Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Effects of long-acting injectable antipsychotics versus oral antipsychotics on autonomic nervous system activity in schizophrenic patients
Authors Suda A, Hattori S, Kishida I, Miyauchi M , Shiraishi Y , Fujibayashi M, Tsujita N , Ishii C , Ishii N, Moritani T, Hirayasu Y
Received 14 May 2018
Accepted for publication 6 July 2018
Published 17 September 2018 Volume 2018:14 Pages 2361—2366
DOI https://doi.org/10.2147/NDT.S173617
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Akira Suda,1 Saki Hattori,1 Ikuko Kishida,1,2 Masatoshi Miyauchi,1 Yohko Shiraishi,1 Mami Fujibayashi,3 Natsuki Tsujita,4 Chie Ishii,2 Norio Ishii,2 Toshio Moritani,5 Yoshio Hirayasu1,6
1Department of Psychiatry, Yokohama City University School of Medicine, Yokohama, 2Department of Psychiatry, Fujisawa Hospital, Kanagawa, 3Division of Physical and Health Education, Setsunan University, Osaka, 4Graduate School of Human and Environmental Studies, Kyoto University, 5Department of Health and Sports Sociology, Faculty of General Education, Kyoto Sangyo University, Kyoto, 6Department of Psychiatry, Hirayasu Hospital, Okinawa, Japan
Objective: Long-acting injections (LAIs) of antipsychotics show distinct pharmacokinetic profiles from oral antipsychotics (OAPs). Although there may be differences in adverse event frequency, any differences in their effects on autonomic nervous system (ANS) remain unclear.
Patients and methods: In total, 270 schizophrenic patients were recruited in this study: 241 received OAPs (risperidone, olanzapine, quetiapine, or aripiprazole) and 29 received LAIs (risperidone LAI, aripiprazole LAI, or paliperidone palmitate) as monotherapy. Heart rate variability was measured as an index of ANS activity, and the low-frequency (0.03–0.15 Hz) component, high-frequency (0.15–0.40 Hz) component, and total power (0.03–0.40 Hz) were calculated. Components were compared between the groups using t-tests.
Results: A significant difference was detected in the low-frequency component between the OAP and LAI groups (P=0.046). No significant difference was found in total power or the high-frequency component between the two groups.
Conclusion: Compared with OAPs, LAIs have fewer adverse effects on ANS activity, particularly the low-frequency component, as determined using a spectral analysis of heart rate variability.
Keywords: long-acting injectable antipsychotics, autonomic nervous system, heart rate variability, adverse effect
Introduction
The mortality risk of schizophrenic patients is two to three times higher than that of the general population,1–3 and one of the notable causes of death is cardiovascular disease.1,2,4–6 Some explanations have been advanced for the higher risk of cardiovascular disease in these patients. For example, antipsychotic medication has been linked to cardiovascular adverse effects and unexplained sudden death.7,8 However, why sudden death can occur during treatment with antipsychotics remains unclear.
In schizophrenic patients, antipsychotics are strongly associated with dysfunction of the autonomic nervous system (ANS),9–15 and decreased ANS activity is associated with morbidity and sudden death due to cardiovascular disease.16 We previously reported the dose-dependent adverse effects of antipsychotic drugs on ANS activity and suggested that higher blood levels of antipsychotics decrease ANS activity.14
Long-acting injections (LAIs) of antipsychotics are an important option for relapse prevention, especially for nonadherent patients.17–21 In terms of safety and tolerability, meta-analysis results suggest that LAIs and oral antipsychotics (OAPs) do not differ with respect to the frequency of treatment discontinuation due to adverse events.22,23 However, it is important to note that LAIs have different pharmacokinetic profiles from OAPs, which could be associated with fewer adverse events. Taipale et al reported that LAI use is associated with an ~30% lower risk of death compared with oral agents.24 Another study reported that extrapyramidal symptoms were possibly improved in patients treated with LAIs.25 A recent study also indicated that switching from oral risperidone to LAI improved verbal capability.26 Some other studies suggest that serum prolactin levels are lower with LAIs than with OAPs.27–29 Therefore, LAIs could have fewer ANS activity-related adverse effects compared with OAPs. However, as far as we know, no previous studies have compared LAIs and OAPs in the presymptomatic state.
