health expenditure for patients. Irrespective of whether patients had prior chronic illnesses, the daily expenses per patient in the emergency department saw an escalation during the pandemic. (Figure 2). During the pandemic, patients with a pre-existing chronic ailment experienced a rise of RMB 362.90 in their average daily expenses (significant at p < 0.01), while emergency patients without a history of chronic diseases encountered an average daily expense increase of RMB 328.14 (also significant at p < 0.01). We examined the effects of various factors like age, disease severity, and the duration of care on the daily expenses incurred by patients (Table 5). The primary focus of our analysis was on the daily expenses of patients who underwent short-term, medium-term, and long-term care in the emergency department, comparing the pre-pandemic period with the pandemic period. The findings revealed that the daily expenses for patients receiving different durations of care were higher during the pandemic, indicating an overall rise in healthcare expenses for critically ill patients in the emergency department. Notably, patients aged 55 and above experienced a significant increase in their daily expenses during the pandemic. Although patients with various health conditions saw increased expenses during the pandemic, only discharged and deceased patients displayed significant differences in their expenses.
 |
Table 5 Impact of Age Groups, Severity of the Condition, and Duration of Diagnosis and Treatment on Daily Patient Spending |
 |
Figure 2 The impact of prior chronic illness history on daily patient spending prior to and amidst the COVID-19 pandemic. |
The results of multivariate analysis of variance indicated that age (p = 0.152) and the presence of chronic illnesses (p = 0.378) did not influence the daily expense per patient. However, disease severity (p < 0.01) and the duration of diagnosis and therapy (p < 0.01) significantly impacted the daily expense per patient.
Discussion
COVID-19, also known as the Coronavirus-2019, marked a significant global health crisis in the 21st century.6 Its rapid emergence was witnessed as it swiftly spread through China within a month,7 subsequently becoming a global pandemic within three months.8 This virus exhibited notable attributes, including its high transmissibility, considerable pathogenicity, and elevated mortality rates.9 This prompted the World Health Organization (WHO) to take substantial notice,10 officially designating it as COVID-1911 and urging worldwide collaborative efforts to combat its impact.12 Primarily affecting the respiratory system, COVID-19 led to critical respiratory failure post-infection.13 As the pandemic progressed, it inflicted harm upon various bodily systems such as the respiratory, nervous, circulatory, digestive, and urinary systems,14,15 resulting in multi-organ failure.14,16 Consequently, the number of critically ill patients surged, leading to heightened healthcare expenditures, particularly in terms of ventilator demand.17
Research has consistently demonstrated that elderly individuals and those with pre-existing conditions such as hypertension, cardiovascular ailments, cerebrovascular diseases, diabetes, and chronic lung disorders faced a greater likelihood of severe illness, heightened complications, increased mortality risk, and unfavorable post-infection prognoses due to the novel coronavirus.3,16,18,19 This trend contributed to elevated rates of severity, mortality, and medical resource consumption among elderly patients with a history of chronic ailments.20 Following the emergence of the COVID-19 pandemic, China implemented a strategy centered on societal measures to prevent the spread of the virus. This approach involved targeted identification and treatment of individuals suspected or confirmed to have the virus. They undertook a three-pronged approach to control the outbreak: managing the sources of infection, obstructing transmission pathways, and safeguarding those who were most susceptible.7
The Chinese government enacted a set of policies to regulate the situation. These measures encompassed early detection, swift diagnosis, prompt reporting, immediate isolation, timely treatment, reduction of social interactions, cancellation of gatherings, postponement of work resumption, and localized treatment efforts.7 Throughout this period, uninfected residents, community healthcare facilities, and designated quarantine hospitals played a pivotal role in managing the spread of COVID-19. Consequently, they effectively contained the extensive outbreak of the pandemic within China.21
Individuals who remained uninfected during the pandemic were actively engaged as the primary population for successful pandemic control.7,21,22 Their significant contributions were integral to the battle for medical and public health. Over the course of the three-year struggle against COVID-19,23 those who remained uninfected spent as much on maintaining their health as those who contracted the virus. Therefore, it is imperative to comprehensively examine the healthcare status of this demographic. Such analysis can guide the development of more scientific approaches for addressing potential future health crises, while also addressing existing gaps in the current medical treatment processes.
