Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Effectiveness of Pulsed Dye Laser Treatment in Tufted Angioma: A Promising Intervention
Authors Dwiyana RF , Lestari ER, Effendi RMRA , Gondokaryono SP , Diana IA, Usman HA , Suhada KU, Anandita R
Received 3 July 2023
Accepted for publication 25 September 2023
Published 17 October 2023 Volume 2023:16 Pages 2885—2891
DOI https://doi.org/10.2147/CCID.S428371
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Reiva Farah Dwiyana,1 Elisabet Risubekti Lestari,1 Raden Mohamad Rendy Ariezal Effendi,1 Srie Prihianti Gondokaryono,1 Inne Arline Diana,1 Hermin Aminah Usman,2 Kamelia Utami Suhada,1 Rafithia Anandita1
1Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital Bandung, West Java, Indonesia; 2Department of Anatomical Pathology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital Bandung, West Java, Indonesia
Correspondence: Reiva Farah Dwiyana, Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital, Jl. Pasteur 38, Bandung, West Java, 40161, Indonesia, Tel +62222032426 ext. 3449, Fax +62222032426, Email [email protected]
Introduction: Tufted angioma (TA) is a rare benign vascular tumor usually occurring in the first year of life. It may present as reddish papules or purplish red to black plaques. Tender lesions commonly affect the neck, upper trunk, and shoulders. Histologic tufts of capillaries infiltrating the dermis in a “cannon ball” distribution pattern confirm the diagnosis. However, effective treatments for TA are scarce. Pulsed dye laser (PDL) is an alternative therapy for TA, particularly concerning cosmetics and pain relief. This case report demonstrates the effectiveness of PDL as a treatment for TA.
Case: We report a 15-year-old girl with five-year history of painful purplish red plaques on her left cheek, neck, chest, left shoulder, and back. Histopathological examination from skin biopsy showed discrete “cannon ball” pattern in the dermis. Laboratory examination revealed normal platelet count and fibrinogen level. Based on these presentations, the diagnosis of TA without complications was made. We treated the lesion using 595-nm PDL with 6.5− 10 J/cm2 fluence of, 1.5 ms pulsed duration, and 5− 7 mm spot size every three weeks. Reductions in redness and pain were seen after four sessions of treatment.
Discussion: PDL promotes selective vascular damage with minimal injury to the surrounding skin. Capillary tufts in TA could therefore serve as a target for laser treatment, which may result in fading redness and pain reduction.
Conclusion: PDL is effective in reducing redness and pain in TA.
Keywords: pulse dye laser, tufted angioma, vascular tumor
Introduction
Tufted angioma (TA), also known as angioblastoma of Nakagawa, is a rare benign vascular neoplasm.1,2 Approximately 25% of the cases are congenital and 50% of the cases appear in the first few years of life.1 The pathogenesis of TA is unknown. It is probably neoplastic in nature and the development of numerous tufts of vessels is most likely triggered by localized secretion of growth factors and interleukin (IL)-8.3,4 Unfortunately, information is lacking on efficient managements for TA.5 Variable outcomes have been reported with medical and surgical treatments including corticosteroids, vincristine, interferon, conventional surgery, and laser therapy.6 Laser modalities such argon-pumped tunable dye laser (APTDL), neodymium-doped yttrium aluminum garnet (Nd:YAG), and pulse dye laser (PDL) have been used by several authors as treatments for TA.5,7–9 In this case study, we describe a case of TA in a 15-year-old girl who demonstrated a good response to PDL treatment, resulting in both aesthetic improvement and pain alleviation.
