Back to Journals » Nature and Science of Sleep » Volume 12
Effects of Patient-Directed Interactive Music Therapy on Sleep Quality in Postoperative Elderly Patients: A Randomized-Controlled Trial
Jeongmin Kim,1 Dain Choi,2 Myung Sun Yeo,2 Ga Eul Yoo,2 Soo Ji Kim,3 Sungwon Na1
1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Republic of Korea; 2Department of Music Therapy, Graduate School, Ewha Womans University, Seoul, Republic of Korea; 3Music Therapy Education, Graduate School of Education, Ewha Womans University, Seoul, Republic of Korea
Correspondence: Sungwon Na
Department of Anesthesiology and Pain Medicine, Yonsei University College of Medicine, 50 Yonsei-Ro, Seodaemun-Gu, Seoul 03722, Republic of Korea
Tel +82-2-2228-6456
Fax +82-2-312-7185
Email [email protected]
Soo Ji Kim
Music Therapy Education, Graduate School of Education, Ewha Womans University, 52 Ewhayeodae-Gil, Seodaemun-Gu, Seoul 03760, Republic of Korea
Tel +82-2-3277-6916
Fax +82-2-393-5903
Email [email protected]
Purpose: This study aimed to investigate the effects of patient-directed interactive music on saliva melatonin levels and sleep quality among postoperative elderly patients in the intensive care unit (ICU).
Patients and Methods: A total of 133 elderly patients were randomized into three groups: interactive music therapy (IMT), passive listening (PL), and the control group. The control group (n = 45) received routine medical care, while IMT and PL groups received music therapy on ICU day 1. The IMT group received up to 20 mins of interactive music sessions, including relaxation techniques. The PL group received only pre-selected relaxing music-listening for 30 mins. Saliva melatonin and cortisol levels were measured three times at 11 p.m. (preoperative, operation day, and postoperative day [POD] 1). The Richards-Campbell Sleep Questionnaire (RCSQ) and Quality of Recovery-40 questionnaire (QoR40) were administered on the preoperative day, as well as PODs 1 and 2.
Results: The RCSQ showed a significant improvement in the IMT group compared to the control group on POD2 (71.50 vs 56.89, p=0.012), but the QoR40 did not show any difference between groups. The quality control of the saliva sample was not available due to the immediate postoperative patient’s condition, resulting in a higher dropout rate. Saliva melatonin levels on POD 1 were elevated in the IMT group compared to the control group (1.45 vs 0.04, p=0.0068). The cortisol level did not show a significant difference between groups.
Conclusion: Single IMT intervention improved subjectively assessed short-term sleep quality in postoperative elderly patients. It is difficult to conclude whether music therapy intervention affects the level of melatonin and cortisol.
Trial Registration: The study was registered at ClinicalTrials.Gov (number NCT03156205).
Keywords: critical care, delirium, music therapy, melatonin, sleep
Introduction
Sleep deprivation or disruption is a common problem in the intensive care unit (ICU).1,2 Both environmental and personal factors contribute to sleep problems and can lead to an increase in delirium, mortality, and the length of ICU/hospital stay.3 Patients admitted to the ICU after surgery are unable to sleep for various reasons. Postoperative pain, separation from the family, fear of unfamiliar surroundings, bright lights at night, noise inside the ICU, and anxiety over the results of surgery can make it difficult for patients to sleep.1,4,5 Moreover, the highest rate of delirium occurs in hospitalized older adults, and it can be more critical in older patients with age-associated changes exacerbating acquired weakness during ICU stay.6 To improve sleep quality in ICU patients, intravenous sedatives like benzodiazepines can increase total sleep time, but they alter the physiological natural sleep pattern, and decrease the time spent in the most restorative phases compared to the phases normally mediated by melatonin; melatonin production is decreased in critically ill patients.7
In response to the need for secondary ICU outcomes, non-pharmacological interventions have been suggested to promote sleep quality in the ICU.8 A recent critical review revealed that a wide range of non-pharmacological interventions have been implemented in the ICU such as massage, mindfulness-based stress reduction, ear plugs, or listening to music. Evidence for the effects of non-pharmacological interventions is generally low because of limitations and inconsistencies in trial design.5 Listening to music has been selected to improve the quantity and quality of sleep due to high accessibility and cost-effectiveness.9 There is a growing interest in applying music in the ICU to mitigate negative physiologic outcomes such as anxiety or stress and altered cortisol and melatonin level10 and possibly reduce the need for drugs.11 Depending on the characteristics of the critical illness, limitations may exist in applying certain interventions.
