Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Effectiveness of the clinical pharmacist in reducing mortality in hospitalized cardiac patients: a propensity score-matched analysis
Received 14 October 2015
Accepted for publication 16 December 2015
Published 18 February 2016 Volume 2016:12 Pages 241—250
DOI https://doi.org/10.2147/TCRM.S98300
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Video abstract presented by Xiao-bo Zhai
Views: 1012
Xiao-bo Zhai,1 Zhi-chun Gu,2 Xiao-yan Liu2
1Department of Pharmacy, Shanghai East Hospital, Affiliated to Tongji University School of Medicine, 2Department of Pharmacy, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
Background: Pharmacist-led medication review services have been assessed in the meta-analyses in hospital. Of the 135 relevant articles located, 21 studies met the inclusion criteria; however, there was no statistically significant difference found between pharmacists’ interventions and usual care for mortality (odds ratio 1.50, 95% confidence interval 0.65, 3.46, P=0.34). These analyses may not have found a statistically significant effect because they did not adequately control the wide variation in the delivery of care and patient selection parameters. Additionally, the investigators did not conduct research on the cases of death specifically and did not identify all possible drug-related problems (DRPs) that could cause or contribute to mortality and then convince physicians to correct. So there will be a condition to use a more precise approach to evaluate the effect of clinical pharmacist interventions on the mortality rates of hospitalized cardiac patients.
Objective: To evaluate the impact of the clinical pharmacist as a direct patient-care team member on the mortality of all patients admitted to the cardiology unit.
Methods: A comparative study was conducted in a cardiology unit of a university-affiliated hospital. The clinical pharmacists did not perform any intervention associated with improper use of medications during Phase I (preintervention) and consulted with the physicians to address the DRPs during Phase II (postintervention). The two phases were compared to evaluate the outcome, and propensity score (PS) matching was applied to enhance the comparability. The primary endpoint of the study was the composite of all-cause mortality during Phase I and Phase II.
Results: Pharmacists were consulted by the physicians to correct any drug-related issues that they suspected may cause or contribute to a fatal outcome in the cardiology ward. A total of 1,541 interventions were suggested by the clinical pharmacist in the study group; 1,416 (92.0%) of them were accepted by the cardiology team, and violation of incompatibilities had the highest percentage of acceptance by the cardiology team. All-cause mortality was 1.5% during Phase I (preintervention) and was reduced to 0.9% during Phase II (postintervention), and the difference was statistically significant (P=0.0005). After PS matching, all-cause mortality changed from 1.7% during Phase I down to 1.0% during Phase II, and the difference was also statistically significant (P=0.0074).
Conclusion: DRPs that were suspected to cause or contribute to a possibly fatal outcome were determined by clinical pharmacist service in patients hospitalized in a cardiology ward. Correction of these DRPs by physicians after pharmacist’s advice caused a significant decrease in mortality as analyzed by PS matching. The significant reduction in the mortality rate in this patient population observed in this study is “hypothesis generating” for future randomized studies.
Keywords: drug-related problems, cardiology ward, clinical pharmacists, intervention, propensity score matching
Introduction
Adverse drug events (ADEs) were classified based on their severity as fatal, life threatening, or significant. A fatal ADE (FADE) was defined as the one that was associated with the death of the patient.1 A preventable FADE was the one in which the absence of drug-related problems (DRPs) would have prevented the ADE. An ameliorable FADE was the one in which the absence of DRPs would have decreased the severity and/or duration of the ADE.2 A study demonstrated that 732 patients died in the internal medicine department over a 2-year period, and the incidence of FADEs was 18.2% (133/732). The authors found that the drugs that were suspected of causing or contributing to the fatal outcomes were mainly those used for treating chronic pulmonary diseases, antithrombotic drugs, and drugs for treating coronary heart disease and heart failure (HF). DRPs such as serious drug–drug and drug–disease interactions, various degrees of inappropriateness in the choice of drug, dosage, or administration route were seen in 50% of the FADE cases.3 The US Institute of Medicine stated that as many as 98,000 people in the US hospitals die each year because of DRPs. Loss of life from DRPs is both tragic and often avoidable.4 In the last few years, the use of polypharmacy has increased in patients with cardiovascular diseases (CVDs), mainly because of the higher number of associated comorbidities in this patient group. Polypharmacy and the disproportionate use of medications combined with age-related and disease-related pharmacokinetic and pharmacodynamic changes place these patients at higher risk of DRPs and FADEs.5 In patients with CVDs, the frequency of DRPs has been reported to be as high as 68%.6 Cardiovascular drugs, such as antithrombotic agents, anticoagulants, hemostatic agents, and cardiac glycoside, are commonly implicated in FADE due to suboptimal medication use in CVD.7 Nosocomial infections in patients in cardiology departments rely on factors such as old age, HF, invasive procedures, concomitant diseases, and inappropriate use of antimicrobial drugs. These infections ultimately increase the risk of death for these patients.8
The clinical pharmacists can play an important role by intervening and correcting DRPs at a hospital cardiology unit.9 It is likely that the clinical pharmacy intervention is best implemented in the cardiology ward if the clinical pharmacist discusses the DRPs face-to-face with the physicians.10 Presumably, cases had been reviewed by a clinical pharmacist, and then DRPs with the potential to cause or contribute to death were discovered by the pharmacist. This prompted the attending physician(s) to change the treatment regimen in time to avert the FADE.11 In these cases, a clinical pharmacist caring for patients with severe infections recommended changes to antibiotic regimens as needed to improve spectrum of coverage and/or antimicrobial activity based on clinical response, culture/sensitivity data, or appropriate duration of therapy to modify antibiotic dosing or frequency.11 In such situations, the mortality rate of hospitalized cardiac patients may decline.12
Aim
Therefore, it is necessary to determine the impact of clinical pharmacy services on the outcomes of hospitalized cardiac patients by conducting a study using a prospective design to compare a standard care group with a pharmaceutical care group.
Methods
The study was carried out in a 60-bed cardiology ward in an internal medicine floor (including coronary care unit [CCU] with 12 beds) of a teaching hospital affiliated to Shanghai Jiao Tong University School of Medicine. A single-centered, two-phased (intervention/no intervention) study was conducted. All patients admitted at the cardiology ward during the study period were involved, and no exclusion criteria were applied. The no-intervention phase was carried out between January 1, 2010 and April 30, 2012 (28 months, Phase I, preintervention). To become a clinical pharmacist in the People’s Republic of China, a pharmacist having a bachelor degree or a higher degree of pharmacy must accept 1 year of professional training organized by the National Ministry of Health, and should obtain a certificate of competency. Then the clinical pharmacist must have more than a decade of clinical experience before becoming a senior clinical pharmacist who can make life-saving pharmacy interventions. The clinical pharmacists had not been scheduled by the supervisor to enter the cardiology ward, and they just collected the baseline data including patient characteristics and recorded the materials without any intervention associated with improper use of medications. The intervention phase was carried out between May 1, 2012 and April 30, 2015 (36 months, Phase II, postintervention). DRPs, which have been described as actual or potential negative outcomes resulting from the way in which drugs are used, may result in drug treatment goals not being achieved and/or patient harm comprising death. It took 40 hours per week for an experienced senior clinical pharmacist to conduct research on all cases of death in the intervention group and to identify all possible DRPs, including violation of contraindications and incompatibilities, harmful interactions, excess or insufficient dosage, incorrect indications, and inappropriate use of antimicrobial drugs that could cause or contribute to mortality. During this consultation, the pharmacist discussed these issues with the cardiologists of the cardiology ward, the doctors in charge agreed on FADEs or ameliorable FADEs, and together they reached a consensus regarding the DRPs that the cardiology physicians had an obligation to correct in principle. The role and actions of the experienced senior clinical pharmacist had been described in detail in three typical cases.
Two clinical pharmacists checked out all the prescriptions and medical records and participated on daily medical rounds to identify and clarify any DRPs in drug orders for each patient every morning. The two clinical pharmacists then talked to the physicians to correct the DRPs. All interventions (accepted or not accepted by cardiologists) were recorded by the two clinical pharmacists. The ratio of pharmacists to patients was 1:30. Nurse and physician staffing ratios were similar during Phase I and Phase II. The study was approved by the Institutional Review Board of Renji Hospital.