Case
A 15-year-old girl presented to our Pediatric Dermatology Clinic with painful purplish red plaques on her left cheek, neck, chest, left shoulder, and back. Her father reported that the lesions were first noted at the age of three months as purplish dots on his daughter’s chest. Five years prior to admission, the lesion gradually progressed to multiple plaques and was increased in size and number, expanding to the left cheek, neck, left shoulder, and back. These skin lesions were painful. Six months prior to admission, the pre-existing skin lesions became more painful. The patient went to a dermatologist and was given 0.1% mometasone furoate cream twice daily for one month but her skin lesions became more painful, and she subsequently underwent PDL treatment. After two sessions, the skin lesions slightly faded but she was still bothered by the localized pain, thus she was referred to our clinic. There were no signs and symptoms of kaposiform hemangioendothelioma (KHE), coagulopathy, and Kasabach-Merritt phenomenon (KMP). Physical examination revealed pain, as indicated by visual analogue scale (VAS) score of 2 as well as purpura, ecchymosis, palpable purpura, purplish red plaques, and hyperpigmented macules on her left cheek, neck, chest, left shoulder, and back without any presence of warmth and tenderness upon palpation. Diascopy examination revealed that they were non-blanching lesions. Spectrophotometric measurements of erythema based on Commission Internationale de l’Eclairage (CIE) L*a*b* color analysis from the skin lesions on the left cheek, chest, left shoulder, and back, showed a* values of 11.4; 13.88; 10.6; and 15.39, respectively. Laboratory examination revealed normal platelet count and fibrinogen level. Skin biopsies were performed and histopathological findings showed lobules of tufts with a “cannonball” appearance in the dermis (Figure 1) and round oval spindle cells resembling this appearance (Figure 2). Based on these findings, the diagnosis of TA without complications was made. We treated the lesions using 595-nm PDL with 6.5−8.5 J/cm2 fluence of, 1.5 ms pulsed duration, and 5−7 mm spot size. The laser treatment was performed once every three weeks. After four sessions of treatment, a* values of spectrophotometric measurements from the skin lesions on the left cheek, chest, left shoulder, and back were decreased to 9.92; 8.92; 8.57; and 12.20, respectively. The purplish red plaques partially faded (Figures 3-6). Furthermore, the patient’s VAS score was reduced from 2 to 0.
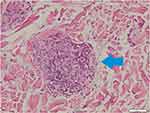 |
Figure 2 Round oval spindle cells resembling “cannon ball” appearance (blue arrow) (Hematoxylin-eosin stain, 200x magnification). |
 |
Figure 3 Comparison between skin manifestation on the left cheek and neck before (A) and after four sessions of PDL treatment (B). |
 |
Figure 4 Comparison between skin manifestation on the chest before (A) and after four sessions of PDL treatment (B). |
 |
Figure 5 Comparison between skin manifestation on the left shoulder before (A) and after four sessions of PDL treatment (B). |
 |
Figure 6 Comparison between skin manifestation on the back before (A) and after four sessions of PDL treatment (B). |
Discussion
Tufted angioma displays various clinical patterns and the most common sites of involvement include the neck, upper trunk, and shoulders.1,2,5 However, the involvement of face, scalp, or upper extremities is rare.10 It may present as a subtle stain-like area that later thickens, as a large, plaque-like, infiltrated, red or dusky blue-purple lesion, or as an exophytic, firm, rubbery, violaceous, and cutaneous nodule.1,11,12 This disease is typically painful.1,2 TA can be found at birth, but generally develops during infancy or adolescence.2 The prevalence of TA in women is similar to that in men.1,2 The diagnosis of TA is generally based on clinical and histological features.1,6 Histologically, TA demonstrate vascular tufts of tightly packed capillaries, randomly dispersed throughout the dermis in a typical “cannon ball distribution” with crescentic spaces surrounding the vascular tufts, and lymphatic-like spaces within the tumor stroma.1,13 The patient in this case report is a 15-year-old girl with painful multiple TA lesions affecting her face, indicating a rare involvement. The patient’s history revealed that the skin disorder initially appeared when she was three months old. Diagnosis of TA was confirmed by histological examinations showing infiltrating tufts of capillaries distributed in a “cannonball” pattern in the dermis.
