Back to Journals » Therapeutics and Clinical Risk Management » Volume 17
Effects of Impacted Lower Third Molar Extraction on Periodontal Tissue of the Adjacent Second Molar
Authors Zhang Y, Chen X, Zhou Z, Hao Y, Li H, Cheng Y, Ren X, Wang X
Received 18 December 2020
Accepted for publication 5 March 2021
Published 22 March 2021 Volume 2021:17 Pages 235—247
DOI https://doi.org/10.2147/TCRM.S298147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Yuan Zhang,1,2,* Xiaohang Chen,1,2,* Zilan Zhou,1,2 Yujia Hao,1,2 Huifei Li,1,2 Yongfeng Cheng,1,2 Xiuyun Ren,1,2 Xing Wang1,2
1Shanxi Medical University School and Hospital of Stomatology, Taiyuan, 030001, People’s Republic of China; 2Shanxi Province Key Laboratory of Oral Diseases Prevention and New Materials, Taiyuan, 030001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xing Wang; Xiuyun Ren
Shanxi Medical University School and Hospital of Stomatology, Taiyuan, 030001, People’s Republic of China
Email [email protected]; [email protected]
Abstract: The extraction of impacted lower third molars (ILTM) is one of the most common procedures in oral-maxillofacial surgery. Being adjacent to lower second molars, most impacted lower third molars often lead to distal periodontal defects of adjacent second molars. Several symptoms may occur after extraction, such as periodontal pocket formation, loss of attachment, alveolar bone loss and even looseness of second molar resulting in extraction. The distal periodontal defects of second molars are affected by many factors, including periodontal conditions, age, impacted type of third molars, and intraoperative operations. At present, several studies have suggested that dentists can reduce the risk of periodontal defects of the second molar after ILTM extraction through preoperative evaluation, reasonable selection of flap design, extraction instruments and suture type, and necessary postoperative interventions. This review summarizes the research progress on the influence factors, interventions methods and some limitations of distal periodontal defects of adjacent second molar after extraction of impacted mandibular third molars, with the aim of opening up future directions for studying effects of ILTM extraction on periodontal tissue of the adjacent second molar.
Keywords: impacted lower third molar, periodontal defect, alveolar bone defect, second molar, teeth extraction
Introduction
Impacted Lower Third Molar(ILTM), with an incidence of 66–77%,1 is the most common impacted tooth. Due to the abnormal position and blocked eruption, ILTM often leads to recurrent wisdom tooth pericoronitis, adjacent tooth caries, lower anterior arch crowding, periodontal defects of adjacent molars, tooth root resorption and even temporomandibular joint disorders.2 Most scholars believe that ILTM with pathological symptoms, especially mid-to-high mesial inclination, should be prophylactically removed early.3
ILTM extraction is more likely to have surgical complications than normal tooth extraction as a result of adjacent teeth obstruction and bone tissue embedding. Common postoperative complications, including pain, swelling, infection and local bleeding, can be effectively controlled by timely symptomatic treatment.4 Other complications, such as adjacent tooth injury, will affect mid-long-term prognosis of the tooth when it occurs.5 Due to the lack of obvious subjective symptoms in a short term, dentists often ignored the effect of ILTM extraction on the periodontal health of the second molar. Therefore, oral surgeons often perform few treatments on the second molar after ILTM extraction.
At present, there is a growing interest in the influence of ILTM extraction on the periodontal health of second molars. The main methods to evaluate the effect of ILTM extraction on the second molar periodontal tissue are periodontal examination and imaging examination. Commonly used indicators are periodontal pocket depth (PPD), clinical attachment loss (CAL), and distal bone level of the second molar. Using 215 ILTM surgery cases and after 2 years, Kugelberg et al6 found that on the distal of the adjacent second molar, 43.3% has probing depth more than 7mm, and 32.1% has intrabony defects more than 4mm. Also, thanks to periodontal defects, plaque accumulation and local inflammation were further accelerated, which cause the second molar periodontal-endodontic combined lesions and even early tooth loss.7 Therefore, during the ILTM extraction surgery, dentists should consider the periodontal health of second molars.
Several studies have suggested that dentists can reduce the risk of periodontal defects of the second molar after ILTM extraction through preoperative evaluation, reasonable selection of flap design, extraction instruments and suture type, and necessary postoperative interventions. So we reviewed the influence factors, and intervention methods of distal periodontal defects of adjacent second molar after ILTM extraction.
Preoperative Evaluation
ILTM extraction is one of the most common procedures in oral-maxillofacial surgery. Detailed consultation, clinical and imaging examinations are still required before surgery to design the best surgical procedure and minimize the damage to the periodontal tissues.
Periodontal Status
Generally, second molars periodontal status was evaluated through consultation, clinical and imaging examinations, specifically including periodontitis history, intrabony defects (IBD), deep periodontal pockets, plaque accumulation, and gingival inflammation. Studies have indicated that the preoperative periodontal condition influences the postoperative periodontal condition of the second molars. Through multiple regression analysis, Kugelberg et al8 showed that the size of the distal bone defect of the second molar after surgery is related to the preoperative periodontal status. Passarelli et al9 found that compared with non-periodontitis patients, patients with periodontitis history have 41 times probability of periodontal disease (PPD>4mm). The preoperative PPD is more than 7mm, and the PPD is still more than 4mm at postoperative 6 months.
ILTM Impacted Type
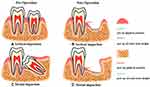
According to the relationship between the long axis of ILTM and the adjacent second molars, Winter classified ILTM into vertical impaction, mesial impaction, distal impaction, horizontal impaction, and inverted impaction.10 Kim et al11 indicated that the incidence of distal alveolar bone loss in the adjacent second molars is closely related to the ILTM impacted type (Figure 1).