Data collection
Patient characteristics, including demographics, nursing acuity score, and primary discharge diagnosis, were documented by review of the medical chart and the hospital information system. Nursing acuity score was considered to reflect the severity of illness to a certain extent: grade 3 (moderate: the patient’s condition is not severe and is relatively stable, and Karnofsky performance scale is 50–80), grade 2 (severe: the patient with severe disease tends to be stable or the patient’s condition is not severe but is unstable, and Karnofsky performance scale is 20–40), grade 1 (critical: the patient is in critical condition, and change in condition may occur at any time and needs to be rescued; moreover, Karnofsky performance scale is <10). The cardiologists decided a patient’s acuity score. Patient characteristics during Phase I (preintervention) and Phase II (postintervention) were compared to determine if they were similar. The types of pharmacotherapy interventions and actions taken by the medical team were documented on the clinical services data capture log. The consultation resulted in the following types of intervention: 1) identification of violation of medication contraindications and recommendation of therapeutic alternative when needed; 2) discovery of intravenous admixture incompatibilities in solution; 3) identification of harmful drug interactions; 4) clarification of drug dosage and frequency; 5) identification of incorrect indications; and 6) identification of inappropriate use of antibiotics.
Outcome measures
We assessed the effect of pharmacist participation using two measures: 1) the number of DRPs that could cause or contribute to mortality raised by the pharmacist and acceptance of interventions recommended by the clinical pharmacists and 2) the composite of all-cause mortality during Phase I and Phase II.
Statistical analysis
Since it was difficult to correct the differences in patient’s characteristics between Phase I (preintervention) and Phase II (postintervention) in our prospective nonrandomized controlled trial, we tried to analyze the data by propensity score (PS) matching.13 To do this, logistic regression was used to develop a PS. The PS included the following variables: age, sex, nursing acuity score, and primary discharge diagnosis. The greedy matching algorithm first identifies matched pairs (a patient in Phase I and a patient in Phase II) within a closeness range of 0.00001 of the PS, and then if no more individuals can be found, the program identifies matched pairs in a range of 0.0001 and so on up to a closeness range of 0.1. Once this threshold was exceeded, that patient was excluded.14 Dichotomous outcomes were summarized in 2×2 tables and were analyzed using the likelihood ratio χ2 test and Fisher’s exact test. Continuous variables were presented as medians along with standard deviation. These variables were tested using grouped t-test and Wilcoxon rank sum test. All statistical analyses were performed using the SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA).15
Results
Finding out DRPs from cases of death in Phase II
All death cases in the study unit were investigated subsequently, and all possible DRPs in these cases were identified. Consensus on the DRPs was reached.
Typical case 1
An 80-year-old man with inferior myocardial infarction was admitted to the CCU on May 5, 2014. The patient’s alanine aminotransferase (ALT) was 19 IU/L (13–69 IU/L), total bilirubin was 13.1 μmol/L (3.4–17.1 μmol/L), and creatinine was 85.6 μmol/L (45–104 μmol/L). The patient received aspirin, clopidogrel, rosuvastatin calcium, pantoprazole sodium, and potassium chloride and underwent percutaneous coronary intervention to right coronary artery successfully at 2.05 pm on May 6. After 4 hours, the patient’s body temperature increased to 38.6°C, and 2 mg of cefepime was given intravenously two times daily from May 6 to May 21. He had a high fever of 39°C on May 9, and the temperature dropped to normal without any kind of antipyretics on May 12 after 0.5 g of levofloxacin had been given intravenously once a day on May 11. The physician stopped using levofloxacin on May 12 for fear of it might cause damage to the liver because his ALT was 91 IU/L (13–69 IU/L) with normal bilirubin index on this day and his temperature rebounded to 39.2°C on May 14. The patient’s bilateral sclerotic appeared xanthochromia, and his total bilirubin was 62.3 μmol/L (3.4–17.1 μmol/L), while ALT decreased to normal. Hepatitis A, hepatitis B, hepatitis C, and hepatitis E were excluded through immunological detection of hepatitis. The patient had a high fever of 39.2°C, despite the use of ice packs and nimesulide on May 19, and his urine volume was 350 mL with only 82% of the oxygen saturation on May 20. The patient’s creatinine rose to 335 μmol/L (45–104 μmol/L) and total bilirubin increased to 107.8 μmol/L (3.4–17.1 μmol/L) on May 21. Furthermore, his blood pressure dropped to 80/50 mmHg and gradually lost consciousness till death on the same day. The patient’s leukocyte count and neutrophil percentage were always lower than normal throughout the course of the disease.