According to Osio et al,14 there were three different clinical patterns of TA: TA without complications, TA complicated by Kasabach-Merritt syndrome (KMS) with thrombocytopenia, and TA without thrombocytopenia but with chronic coagulopathy.2,14,15 The first clinical pattern of TA occurred with no complications. The second most frequent clinical pattern was TA complicated by KMS, presenting as expanding, indurated, tender, and painful inflammatory mass with coagulopathy. Laboratory examination revealed thrombocytopenia, low fibrinogen level, and high D-dimer level.1,14 The third clinical pattern, TA without thrombocytopenia but with chronic coagulopathy, clinically presents as vascular tumor that became inflammatory with signs of warmth, erythema, edema, pain, induration, and associated with fluctuating coagulopathy and normal platelet count.14 In this case, findings from the patient’s history, as well as physical, laboratory, and histopathological examinations were consistent with TA without complications.
Some authors believe that TA lesions require only observation due to its tendency for spontaneous regression in a number of cases.14,16–18 When spontaneous regression does not occur, TA requires treatment.6,19 The management of TA is difficult and treatment guidelines have not yet been established.1,14 Treatment may be categorized as that administered for aesthetic reasons or that instituted due to complications or anticipated complications, such as KMS or functional compromises.5 Treatment options included surgical excision, topical and systemic corticosteroids, vincristine, interferon, various lasers, and intense pulsed light, with variable responses.1,11 There is thus a need for simple yet effective and less invasive procedure for TA, especially in cosmetically important areas, such as the face, head, and neck.20
Several authors have implemented laser modalities such APTDL, Nd:YAG, and PDL as treatments for TA. The use of APTDL for tufted angiomas has not been very successful,8,21 while some authors reported TA aggravation following a long pulsed Nd:YAG laser.9 On the other hand, successful results in terms of cosmetic improvement and alleviation of pain after PDL treatment have also been reported.2,5,6,11 PDL causes selective cutaneous vascular damage with minimal injury to the overlying epidermis and is used to treat a variety of vascular lesions.5,22 Laser light absorbed by hemoglobin in the vascular channels may be responsible for the perivascular damage.5 TA is histologically characterized by grouped dermal capillary tufts, providing a target for the laser.3,6 Mahendran et al5 reported that the use of 585-nm PDL with 450 microsecond pulse width was efficient in reducing pain and discomfort for pediatric TA. Their patient underwent five treatments with fluences ranging from 6.0 to 7.5 J/cm2 with 5-mm spot size and received five additional treatments with a 7-mm spot size and fluences increasing from 6.5 to 8.0 J/cm2. This result is in accordance with a case report from Cardoso et al6 who used four sessions of PDL treatment with fluences ranging from 8.0 to 9.0 J/cm2, 7-mm spot size, and pulse durations ranging from 0.45 to 3 ms for a girl with TA. By the end of the sessions, clinical improvement with an almost total decrease in pain were observed. Based on these references, we chose PDL as the treatment for our patient. We treated the lesions using 595-nm PDL with fluences ranging from 6.5 to 8.5 J/cm2, pulsed duration of 1.5 ms, and spot sizes ranging from 5 to 7 mm. After four treatments using these procedures, significant reductions of TA color and pain were achieved.
Conclusion
PDL therapy in the current case showed a satisfying result. There is a significant reduction in the color of the lesions measured by spectrophotometer and an improvement of pain as measured using VAS score, which was reduced from 2 to 0 after the 4th procedure. In conclusion, PDL is effective in reducing redness and pain for TA cases.
Ethical Statement
The publications of images were included in the parents’ consent along with the patient consent for publication of the case. Institutional approval from The Research Ethic Committee of Dr. Hasan Sadikin General Hospital Bandung, Indonesia has been obtained to publish the case details (approval number: LB.02.01/X.6.5/314/2023).
Consent Statement
The authors certify that they have obtained all appropriate patient and patient’s parents consent forms. The patient and her parents signed a consent form for the publication of the case details and images.
Acknowledgments
The authors would like to thank the staff of Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia.
Disclosure
The authors reports no conflicts of interest in this work.
References
1. McArthur K, Putggen K. Vascular tumors. In: Kang S, Amagai M, Bruckner A, et al., editors. Fitzpatricks’s Dermatol.
2. Prasuna A, Rao PN. A tufted angioma. Indian Dermatol Online J. 2015;6(4):266. doi:10.4103/2229-5178.160259
3. Su X, Liu Y, Liu Y, et al. A retrospective study: clinicopathological and immunohistochemical analysis of 54 cases of tufted angioma. IJVDL. 2020;86(1):56.