Therefore, in this study, we investigated the effects of four atypical antipsychotic drugs and three LAIs of atypical antipsychotics on ANS activity. We evaluated ANS activity noninvasively by assessing 5-minute resting heart rate variability (HRV), which can indicate autonomic imbalance. HRV power spectral analysis has been used in both basic medical science and clinical research to identify the three major spectral components of HRV under various psychophysiological conditions, and its reliability, validity, and practicability are well documented.30–32 Comparing ANS activities associated with the two groups could offer important information on antipsychotic safety.
Patients and methods
Participants
This cross-sectional study assessed 270 consecutive Japanese schizophrenic patients (62 inpatients and 208 outpatients; 142 women; mean age±SD, 51.68±15.65 years) receiving treatment at Fujisawa Hospital and Yokohama City University Hospital, Japan, from July 2007 to November 2017. All patients had received either an OAP (risperidone, olanzapine, aripiprazole, or quetiapine) or an LAI (risperidone LAI, aripiprazole LAI, or paliperidone palmitate) as monotherapy for >3 months at the same dosage and without adjustment in the previous 3 months. The 241 patients in the OAP group were those involved in our previous study comparing the effects of the same four OAPs on ANS activity,33 and the patients receiving LAI were newly recruited for the present study. In the LAI group, 17 patients (58.6%) received paliperidone palmitate, 9 (31.0%) received aripiprazole LAI, and 3 (10.3%) received risperidone LAI.
All participants were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition34 by sufficiently experienced psychiatrists. Patients unable to take the antipsychotics as prescribed and/or attend the hospital for at least 1 year were excluded, as well as those with current or past history of substance abuse possibly obscuring diagnosis or any neurological, endocrine, respiratory, or cardiovascular illness. Also excluded were any patients receiving medication for physical conditions. Severity of patients’ positive, negative, and general signs was assessed using a Japanese translation of the Positive and Negative Syndrome Scale (PANSS)35 on the day the electrocardiography (ECG) was recorded. Participants’ clinical information was collected from their medical records. All prescribed psychotropic medications were assessed, including antiparkinsonian, antipsychotic, and benzodiazepine agents. Doses were calculated by conversion to standard equivalents of biperiden, chlorpromazine, and diazepam.36
The protocol was approved by the institutional ethics committee of Fujisawa Hospital and adhered to the Declaration of Helsinki. Participants provided written informed consent after receiving a complete explanation of the study.
R–R interval power spectral analysis
As in our previous studies,38,39 5-minute resting HRV was assessed to evaluate ANS activity noninvasively. All measurements were performed between 09:00 and 12:00. The ECG was performed for 5 minutes in seated patients who had not consumed caffeine or smoked that morning and had rested for at least 10 minutes beforehand. In HRV power spectral analysis, a series of sequential R–R intervals obtained from the 5-minute ECG are decomposed via fast Fourier transform into the sum of sinusoidal functions of different amplitudes and frequencies.37–42
As in our previous studies,30–32,37,38 the areas under the curve in the following frequency bands were determined to quantify the spectral power in each frequency domain: low-frequency (LF; 0.03–0.15 Hz) HRV, high-frequency (HF; 0.15–0.40 Hz) HRV, and total power (TP; 0.03–0.40 Hz).39–41 These domains correlate to sympathetic and parasympathetic nerve activity, primarily parasympathetic nerve activity, and overall ANS activity, respectively.
Statistical analysis
Student’s t-tests were used to assess differences in clinical characteristics (age, body mass index [BMI], disease duration, antipsychotic drug dose, anticholinergic agent dose, benzodiazepine agent dose, and PANSS score) and the LF, HF, and TP components of HRV. The chi-squared test was used to examine the proportions of male and female participants, inpatients and outpatients, and smokers and non-smokers. The effects of clinical factors on ANS activity were evaluated using multiple regression analysis. The LF, HF, and TP components of the HRV were considered as the dependent variables, whereas the independent variables possibly affecting ANS activity were age, BMI, PANSS score, and antipsychotic drug formulation.12,43 After adjustment for these possible factors, the relationship between all HRV components and the drug formulation was assessed. Because the data were skewed, the absolute values of the HRV spectral components were log-transformed before the statistical analysis. The statistical analysis was performed using SPSS for Windows version 24 (IBM Corporation, Armonk, NY, USA). A P-value <0.05 was considered significant.
Results
The demographic and medication data of the 241 participants in the OAP group and the 29 participants in the LAI group are shown in Table 1. There were no significant differences in demographics, PANSS score, anticholinergics, or benzodiazepines between the two groups. However, the mean dose of antipsychotics administered was significantly higher in the LAI group (P=0.021).