The research by Kugelberg et al12 showed that the type of impacted third molars that are most likely to form periodontal pockets and bone defects in the distal part of the second molars is the mesial impaction, followed by the horizontal impaction, and the vertical impaction is the lowest.13 It was so hard to maintain oral hygiene in the mesial or horizontal impaction, resulting in the accumulation of plaque microorganisms, and then the formation of periodontal pockets and alveolar bone loss in the distal adjacent second molars.14
In addition, for non-eruptive ILTM, it can be divided into completely impacted (completely in bone) and submucosal impacted (completely covered by oral mucosa), which have different effects on postoperative periodontal tissues. Studies have shown that if there is a bone plate above the ILTM, the postoperative PPD and CAL levels only have a little change.15 This is consistent with a recent study by Nunn et al, who found that a significantly increased risk of submucosal ILTM periodontal defect compared with complete ILTM, with a 4.8-fold increase after submucosal ILTM removal and only a 1.7-fold increase after complete ILTM removal.16 Complete ILTM removal usually only has buccal defects, while the submucosal ILTM already has a coronal bone wall missing, and the buccal bone wall usually needs to be partially removed intraoperatively. Especially in the coronal plane, the ILTM is in close contact with the second molar, and there is no obvious bone boundary, which will cause greater defects in the distal periodontal tissue of the second molar after surgery.17
Age of Patients
The difficulty of ILTM extraction increases with age, owing to continuous root development, periodontal ligament thinning, ankylosis of the tooth, mandible becomes harder and brittler, and hypercementosis.18 Many studies suggested that the best extraction period is before the age of 25, from which complications increase significantly and healing time is longer.19 In a case-control study of 868 patients, Chiapasco et al20 reported that the PPD of the distal second molar after the third molar surgery over 25 years old was 3 times that of those before 25 years old. Through a retrospective study, Kugelberg et al21 showed significant differences in the level of bone defect between 2 and 4 years after ILTM extraction. Two years after tooth extraction, patients ≤25 years old had l6.7% of bone defects exceeding 4mm in the distal second molar, 40.7% of patients >25 years old had bone defects exceeding 4mm. After 4 years, the former dropped to 4.2%, while the latter rose to 44.4%, indicating that ILTM extraction before the age of 25 may have a beneficial effect on periodontal health of the second molar.
Currently, some recognized risk factors for preoperative evaluation include periodontal status, ILTM impacted type and age of patients. Thus, ILTM extraction often leads to the risk of sustainable periodontal defects or forming new periodontal defects in the distal second molar after surgery, which mostly occurs in the following situations: ①Mesial or horizontal impaction of mandibular third molars; ②Age >25 years old; ③Preoperative probing depth exceeding 7mm, attachment loss exceeding 6mm; ④Patients with periodontal inflammation, poor oral hygiene, and poor plaque control.
Tooth Extraction Operation
ILTM is often hindered by adjacent tooth, bones, and soft tissues, which requires flap surgery, bone removal, tooth separation and soft tissue suture during extraction process. Flap design, bone removal and suture may affect the distal periodontal health of the second molar after surgery. To reduce the influence of ILTM extraction, scholars have designed different flap approaches, extraction instruments used to remove bone and split teeth and suture type.
Flap Design
Each step of the mucoperiosteal flap will break the homeostasis of the alveolar bone and activate osteoclasts.22 After ILTM surgery, an important factor affecting the periodontal healing of second molars is the remaining amount of periodontal ligaments and gingival fibers.23 In the case of a thin gingival biotype, the design of the standard flap may lead to attachment loss and periodontal pockets formation of the second molar.24 The modified design of standard flaps, such as triangular, Szmyd and envelope flaps, which moved 1–2mm down from the standard incision line that preserves the periodontal ligament adjacent to the second molar and the attached gingiva to the buccal surface can reduce potential periodontal complications of the adjacent second molars25 (Figure 2).
 |
Figure 2 Illustration of the flap designs used in impacted mandibular third molar extraction: (A) standard envelope flap, (B) standard triangular flap, (C) Szmyd flap, (D–F) modification flaps. |
Multiple studies suggested that the correct flap design is beneficial to periodontal health in the short term. Suarez-Cunqueiro et al26 evaluated the effects of triangular flaps and modified triangular flaps on the periodontal condition of the second molar after ITLM extraction. At 5 and 10 days postoperatively, they observed that compared with the triangular flap, the modified triangular flap design can reduce the PPD of the distal second molar, indicating that the modified triangular flap is more beneficial to postoperative periodontal health. Similarly, Kirtiloğlu et al27 reported that the modified Szmyd flap has a smaller probing depth than the triangular flap at 1 week, 2 weeks and 4 weeks after surgery. Also, the preoperative and postoperative plaque index and gingival index are similar, revealing that the early differences between the two flap designs are not caused by plaque accumulation, but may be related to the preservation of the intact gingival margin around the second molar and no crevicular incision.
Clinical studies have shown that it takes at least 3 months for the distal periodontal healing of the second molars.28,29 Therefore, the relevant indicators of periodontal status 3 months after extraction have evaluation significance. In a systematic review and meta-analysis, Chen et al30 used cases followed up for at least 3 months to assess the effect of different flap designs on periodontal status. They showed that the Syzmd flap and modified flap design may be the most effective way to reduce the postoperative probing depth. Comparing the effects of the envelope flap and the triangular flap on the periodontal condition of the adjacent second molars, Korkmaz et al31 found that probing depth of the triangular flap was significantly less than that of the envelope flap at 3 months after surgery. Therefore, compared with the envelope flap, the triangular flap design is better for periodontal health (Table 1).
 |
Table 1 Clinical Periodontal Characteristics of Flap Design |
The above research shows that different flap designs affect the probing depth of the postoperative periodontal pocket. Compared with the triangular flap design, the Syzmd flap and the modified flap are more beneficial to periodontal health, while the triangular flap design is better than the envelope flap.