The management of individuals afflicted by COVID-19 necessitates specific treatment protocols24 along with rigorous disinfection and sterilization measures.25 Employing fixed-point treatment and control can effectively contain the source of infection. Although our hospital was not initially designated for treating COVID-19 cases during the pandemic response, it assumed responsibilities for screening, daily diagnosis, and treatment of such cases. Over a span of three years, our hospital’s emergency department accumulated a substantial volume of real-world data pertaining to the diagnosis and treatment of non-COVID-19 cases. Notable differences exist in this emergency care data when comparing the period before and after the pandemic outbreak. In contrast to the emergency care data for the entire year of 2019, no statistically significant distinctions were evident in terms of patient gender (p = 0.087) or disease types (p = 0.124) during the pandemic. This indicates that gender distribution among critically ill patients and the spectrum of diseases remained largely unchanged throughout the pandemic.26
Patients seeking medical attention before and during the pandemic were drawn from the same population pool in terms of disease origin and gender. Nevertheless, noteworthy disparities surfaced between these two groups in relation to age, presence of chronic medical history, treatment duration, post-treatment status, total patient expenditure, and daily patient expenses. Age and chronic medical history represented fundamental patient attributes. Critically ill patients during the pandemic exhibited an average age 1.37 years higher than their pre-pandemic counterparts (p < 0.01), with a 5.86% increase in the proportion of patients with a history of chronic diseases (p < 0.01). In accordance with survivor bias theory, this difference may be attributed to younger patients and those lacking chronic medical history being less inclined to seek emergency medical aid. The average duration of emergency treatment during the pandemic witnessed an extension of 0.37 days (p < 0.01). Post-treatment, the percentage of hospitalized patients rose by 12.78%, the proportion of patients requiring intensive care doubled, and the fatality rate increased by a factor of 1.72 compared to the period before the pandemic. The epidemic resulted in a notable rise in medical support required for patients not infected with COVID-19, particularly in critical care scenarios. Analyzing healthcare expenses before and following the pandemic, a significant difference was discovered. The overall healthcare expenses of patients during the pandemic surpassed pre-pandemic levels by RMB 2,031.14 per patient, with a daily increase of RMB 336.3 per patient. This illustrates that the pandemic elevated the emergency healthcare costs for non-COVID-19 patients, both in terms of total expenses and daily expenses. Distinct variations exist in medical and health regulations,21 public sentiment alignment,27 and medical care protocols22 before and after the pandemic. These variations could serve as the primary factors contributing to differences in the duration of emergency medical care, the status post emergency care, and healthcare expenditures. Nevertheless, disparities in age and previous chronic disease records were also evident. To ascertain whether age and medical history of chronic disease exert an influence on the duration of diagnosis and treatment, the status post emergency care, and healthcare expenses, a more in-depth internal comparative analysis is warranted. The medical history of chronic conditions significantly influences the treatment and outlook for individuals who contract a COVID-19 infection. According to a study by Jessica et al, patients with chronic respiratory issues (such as asthma and chronic obstructive pulmonary disease) face an elevated risk of COVID-19 infection and generally experience poorer outcomes.18,28 Investigations carried out by the Saudi Arabian Ministry of Health have identified that conditions like diabetes, hypertension, chronic heart diseases, asthma, and chronic obstructive pulmonary disease heighten the likelihood of hospitalization and lead to extended stays in intensive care units.29,30 Additional research has corroborated the negative consequences of pre-existing chronic illnesses on COVID-19 patients,31 particularly noting the unfavorable prognosis for individuals with both diabetes and COVID-19.32 The research also found that regardless of the presence of chronic conditions, there was an increase in the duration of emergency treatment and daily expenses per patient. Notably, statistical analysis considering multiple factors indicated that a history of chronic diseases did not impact the status of post emergency care (p = 0.219), treatment duration (p = 0.275), or daily expenses per patient (p = 0.659). Throughout the pandemic, the history of chronic diseases did not significantly influence the standard diagnosis and treatment of emergency patients. The research by Halpin also suggested that consistent management of chronic respiratory diseases may correlate with a reduced incidence of COVID-19,21 though this perspective might overlook the preventive benefits of measures like mask-wearing against viruses, bacteria, and harmful particles during the pandemic.33 In investigations pertaining to individuals afflicted by COVID-19 infection, the elderly patient demographic displayed elevated rates of both morbidity and mortality.34,35 Initial examinations conducted during the early phase of the COVID-19 outbreak revealed that among all age brackets, the mortality rate was most pronounced among elderly patients.7 The study by Rupak et al, found that COVID-19-infected patients over the age of 50 exhibited a heightened incidence of shock and an escalation in healthcare expenses.3 Increased incidence of adverse outcomes and fatalities among elderly hospitalized patients due to