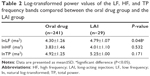
As shown in Table 2, there was a significant difference in the LF component between the OAP and LAI groups (P=0.001), but no significant difference in TP or the HF component.
Multiple regression analysis revealed that all three HRV components were significantly associated with age. Because the strong association of age with HRV had already been reported,43,44 we performed multiple regression analyses excluding age. Consequently, the antipsychotic formulation was significantly associated with the LF component (Table 3), but not with the HF component or TP. There were no associations between any of the components of HRV and the PANSS score or BMI.
Discussion
This study is the first to analyze the different effects of OAPs and LAIs on ANS activity, which were assessed using the noninvasive method of HRV power spectral analysis. Our results reveal significant differences in HRV between OAP and LAI patients. The LF component values were lower in the OAP group, even though their mean dose of given antipsychotics was lower. Because the LF component represents sympathetic and partially vagal modulation, our results suggest that the sympathetic nervous activity is lower in OAP patients.
Bioequivalence to oral formulations has been established for LAIs. On the other hand, some previous studies suggest that LAIs have better safety and tolerability than OAPs. Some suggest that serum prolactin levels are lower with LAIs than with OAPs.27–29 Some also suggest that switching from paliperidone to paliperidone palmitate decreases extrapyramidal side effect liability.29,45 The steady-state, peak-to-trough, plasma concentration ratios of risperidone vary according to the type of drug, with the results indicating that LAIs have lower peak-to-trough blood level variations than OAPs.46,47 We previously reported that antipsychotic medications can exacerbate ANS dysfunction in schizophrenic patients in a dose-related fashion.14 Considering that many previous studies support a significant correlation between plasma concentration and increased adverse events,48,49 this pharmacokinetic difference between the two preparations could be associated with the frequency of adverse effects of LAIs. Therefore, this pharmacokinetic profile could help to explain our results.
A recent report showed no significant differences between LAIs and OAPs in terms of cardiovascular adverse events.23 In our study, we excluded individuals with any diagnosed cardiovascular complication to estimate their ANS activity at a presymptomatic state. We need to investigate the course of the two groups over a longer period of time to clarify whether the lower effect of the drugs on ANS activity could lead to lower risks of cardiovascular events.
Multiple regression analysis revealed significant associations between the drug formulations of the atypical antipsychotic drugs and all components of ANS activity. However, BMI and the PANSS score were not associated with any component of ANS activity, suggesting that formulations of atypical antipsychotics alone affect the LF component. Also, our results showed that drug formulations are unlikely to be influenced by the HF component and TP. The HF component of HRV is also reported to have a stronger association with various factors, including the severity of negative symptoms, compared with the LF component.50–52 Thus, the effect of severity might lessen the influence of the drug formulation on the HF component.
This study has some limitations. First, the number of participants was small, especially in the LAI group, and we could not perform subanalysis to compare OAPs and LAIs of the same drug. Second, we could not elucidate causal relationships due to the cross-sectional design. Third, various factors such as treatment history may have caused variation in the ANS activities before the patients were grouped. Fourth, we could not eliminate the effect of difference in antipsychotic doses between the two groups. In addition, because of the age differences between the study groups, we could not exclude the possibility that age affects ANS activity or interacts with the effects of antipsychotics.
Conclusion
As determined using HRV power spectral analysis, LAIs have fewer adverse effects on ANS, particularly sympathetic nerve activity, than OAPs. We need to clarify the course of patients with decreased ANS activity and perform further studies with larger populations to clarify the safety of LAIs in terms of ANS activity.
Disclosure
The authors report no conflicts of interest in this work.