Extraction Instrument
Chisels, a common tool in traditional tooth extractions, are used to remove bones and split teeth, which are likely to bring about inevitable postoperative trauma.33 With the development of minimally invasive concept, minimally invasive tooth extraction instruments, including ultrasonic bone knife, 45° contrast-angle turbine handpiece, elongated impacted tooth bur, modified minimally invasive dental elevator (thinner edge), and buccal retractor, has been widely used.34 The different ILTM extraction instruments affect the second molar not only in postoperative reaction but in the periodontal health. Coomes et al shown that after using a traditional chisel to split the crown of the mandibular third molar, which appeared a fracture seam of 0.47 to 0.7 mm on the buccal plate.35 Araujo MG et al36 suggested that the fracture of the buccal bone plate had adverse effects on the adjacent teeth, such as the alveolar bone resorption. Wang et al37 compared the alveolar bone healing after traditional bone removal and minimally invasive high-speed turbine tooth extraction. The result showed that the alveolar bone density after the minimally invasive tooth extraction group was higher than conventional tooth extraction group at 7 days and 30 days, and the difference was significant (p < 0.05). In the accuracy and safety of bone removal, the ultrasonic bone knife is better than the high-speed turbine. It can not only reduce postoperative swelling, pain and soft tissue damage but also avoid the negative effects of high-speed turbines, such as osteonecrosis caused by heat generation. The use of ultrasonic osteotome can reduce the distal bone defect of the adjacent second molar and increase the alveolar bone density in the surgery area.38 Therefore, ultrasonic osteotome can better preserve the bone mass in the distal second molars. The above results show that traditional tooth extractions surgery causes different degrees of periodontal damage, while minimally invasive tooth extractions surgery can effectively promote alveolar bone healing.
In addition, for the lower ILTM, conventional minimally invasive tooth extraction surgery may still result in bone loss and periodontal pockets formation in the distal second molar.39 Therefore, scholars designed ultrasonic osteotome window: using ultrasonic osteotome to open a window on the mandibular buccal bone plate, removing tooth, and resetting bone fragments.40 The extraction socket formes a closed space that effectively isolates the growth of epithelial cells to benefit bone tissue regeneration41 and shortens the healing time.
Suture Type
Suture is the last step in the ILTM extraction procedures. The close suture of the extraction wound can improve postoperative wound healing.42 However, studies have shown that different suture types have different effects on the periodontal tissue.43 Widely used interrupted sutures are usually the surgeon’s first choice. The anchor suture is another suture technique, which fixes the distal buccal-lingual gingival flap to the adjacent tooth in an anchor-like manner to avoid the V-shaped gap formation in the distal adjacent tooth. Cetinkaya et al44 compared the effects of interrupted sutures and anchor sutures on the periodontal tissue of the adjacent second molar 6 months after ILTM extraction. They found that the PPD and CAL of distal second molars in the interrupted suturing group were significantly higher than those in the anchored suturing group, indicating that anchor sutures may be a better choice, to maintain the health of periodontal tissues and prevent periodontal problems. Furthermore, Zhu et al45 adopted the self-comparison research method and found that interrupted suture and “8” suture were statistically significant in terms of PPD at 6 months after surgery. The “8” suture is more conducive to the healing of the distal periodontal tissue of the adjacent teeth, which may make the mucosal epithelium closer to the distal root surface of the adjacent tooth to form a barrier to prevent food debris from embedding, thereby protecting the periodontal tissue in this area for regeneration and restoration.46 The above studies show that anchor suture and “8” suture are more beneficial to periodontal tissue healing than interrupted suture. Currently, no controlled studies of other suture types have been reported and need to be further studied.
Postoperative Intervention of ILTM Extraction on Periodontal Effects of Second Molars
Surgical extraction of ILTM will increase the risk of persistent or developing new periodontal defects in the distal second molar. Over the years, scholars have proposed different interventions to promote periodontal tissue regeneration, including non-surgical periodontal treatment, guided tissue regeneration, bone graft, filling collagen sponge, transplantation of cell active ingredients and so on (Figure 3). Space provision, wound stabilization and cell induction are the key factors, which can be obtained by using these technologies.
 |
Figure 3 Endogenous tissue engineering for periodontal regeneration. |
Non-Surgical Periodontal Treatment
Scaling and root planing, as the main methods of periodontal basic treatment, is widely used in clinic. Pons-Vicente et al47 compared the effects of ultrasound and simple manual scaling and root planing on the distal second molar after ILTM extraction. The results show that there is no significant difference between the two treatment methods on the distal periodontal tissue of the second molar. Because periodontal treatment can completely remove the plaque and calculus, which locate on the distal surface of the second molar and expose on the root surface. After ILTM extraction, relevant periodontal treatment intervention can provide strong conditions for the recovery of the distal periodontal tissue of the second molar.48 Xie et al49 performed ILTM extraction combined with simultaneous periodontal treatments. After 6 months, they found that plaque index, gingival index, bleeding index, probing depth of periodontal pocket and bone loss in the experiment group was significantly lower than those in the control group, indicating that periodontal treatment can make the distal alveolar bone of the adjacent second molar more flatter, which is beneficial to eliminate periodontal pockets and intrabony defects. Also, the elimination of periodontal pocket benefits plaque control, gingiva health and accelerates wound healing.50,51
Guided Tissue Regeneration
Guided tissue regeneration (GTR) technology uses biocompatible barrier membranes (absorbable or non-absorbable) between the bone defect area and the surrounding tissues as a barrier, which prevents gingival epithelium and connective tissue from infringing the root surface during the healing process while allowing the periodontal cell to selectively migrate into the defect. In this way, the new cementum and periodontal ligament fibers are formed, that is, the formation of new adhesive healing. Cortell-Ballester et al52 initiated an experiment after ILTM extraction, setting an absorbable collagen membrane placed on one side and a blank control on the other side. Six months after surgery, PPD and CAL of the distal second molars in the experimental group were significantly reduced compared with those in the control group, indicating that the absorbable collagen membrane can stimulate bone regeneration, improve the attachment level and bone filling, reduce the probing depth, and lead to faster healing of periodontal tissues. Similar to the former experimental design, Corinaldesi et al53 evaluated 11 cases of bilateral mandibular second molars with preoperative PD ≥6mm and bone defect ≥3mm to GTR using absorbable collagen membrane and non-absorbable collagen membrane. The results confirmed that the absorbable collagen membrane had the same effect as the non-absorbable membrane in terms of the probing depth and attachment loss. Both treatment methods were successful 9 months after surgery.