increased vulnerability and advanced age threatens standard diagnosis and treatment of elderly patients not infected with COVID-19 and may delay therapeutic interventions. Consequently, when medical intervention becomes imperative, the urgency and severity of the patient’s condition are often exacerbated, leading to an elevation in hospitalization rates and mortality rates among critically ill patients. In the data analysis in this study, the proportion of critically ill non-COVID-19 patients aged ≥ 35 years who were successfully discharged witnessed a marked reduction, whereas the proportion of such patients requiring hospitalization or emergency care exhibited a substantial increase. In evaluating the influence of age on the duration of emergency care, the average duration of emergency care for patients aged < 25 was reduced by 0.25 days (p = 0.023), and there was no notable rise in daily per-patient expenses (p = 0.327). Conversely, the average duration of emergency care for elderly patients aged ≥ 65 experienced an extension by 0.29 to 1.03 days during the pandemic, concomitantly leading to augmented daily per-patient expenses for the elderly demographic (aged ≥ 55 years) during the COVID-19 pandemic (p < 0.01). This underscores that critically ill patients of younger age were less inclined to endure prolonged stays in the emergency department during the pandemic, with their diagnostic and treatment processes not inducing heightened expenditures on emergency healthcare. In contrast, the emergency care of elderly patients during the pandemic not only demanded more time and financial resources but also necessitated increased reliance on post-emergency medical support. The patient’s discharge, entry into either the regular hospital ward or the intensive care unit, or death, all provide some insight into the severity of the patient’s condition. Analysis of the data indicated that, during the pandemic, the typical duration of emergency medical care for discharged patients saw an increase of 0.87 days (p < 0.01). This could potentially be attributed to enhanced hospital assessments and societal oversight throughout the pandemic.36 Within this same pandemic period, the daily expenses for each critically ill patient rose; however, only the difference in expenses between those who were discharged and those who died held statistical significance. By examining healthcare expenditure concerning the duration of emergency care, it becomes evident that there was a noteworthy increase in daily expenses per patient during the pandemic period, regardless of whether the medical attention was required for a brief, moderate, or extended duration. An analysis considering multiple variables also validated that the duration of diagnosis and treatment significantly influenced the intensity of healthcare spending (p < 0.01). This suggests that throughout the pandemic, all types of emergency medical care, be it short-term, medium-term, or long-term, necessitated higher healthcare expenditure. The heightened healthcare expenses could potentially be attributed to activities like the screening for novel coronaviruses or the inappropriate use of antibiotics in the context of the COVID-19 pandemic.20,37,38 To enhance the emergency care process during the pandemic, it is important to avoid unnecessary screenings and the excessive use of antibiotics driven by panic.
This research comprises a retrospective cohort study conducted at a single medical center, without the inclusion of extensive statistical outcomes from multiple centers and a large participant pool. The findings from this study are valuable in presenting an overview of standard emergency care trends throughout the pandemic timeframe. The study also involves an analysis of the attributes associated with emergency diagnosis, treatment patterns, and healthcare expenditure during the pandemic. These outcomes serve as a valuable dataset for potential future pandemics.
Conclusion
There was no difference in the disease spectrum of emergency critical ill patients with non-COVID-19 infection between the periods of pandemic and 2019 year. The presence of chronic diseases among patients during the pandemic did not influence the standard care provided to critically ill emergency cases. During the pandemic, elderly individuals had a higher prevalence of chronic diseases, experienced more severe conditions, lengthier periods of diagnosis and treatment, and subsequently, higher utilization of healthcare resources. This had a notable impact on health expenses and the overall economy, necessitating additional resources for post-emergency medical care. But younger patients displayed a willingness to reduce the duration of their emergency treatments, without causing a surge in healthcare spending. Throughout the pandemic, regardless of the duration of emergency treatment—be it short-term, medium-term, or long-term—there was an elevated requirement for healthcare spending.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki.This study was conducted with approval from the Ethics Committee of the Fourth Medical Center, Chinese PLA General Hospital.A written informed consent was obtained from all participants.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. PMID: 31986257; PMCID: PMC7135038. doi:10.1016/S0140-6736(20)30185-9
2. Feng ZH, Cheng YR, Chen J, Ye L, Zhou MY, Wang MW. Chinese medical personnel against the 2019-nCoV. J Infect. 2020;80(5):578–606. PMCID: PMC7126162. doi:10.1016/j.jinf.2020.02.011
3. Desai R, Singh S, Parekh T, et al. COVID-19 and shock: a cautionary tale for elderly patients from a pooled analysis. Ann Emerg Med. 2020;75(6):789–791. PMCID: PMC7151519. doi:10.1016/j.annemergmed.2020.04.014
4. Sima YJ. White paper on China’s Actions to combat COVID-19 [EB/ OL]. Beijing: Website of The State Council Information Office of the People’s Republic of China; 2020. Available from: http://www.scio.gov.cn/zfbps/32832/Document/.
