Back to Journals » Clinical Ophthalmology » Volume 10
Effects of laser in situ keratomileusis on mental health-related quality of life
Authors Tounaka-Fujii K, Yuki K, Negishi K, Toda I , Abe T, Kouyama K, Tsubota K
Received 31 July 2016
Accepted for publication 18 August 2016
Published 26 September 2016 Volume 2016:10 Pages 1859—1864
DOI https://doi.org/10.2147/OPTH.S118545
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kaoru Tounaka-Fujii,1 Kenya Yuki,2 Kazuno Negishi,2 Ikuko Toda,3 Takayuki Abe,4 Keisuke Kouyama,4 Kazuo Tsubota2
1Health Center, Keio University, 2Department of Ophthalmology, Keio University School of Medicine, 3Minamiaoyama Eye Clinic, 4Center for Clinical Research, Keio University School of Medicine, Tokyo, Japan
Purpose: The aims of our study were to investigate whether laser in situ keratomileusis (LASIK) improves health-related quality of life (HRQoL) and to identify factors that affect postoperative HRQoL.
Materials and methods: A total of 213 Japanese patients who underwent primary LASIK were analyzed in this study. The average age of patients was 35.0±9.4 years. The subjects were asked to answer questions regarding subjective quality of vision, satisfaction, and quality of life (using the Japanese version of 36-Item Short Form Health Survey Version 2) at three time points: before LASIK, 1 month after LASIK, and 6 months after LASIK. Longitudinal changes over 6 months in the outputs of mental component summary (MCS) score and the physical component summary (PCS) score from the 36-Item Short Form Health Survey Version 2 questionnaire were compared between time points using a linear mixed-effects model. Delta MCS and PCS were calculated by subtracting the postoperative score (1 month after LASIK) from the preoperative score. Preoperative and postoperative factors associated with a change in the MCS score or PCS score were evaluated via a linear regression model.
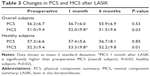
Results: The preoperative MCS score was 51.0±9.4 and increased to 52.0±9.8 and 51.5±9.6 at 1 month and 6 months after LASIK, respectively, and the trend for the change from baseline in MCS through 6 months was significant (P=0.03). PCS score did not change following LASIK. Delta MCS was significantly negatively associated with preoperative spherical equivalent, axial length, and postoperative quality of vision, after adjusting for potential confounding factors.
Conclusion: Mental HRQoL is not lost with LASIK, and LASIK may improve mental HRQoL. Preoperative axial length may predict postoperative mental HRQoL.
Keywords: laser in situ keratomileusis, refractive surgery, quality of vision, SF-36, mental health-related quality of life
Introduction
Laser in situ keratomileusis (LASIK) is one of the most established corneal refractive surgeries in the world. The safety, efficacy, and predictability following LASIK are excellent.1 Kato et al2 reported that the uncorrected visual acuity (UCVA; logarithm of the minimum angle of resolution) of patients undergoing LASIK improved from 1.27 preoperatively to −0.08 at 1 month following surgery and remained stable up to 1 year after surgery. UCVAs (logarithm of the minimum angle of resolution) >0.0 were obtained in 85% of patients at 1 month after surgery.2 In a systematic review, Solomon et al3 reported patient satisfaction rate after myopic LASIK to be 95.3% (1,811 of 1,901 patients). While there is strong evidence for visual function improvement following LASIK, it remains unclear whether LASIK also improves quality of life (QOL).4,5
Health-related quality of life (HRQoL) includes physical and mental health perceptions (http://www.cdc.gov/hrqol/concept.htm). The 36-Item Short Form Health Survey (SF-36) is a multipurpose questionnaire that evaluates mental and physical aspects of HRQoL (http://www.sf-36.org). SF-36 is one of the most widely used and standardized questionnaires for evaluating HRQoL and is capable of dissecting the mental and physical aspects of QOL through calculation of mental component summary (MCS) and physical component summary (PCS) scores.6
The aims of our study were to investigate whether LASIK improves HRQoL and to identify factors that affect postoperative QOL, using the Japanese version of SF-36 Version 2 questionnaire.7
Materials and methods
This study’s procedures conformed to the tenets of the Declaration of Helsinki and to national (Japanese) and institutional (Minamiaoyama Eye Clinic) regulations. The study was approved by the Ethics Committee of the Minamiaoyama Eye Clinic. All study subjects gave written informed consent prior to enrollment.