Subsequent evaluation of the treatment protocol by the clinical pharmacist revealed several issues. The main factor for death of the patient was multiple organ dysfunction syndrome, which was caused by systemic inflammatory response syndrome because of serious infection. When the patient had received levofloxacin on May 11, he did not have a fever the next day but had a high fever again after levofloxacin was deactivated, and this suggested that levofloxacin was effective. The cefepime insert states that “A course of cefepime is usually 7–10 days for serious infections”. However, cefepime had been used for 16 days and had not been replaced by other antibiotics until the patient died on May 21. According to the rule, the patient with a serious infection or infection with severe underlying diseases should receive a combination of broad spectrum antibiotics to cover resistant Gram-negative bacilli and Gram-positive cocci pending the outcome of bacterial culture + sensitivity. Furthermore, if not effective after 48–72 hours, timely adjustment of antimicrobial agents should be considered.16
Therefore, in this case, one DRP that may have contributed to the patient’s death was identified, that is, irrational usage of antibiotics.
Typical case 2
An 82-year-old man presented to the CCU on December 11, 2013 with acute coronary syndrome, chronic HF in New York Heart Association class III–IV with a history of type 2 diabetes mellitus, and chronic kidney disease 3. The patient received aspirin, clopidogrel, rosuvastatin calcium, furosemide, pantoprazole sodium, and nitroglycerin from December 11, 2013 to January 11, 2014 and underwent percutaneous coronary intervention to circumflex branch successfully on December 17, 2013. The patient had a blood pressure of 130/75 mmHg on December 19, 2013, which dropped to 114/60 mmHg after perindopril 4 mg orally once a day had been given from December 22, 2013 to January 9, 2014. However, isosorbide mononitrate sustained-release capsules 50 mg orally two times daily were given to the patient from December 25, 2013 to January 11, 2014. The patient experienced a sustaining drop of blood pressure in spite of dopamine infusion via an intravenous pump persistently from December 27, 2013 to January 11, 2014, and syncope occurred because of postural hypotension on January 7, 2014 with HF being aggravated by severe hypotension (73/34 mmHg) as well as other factors on the next day. Although perindopril was deactivated on January 9, 2014, isosorbide mononitrate sustained-release capsules were not decremented. Electrocardiogram displayed an exacerbation of myocardial ischemia, and the patient died of ventricular fibrillation on January 11, 2014.
The patient was 82 years old with chronic renal insufficiency, coupled with severe HF. The insert mentions that “the initial dose of perindopril should not exceed 2 mg per day in such a case”, but the initial dose was 4 mg in fact. Moreover, the instruction regulates that “dosage of isosorbide mononitrate sustained-release capsules is 50 mg per day”; however, the actual situation was that the patient received double dose.
Therefore, in this case, two DRPs that may have contributed to the death of this patient were identified: inappropriate dose and frequency associated with perindopril and isosorbide mononitrate sustained-release capsules.
Typical case 3
A 36-year-old young woman presented to the cardiology ward with dilated cardiomyopathy in NYHA class IV on September 4, 2014 with a history of upper gastrointestinal hemorrhage. The patient’s creatinine was 79.2 μmol/L (45–104 μmol/L). She received metoprolol 6.25 mg two to three times daily from September 19 to October 14 and 12.5 mg two times daily from October 14 to October 27. Omeprazole enteric-coated capsules 20 mg per day were given from September 24 to October 28, and torasemide 20 mg per day was given from September 25 to October 10 and torasemide 20 mg two times daily from October 10 to October 28. The patient received digoxin 0.125 mg per day from September 29 to October 27 and furosemide 20 mg two times daily from October 10 to October 28. She had watery diarrhea from October 14 to October 18 and received doxepin 12.5 mg two times daily from October 17 to October 27 because of emotional factors. A sudden loss of consciousness happened with blood pressure of only 75/40 mmHg on October 19 after torasemide 40 mg had been given via an intravenous pump. The patient’s creatinine rose to 111 μmol/L (45–104 μmol/L) and further went up to 185 μmol/L (45–104 μmol/L) on October 25. Her heart rate slowed down to 40 times a minute suddenly on October 27, and ECG displayed 2° atrioventricular block after she had received deslanoside 0.4 mg intravenous injection. She died on the next day despite aggressive rescue.
The insert states that “the daily dose of torasemide should not exceed 40 mg usually when being used to treat heart failure”, while the patient received 80 mg torasemide totally with the addition of 40 mg furosemide on October 19, coupled with possible hypovolemia for watery diarrhea. We believed that these reasons coupled with decompensated HF led to hypotension and syncope on October 19.
The patient accepted deslanoside on October 27 although having received digoxin almost a month, along with her deteriorating renal function, plus both of doxepin and omeprazole could increase digoxin toxicity; furthermore, both doxepin and metoprolol could decrease the heart rate, and the insert states that “patients with severe heart disease were prohibited from receiving this drug”. We considered that these reasons plus the patient’s primary disease triggered 2° atrioventricular block.