Bone Graft
Although autologous bone graft remains the “gold standard” for bone regeneration,54 it can also aggravate patient’s injury and limit by the patient’s own bone mass.55 Therefore, it is recommended to use bone substitute materials or autogenous bone with bone substitute materials.56
Bone substitute materials include allograft bone, xenograft bone and synthetic bone. Due to immunogenic reaction, disease transmission, ethical problems and infection risks, allograft bone is currently rarely used in the repair of distal bone defects in the second molar after ILTM extraction.57 In the synthetic bone substitute materials, hydroxyapatite (HA) and bioactive glass are mainly used for bone defect repair. Singh et al suggested that HA with collagen membrane can increase bone regeneration in distal bone defects of second molars, but it is no longer used for repairing bone defects because of its degradability and poor plasticity.58 Throndson et al59 demonstrated that bioactive glass had a good effect on CAL, but no significant change in bone height, indicating that its osteogenic effect was poor. However, xenograft bone is widely used in clinical practice, among which the most commonly used is Geistlich Bio-Oss®. Emerging investigations are demonstrating that single Bio-Oss materials can promote the repair of periodontal bone defects.60 Sammartino et al61 further also confirmed that both single Bio-OSS and the mixture can significantly decrease CAL and PPD, promote distal bone regeneration of the second molars, and the combined effect is better after ILTM extraction.
Filling Collagen Sponge
Collagen sponge, a kind of biomedical material with a similar structure to human collagen, is the main constituent protein of the extracellular matrix and an important component of tissues and scaffolds for cells.62 Studies have shown that filling the collagen sponge after ILTM extraction benefits the migration of osteoblasts, stabilizes blood clots, promotes soft tissue healing, and protects wounds and bone reconstruction.63 Clinically, collagen sponge has been mainly used to prevent and repair periodontal defects. Wang et al64 have found that the alveolar bone loss in the experimental group (filling collagen sponge after the mesial ILTM extraction) was significantly reduced compared with the control group, indicating that collagen sponge prevents postoperative periodontal defects and maintains the periodontal health of the second molars. In addition, Kim et al65 also proved that the placement of absorbable collagen sponge reduced the periodontal probing depth and accelerated the healing of periodontal defect in the adjacent second molars.
Transplantation of Cell Active Ingredients
Cell active component transplantation implants various cell active components into the extraction socket, such as platelet-rich plasma (PRP), platelet-rich fibrin (PRF), concentrated growth factor (CGF) and other blood platelet concentrates. Cell active component transplantation stimulates cell proliferation, repairs bone defects and promotes bone regeneration by releasing various growth factors.66 Multiple studies reported that PRP can promote alveolar defects healing and new bone formation after ILTM extraction, and reduce postoperative reactions. Gandevivala et al67 put the PRP into the extraction socket, and the experimental group was significantly different from the control group in terms of PPD. Similarly, Bhujbal et al68 conducted the same study and found that the average bone density of the PRP group was significantly higher than that of the control group. Doiphode et al69 further evaluated the repair effect of PRP and PRF on bone defects, and found that PRF improved periodontal health more significantly.
The periodontal management of the adjacent second molar after ILTM extraction is challenging in clinicians. Different interventions can restore the original periodontal structure and a functional attachment to promote periodontal tissue regeneration. These interventions have good clinical effects in the treatment of periodontal defects, and can be used as treatment to prevent periodontal complications after third molar extraction (Table 2)
 |
Table 2 Clinical Periodontal Characteristics of Bone Regeneration Techniques |
Limitations of Current Research
Insufficient Attention of Oral Surgeons
The ILTM extraction is a complicated surgery because of its special location, adjacency to important anatomical structures and small surgical fields. Extraction involves the manipulation of both soft and hard tissues, so the patient usually experiences pain, swelling, trismus, inferior alveolar nerve and lingual nerve injury in the immediate postoperative period. Generally, these complications seriously affect the patient’s quality of life and have attracted great attention from clinicians, which is why they can be well controlled in a short term. However, postoperative complications are not limited to these, periodontal defects in the distal part of adjacent second molars often occurs. Due to the lack of obvious subjective symptoms, clinicians often ignore them and do not receive timely postoperative treatment, leading to plaque accumulation and local inflammatory diseases, which eventually affects the mid-long-term prognosis of second molars.5
Different Periodontal Examination Methods
Periodontal examination methods comprised periodontal probing and imaging evaluation, but different examination methods may show the state of the disease unilaterally, bringing different experimental results. Periodontal probing, including common periodontal probe and the electronic periodontal probe, can detect the PPD and CAL. Compared with electronic periodontal probing, the accuracy of common periodontal probes is greatly affected by subjective factors (probing intensity, angle and so on), patient cooperation, soft tissue inflammation.70 Therefore, the experimental data obtained by using different periodontal probe have a large error, leading to wrong conclusions. Imaging methods, including curved tomography and cone-beam CT (CBCT), can assess the distal bone level of the second molar. Assessing the same group of patients, curved tomography showed that 62.9% of patients had bone defects, while CBCT showed that 80% of patients had bone defects, indicating a significant difference between the two methods.71 Compared with CBCT, curved tomography underestimated the severity of the distal bone defect of the second molar (p <0.05). It is currently believed that CBCT can assess the level of alveolar bone more detail and reliability.