Subject enrollment
This is a prospective hospital-based study. A total of 213 Japanese patients (male 72 and female 141) who underwent primary LASIK at Minamiaoyama Eye Clinic between January 20, 2012, and June 6, 2013, were consecutively included and analyzed in this study. The demographic characteristics of the subjects are listed in Table 1. Of the 213 subjects who responded to the preoperative SF-36 questionnaire, 212 subjects (99.5%) responded to the SF-36 at 1 month after surgery and 114 subjects (53.5%) responded at 6 months. Among the 213 subjects, 203 subjects underwent conventional LASIK and ten subjects underwent topography-guided LASIK. We also conducted a subgroup analysis in which we excluded subjects with systemic diseases, including hypertension, Sjögren syndrome, and carcinomas, and ocular diseases, including glaucoma, atopic keratoconjunctivitis, and history of ocular surgery. In this subgroup analysis, 40 subjects were excluded and 173 healthy subjects were analyzed.
LASIK procedure
LASIK was performed on both eyes of each patient successively, using an identical method. A corneal flap was created with a femtosecond laser (IntraLase FS 60 or iFS; Abbott Laboratories, Abbott Park, IL, USA), and laser ablation was performed using an excimer laser, EC-5000 (NIDEK Co. Ltd., Aichi, Japan) or STAR S4IR (Abbott Laboratories). After surgery, antibiotic eyedrops (Cravit; Santen, Osaka, Japan) were prescribed five times per day and discontinued at 1 week postoperatively. We did not use topical steroid after surgery.
Preoperative and postoperative examination
Postoperative examinations were performed at the time of questionnaire response collection. All the subjects underwent slit lamp microscopy, including fundus examination, noncorrected visual acuity (NCVA) assessment, best-corrected visual acuity (BCVA) assessment, pupil diameter measurement (OPD-Scan II; NIDEK Co. Ltd.), and axial length measurement (IOLMaster 500; Carl Zeiss Meditec AG, Jena, Germany). The ocular surface was stained with 2 μL of 1% preservative-free fluorescein solution instilled into the conjunctival sac. Tear break-up time (BUT) was defined as the interval between the last complete blink and the first disturbance of the stained corneal tear film. Fluorescein staining was graded from 0 to 3 for each cornea, according to the extent of staining: 0, negative; 1, scattered minute; 2, moderate spotty; and 3, diffuse blotchy staining. We measured BUT and fluorescein staining preoperatively and 1 month after LASIK. The patients were asked to report any history of systemic or ocular disease and any medications they were taking before LASIK. The changes in NCVA, BCVA, BUT, and fluorescein scores are listed in Table 2.
Assessment of QOL, quality of vision, ocular symptoms, and satisfaction
QOL was assessed by the Japanese version of SF-36 Version 2, for which the reliability and validity have been reported with normative data, and is considered to be appropriate for those aged 20–70 years.6,7 Subjects were asked to answer each of the 36 questionnaire items in terms of the past 4 weeks. These 36 items related to the following eight scales of QOL: physical functioning, role-physical, bodily pain, general health perception, vitality, social functioning, role-emotional, and mental health. MCS and PCS scores were then calculated from these eight scale scores according to the manual. Delta MCS was calculated by subtracting the preoperative MCS value from the MCS value 1 month after LASIK. Delta PCS was calculated using the same method.
All participants were also asked to complete a separate questionnaire. We surveyed quality of vision and ocular symptoms 1 month after LASIK by asking questions about quality of far-vision, quality of near-vision, halo, glare, double vision, and asthenopia using a response scale of 0–4 (0= very good, 1= good, 3= bad, and 4= very bad). We also surveyed patient satisfaction with LASIK outcome 1 month and 6 months after surgery by asking patients to grade outcome satisfaction on a scale of 1–4 (1= very satisfied, 2= satisfied, 3= not very satisfied, and 4= not satisfied at all). The subjects who responded with 1 or 2 were defined as subjects who were satisfied. The satisfaction rate was calculated by dividing the number of subjects who were satisfied by the number of subjects who answered this question. QOL assessment and questionnaires were completed before LASIK and 1 month ±1 week and 6 months ±1 month after LASIK.
Statistical analysis
A trend in change from baseline over 6 months in MCS, PCS, UCVA, spherical equivalent, BUT, and fluorescein scores before LASIK and 1 month and 6 months after LASIK was compared using a linear mixed-effects model. This model contains change from baseline at each time point as a response and month (degree of freedom =1) as a fixed effect and patient as a random effect.
In the univariate analysis, the correlation between preoperative MCS, delta MCS, and the preoperative factors age, NCVA, BCVA, spherical equivalent, axial length, pupil diameter, BUT, and fluorescein score was analyzed by Pearson’s correlation coefficient or Spearman’s correlation coefficient.