Music therapy has been shown to be effective for patients with primary insomnia.12 A study of surgical patients reported that patients who underwent cardiac surgery had a 30-min music session at 9:00 p.m. and experienced improved sleep quality.10 A meta-analysis of music therapy clinical studies in the ICU by Umbrello et al13 indicated that music therapy could reduce anxiety and stress in critically ill patients. In 2018, the Society of Critical Care Medicine referred to music therapy as a non-pharmacologic pain therapy for critically ill patients.4 As such, evidence is accumulating that music therapy can be an important treatment approach for critically ill patients.
While music-listening is a musically receptive behavior to address stress, anxiety, or pain in medical research, music therapy is defined as a therapeutic process including music therapists and an interaction developed through music experience.14 Considering the multiple factors underscoring sleep deprivation, the active use of music will likely be necessary to maximize the therapeutic effects of music.15 Recent studies have examined active music therapy incorporated with guided imagery or relaxation with music and patient-selected song choices in treatment procedures.11,16
Increased patient participation is a major concern for music therapy to promote sleep among older ICU patients. Moreover, promoting sleep and rest can be achieved by regulating energy consumption throughout the day and night;17 therefore, the frequency and engagement level are both important in ICU interventions. Due to disrupted circadian rhythms interfering with the sleep-wake cycle, consistent and continuing interventions to achieve restorative sleep among older ICU patients are required.1 To date, there have been no studies integrating proportioned interventions to match sleep patterns with increased participation levels in elderly ICU patients. Therefore, the aim of this study was to compare the effects of two different interventions (patient-directed interactive music therapy and passive listening) on sleep quality and melatonin/cortisol levels in postoperative elderly patients admitted to ICU, as well as investigate the impact of music therapy on clinical outcomes.
Patients and Methods
This study was conducted in accordance with the principles of Good Clinical Practice and was approved by the Institutional Research Board of Severance Hospital (reference number 4–2016-0873). Severance hospital is a tertiary university hospital with a total of 2500 beds. The day before surgery, researchers screened subjects scheduled for ICU admission after elective major surgery, confirmed their intention to participate in this randomized-controlled study, and obtained written consent. The patients received fully informed interactive music therapy during their postoperative ICU stay. Patients were randomly allocated to three groups (patient-directed interactive music therapy group, passive listening group, control group) by an investigator using a reproducible set of computer-generated random numbers via a web-based system (REDCap). The allocation was thus concealed until the last minute of the process of obtaining consent. The trial was conducted in accordance with the Declaration of Helsinki. The study was registered at ClinicalTrials.Gov with the number NCT03156205.
Exclusion criteria included neuropsychiatric history, alcoholism, dementia, impaired cognitive dysfunction, cerebral infarction, transient cerebral ischemic attack, severe liver disease, kidney disease, diabetes, sleep disorders before admission, and emergency surgery. The control group received only routine medical care (n=45). The other two experimental groups received either patient-directed interactive music therapy (IMT) (n=44) or passive listening (PL) (n=44). Figure 1 shows a schematic of the research process. Figure 2 shows a flow diagram of the patients. Before surgery, to evaluate the quality and duration of sleep, the Richards-Campbell Sleep Questionnaire (RCSQ) was administered to all participants. This five-item, visual analogue scale was designed as an outcome measure for assessing the perception of sleep in critically ill patients.18 The scale evaluates perceptions of the depth of sleep, sleep onset latency, number of awakenings, time spent awake, and overall sleep quality. Each RCSQ response was recorded on a 100-mm visual-analogue scale, with higher scores representing better sleep and the mean score of these 5 items, known as the “total score,” representing the overall perception of sleep. The Quality of Recovery-40 questionnaire (QOR40) was used to assess the quality of recovery after general anesthesia, which may affect sleep. The QOR40 is a widely used, self-rated, and self-completed questionnaire for postoperative patients. The questionnaire is composed of 40 items divided into 5 sub-scales, including physical comfort, emotional state, psychological support, physical independence, and pain.19 The average time taken to complete the QoR-40 is 5 mins.20 The RCSQ and QOR40 were measured once a day between 8 a.m. and 9 a.m. on the first and second PODs. All subjects were screened for postoperative delirium with the Confusion Assessment Method for the ICU (CAM-ICU) three times a day during ICU stay. The CAM-ICU appears to be rapid, valid, and reliable for diagnosing delirium in the ICU setting and may be a useful instrument for both clinical and research purposes.21 It has four features: (1) altered mental status/fluctuating course, (2) inattention, (3) altered level of consciousness, and (4) disorganized thinking. The result is positive if a patient has both altered mental status or fluctuating course (Feature 1) and inattention (Feature 2) and either altered level of consciousness (Feature 3) or disorganized thinking (Feature 4). Pain was assessed daily by assigned nurses on a numeric rating scale (NRS). We assessed postoperative pain using the NRS at least four times a day and controlled the pain so that the NRS did not exceed four points.