Four DRPs that may have contributed to the death of this patient were identified: 1) inappropriate dose and frequency related to torasemide; 2) violation of the medication’s contraindications about doxepin; and 3) two harmful interactions between digoxin and doxepin and between digoxin and omeprazole.
It was later recommended that patients with severe heart disease should take fluoxetine, paroxetine, etc., instead of doxepin.
Reach a consensus on DRPs from the above-described cases of death in the study unit
As shown in these cases of death, all the possible DRPs that were suspected of causing or contributing to the death of the patient were identified through analysis and research. After repeated discussion with the head cardiologist on call, a report of these incidents was created, including the DRPs that had been extracted and summarized from all the cases of death. The consensus contained 26 instances of violation of contraindications, eight instances of violation of incompatibilities, 15 instances of harmful interactions of combination therapy, nine instances of dose problems, eight instances of indication problems, and six instances of problems due to irrational use of antibiotics.
Pharmacist interventions and their effect
In all, 15,197 patients were enrolled in the study (Phase I, preintervention =5,703; Phase II, postintervention =9,494). Characteristics including age, sex, nursing acuity score, and distribution of the number of patients diagnosed with acute myocardial infarction, bradyarrhythmia, hypertension, cardiomyopathy, replaced cardiac pacemakers, valvular disease, hyperlipidemia, HF, pulmonary embolism, and syncope were not significantly different between Phase I and Phase II. Since many characteristics including coronary artery disease, acute coronary syndrome, tachyarrhythmia, old myocardial infarction, myocardial bridge, pulmonary hypertension, myocarditis, and other diseases were significantly different between Phase I and Phase II (Table 1) and this difference was difficult to correct, we applied PS matching.17 A total of 4,000 patients were retained in each of the two groups, and none of these differences was statistically significant after PS matching (Table 2).
  | Table 1 Patient characteristics in Phase I and Phase II before PSM |
  | Table 2 Patient characteristics in Phase I and Phase II after PSM |
A total of 1,541 interventions were provided by the clinical pharmacist in the study group; 1,416 (92.0%) of them were accepted by the cardiology team. The types of interventions performed are described in Table 3, and violation of incompatibilities had the highest percentage of acceptance by the cardiology team. An exploratory economic modeling study estimated that a pharmacy-based intervention to reduce DRPs would have a probability of being cost-effective with a quality-adjusted life-year value of £10,000 of >60%.18 This suggested that our interventions might reduce medical costs and the research should be conducted in the future.
  | Table 3 Interventions suggested by the pharmacist in the study unit |
The main reason for the 8% of interventions not being accepted was that the cardiologists believed that the DRPs could be ignored under certain conditions. All-cause mortality changed from 1.5% during Phase I (preintervention) down to 0.9% during Phase II (postintervention). The difference was statistically significant (P=0.0005; Table 4). After PS matching, all-cause mortality changed from 1.7% during Phase I (preintervention) down to 1.0% during Phase II (postintervention), the difference being statistically significant (P=0.0074; Table 5).
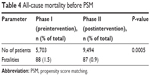  | Table 4 All-cause mortality before PSM |
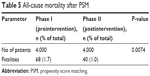  | Table 5 All-cause mortality after PSM |
Discussion
The addition of a clinical pharmacist to the care of patients with CVD can lead to an improvement in patients with CVD in many areas, including a reduction in CVD risk rates, optimizing CVD medications, and preventing DRPs. These improvements can lead to increased quality of life for patients with CVD, decreased number of hospitalizations or emergency rooms, reduced drug costs, and decreased mortality rates.19 Some recent studies have suggested that pharmacist intervention has no discernable effect on patient mortality.20,21 The authors suggested that the inability to demonstrate benefit might stem from the wide variations in the delivery of care and patient selection in the existing trials, and it might be possible to develop higher quality research into potentially effective interventions.21
Some studies showed that critically ill patients with end-stage heart diseases were more vulnerable to developing FADEs and appeared to be at a particularly high risk of which were associated with DRPs because of changing organ function, complex drug regimens, and alterations in pharmacokinetics.22,23 For example, hypotension or poorly controlled hypertension was a frequent complication following therapy with diuretics, nitrates, angiotensin-converting enzyme inhibitors, calcium channel blockers, dopamine, metaraminol, norepinephrine, and epinephrine. In addition, relative to the patient’s age, weight, liver and kidney function, and disease status, treatment with an excessive dose of antithrombotic agents, such as heparins; low-molecular weight heparin; warfarin; aspirin; clopidogrel; and alteplase increased the bleeding risk of intracerebral and other vital organs. However, when treated with an inadequate dose of the treatment drug, the risk of cerebral or myocardial infarction