Different Periodontal Evaluation Indicators
PPL, CAL, alveolar bone height and density are often used to evaluate the influence of ILTM extraction on the periodontal health of adjacent second molars. However, there is currently no recognized index and index standard for this, four indicators are rarely used at the same time after tooth extraction, and normally only one or two of them are used, which may not accurately describe the actual periodontal condition. Christiaens et al72 believed that the diagnosis of periodontal disease should combine clinical examination index (including PPD and CAL) with imaging analysis, which has high diagnostic sensitivity. Therefore, combining the four evaluation indicators can more objectively and accurately study the periodontal effect of ILTM extraction on the adjacent second molars.
Different Standards for Periodontal Probing
When performing periodontal probing on the distal of the second molar before and after ILTM extraction, some scholars focused on a specific location, and some scholars focused on the average of 2–3 locations. Tabrizi et al73 thought that if there are pre-operative intrabony defects and iatrogenic injury during third molar surgery, it is more valuable that the periodontal parameters are measured at three sites at the distal part of the second molar to provide a more accurate and visible periodontal condition. However, only a few scholars74 selected five sites around the distal second molars, that is, buccal, dis-buccal, mid-distal, dis-lingual, lingual. They believed that multi-site measurements permitted the detailed assessment of the distal periodontal status of the second molar in an unprecedented way, although greatly complicates the analyses of the results.
Critical Consideration
Since the 1980s, many studies have focused on the relationship between ILTM and periodontal health, as well as the impact of ILTM extraction on periodontal tissue health.75 In our previous study, ILTM extraction resulted in periodontal tissue defects in adjacent second molars.73,76,77 However, there are some controversies in the scientific literature. Blakey et al78 investigated the periodontal pathology following asymptomatic ILTM extraction. Preoperatively, the sites with PPD ≥4mm in the distal second molars was 6.6%, while the postoperative reduction was 1.4%. The same research was done by Pham et al.79 After 3 and 6 months, PPD decreased and bone level increased, which was statistically significant, further indicating that ILTM extraction contributes to periodontal health of the distal second molar. Besides, Dicus-Brookes et al80 evaluated the effect of ILTM extraction with mild pericoronitis on the periodontal status of adjacent second molars and found that significantly fewer patients (46%) had at least one site PPD ≥4mm in the distal second molar after 3 months compared with before surgery (88%). These results demonstrated that ILTM extraction significantly improved the distal periodontal condition of the second molar and had a positive effect on the overall periodontal health. Careful analysis revealed that the study sample lacks homogeneity. Moreover, different studies use different periodontal evaluation indicators and imaging methods to assess periodontal conditions. Technical errors are often not considered, and there is a lack of detailed assessment of periodontal tissue healing. Therefore, further standardized studies are needed in the current literature to determine the effect of ILTM extraction on periodontal healing.
Conclusion and Perspectives
The periodontal condition of the adjacent second molars is affected by many factors, including preoperative periodontal status, ILTM extraction time, impacted type, flap design, extraction instruments and suture type. To minimize the periodontal damage of the adjacent second molars, it is recommended that the ILTM extraction should be evaluated by preoperative consultation, clinical and imaging examinations. The reasonable flap design, suture type and minimally invasive tooth extraction surgery will reduce periodontal damage. Whether to perform periodontal interventions is based on preoperative evaluation and intraoperative procedures. Valid postoperative periodontal interventions promote the repair of the distal periodontal defects of the second molars. However, owning to the inconsistency of indicators, there is a lack of effective comparison in the literature regarding which intervention offers the better postoperative periodontal healing, so a larger sample size must be needed to validate in the future. As far as current research is concerned, there are still some limitations in the effect of ITLM extraction on the periodontal tissue of adjacent second molars, which need to be further improved.
Funding
This work was supported by Shanxi Province Key Research and Development Program (201903D321148), National Natural Science Foundation of China (81801004 and 82071155), Scientific and Technological Innovation Programs of Higher Education Institutions in Shanxi (2019L0438 and 2020L0209), Graduate Education Innovation Project of Shanxi Province (2020YJJG118 and J2020111).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Xiao Y, Huang J, Xiao L. Effects of bone grafting after impacted mandibular third molar extraction for treatment of distal periodontal defects of second molar: a meta-analysis. J Clin Stomatol. 2019;35(2). doi:10.1016/j.joms.2018.07.025
2. Passarelli PC, Pasquantonio G, D’Addona A. Management of surgical third lower molar extraction and postoperative progress in patients with factor VII deficiency: a clinical protocol and focus on this rare pathologic entity. J Oral Maxillofac Surg. 2017;75(10):
3. Galvão EL, da Silveira EM, de Oliveira ES, et al. Association between mandibular third molar position and the occurrence of pericoronitis: a systematic review and meta-analysis. Arch Oral Biol. 2019;107:104486. doi:10.1016/j.archoralbio.2019.104486
4. Cho H, Lynham AJ, Hsu E. Postoperative interventions to reduce inflammatory complications after third molar surgery: review of the current evidence. Aust Dent J. 2017;62(4):412–414. doi:10.1111/adj.12526
5. Sayed N, Bakathir A, Pasha M, Al-Sudairy S. Complications of third molar extraction: a retrospective study from a tertiary healthcare centre in Oman. Sultan Qaboos Univ Med J. 2019;19(3):e230–e235. doi:10.18295/squmj.2019.19.03.009
6. Du YJ. Clinical effects and safety of mesial and horizontal impacted third molars removed by mesial occlusal surface grinding. Hebei Med J. 2018;40(03):416–420.
7. Lei L, Li HX, Pan SB, Yan FH. [Expression of triggering receptors expressed on myeloid-1 in innate response to Porphyromonas gingivalis in macrophages]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2013;48(12):730–733. Chinese.