 |
Figure 1 Time table. |
 |
Figure 2 Participant flow chart. |
In order to measure cortisol and melatonin, a commercial Salivette® (SARSTEDT AG & Co, Nümbrecht, Germany) tube containing a cotton wool swab was used to collect saliva. The swab was rotated in the mouth for at least 2 min and inserted back into the tube. Saliva was collected at 9 p.m. every night before surgery, on the day of surgery, and 1 day after surgery. The samples were analyzed by a commercial enzyme immunoassay (EIA, Salivary Cortisol Enzyme Immunoassay Kit, Salimetrics LLC, State College, PA, USA). The limit of quantification of the ELISA assay is the melatonin and cortisol concentrations in saliva that can be measured with an inter-assay coefficient of variation (CV) of less than 15%.
Patient-Directed Interactive Music Therapy Intervention
The IMT group participated in (a) individual music therapy implemented by a certified music therapist during the day and (b) individual music-listening at night. During the day, patients participated in an individual music therapy intervention for approximately 15–20 mins between 10 a.m. and 12 p.m. The intervention was composed of the following sequence: a breathing exercise with music, interactive music-making, followed by the same breathing exercise. For breathing control with music, exercises for breathing in and out slowly and deeply were performed with the provision of music in which the type of melodic pattern (eg, rising and falling) and changes in loudness (eg, increasing and decreasing) were composed to match the cycle of inhalation and exhalation. The selection of music was determined on the basis of the patient’s preferred genres of music reported by the patient at their initial interview. The type of musical task and level of engagement varied depending on patient’s physical and emotional states. The intervention ended with a breathing exercise so that the patient was reminded of how to self-initiate simple exercises during their ICU stay or during music-listening at night.
At night, earphones and an MP3 player were provided with which participants could listen to music for 30 mins between 8 and 10 p.m. Prior to music-listening, a music therapist assessed whether each patient was willing to listen to the list of music presented. Each participant was then encouraged to perform this exercise while listening to music. If a patient requested to stop their participation, or if medical professionals judged that a patient’s medical condition prevented them from continuing their participation, they were withdrawn from the study.
Passive Music-Listening Intervention
The PL group listened to music at night without music intervention during the day. As per the IMT group, the duration of music-listening was 30 mins. The MP3 player was set to automatically turn off after 30 mins. The selected music had been judged as relaxing in prior studies. Classical pieces of music or contemporary instrumental music, including Air for G string, Allemande, Canon, Nocturne, and Swan were selected. Prior to music-listening, a list of music pre-selected by the therapist was shown to each patient. If a patient opted not to listen to the music provided, another list of pre-selected music was presented. If the patient requested to stop listening to music, they were withdrawn from the study.