References
Brown S, Kim M, Mitchell C, Inskip H. Twenty-five year mortality of a community cohort with schizophrenia. Br J Psychiatry. 2010;196(2):116–121. | ||
Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172–1181. | ||
Walker ER, Mcgee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. | ||
Healy D, Le Noury J, Harris M, et al. Mortality in schizophrenia and related psychoses: data from two cohorts, 1875–1924 and 1994–2010. BMJ Open. 2012;2(5):e001810. | ||
Ifteni P, Correll CU, Burtea V, Kane JM, Manu P. Sudden unexpected death in schizophrenia: autopsy findings in psychiatric inpatients. Schizophr Res. 2014;155(1–3):72–76. | ||
Koponen H, Alaräisänen A, Saari K, et al. Schizophrenia and sudden cardiac death: a review. Nord J Psychiatry. 2008;62(5):342–345. | ||
Appleby L, Thomas S, Ferrier N, Lewis G, Shaw J, Amos T. Sudden unexplained death in psychiatric in-patients. Br J Psychiatry. 2000;176:405–406. | ||
Mentonen OP, Aranko K, Malkonen L, Vapaatalo H. A survey of 49 cases of sudden death associated with the use of antipsychotic or antidepressant drugs. Acta Psychiatr Scand. 1991;84(1):58–64. | ||
Agelink MW, Majewski T, Wurthmann C, et al. Effects of newer atypical antipsychotics on autonomic neurocardiac function: a comparison between amisulpride, olanzapine, sertindole, and clozapine. J Clin Psychopharmacol. 2001;21(1):8–13. | ||
Birkhofer A, Geissendoerfer J, Alger P, et al. The deceleration capacity – a new measure of heart rate variability evaluated in patients with schizophrenia and antipsychotic treatment. Eur Psychiatry. 2013;28(2):81–86. | ||
Cohen H, Loewenthal U, Matar M, Kotler M. Association of autonomic dysfunction and clozapine. Heart rate variability and risk for sudden death in patients with schizophrenia on long-term psychotropic medication. Br J Psychiatry. 2001;179(2):167–171. | ||
Huang WL, Chang LR, Kuo TB, Lin YH, Chen YZ, Yang CC. Impact of antipsychotics and anticholinergics on autonomic modulation in patients with schizophrenia. J Clin Psychopharmacol. 2013;33(2):170–177. | ||
Ieda M, Miyaoka T, Wake R, et al. Evaluation of autonomic nervous system by salivary alpha-amylase level and heart rate variability in patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2014;264(1):83–87. | ||
Iwamoto Y, Kawanishi C, Kishida I, et al. Dose-dependent effect of antipsychotic drugs on autonomic nervous system activity in schizophrenia. BMC Psychiatry. 2012;12:199. | ||
Kim JH, Yi SH, Yoo CS, et al. Heart rate dynamics and their relationship to psychotic symptom severity in clozapine-treated schizophrenic subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(2):371–378. | ||
Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol. 2010;141(2):122–131. | ||
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S. Oral versus depot antipsychotic drugs for schizophrenia – a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127(1–3):83–92. | ||
Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. 2013;74(10):957–965. | ||
Kishimoto T, Robenzadeh A, Leucht C, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr Bull. 2014;40(1):192–213. | ||
Taipale H, Mehtälä J, Tanskanen A, Tiihonen J. Comparative Effectiveness of antipsychotic drugs for rehospitalization in schizophrenia–a nationwide study with 20-year follow-up. Schizophr Bull. Epub 2017 Dec 20; doi:10.1093/schbul/sbx176. | ||
Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29 823 patients with schizophrenia. JAMA Psychiatry. 2017;74(7):686–693. | ||
Misawa F, Kishimoto T, Hagi K, Kane JM, Correll CU. Safety and tolerability of long-acting injectable versus oral antipsychotics: a meta-analysis of randomized controlled studies comparing the same antipsychotics. Schizophr Res. 2016;176(2–3):220–230. | ||
Ostuzzi G, Bighelli I, So R, Furukawa TA, Barbui C. Does formulation matter? A systematic review and meta-analysis of oral versus long-acting antipsychotic studies. Schizophr Res. 2017;183:10–21. | ||
Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr Res. 2018;197:274–280. | ||
Kimura H, Kanahara N, Sasaki T, et al. Risperidone long-acting injectable in the treatment of treatment-resistant schizophrenia with dopamine supersensitivity psychosis: results of a 2-year prospective study, including an additional 1-year follow-up. J Psychopharmacol. 2016;30(8):795–802. | ||
Hori H, Katsuki A, Atake K, Yoshimura R. Effects of continuing oral risperidone vs. switching from risperidone to risperidone long-acting injection on cognitive function in stable schizophrenia patients: a pilot study. Front Psychiatry. 2018;9(9):74. | ||