5. Expert Consensus group on emergency pre-screening triage. Expert consensus on emergency predetection and triage. Chinese Journal of Emergency Medicine. 2018;27(6):599–604. 10.3760/cma.j.issn.1671-0282.2018.06.006
6. Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. PMID: 32015508; PMCID: PMC7094943. doi:10.1038/s41586-020-2008-3
7. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) - China, 2020. China CDC Wkly. 2020;2(8):113–122. PMID: 34594836; PMCID: PMC8392929. doi:10.46234/ccdcw2020.032
8. Steffens I. A hundred days into the coronavirus disease (COVID-19) pandemic. Euro Surveill. 2020;25(14):2000550. PMID: 32290905; PMCID: PMC7160442. doi:10.2807/1560-7917.ES.2020.25.14.2000550
9. Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): pooled analysis of early reports. J Crit Care. 2020;58:27–28. PMID: 32279018; PMCID: PMC7118619. doi:10.1016/j.jcrc.2020.03.011
10. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. PMID: 32112977; PMCID: PMC7105032. doi:10.1016/j.ijsu.2020.02.034
11. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID-19 - 5 February 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19---5-february-2020.
12. Hermans C, Weill A, Pierce GF. The COVID-19 pandemic: new global challenges for the haemophilia community. Haemophilia. 2020;26(3):371–372. PMID: 32246879. doi:10.1111/hae.14001
13. Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395(10223):473–475. PMID: 32043983; PMCID: PMC7134694. doi:10.1016/S0140-6736(20)30317-2
14. Sarkar S, Karmakar S, Basu M, Ghosh P, Ghosh MK. Neurological damages in COVID-19 patients: mechanisms and preventive interventions. MedComm. 2023;4(2):e247. PMID: 37035134; PMCID: PMC10080216. doi:10.1002/mco2.247
15. Ferrando C, Mellado-Artigas R, Gea A, et al.; de la Red de UCI Española para COVID-19. Patient characteristics, clinical course and factors associated to ICU mortality in critically ill patients infected with SARS-Cov-2 in Spain: a prospective, cohort, multicentre study. Rev Esp Anestesiol Reanim. 2020; 67(8):425–437. English, Spanish. PMID: 32800622; PMCID: PMC7357496. doi:10.1016/j.redar.2020.07.003
16. Xu J, Yang X, Yang L, et al. Clinical course and predictors of 60-day mortality in 239 critically ill patients with COVID-19: a multicenter retrospective study from Wuhan, China. Crit Care. 2020;24(1):394. PMID: 32631393; PMCID: PMC7336107. doi:10.1186/s13054-020-03098-9
17. Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323(16):1612–1614. PMID: 32191259; PMCID: PMC7082763. doi:10.1001/jama.2020.4326
18. Calver JF, Fabbri L, May J, Jenkins RG. COVID-19 in patients with chronic lung disease. Clin Chest Med. 2023;44(2):385–393. PMID: 37085227; PMCID: PMC9678841. doi:10.1016/j.ccm.2022.11.013
19. Kole C, Stefanou Ε, Karvelas N, Schizas D, Toutouzas KP. Acute and post-acute covid-19 cardiovascular complications: a comprehensive review. Cardiovasc Drugs Ther. 2023;20:1–16. PMID: 37209261; PMCID: PMC10199303. doi:10.1007/s10557-023-07465-w
20. AlQadheeb N, AlMubayedh H, AlBadrani S, et al. Impact of common comorbidities on antimicrobial consumption and mortality amongst critically ill COVID-19 patients: a retrospective two center study in Saudi Arabia. Clin Infect Pract. 2023;19:100229. PMID: 37168925; PMCID: PMC10156636. doi:10.1016/j.clinpr.2023.100229
21. Halpin DMG, Faner R, Sibila O, Badia JR, Agusti A. Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection? Lancet Respir Med. 2020;8(5):436–438. PMID: 32251625; PMCID: PMC7270536. doi:10.1016/S2213-2600(20)30167-3
22. Liu NN, Tan JC, Li J, Li S, Cai Y, Wang H. COVID-19 pandemic: experiences in china and implications for its prevention and treatment worldwide. Curr Cancer Drug Targets. 2020;20(6):410–416. PMID: 32286947. doi:10.2174/1568009620666200414151419
23. The Comprehensive Group of the Joint Prevention and Control Mechanism of The State Council in response to the Novel Coronavirus Infection. Notice on issuing the overall plan of implementing the “class b and b management” for the novel coronavirus infection. National Health Commission of the People’s Republic of China[EB/ OL]; 2022. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202212/e97e4c449d7a475794624b8ea12123c6.shtml.