Statistical Analysis
IBM SPSS version 20.0 (IBM Corporation, Armonk, NY, USA) was used for all analyses. We calculated the number of subjects based on a previous study comparing the quality of sleep according to relaxation music therapy.10 Based on the results from the previous study, we assumed that the IMT group and the control group had a significant difference in sleep quality scores of 28 points or more (α = 0.05, power = 80%), and 45 people per group were calculated using the PASS software (power analysis and sample-e package, NCSS statistical software). Efficacy was evaluated by both the full Analysis set (FAS, based on the intention-to-treat principle) and the per-protocol set (PPS); FAS findings were interpreted as the main results. The FAS comprised participants who underwent music therapy after randomization and did not violate the inclusion or exclusion criteria. The PPS comprised participants who completed the trial without any significant protocol deviations that could affect efficacy. The per-protocol set consisted of subjects whose evaluated variables were observed in POD2, which was the main evaluation point. Observed-case analysis included those with missing data, which were not imputed for the missing value. To compensate for the missing value due to the limitations of saliva sample collection, the linear mixed-effects models with a random intercept that is a more informative method using repeated measured data was further used. (Figure 3) Results of demographics are expressed as the mean ± standard deviation, numbers (proportion), median (interquartile), or least-squares means ± standard error. To test for difference in baseline characteristics between three groups, Kruskal–Wallis test or one-way ANOVA was used for continuous variables. Chi-square test, or Fisher’s exact test was used for categorical variables. Bonferroni correction was adapted for multiple comparisons.
Results
A total of 200 patients were screened (Figure 2). With the exception of 48 patients who altered their postoperative plans and were transferred to the general ward after surgery, and five patients who canceled the surgery, 147 patients were enrolled in the study. A total of 133 patients were included in the final analysis, excluding three patients who refused to participate in the study and 11 who were lost to follow-up (Table 1). No subject refused to listen to music after participating in the study. Table 1 summarizes the characteristics of the patients. There was no difference in demographics between the three groups. Patients’ outcomes including ICU/hospital stay, mortality, and delirium were not significantly different among the groups.
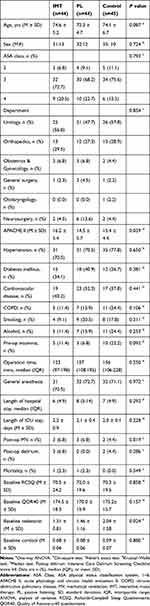 |
Table 1 Demographics (N=133) |
Sleep Quality and Quality of Recovery from Surgery
Sleep quality evaluated with RCSQ on POD2 was significantly improved in the IMT group than in control groups (Table 2). After intervention, the mean and standard deviation of RCSQ values were statistically different with IMT vs control 71.50 ± 26.07 vs 56.89 ± 23.77 (p=0.007) Post-hoc analysis with the Bonferroni correction were performed for multiple comparisons when RCSQ showed significant differences between groups (p=0.00021). The mean and standard deviation of QOR40 values after intervention were not statistically significant, 167.4 ± 22.16 vs 160.2 ± 22.49. (p=0.1338)
 |
Table 2 Richards-Campbell Sleep Questionnaire and Quality of Recovery 40 Questionnaire (N=133) |
Biomarkers, Melatonin, and Cortisol in Saliva
Saliva melatonin levels on POD 1 were elevated in the IMT group compared to the control group (1.45 vs 0.04, p=0.0068). No significant differences in cortisol levels were detected among the three groups (Table 3).
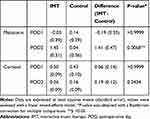 |
Table 3 Melatonin and Cortisol Level in Saliva Sample |
Discussion
Adequate sleep is required for recovery from critical illness and prevention of delirium. Recent trials have reported that ICU patients suffer from severe sleep disturbances because of various factors such as pain, noise, anxiety, and environmental discomfort.1 Many complementary and alternative measures including music-listening, massage, and environmental modification have been implemented to attenuate factors interrupting sleep.5,22 Providing music can be an effective way to promote sleep in critically ill patients, and patient-directed interactive treatment may be therapeutically superior to passive listening for patient outcomes.11,16 We observed that interactive music therapy could improve the quality of sleep in postoperative elderly patients after surgery over routine care or passive music-listening.
These results support the fact that patient-directed interactive music therapy could be a potential option for addressing the sleep-related issues of critically ill patients. Numerous trials have attempted to improve sleep and prevent delirium in critically ill patients. Hypnotics (including benzodiazepines and propofol) have been used in clinical fields for many years to promote sleep, but have been associated with delirium and are no longer recommended.8 Antipsychotics and antidepressants are the most widely used agents to mitigate anxiety and improve sleep; however, their use can be complicated by side effects such as arrhythmia. Recent trials using melatonin and dexmedetomidine have shown promising results. Skrobik et al23 reported that nocturnal dexmedetomidine could reduce the incidence of delirium in ICU patients. Administration of low-dose intravenous dexmedetomidine from 9 p.m. to 6 a.m. improved sleep quality. Although there is insufficient evidence for improvement of delirium or sleep in critically ill patients by melatonin administration, it is well established that surgical patients are more vulnerable than medical patients to sleep disruption and melatonin imbalances.24 Perioperative stress including pain, anxiety, and inflammatory responses influences the balance between melatonin secretion and elimination.