8. Kugelberg CF, Ahlström U, Ericson S, Hugoson A, Thilander H. The influence of anatomical, pathophysiological and other factors on periodontal healing after impacted lower third molar surgery. A multiple regression analysis. J Clin Periodontol. 1991;18(1):37–43. doi:10.1111/j.1600-051x.1991.tb01117.x
9. Passarelli PC, Lajolo C, Pasquantonio G, et al. Influence of mandibular third molar surgical extraction on the periodontal status of adjacent second molars. J Periodontol. 2019;90(8):847–855. doi:10.1002/JPER.18-0415
10. Weiliu Q. Oral and Facial Surgery [M]. Version 6. Beijing: People’s Medical Publishing House; 2008:76.
11. Kim E, Eo MY, Nguyen TTH, Yang HJ, Myoung H, Kim SM. Spontaneous bone regeneration after surgical extraction of a horizontally impacted mandibular third molar: a retrospective panoramic radiograph analysis. Maxillofac Plast Reconstr Surg. 2019;41(1):4. doi:10.1186/s40902-018-0187-8
12. Kugelberg CF, Ahlström U, Ericson S, Hugoson A. Periodontal healing after impacted lower third molar surgery. A retrospective study. Int J Oral Surg. 1985;14(1):29–40. doi:10.1016/s0300-9785(85)80007-7
13. Du LZ. The effect of impacted mandibular wisdom teeth on the health of adjacent teeth. Proc Clin Med. 2011;20(8).
14. Leung WK, Corbet EF, Kan KW, Lo EC, Liu JK. A regimen of systematic periodontal care after removal of impacted mandibular third molars manages periodontal pockets associated with the mandibular second molars. J Clin Periodontol. 2005;32(7):725–731. doi:10.1111/j.1600-051X.2005.00773.x
15. Yan ZY, Tan Y, Xie XY, He W, Guo CB, Cui NH. Computer-aided three-dimensional assessment of periodontal healing distal to the mandibular second molar after coronectomy of the mandibular third molar: a prospective study. BMC Oral Health. 2020;20(1):264. doi:10.1186/s12903-020-01250-z
16. Nunn ME, Fish MD, Garcia RI, et al. Retained asymptomatic third molars and risk for second molar pathology. J Dent Res. 2013;92(12):1095–1099. doi:10.1177/0022034513509281
17. Petsos H, Korte J, Eickholz P, Hoffmann T, Borchard R. Surgical removal of third molars and periodontal tissues of adjacent second molars. J Clin Periodontol. 2016;43(5):453–460. doi:10.1111/jcpe.12527
18. Rossi D, Rossi D, Rossi D, et al.; Dental Supplement. Complication in third molar extractions. J Biol Regul Homeost Agents. 2019;33(3 Suppl. 1):169–172.
19. Pogrel MA. What is the effect of timing of removal on the incidence and severity of complications? J Oral Maxillofac Surg. 2012;70(Suppl 9):S37–S40. doi:10.1016/j.joms.2012.04.028
20. Chiapasco M, Crescentini M, Romanoni G. Germectomy or delayed removal of mandibular impacted third molars: the relationship between age and incidence of complications. J Oral Maxillofac Surg. 1995;53:418. doi:10.1016/0278-2391(95)90715-7
21. Kugelberg CF. Periodontal healing two and four years after impacted lower third molar surgery. A comparative retrospective study. Int J Oral Maxillofac Surg. 1990;19(6):341–345. doi:10.1016/s0300-9785(85)80007-7
22. Fickl S, Fischer KR, Negri B, et al. Tissue response following papilla-sparing and sulcular incisions in oral surgery–an experimental study. Clin Oral Investig. 2014;18(4):1313–1317. doi:10.1007/s00784-013-1069-1
23. Alqahtani NA, Khaleelahmed S, Desai F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. J Oral Maxillofac Pathol. 2017;21(2):317–318. doi:10.4103/jomfp.JOMFP_75_17
24. Yaffe A, Iztkovich M, Earon Y, Alt I, Lilov R, Binderman I. Local delivery of an amino bisphosphonate prevents the resorptive phase of alveolar bone following mucoperiosteal flap surgery in rats. J Periodontol. 1997;68(9):884–889. doi:10.1902/jop.1997.68.9.884
25. Rosa AL, Carneiro MG, Lavrador MA, Novaes AB. Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(4):404–407. doi:10.1067/moe.2002.122823
26. Suarez-Cunqueiro MM, Gutwald R, Reichman J, Otero-Cepeda XL, Schmelzeisen R. Marginal flap versus paramarginal flap in impacted third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(4):403–408. doi:10.1067/moe.2003.84
27. Kirtiloğlu T, Bulut E, Sümer M, Cengiz I. Comparison of 2 flap designs in the periodontal healing of second molars after fully impacted mandibular third molar extractions. J Oral Maxillofac Surg. 2007;65(11):2206–2210. doi:10.1016/j.joms.2006.11.029
28. Jakse N, Bankaoglu V, Wimmer G, Eskici A, Pertl C. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(1):7–12. doi:10.1067/moe.2002.119519
29. Monaco G, Daprile G, Tavernese L, Corinaldesi G, Marchetti C. Mandibular third molar removal in young patients: an evaluation of 2 different flap designs. J Oral Maxillofac Surg. 2009;67(1):15–21. doi:10.1016/j.joms.2007.05.032
30. Chen YW, Lee CT, Hum L, Chuang SK. Effect of flap design on periodontal healing after impacted third molar extraction: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46(3):363–372. doi:10.1016/j.ijom.2016.08.005
31. Korkmaz YT, Mollaoglu N, Ozmeriç N. Does laterally rotated flap design influence the short-term periodontal status of second molars and postoperative discomfort after partially impacted third molar surgery? J Oral Maxillofac Surg. 2015;73(6):1031–1041. doi:10.1016/j.joms.2015.01.005
32. Briguglio F, Zenobio EG, Isola G, et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: clinical and statistical evaluations. Quintessence Int. 2011;42(6):445–453.
33. Mistry FK, Hegde ND, Hegde MN. Postsurgical consequences in lower third molar surgical extraction using micromotor and piezosurgery. Ann Maxillofac Surg. 2016;6(2):251–259. doi:10.4103/2231-0746.200334
34. Wang W, Shang YY. Clinical observation of minimally invasive extraction of the impacted mandibular third molar. World Latest Med Info. 2020;20(62).