and embolism of other vital organs increased significantly.24 Moreover, patients with serious CVD often also had chronic obstructive lung disease and required bronchodilatory therapies such as glucocorticoids, β-adrenergic agonists, and methylxanthines. These drugs had both positive inotropic and chronotropic effects, directly increasing contractility, cardiac output, and heart rate, followed by increased cardiac oxygen consumption. Consequently, such drugs may precipitate myocardial ischemia, myocardial infarction, and serious dysrhythmias in patients with coronary artery disease and impede myocardial repair after myocardial infarction. Furthermore, hospitalized patients in the cardiology department were also suffering from nosocomial infections, which may have been attributable to their low immunity because of old age and comorbidities. Low or high blood pressure and vital organ bleeding or embolism associated with improper use of medication, as well as nosocomial infection and inappropriate use of antimicrobial drugs, were extremely deleterious to patients with existing complications such as severe CVD. Unfortunately, this was often observed too late to prevent a fatal outcome. Therefore, mortality rates of hospitalized cardiac patients could be minimized by the safe use of drugs.25
In this study, we have focused on DRPs that were suspected to cause or contribute to the mortalities of patients in the department of cardiology and identified all possible medication errors and inappropriate use of antimicrobial drugs that could have caused death. Subsequently, recommendations for changes in approach were created. The collaboration between the pharmacists and the physicians to develop the final treatment plan existed in some cases. For example, a 72-year-old man with acute coronary syndrome was admitted to the CCU. The patient developed severe pneumonia and was invalid after cefradine had been used and the pathogens had not been cultivated. According to the principle of antibacterials for a serious infection or infection with severe underlying diseases (see Supplementary material), the clinical pharmacist recommended imipenem cilastatin sodium plus teicoplanin that were accepted by the cardiologists, and finally, the severely infected patient was cured. Although cardiology physicians in the study unit should comply with these recommendations in principle, the recommendations of clinical pharmacists could not be adopted in a few cases. The main reason for this was that the original treatment was highly necessary in spite of violations of contraindications. For example, morphine was contraindicated in a patient with severe liver damage, but the patient had acute left HF complicated with severe angina pectoris, and morphine was a very strong indication in this condition. Therefore, the cardiologists decided that morphine had to be used despite the patient’s severe liver damage, but the dose was reduced based on the suggestion of clinical pharmacists. In addition, even if the patient was experiencing a harmful interaction, the indications were very definite. For example, the use of warfarin and amiodarone in combination could significantly increase the risk of bleeding. However, in one case, the patient had atrial fibrillation with rapid ventricular rate complicated by Wolff–Parkinson–White syndrome, and amiodarone had to be used with warfarin. The cardiologists reduced the dose of warfarin and strengthened monitoring of International Normalized Ration according to the recommendations of clinical pharmacists. In addition, even though the dose of a drug was inaccurate according to regulations, the cardiologists believed that the dose was accurate according to the specific conditions of the patient. For example, the initial dose of benazepril should be 2.5 mg daily in patients with congestive HF, but a patient’s blood pressure was so high that the cardiologists decided to give an initial dose of 5 mg. Moreover, although drugs should be administered when there is an indication, in some cases, the risk may be greater than the benefit. For example, a patient with atrial fibrillation complicated by HF should receive long-term warfarin to prevent thrombosis, but in the case of one older patient with liver and kidney impairment, the cardiologists judged that there was a higher risk of bleeding if the patient was given warfarin. Finally, in spite of the apparently inappropriate use of antibiotics according to the consensus, the cardiologists considered it to be reasonable when combined with the patient’s condition of infection. For example, when there is a creatinine clearance of <11 mL/min, the dose of cefepime should be 0.25–1 g once a day intravenously, but one patient had a septic shock and the cardiologists believed that the dose of cefepime should be 1 g twice a day intravenously to control the infection.
PS analysis was performed to adjust for potential bias and was used often in observational studies because of nonrandomized group assignment. We applied this statistical method to match each patient in Phase I to a patient in Phase II who had a PS that was identical to five digits. If this could not be done, we then proceeded to a four-, three-, two-, or one-digit match. The patient was excluded once this threshold was exceeded. After PS matching, age, sex, nursing acuity score, and primary discharge diagnosis of patients were similar between Phase I and Phase II, and all-cause mortality changed from 1.7% during Phase I down to 1.0% during Phase II, and the difference was also statistically significant (P=0.0074).