For non-pharmacologic approaches, many modalities of care have been attempted, including music, modification of ventilatory mode, masking sensory input such as wearing eye masks or earplugs, providing quiet time, acupuncture, and aromatherapy.8 Among them, providing music therapy in combination with other modalities has demonstrated some benefits of relieving pain and anxiety and/or promoting sleep.9–13,16 Hu et al10 investigated the effects of sensory masking with earplugs and eye masks combined with relaxing music in 50 adult cardiac surgical patients. They observed that earplugs, eye masks, and music could improve sleep quality; however, urinary melatonin and cortisol levels were not significantly different. A common finding between this study and our work was that music improved the subjective perception of sleep in postoperative ICU patients. While we observed increased salivary melatonin levels with interactive music therapy, Hu et al reported that passive music-listening with sensory masking did not increase urine melatonin levels. The main difference between interactive and passive music therapy is patients’ engagement level in musical tasks to stimulate their physical and emotional states. Music therapy in the ICU has gained interest as a tool for distraction from pain or negative emotions by masking environmental sounds. Recent studies have reported the extensive use of music including composing music25 or making music lists for individual music-listening.16 By increasing patients’ engagement level in musical tasks, PDIMT (Patient-directed Interactive Music therapy) in this study highlighted the potential of applying music-making procedures in elderly patients to stimulate physiological and psychological changes. Previous studies have reported the effects of using music on patients in the ICU,13,16 yet the patients’ engagement level has not been considered to the same degree. Here, IMT focused on double intervention during the day and at night for encouraging self-initiated use of music as a patient-centered perspective in ICU care. In this regard, IMT is the first attempt to tailor musical tasks for elderly patients in the ICU by integrating both listening to playing music and vocal participation. This implies that active musical participation should be considered for elderly patients in the ICU to promote physical and mental recovery by improving sleep quality.
From the perspective of clinical implications of our work, patient-centered and family-centered care are highlighted in clinical fields, especially in critical care.26 Our research group published a study investigating the effects of mothers’ voice recordings on postoperative anxiety in pediatric patients.27 We observed that music experience influences the depression levels of family caregivers of critically ill patients.28 We observed that both patients and their families were satisfied with their involvement in the treatment and recovery process. Further trials should focus on the involvement of the family in music therapy, which can provide positive effects on post-intensive care syndrome for the family.
This study has several limitations. First, it is a single-center randomized trial with a small study population, the subjects of our study were limited to patients who do not need mechanical ventilation, are capable of spontaneous ventilation, and are relatively less severe. Second, we evaluated sleep quality with the RCSQ, which is a subjective questionnaire instead of the gold standard of polysomnography. The use of polysomnography would have been ideal but applying this method to surgical ICU patients would have been challenging due to discomfort of the electroencephalogram and the associated expense. While polysomnography has been used in medical or neurological ICUs,25,29 trials applying it in surgical ICU patients are scarce. Third, we investigated the short-term effects of only one music intervention session. We observed that interactive music intervention induced better sleep on that day, but ICU patients typically suffer from prolonged periods of insomnia.30 Further investigations should target multiple sessions of music interventions and their effects on sleep and other clinical outcomes such as delirium, anxiety, and pain. Fourth, the limitation of this study is the effect of IMT on the level of melatonin is statistically significant, but interpretation should be very careful. Melatonin is very important for investigating the human biological circadian rhythm. However, without controlling the ICU environment such as shade or noise insulation at night that affects the level of melatonin,2 there are definite limitations to interpreting the results. Unlike animal experimental conditions, the subject’s space cannot be separated from other patients’, and unexpected emergencies may occur day and night, making it very difficult for ICU to secure a controlled sleep environment. More studies using controlled trials are needed to confirm that IMT can affect hormonal changes in postoperative elderly patients. The last issue which should be mentioned is the appropriateness of saliva samples to measure melatonin and stress hormones. Due to various factors such as hypovolemia, anesthetic pre-medication, and the old age of the study population, acquiring an appropriate amount of saliva sample was challenging, especially on the night of the operation. However, we opted to use saliva due to minimal invasiveness and patient comfort. Sampling blood or urine during the nighttime could interrupt patients’ sleep due to pain or discomfort of moving to the restroom to obtain urine. Considering the advantages of saliva samples, only saliva collection was planned, but in reality, the saliva secretion was reduced in patients after surgery, making it difficult to obtain feasible samples, resulting in a high dropout rate for biomarker analysis. In addition, continuous sampling of melatonin measured in saliva is desirable to assess circadian timing by determining the onset of dim light melatonin (DLMO), which is the time when the level rises above baseline.31 The primary outcome of our study is to prove the hypothesis that IMT affects the sleep quality score. There are unexpected methodological limitations in proving biological evidence to support this. This would be a fruitful area for further work.