Nasrallah HA. The case for long-acting antipsychotic agents in the post-CATIE era. Acta Psychiatr Scand. 2007;115(4):260–267. | ||
Chue P, Eerdekens M, Augustyns I, et al. Comparative efficacy and safety of long-acting risperidone and risperidone oral tablets. Eur Neuropsychopharmacol. 2005;15(1):111–117. | ||
Bai YM, Ting Chen T, Chen JY, et al. Equivalent switching dose from oral risperidone to risperidone long-acting injection: a 48-week randomized, prospective, single-blind pharmacokinetic study. J Clin Psychiatry. 2007;68(8):1218–1225. | ||
Matsumoto T, Miyawaki T, Ue H, Kanda T, Zenji C, Moritani T. Autonomic responsiveness to acute cold exposure in obese and non-obese young women. Int J Obes Relat Metab Disord. 1999;23(8):793–800. | ||
Matsumoto T, Ushiroyama T, Morimura M, et al. Autonomic nervous system activity in the late luteal phase of eumenorrheic women with premenstrual symptomatology. J Psychosom Obstet Gynaecol. 2006;27(3):131–139. | ||
Moritani T, Kimura T, Hamada T, Nagai N. Electrophysiology and kinesiology for health and disease. J Electromyogr Kinesiol. 2005;15(3):240–255. | ||
Hattori S, Kishida I, Suda A, et al. Effects of four atypical antipsychotics on autonomic nervous system activity in schizophrenia. Schizophr Res. 2018;193:134–138. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington DC: APA; 1994. | ||
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. | ||
Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci. 2015;69(8):440–447. | ||
Fujibayashi M, Matsumoto T, Kishida I, et al. Autonomic nervous system activity and psychiatric severity in schizophrenia. Psychiatry Clin Neurosci. 2009;63(4):538–545. | ||
Kimura T, Matsumoto T, Akiyoshi M, et al. Body fat and blood lipids in postmenopausal women are related to resting autonomic nervous system activity. Eur J Appl Physiol. 2006;97(5):542–547. | ||
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213(4504):220–222. | ||
Pagani M, Lombardi F, Guzzetti S, et al. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ Res. 1986;59(2):178–193. | ||
Pomeranz B, Macaulay RJ, Caudill MA, et al. Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol Heart Circ Physiol. 1985;248(1):H151–H153. | ||
Rompelman O, Coenen AJ, Kitney RI. Measurement of heart-rate variability: part 1-comparative study of heart-rate variability analysis methods. Med Biol Eng Comput. 1977;15(3):233–239. | ||
Chang HA, Chang CC, Tzeng NS, Kuo TB, Lu RB, Huang SY. Cardiac autonomic dysregulation in acute schizophrenia. Acta Neuropsychiatr. 2013;25(3):155–164. | ||
Jokinen V, Syvänne M, Mäkikallio TH, Airaksinen KEJ, Huikuri HV. Temporal age-related changes in spectral, fractal and complexity characteristics of heart rate variability. Clin Physiol. 2001;21(3):273–281. | ||
Geerts H, Spiros A, Roberts P, Alphs L. A quantitative systems pharmacology study on optimal scenarios for switching to paliperidone palmitate once-monthly. Schizophr Res. 2018;9964(17):261–268. | ||
Sheehan JJ, Reilly KR, Fu DJ, Alphs L. Comparison of the peak-to-trough fluctuation in plasma concentration of long-acting injectable antipsychotics and their oral equivalents. Innov Clin Neurosci. 2012;9(7–8):17–23. | ||
Iyo M, Tadokoro S, Kanahara N, et al. Optimal extent of dopamine D2 receptor occupancy by antipsychotics for treatment of dopamine supersensitivity psychosis and late-onset psychosis. J Clin Psychopharmacol. 2013;33(3):398–404. | ||
Kakihara S, Yoshimura R, Shinkai K, et al. Prediction of response to risperidone treatment with respect to plasma concentrations of risperidone, catecholamine metabolites, and polymorphism of cytochrome P450 2D6. Int Clin Psychopharmacol. 2005;20(2):71–78. | ||
Yoshimura R, Ueda N, Nakamura J. Possible relationship between combined plasma concentrations of risperidone plus 9-hydroxyrisperidone and extrapyramidal symptoms. Neuropsychobiology. 2001;44(3):129–133. | ||
Chung MS, Yang AC, Lin YC, et al. Association of altered cardiac autonomic function with psychopathology and metabolic profiles in schizophrenia. Psychiatry Res. 2013;210(3):710–715. | ||
Moon E, Lee S-H, Kim D-H, Hwang B. Comparative study of heart rate variability in patients with schizophrenia, bipolar disorder, post-traumatic stress disorder, or major depressive disorder. Clin Psychopharmacol Neurosci. 2013;11(3):137–143. | ||
Quintana DS, Westlye LT, Kaufmann T, et al. Reduced heart rate variability in schizophrenia and bipolar disorder compared to healthy controls. Acta Psychiatr Scand. 2016;133(1):44–52. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.