35. Coomes AM, Mealey BL, Huynh-Ba G, et al. Buccal bone formation after flapless extraction: a randomized, controlled clinical trial comparing recombinant human bone morphogenetic protein 2/absorbablecollagen carrier and collagen sponge alone. J Periodontol. 2014;85(4):525–535. doi:10.1902/jop.2013.130207
36. Araujo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009;20(6):545–549. doi:10.1111/j.1600-0501.2008.01703.x
37. Wang HB. The effect of minimally invasive extraction on the degree of discomfort and the healing of alveolar bone in patients.General. J Stomatol. 2018;5(5):1–2.
38. Basheer SA, Govind RJ, Daniel A, Sam G, Adarsh VJ, Rao A. Comparative study of piezoelectric and rotary osteotomy technique for third molar impaction. J Contemp Dent Pract. 2017;18(1):60–64. doi:10.5005/jp-journals-10024-1990
39. Stella PEM, Falci SGM, Oliveira de Medeiros LE, et al. Impact of mandibular third molar extraction in the second molar periodontal status: a prospective study. J Indian Soc Periodontol. 2017;21(4):285–290. doi:10.4103/jisp.jisp_79_17
40. Zhang XM, Hou GY, Wang WW, Liao JX, Kang FW. Application of the buccal bone osteotomy with piezosurgery in extracting deeply impacted mandibular third molars. J Oral Maxillofac Surg. 2019;29(1):30–33.
41. Mattout P, Mattout C. Conditions for success in guided bone regeneration: retrospective study on 376 implant sites. J Periodontol. 2000;71(12):1904–1909. doi:10.1902/jop.2000.71.12.1904
42. Osunde OD, Adebola RA, Saheeb BD. A comparative study of the effect of suture-less and multiple suture techniques on inflammatory complications following third molar surgery. Int J Oral Maxillofac Surg. 2012;41(10):1275–1279. doi:10.1016/j.ijom.2012.04.009
43. Burkhardt R, Lang NP. Influence of suturing on wound healing. Periodontol 2000. 2015;68(1):270–281. doi:10.1111/prd.12078
44. Cetinkaya BO, Sumer M, Tutkun F, Sandikci EO, Misir F. Influence of different suturing techniques on periodontal health of the adjacent second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(2):156–161. doi:10.1016/j.tripleo.2009.03.024
45. Zhu YG, Zhong ZH, Chang SH. Influence of the suture method of mandibular impacted wisdom tooth extraction on the distal periodontal tissue of adjacent teeth. Jilin Medicine. 2014;35(17):3765–3766.
46. Jeong JS, Chang M. food impaction and periodontal/peri-implant tissue conditions in relation to the embrasure dimensions between implant-supported fixed dental prostheses and adjacent teeth: a cross-sectional study. J Periodontol. 2015;86(12):1314–1320. doi:10.1902/jop.2015.150322
47. Pons-Vicente O, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Effect on pocket depth and attachment level of manual versus ultrasonic scaling of lower second molars following lower third molar extraction: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):e11–e9. doi:10.1016/j.tripleo.2008.12.001
48. Xu J. The influence of the impacted mandibular third molar extraction on the distal periodontal tissue of the mandibu- lar second molar. J Dent Prev Treat. 2016;24(1).
49. Xie C, Guo FY, Li XS, Cheng B. Effect of third molar extraction combined with simultaneous periodontal repair on periodontal tissue. Chin J Aesthet Med. 2018;27(1).
50. Wriedt S, Al-Nawas B, Schmidtmann I, et al. Analyzing the teeth next to the alveolar cleft: examination and treatment proposal prior to bone grafting based on three-dimensional versus twodimensional diagnosis-A diagnostic study. J Craniomaxillofac Surg. 2017;45(8):1272–1277. doi:10.1016/j.jcms.2017.05.024
51. Soeroso Y, Akase T, Sunarto H, et al. The risk reduction of recurrent periodontal pathogens of local application minocycline HCl 2% gel, used as an adjunct to scaling and root planing for chronic periodontitis treatment. Ther Clin Risk Manag. 2017;13:307–314. doi:10.2147/TCRM.S130257
52. Cortell-Ballester I, Figueiredo R, Valmaseda-Castellón E, Gay-Escoda C. Effects of collagen resorbable membrane placement after the surgical extraction of impacted lower third molars. J Oral Maxillofac Surg. 2015;73(8):1457–1464. doi:10.1016/j.joms.2015.02.015
53. Corinaldesi G, Lizio G, Badiali G, Morselli-Labate AM, Marchetti C. Treatment of intrabony defects after impacted mandibular third molar removal with bioabsorbable and non-resorbable membranes. J Periodontol. 2011;82(10):1404–1413. doi:10.1902/jop.2011.100466
54. Lobb DC, DeGeorge BR, Chhabra AB. Bone graft substitutes: current concepts and future expectations. J Hand Surg Am. 2019;44(6):497–505. doi:10.1016/j.jhsa.2018.10.032
55. Ge J, Yang C, Zheng J, Hu Y. Autogenous bone grafting for treatment of osseous defect after impacted mandibular third molar extraction: a randomized controlled trial. Clin Implant Dent Relat Res. 2017;19(3):572–580. doi:10.1111/cid.12466
56. Su YC. Autologous bone graft materials. Oral Implantol. 2014;(08):466–467. doi:10.1902/jop.2000.71.12.1904
57. Liang Y, Kang FW. Repair of distal bone defect of the second molar after extraction of fully impacted mandibular third molars. Stomatology. 2020;40(1).