Conclusions
In conclusion, the results of this study demonstrated that providing patient-directed interactive music sessions could promote subjective sleep quality in postoperative elderly patients in the ICU. In addition to pharmacological measures, our work highlights the potential of non-pharmacological interventions, including music, to promote sleep in elderly ICU patients.
Abbreviations
CAM-ICU, Confusion Assessment Method for the intensive care unit; CV, coefficients of variation; ICU, intensive care unit; IQR, interquartile range; PDIMT, patient-directed interactive music therapy; NRS, numeric rating scale; PL, passive listening; QOR40, Quality of Recovery-40 questionnaire; RCSQ, Richards-Campbell Sleep Questionnaire; SD, standard deviation.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the principles of Good Clinical Practice and was approved by the Institutional Research Board of Severance Hospital (reference number 4-2016-0873). All patients provided written informed consent.
Funding
This work was supported by a grant from the National Research Foundation of Korea (2016R1A2B1012708).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pisani MA, Friese RS, Gehlbach BK, Schwab RJ, Weinhouse GL, Jones SF. Sleep in the intensive care unit. Am J Respir Crit Care Med. 2015;191(7):731–738. doi:10.1164/rccm.201411-2099CI
2. Boyko Y, Jennum P, Toft P. Sleep quality and circadian rhythm disruption in the intensive care unit: a review. Nat Sci Sleep. 2017;9:277–284. doi:10.2147/NSS.S151525
3. Weinhouse GL, Schwab RJ, Watson PL, et al. Bench-to-bedside review: delirium in ICU patients - importance of sleep deprivation. Crit Care. 2009;13(6):234. doi:10.1186/cc8131
4. Devlin JW, Skrobik Y, Gelinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–e873. doi:10.1097/CCM.0000000000003299
5. Hu RF, Jiang XY, Chen J, et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev. 2015;10:CD008808. doi:10.1002/14651858.CD008808.pub2
6. Elias MN, Munro CL, Liang Z, Calero K. Sleep and intensive care unit-acquired weakness in critically ill older adults. Dimens Crit Care Nurs. 2019;38(1):20–28. doi:10.1097/DCC.0000000000000335
7. Mistraletti G, Carloni E, Cigada M, et al. Sleep and delirium in the intensive care unit. Minerva Anestesiol. 2008;74(6):329–333.