Multivariate analysis was used to investigate the association between preoperative factors and delta MCS. Specifically, delta MCS was treated as an independent variable in a linear regression model by adjusting for preoperative factors, including age, sex, axial length, presence of systemic disease, BUT, pupil diameter, and fluorescein score. To investigate the association between postoperative factors and delta MCS, we evaluated delta MCS as an independent variable using a linear regression model by adjusting for confounding factors, including age, sex, postoperative NCVA, spherical equivalent, BUT, fluorescein score, and postoperative symptoms.
PCS and delta PCS were also analyzed by the same method.
A P-value of <0.05 was considered statistically significant. All statistical analyses were performed using SPSS software, Version 21 (IBM Corporation, Armonk, NY, USA).
Results
Changes in MCS and PCS scores before and after LASIK are listed in Table 3. Compared with the preoperative score, the MCS score was significantly improved 1 month after surgery (P=0.03). However, no significant difference was observed between preoperative MCS score and MCS score 6 months after LASIK (P=0.99). Similar results were obtained when the analysis was restricted to healthy subjects, with significant MCS score improvement over preoperative baseline at 1 month after surgery (P=0.02). Again, no significant difference was observed between preoperative MCS score and MCS score 6 months after LASIK (P=0.99). No significant change was observed in the PCS score after LASIK (P=0.54) at either time point in either subject group.
In a univariate analysis, spherical equivalent (r=0.16, P=0.02 in the right eye; r=0.16, P=0.02 in the left eye) was correlated with delta MCS. In healthy subjects, spherical equivalent (r=0.22, P=0.005 in the right eye; r=0.21, P=009 in the left eye), axial length (r=−0.20, P=0.02 in the right eye; r=−0.25, P=0.002 in the left eye), and NCVA (r=−0.23, P=0.005 in the right eye; r=−0.25, P=0.002 in the left eye) were correlated with delta MCS. Other included factors were not correlated with delta MCS. No factor was correlated with PCS in either subject group.
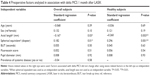
In a stepwise multiple linear regression analysis, the association between delta MCS and preoperative factors was calculated and is listed in Table 4. Delta MCS was significantly related to preoperative spherical equivalent and axial length in both groups. Other factors were not associated with delta MCS. No preoperative factors were associated with delta PCS.
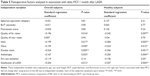
Table 5 lists the associations between delta MCS and postoperative factors. The severity of halo, glare, double vision, and asthenopia were all negatively correlated with delta MCS. The satisfaction rate for LASIK was positively correlated with delta MCS. All included variables were significantly associated with delta MCS after adjustment for possible confounding factors. No postoperative factors were associated with delta PCS.
Discussion
In this study, we showed that LASIK may improve mental HRQoL 1 month after surgery.
Some studies have shown that LASIK improves patients’ QOL. Schein et al8 evaluated the effect of LASIK on vision-related QOL using the questionnaire the Refractive Status and Vision Profile and showed that LASIK significantly improved vision-related psychological concern and physical function. Awwad et al evaluated psychological and role/social QOL in 30 myopic subjects who underwent wavefront-guided LASIK using another survey based on four vision-related QOL questionnaires: the National Eye Institute Refractive Error Quality of Life, the Refractive Status and Vision Profile, the Quality of Life Impact of Refractive Correction, and the Myopia-Specific Quality of Life. In this study, the authors showed that the indicators of psychological well-being, such as energy level, stress level, self-confidence, self-esteem, expectation for the future, and sense of safety, were each significantly improved (10%–25%) after LASIK.9 Lee et al5 examined QOL change following LASIK using the Myopia-Specific Quality of Life Questionnaire and reported that LASIK improved the psychological well-being score by 36%. However, Lazon et al10 evaluated multidimensional QOL using the Institute for Eye Research’s multidimensional QOL scale before and after LASIK, but was unable to detect a statistical difference. Therefore, in agreement with our results, the majority of studies have demonstrated a positive effect of LASIK on mental HRQoL. Importantly, however, the questionnaires used in previous studies were based on vision-related QOL, which may be predicted to be directly affected by vision improvement surgery.5,8–11 In our study, we used a nonvision-related health questionnaire to convincingly demonstrate that LASIK improves mental HRQoL.