4. Bernstein EF, Kantor G, Howe N, Savit RM, Koblenzer PJ, Uitto J. Tufted angioma of the thigh. J Am Acad Dermatol. 1994;31(2):307–311. doi:10.1016/S0190-9622(94)70160-1
5. Mahendran R, White SI, Clark AH, Sheehan RA. Response of childhood tufted angioma to the pulsed-dye laser. J Am Acad Dermatol. 2002;47(4):620–622. doi:10.1067/mjd.2002.124074
6. Cardoso AO, Tayti T, Oliveira JP, et al. Tufted angioma: a case report treated with pulsed-dye laser. An Bras Dermatol. 2006;81:S273–6.
7. Ladoyanni E, Neil DA, Shah F. A tender red plaque on the elbow of a 93‐year‐old woman. Clin Exp Dermatol. 2007;32(2):
8. Metry DW, Hebert AA. Benign cutaneous vascular tumors of infancy: when to worry, what to do. Arch Dermatol. 2000;136(7):905–914. doi:10.1001/archderm.136.7.905
9. Na JI, Cho KH, Kim YG, Park KC. Angioblastoma showing aggravation after treatment with long‐pulsed Nd: YAG laser (1064 nm). Pediatr Dermatol. 2007;24(4):
10. Bedir R, Güçer H, Coskunoglu EZ, Sehitoglu I. Acquired tufted angioma: case report/Edinsel tufted angioma: olgu sunumu. Dicle Tip Dergisi. 2013;40(3):480. doi:10.5798/diclemedj.0921.2013.03.0314
11. Robati RM, Hejazi S, Shakoei S, Bidari F. Late-onset tufted angioma with remarkable response to pulsed dye laser. Indian J Dermatol. 2014;59(6):635. doi:10.4103/0019-5154.143603
12. Van Hoang M, Phan AQ, The Tran V, et al. Tufted angiomas: report of two cases. J Am Acad Dermatol. 2019;81:291–292.
13. Kim SH, Choi JH, Sung KJ, Moon KC, Koh JK. Clinical and histopathologic study on tufted angioma. Korean J Dermatol. 2000;72–78.
14. Osio A, Fraitag S, Hadj-Rabia S, Bodemer C, de Prost Y, Hamel-Teillac D. Clinic spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146(7):758–763. doi:10.1001/archdermatol.2010.135
15. Pfister BK, King EC, Samet JD, Gulliver J, Wolf SF. Tufted angioma of the index finger middle phalanx. J Am Acad Orthop Surg Glob Res Rev. 2022;6(7):1–5.
16. Li MF, Zeng XS, Zhang GY, et al. Facial tufted angioma: a case report. Int J Dermatol Venereol. 2018;1(02):126–128.
17. Browning J, Frieden I, Baselga E, Wagner A, Metry D. Congenital, self-regressing tufted angioma. Arch Dermatol. 2006;142(6):
18. McKenna KE, McCusker G. Spontaneous regression of a tufted angioma. Clin Exp Dermatol. 2000;25(8):656–658. doi:10.1046/j.1365-2230.2000.00730-3.x
19. Fabbri N, Quarantotto F, Caruso A, et al. Surgical excision of a tufted angioma of the hand in an adult—a rare case report with a review of literature. AME Case Rep. 2019;3:
20. Zawar V, Karad G, Pawar M. Propranolol followed by a foam sclerotherapy for treatment of tufted angioma over neck: a novel therapeutic approach. J Cutan Aesthet Surg. 2020;13(4):335. doi:10.4103/JCAS.JCAS_106_19
21. Tan OT, Carney JM, Margolis R, et al. Histological responses of port wine stains treated by argon, carbon dioxide, and tunable lasers. A preliminary report. Arch Dermatol. 1986;122:1016–1022.
22. Vazquez T, Forouzandeh M, Gurnani P, Akhtar S, Nouri K. Cutaneous vascular lesions in the pediatric population: a review of laser surgery applications and lesion-specific device parameters. Lasers Med Sci. 2020;35(8):
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