24. Chinese Thoracic Society; Chinese Association of Chest Physicians. 新型冠状病毒肺炎防治专家意见 [Guide for the prevention and treatment of coronavirus disease 2019]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(6):473–489.Chinese. Chinese. doi:10.3760/cma.j.cn112147-112147-20200321-00392
25. Balakrishnan A, Jacob MM, Senthil Kumar P, et al. Strategies for safe management of hospital wastewater during the COVID-19 pandemic. Int J Environ Sci Technol. 2023;13:1–16. PMID: 36817164; PMCID: PMC9925218. doi:10.1007/s13762-023-04803-1
26. Jiang JM, Feng QM, Fu YM, et al. Wu W. Changes of disease spectrum in emergency critical patients during the epidemic period of novel coronavirus Omicron variant.Chinese. J Critical Care Med. 2022;42(7):596–599. doi:10.3969/j.issn.1002-1949.2022.07.009
27. Romano A, Sotis C, Dominioni G, Guidi S. The scale of COVID-19 graphs affects understanding, attitudes, and policy preferences. Health Econ. 2020;29(11):1482–1494. PMID: 32844495; PMCID: PMC7461444. doi:10.1002/hec.4143
28. George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med. 2020;8(8):807–815. PMID: 32422178; PMCID: PMC7228727. doi:10.1016/S2213-2600(20)30225-3
29. Alali AS, Alshehri AO, Assiri A, et al. Demographics, comorbidities, and outcomes among young and middle-aged COVID-19 patients in Saudi Arabia. Saudi Pharm J. 2021;29(8):833–842. PMID: 34177315; PMCID: PMC8213516. doi:10.1016/j.jsps.2021.06.005
30. Al-Otaiby M, Almutairi KM, Vinluan JM, et al. Demographic characteristics, comorbidities, and length of stay of covid-19 patients admitted into intensive care units in Saudi Arabia: a nationwide retrospective study. Front Med Lausanne. 2022;9:893954. PMID: 35911421; PMCID: PMC9325959. doi:10.3389/fmed.2022.893954
31. Barkhordarian M, Behbood A, Ranjbar M, Rahimian Z, Prasad A. Overview of the cardio-metabolic impact of the COVID-19 pandemic. Endocrine. 2023;80(3):477–490. PMID: 37103684; PMCID: PMC10133915. doi:10.1007/s12020-023-03337-3
32. Schlesinger S, Lang A, Christodoulou N, et al. Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis. Diabetologia. 2023;19:1–18. PMID: 37204441; PMCID: PMC10198038. doi:10.1007/s00125-023-05928-1
33. SeyedAlinaghi S, Karimi A, Afsahi AM, et al. The effectiveness of face masks in preventing covid-19 transmission: a systematic review. Infect Disord Drug Targets. 2023;23(8). PMID: 37259934. doi:10.2174/1871526523666230601090905
34. Naorungroj T, Viarasilpa T, Tongyoo S, et al. Characteristics, outcomes, and risk factors for in-hospital mortality of COVID-19 patients: a retrospective study in Thailand. Front Med Lausanne. 2023;9:1061955. PMID: 36687414; PMCID: PMC9846200. doi:10.3389/fmed.2022.1061955
35. Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201(10):1299–1300. PMID: 32228035; PMCID: PMC7233352. doi:10.1164/rccm.202003-0817LE
36. The Comprehensive Team of the Joint Prevention and Control Mechanism of The State Council for the Novel Coronavirus Infection. Notice on issuing four documents including the implementation measures for nucleic acid testing for the prevention and control of the novel coronavirus pneumonia epidemic. Website of National Health Commission of the People’s Republic of China[EB/ OL]; 2022. Available from: https://www.gov.cn/xinwen/2022-11/21/content_5728107.htm.
37. Khan S, Hasan SS, Bond SE, Conway BR, Aldeyab MA. Antimicrobial consumption in patients with COVID-19: a systematic review and meta-analysis. Expert Rev Anti Infect Ther. 2022;20(5):749–772. PMID: 34895002. doi:10.1080/14787210.2022.2011719
38. Saha A, Ahsan MM, Quader T-U, et al. Characteristics, management and outcomes of critically ill COVID-19 patients admitted to ICU in hospitals in Bangladesh: a retrospective study. J Prev Med Hyg. 2021;62(1):E33–E45. PMID: 34322614; PMCID: PMC8283638. doi:10.15167/2421-4248/jpmh2021.62.1.1838
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