According to the consensus report in Phase II, the clinical pharmacists proposed 1,541 recommendations in which 1,416 were accepted by the cardiology physicians. We assumed that this had led to a decline in the mortality rate with statistical significance.
The previous studies did not show a difference in mortality probably because they were not particularly concerned about the DRPs that could cause or contribute to mortality. Our result demonstrated that the presence of an experienced, senior clinical pharmacist who conducted research on the cases of death specifically and identified all possible DRPs that could cause or contribute to mortality and then let the cardiologists accept had been associated with reduced mortality in a cardiology unit of a university-affiliated hospital. This pattern may also apply to other departments and other hospitals.
There were limitations to our study. DRPs, including ADEs, can result in admission to hospital, increase the cost of the hospital stay, and increase mortality. The US Institute of Medicine stated that as many as 98,000 patients in the US hospitals die each year because of fatal DRPs. Although one study has shown that life-threatening events associated with ADEs occur in 26% of intensive care unit patients,25 there was still insufficient evidence to prove the causal relationship between ADEs and fatal outcome. The design was not randomized by the subject. True patient randomization was not feasible since it would have interfered with the admitting process of the hospital. Blinding was also not possible in our study due to the presence of the pharmacist. Patient characteristics of Phase I and Phase II were compared, and some types of primary discharge diagnosis, including coronary artery disease, acute coronary syndrome, tachyarrhythmia, old myocardial infarction, myocardial bridge, myocarditis, and other diseases, had significant differences between the two phases. For example, the number of patients diagnosed with acute coronary syndrome was 453 and accounted for 7.9% of the total of 5,703 patients during Phase I, while during Phase II, there were 1,176 such patients and they accounted for 12.4% of the total of 9,494 patients. PS matching can reduce most of the confounding bias of the observational study.26 All patients’ characteristics were similar between Phase I and Phase II after PS matching; however, it was only done on four variables that included age, sex, nursing acuity score, and primary discharge diagnosis, and it could not be excluded that some other factors would have an effect on mortality. The decline in all-cause mortality was significantly different after intervention during Phase II just like before PS matching. PS matching can obtain approximately the same study effects as a randomized controlled trial when used in the design of an epidemiological study and it will be better if a randomized controlled trial is to be carried out.27
Conclusion
An experienced senior clinical pharmacist discovered a surprising number of DRPs in a cardiology ward that were suspected to cause or contribute to the fatal outcome of the patients. Two clinical pharmacists consulted with the physicians to address these DRPs so that the mortality rate could be significantly decreased in the cardiology ward. The significant reduction in the mortality rate should be considered “hypothesis generating” for future randomized studies that will need to further test the conclusions. A multicenter randomized controlled trial is the best analysis to demonstrate the effectiveness of this specific intervention.
Acknowledgment
The authors would like to thank the physicians in the cardiology ward who participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Dipoto JP, Buckley MS, Kane-Gill SL. Evaluation of an automated surveillance system using trigger alerts to prevent adverse drug events in the intensive care unit and general ward. Drug Saf. 2015;38:311–317. | ||
Schnipper JL, Roumie CL, Cawthon C, et al; PILL-CVD Study Group. Rationale and design of the pharmacist intervention for low literacy in cardiovascular disease (PILL-CVD) study. Circ Cardiovasc Qual Outcomes. 2010;3:212–219. | ||
Buajordet I, Ebbesen J, Erikssen J, Brørs O, Hilberg T. Fatal adverse drug events: the paradox of drug treatment. J Intern Med. 2001;250:327–341. | ||
Kelly WN. Can the frequency and risks of fatal adverse drug events be determined? Pharmacotherapy. 2001;21(5):521–527. | ||