58. Singh M, Bhate K, Kulkarni D, Santhosh Kumar SN, Kathariya R. The effect of alloplastic bone graft and absorbable gelatin sponge in prevention of periodontal defects on the distal aspect of mandibular second molars, after surgical removal of impacted mandibular third molar: a comparative prospective study. J Maxillofac Oral Surg. 2015;14(1):101–106. doi:10.1007/s12663-013-0599-z
59. Throndson RR, Sexton SB. Grafting mandibular third molar extraction sites: a comparison of bioactive glass to a nongrafted site. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(4):413–419. doi:10.1067/moe.2002.127582
60. Chen ZF. Tissue engineered bone scaffold material in restoration of alveolar socket after extraction of lower impacted third molar. Shanghai Kou Qiang Yi Xue. 2011;20(1):93–96.
61. Sammartino G, Tia M, Bucci T, Wang HL. Prevention of mandibular third molar extraction-associated periodontal defects: a comparative study. J Periodontol. 2009;80(3):389–396. doi:10.1902/jop.2009.080503
62. Meyer M. Processing of collagen based biomaterials and the resulting materials properties. Biomed Eng Online. 2019;18(1):24. doi:10.1186/s12938-019-0647-0
63. Koshinuma S, Murakami S, Noi M, et al. Comparison of the wound healing efficacy of polyglycolic acid sheets with fibrin glue and gelatin sponge dressings in a rat cranial periosteal defect model. Exp Anim. 2016;65(4):473–483. doi:10.1538/expanim.16-0031
64. Wang LC, Chen Z, Chen JP, Bai DH. Comparison of collagen sponge and gelatin sponge in preventing complications after impacted tooth extraction. J Guangdong Med Coll. 2018;36(5).
65. Kim JW, Seong TW, Cho S, Kim SJ. Randomized controlled trial on the effectiveness of absorbable collagen sponge after extraction of impacted mandibular third molar: split-mouth design. BMC Oral Health. 2020;20(1):77. doi:10.1186/s12903-020-1063-3
66. Yelamali T, Saikrishna D. Role of platelet rich fibrin and platelet rich plasma in wound healing of extracted third molar sockets: a comparative study. J Maxillofac Oral Surg. 2015;14:410. doi:10.1007/s12663-014-0638-4
67. Gandevivala A, Sangle A, Shah D, et al. Autologous platelet-rich plasma after third molar surgery. Ann Maxillofac Surg. 2017;7(2):245–249. doi:10.4103/ams.ams_108_16
68. Bhujbal R, Malik NA, Kumar N, Kv S, Parkar MI, Mb J. Comparative evaluation of platelet rich plasma in socket healing and bone regeneration after surgical removal of impacted mandibular third molars. J Dent Res Dent Clin Dent Prospects. 2018;12(3):153–158. doi:10.15171/joddd.2018.024
69. Doiphode AM, Hegde P, Mahindra U, Santhosh Kumar SM, Tenglikar PD, Tripathi V. Evaluation of the efficacy of platelet-rich plasma and platelet-rich fibrin in alveolar defects after removal of impacted bilateral mandibular third molars. J Int Soc Prev Community Dent. 2016;6(Suppl 1):S47–S52. doi:10.4103/2231-0762.181167
70. Renatus A, Trentzsch L, Schönfelder A, Schwarzenberger F, Jentsch H. Evaluation of an electronic periodontal probe versus a manual probe. J Clin Diagn Res. 2016;10(11):ZH03–ZH07. doi:10.15171/joddd.2018.024
71. Dias MJ, Franco A, Junqueira JL, Fayad FT, Pereira PH, Oenning AC. Marginal bone loss in the second molar related to impacted mandibular third molars: comparison between panoramic images and cone beam computed tomography. Med Oral Patol Oral Cir Bucal. 2020;25(3):e395–e402. doi:10.4317/medoral.23443
72. Christiaens V, De Bruyn H, Thevissen E, Koole S, Dierens M, Cosyn J. Assessment of periodontal bone level revisited: a controlled study on the diagnostic accuracy of clinical evaluation methods and intra-oral radiography. Clin Oral Investig. 2018;22(1):425–431. doi:10.1007/s00784-017-2129-8
73. Tabrizi R, Arabion H, Gholami M. How will mandibular third molar surgery affect mandibular second molar periodontal parameters? Dent Res J (Isfahan). 2013;10(4):523–526.
74. Faria AI, Gallas-Torreira M, López-Ratón M. Mandibular second molar periodontal healing after impacted third molar extraction in young adults. J Oral Maxillofac Surg. 2012;70(12):2732–2741. doi:10.1016/j.joms.2012.07.044
75. Leone SA, Edenfield MJ, Cohen ME. Correlation of acute pericoronitis and the position of the mandibular third molar. Oral Surg Oral Med Oral Pathol. 1986;62(3):245–250. doi:10.1016/0030-4220(86)90001-0
76. Peng KY, Tseng YC, Shen EC, Chiu SC, Fu E, Huang YW. Mandibular second molar periodontal status after third molar extraction. J Periodontol. 2001;72(12):1647–1651. doi:10.1902/jop.2001.72.12.1647
77. Montero J, Mazzaglia G. Effect of removing an impacted mandibular third molar on the periodontal status of the mandibular second molar. J Oral Maxillofac Surg. 2011;69(11):2691–2697. doi:10.1016/j.joms.2011.06.205
78. Blakey GH, Parker DW, Hull DJ, et al. Impact of removal of asymptomatic third molars on periodontal pathology. J Oral Maxillofac Surg. 2009;67(2):245–250. doi:10.1016/j.joms.2008.08.022
79. Pham TAV, Nguyen NH. Periodontal status of the adjacent second molar after impacted mandibular third molar surgical extraction. Contemp Clin Dent. 2019;10(2):311–318. doi:10.4103/ccd.ccd_634_18
80. Dicus-Brookes C, Partrick M, Blakey GH, et al. Removal of symptomatic third molars may improve periodontal status of remaining dentition. J Oral Maxillofac Surg. 2013;71(10):1639–1646. doi:10.1016/j.joms.2013.06.190
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.