Surprisingly, no significant improvement was observed in HRQoL after 6 months of LASIK, although neither the visual outcome nor the satisfaction rate changed significantly between 1 month and 6 months after surgery. More than 90% of the subjects were satisfied with LASIK after 6 months of surgery. The adaptation theory of well-being, which posits that good and bad events temporarily affect happiness, but people quickly adapt back to hedonic neutrality after 6–12 months of the event, may explain the results.12 Suh et al13 found that good and bad life events affected happiness only if they occurred in the past 2 months. In this case, the postoperative MCS score would revert back toward the preoperative score by 6 months post LASIK.
The preoperative MCS score in our study was 51.0. The average age of subjects in our study was 36.0 years. The average MCS score for 20-to-29-year-old and 30-to-39-year-old Japanese subjects was 48.4 and 48.8, respectively. Therefore, the MCS score in our study is slightly higher but overall comparable with the Japanese norm.6,7 The preoperative PCS score in our study was 56.2. The average PCS scores for 20–29-year-old and 30–39-year-old Japanese subjects were 56.1 and 53.6, respectively.6,7 Together, this suggests that our data are reasonable and compatible with those of the normal Japanese population.
Severity of halo, glare, double vision, asthenopia, and low satisfaction of LASIK 1 month after surgery were significantly associated with decreased MCS score. These results suggest that reduced QOL is associated with reduced mental HRQoL. Delta MCS was significantly associated with preoperative spherical equivalent and axial length in the univariate and multivariate analyses in both subject groups. This result suggests that myopic patients who have severe myopia may experience reduced mental HRQoL after LASIK.
This study is subject to several limitations. First, we were unable to gather data from every subject who underwent LASIK, which may introduce bias. Second, information about education, marital status, and income, each of which is a potentially confounding factor, was not collected or analyzed in this study. Another limitation of our study is that 50% of our 1-month eyes did not provide 6 months data. Long-term result would be valuable such as week data.
This study can conclude that quality of life is not lost with LASIK.
LASIK may improve mental HRQoL. Both preoperative axial length and spherical equivalent may be a predictor of change in the MCS score after LASIK. Poorer postoperative quality of vision is associated with lower mental HRQoL.
Acknowledgment
The authors are grateful to Doctor Sheri Perterson for her valuable comments.
Disclosure
The authors report no conflicts of interest in this work.
References
Wilson SE. Clinical practice. Use of lasers for vision correction of nearsightedness and farsightedness. N Engl J Med. 2004;351(5):470–475. | ||
Kato N, Toda I, Hori-Komai Y, Sakai C, Tsubota K. Five-year outcome of LASIK for myopia. Ophthalmology. 2008;115(5):839–844. | ||
Solomon KD, Fernandez de Castro LE, Sandoval HP, et al; Joint LASIK Study Task Force. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691–701. | ||
Mitka M. FDA focuses on quality-of-life issues for patients following LASIK surgery. JAMA. 2009;302(22):2420–2422. | ||
Lee J, Lee J, Park K, Cho W, Kim JY, Kang HY. Assessing the value of laser in situ keratomileusis by patient-reported outcomes using quality of life assessment. J Refract Surg. 2005;21(1):59–71. | ||
Fukuhara S, Ware JE Jr, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J Clin Epidemiol. 1998;51(11):1045–1053. | ||
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 health survey for use in Japan. J Clin Epidemiol. 1998;51(11):1037–1044. | ||
Schein OD, Vitale S, Cassard SD, Steinberg EP. Patient outcomes of refractive surgery. The refractive status and vision profile. J Cataract Refract Surg. 2001;27(5):665–673. | ||
Awwad ST, Alvarez-Chedzoy N, Bowman RW, Cavanagh HD, McCulley JP. Quality of life changes after myopic wavefront-guided laser in situ keratomileusis. Eye Contact Lens. 2009;35(3):128–132. | ||
Lazon de la Jara P, Erickson D, Erickson P, Stapleton F. Visual and non-visual factors associated with patient satisfaction and quality of life in LASIK. Eye(Lond). 2011;25(9):1194–1201. | ||
Queirós A, Villa-Collar C, Gutiérrez AR, Jorge J, González-Méijome JM. Quality of life of myopic subjects with different methods of visual correction using the NEI RQL-42 questionnaire. Eye Contact Lens. 2012;38(2):116–121. | ||
Diener E, Lucas RE, Scollon CN. Beyond the hedonic treadmill: revising the adaptation theory of well-being. Am Psychol. 2006;61(4):305–314. | ||
Suh E, Diener E, Fujita F. Events and subjective well-being: only recent events matter. J Pers Soc Psychol. 1996;70(5):1091–1102. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.