8. Brito RA. Pharmacological and non-pharmacological interventions to promote sleep in intensive care units: a critical review. Sleep Breath. 2019. doi:10.1007/s11325-019-01902-7
9. Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Syst Rev. 2006;(2):CD004843. doi:10.1002/14651858.CD004843.pub2
10. Hu RF, Jiang XY, Hegadoren KM, Zhang YH. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care. 2015;19(1):115. doi:10.1186/s13054-015-0855-3
11. Gullick JG, Kwan XX. Patient-directed music therapy reduces anxiety and sedation exposure in mechanically-ventilated patients: a research critique. Aust Crit Care. 2015;28(2):103–105. doi:10.1016/j.aucc.2015.03.003
12. Feng F, Zhang Y, Hou J, et al. Can music improve sleep quality in adults with primary insomnia? A systematic review and network meta-analysis. Int J Nurs Stud. 2018;77:189–196. doi:10.1016/j.ijnurstu.2017.10.011
13. Umbrello M, Sorrenti T, Mistraletti G, Formenti P, Chiumello D, Terzoni S. Music therapy reduces stress and anxiety in critically ill patients: a systematic review of randomized clinical trials. Minerva Anestesiol. 2019;85(8):886–898. doi:10.23736/S0375-9393.19.13526-2
14. Zhang Y, Cai J, An L, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev. 2017;35:1–11. doi:10.1016/j.arr.2016.12.003
15. Loewy J. Music therapy as a potential intervention for sleep improvement. Nat Sci Sleep. 2020;12:1–9. doi:10.2147/NSS.S194938
16. Chlan LL, Weinert CR, Heiderscheit A, et al. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilatory support: a randomized clinical trial. JAMA. 2013;309(22):2335–2344. doi:10.1001/jama.2013.5670
17. Lai HL, Good M. Music improves sleep quality in older adults. J Adv Nurs. 2005;49(3):234–244. doi:10.1111/j.1365-2648.2004.03281.x
18. Richards KC, O’Sullivan PS, Phillips RL. Measurement of sleep in critically ill patients. J Nurs Meas. 2000;8(2):131–144. doi:10.1891/1061-3749.8.2.131
19. Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth. 2000;84(1):11–15. doi:10.1093/oxfordjournals.bja.a013366
20. Gornall BF, Myles PS, Smith CL, et al. Measurement of quality of recovery using the QoR-40: a quantitative systematic review. Br J Anaesth. 2013;111(2):161–169. doi:10.1093/bja/aet014
21. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patientsvalidity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703–2710. doi:10.1001/jama.286.21.2703
22. Richards K, Nagel C, Markie M, Elwell J, Barone C. Use of complementary and alternative therapies to promote sleep in critically ill patients. Crit Care Nurs Clin North Am. 2003;15(3):329–340. doi:10.1016/S0899-5885(02)00051-5
23. Skrobik Y, Duprey MS, Hill NS, Devlin JW. Low-dose nocturnal dexmedetomidine prevents ICU delirium. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2018;197(9):1147–1156. doi:10.1164/rccm.201710-1995OC
24. Bourne RS, Mills GH. Melatonin: possible implications for the postoperative and critically ill patient. Intensive Care Med. 2006;32(3):371–379. doi:10.1007/s00134-005-0061-x
25. Su C-P, Lai H-L, Chang E-T, Yiin L-M, Perng S-J, Chen P-W. A randomized controlled trial of the effects of listening to non-commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care unit. J Adv Nurs. 2013;69(6):1377–1389. doi:10.1111/j.1365-2648.2012.06130.x
26. Kleinpell R, Heyland DK, Lipman J, et al. Patient and family engagement in the ICU: report from the task force of the world federation of societies of intensive and critical care medicine. J Crit Care. 2018;48:251–256. doi:10.1016/j.jcrc.2018.09.006
27. Kim SJ, Oh YJ, Kim KJ, Kwak YL, Na S. The effect of recorded maternal voice on perioperative anxiety and emergence in children. Anaesth Intensive Care. 2010;38(6):1064–1069. doi:10.1177/0310057X1003800617
28. Yoo GE, Kim J, Choi DI, Yeo MS, Kim SJ. Music experience is associated with lower depression level and higher quality of life among family caregivers of critically ill patients. Psychol Music. 2020;0305735620906881.
29. Foreman B, Westwood AJ, Claassen J, Bazil CW. Sleep in the neurological intensive care unit: feasibility of quantifying sleep after melatonin supplementation with environmental light and noise reduction. J Clin Neurophysiol. 2015;32(1):66–74. doi:10.1097/WNP.0000000000000110
30. Pulak LM, Jensen L. Sleep in the intensive care unit: a review. J Intensive Care Med. 2016;31(1):14–23. doi:10.1177/0885066614538749
31. Keijzer H, Smits MG, Duffy JF, Curfs LMG. Why the dim light melatonin onset (DLMO) should be measured before treatment of patients with circadian rhythm sleep disorders. Sleep Med Rev. 2014;18(4):333–339. doi:10.1016/j.smrv.2013.12.001
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