Chen YC, Huang HH, Fan JS, et al. Comparing characteristics of adverse drug events between older and younger adults presenting to a Taiwan emergency department. Medicine. 2015;94(7):1–6. | ||
Urbina O, Ferrandez O, Luque S, et al. Patient risk factors for developing a drug-related problem in a cardiology ward. Ther Clin Risk Manag. 2015;11:9–15. | ||
Meier F, Maas R, Sonst A, et al. Adverse drug events in patients admitted to an emergency department: an analysis of direct costs. Pharmacoepidemiol Drug Saf. 2015;24:176–186. | ||
MacLaren R, Bond CA, Martin SJ, Fike D. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med. 2008;36:3184–3189. | ||
Magalhães GF, Santos GN, Rosa MB, Noblat Lde A. Medication reconciliation in patients hospitalized in a cardiology unit. PLoS One. 2014;9(12):e115491. | ||
Milfred-LaForest SK, Chow SL, DiDomenico RJ, et al. Clinical pharmacy services in heart failure society of America and American college of clinical pharmacy cardiology practice and research network. Pharmacotherapy. 2013;33(5):529–548. | ||
Graabak T, Kjeldsen LJ. Medication reviews by clinical pharmacist at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol. 2013;112:359–373. | ||
Maclaren R, Devlin JW, Martin SJ, Dasta JF, Rudis MI, Bond CA. Critical care pharmacy services in United States hospitals. Ann Pharmacother. 2006;40:612–618. | ||
Alehagen U, Benson L, Edner M, Dahlström U, Lund LH. Association between use of statins and outcomes in heart failure with reduced ejection fraction: prospective propensity score matched cohort study of 21 864 patients in the Swedish Heart Failure Registry. Circ Heart Fail. 2015;8(2):252–260. | ||
Masahiko H, Yasuhiko S, Daisaku N, et al; OACIS Investigators. Comparison of 5-year survival after acute myocardial infarction using angiotensin-converting enzyme inhibitor versus angiotensin II receptor blocker. Am J Cardiol. 2014;114:1–8. | ||
SAS Institute Inc. SAS Procedures Guide. Version 6. Vol 3. Cary, NC: SAS Institute Inc.; 1990:339. | ||
Hoffken G, Niederman MS. Nosocomial pneumonia: the importance of a de-escalating strategy for antibiotic treatment of pneumonia in the ICU. Chest. 2002;122(6):2183–2196. | ||
Helin-Salmivaara A, Lavikainen P, Aarnio E, Huupponen R, Korhonen MJ. Sequential cohort design applying propensity score matching to analyze the comparative effectiveness of atorvastatin and simvastatin in preventing cardiovascular events. PLoS One. 2014;9:e90325. | ||
Anthony JA, Sarah R, Judith AC, et al. A pharmacist-led information technology intervention for medication errors(PINCER): a multicentre, cluster randomised controlled trial and cost-effectiveness analysis. Lancet. 2012;379:1310–1319. | ||
Abdulaziz A, Ceri JP, Deborah F. A systemic review of the clinical and economic effectiveness of clinical pharmacist intervention in secondary prevention of cardiovascular disease. J Manag Care Pharm. 2013;19(5):408–416. | ||
Hatah E, Braund R, Tordoff J, Duffull SB. A systematic review and meta-analysis of pharmacist-led fee-for-services medication review. Br J Clin Pharmacol. 2013;77(1):102–115. | ||
Graabæk T, Kjeldsen LJ. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol. 2013;112:359–373. | ||
Michalets E, Creger J, Shilinglaw WR. Outcomes of expanded use of clinical pharmacist practitioners in addition to team-based care in a community health system intensive care unit. Am J Health Syst Pharm. 2015;72:47–53. | ||
Kane-Gill SL, Kirisci L, Verrico MM, Rothschild JM. Analysis of risk factors for adverse drug events in critically ill patients. Crit Care Med. 2012;40(3):823–828. | ||
Ripley TL, Adamson PB, Hennebry TA, Van Tuyl JS, Harrison DL, Rathbun RC. Collaborative practice model between cardiologists and clinical pharmacists for management of patients with cardiovascular disease in an outpatient clinic. Ann Pharmacother. 2014;48(3):412–419. | ||
Buckley MS, Harinstein LM, Clark KB, et al. Impact of a clinical pharmacy admission medication reconciliation program on medication errors in “high-risk” patients. Ann Pharmacother. 2013;47(12):1599–1610. | ||
Shin JY, Park MJ, Lee SH, et al. Risk of intracranial haemorrhage in antidepressant users with concurrent use of non-steroidal anti-inflammatory drugs: nationwide propensity score matched study. BMJ. 2015;351:h3517. | ||
Rose O, Schaffert C, Czarnecki K, et al. Effect evaluation of an interprofessional medication therapy management approach for multimorbid patients in primary care: a cluster-randomized controlled trial in community care. BMC Fam Pract. 2015;22(16):84. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
