Back to Journals » Clinical Ophthalmology » Volume 17
Effectiveness of Intra-Arterial Chemotherapy for the Treatment of Intraocular Retinoblastoma: Relevance of a Multidisciplinary Setting
Authors Castela G , Providência J , Monteiro M, Oliveiros B, Silva S, Brito M , Machado E, Neto Murta J, Castelo-Branco M, Correa Z
Received 7 December 2022
Accepted for publication 20 January 2023
Published 2 February 2023 Volume 2023:17 Pages 487—496
DOI https://doi.org/10.2147/OPTH.S398488
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Guilherme Castela,1– 3 Joana Providência,1,2 Madalena Monteiro,1 Bárbara Oliveiros,2 Sónia Silva,4 Manuel Brito,4 Egídio Machado,5 Joaquim Neto Murta,1,2 Miguel Castelo-Branco,2,3,* Zélia Correa6,*
1Department of Ophthalmology, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 2Faculty of Medicine, University of Coimbra (FMUC), Coimbra, Portugal; 3Coimbra Institute for Biomedical Imaging and Translational Research (CIBIT), Coimbra, Portugal; 4Department of Pediatric Oncology, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 5Department of Medical Imaging, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 6University of Miami, Bascom Palmer Eye Institute, Miami, FL, USA
*These authors contributed equally to this work
Correspondence: Guilherme Castela, Department of Ophthalmology, Centro Hospitalar e Universitário de Coimbra, Praceta Prof Mota Pinto, Coimbra, 3004-561, Portugal, Tel +351919702206, Email [email protected]
Purpose: We aim to report about effectiveness and safety in the context of our centers’ setting in the management of retinoblastoma with intra-arterial chemotherapy (IAC) in a 5-year retrospective analysis of the Portuguese population.
Patients and Methods: Retrospective analysis of consecutive cases of retinoblastoma selected to initiate IAC between 2015 and 2020, at the Portuguese National Reference Center. All included patients underwent complete ophthalmological evaluation under anesthesia with fundus photography. Diagnosis and classification of retinoblastoma was made according to the International Classification of Intraocular Retinoblastoma (ICRB). The patients were further divided into two groups: Group I for primary IAC and Group II for secondary IAC. Tumor recurrence or relapses, systemic metastasis and deaths were documented. Main efficacy outcome included ocular salvage and recurrence-free survival rates estimated using the Kaplan–Meier method.
Results: Twenty-eight eyes (19 eyes included in Group I and 9 eyes included in Group II) were eligible and a total of 130 IAC procedures were performed, with a median number of sessions of 4 (range 1– 8) for each treated eye, during a median follow-up of 21 months (range 4– 64). Of the included eyes, 22 (78.6%) were preserved. An overall survival of 100% was achieved. Considering the preserved eyes, the overall median decimal visual acuity achieved at the last visit was 0.15 (range 0.02– 0.8). Three patients had permanent adverse events related to IAC (cataract, vitreous hemorrhage and choroidal ischemia). Considering the survival analysis of recurrence, the mean survival without recurrence was 84.2% for Group I and 66.7% for Group II, and the mean survival without enucleation was 78.6% (no events in Group II).
Conclusion: IAC has been shown to be an effective and safe treatment for children with intraocular retinoblastoma. This study demonstrates that IAC is effective even in moderate sample sizes, when a multidisciplinary approach is available.
Keywords: retinoblastoma, intra-arterial chemotherapy, ocular oncology, pediatric oncology
Introduction
Retinoblastoma is the most common malignant eye tumor in the pediatric population. However, with its estimated incidence of 1 in 16,000 to 18,000 live births, it is considered a rare disease, with only a few centers of expertise dedicated to its management worldwide.1 Treatment modalities for retinoblastoma have shown tremendous improvement in survival and globe salvage in recent decades. Intra-arterial chemotherapy (IAC) is now considered one of the primary treatment modalities for intraocular retinoblastoma worldwide. Compared with conventional intravenous chemotherapy (IVC), IAC has been demonstrated to provide more efficacy in eye salvage of group D and E retinoblastoma, with the advantage of minimal systemic toxicity.2
Intra-arterial chemotherapy for the treatment of intraocular retinoblastoma was first performed by Algernon B. Reese in 1958, with direct internal carotid artery injection; it wasabandoned due to systemic toxicity of the drug used, triethylene melamine. In 1998, Kaneko et al revisited the idea of selective ophthalmic artery infusion, describing the technique of introducing a microballoon catheter through a transfemoral approach to administer melphalan at higher concentrations. However, with this new described technique, small arterial branches proximal to the origin of the ophthalmic artery were also infused, making it not truly selective.3 The Japanese group was pioneering in describing melphalan as superior to other chemotherapeutic drugs used in the treatment of retinoblastoma. In 2006, the group of Abramson and Gobin described a refined technique of direct catheterization of the ophthalmic artery using a guide wire.4
Currently, the procedure of IAC is done under general anesthesia by an interventional neuroradiologist experienced with the anatomic dimensions of pediatric vasculature. A microcatheter is positioned at the ostium of the ophthalmic artery through a femoral artery access. A selective contrast angiogram is performed to confirm the catheter placement and to assure a proper flow of the ophthalmic artery to the eye, and then the chemotherapy drugs (melphalan, topotecan and/or carboplatin) are injected manually by repeated small boli.4,5
In the last few years, different groups have reported the efficacy and safety of IAC used as a primary treatment,6–11 as salvage therapy in advanced disease, including vitreous seeding and retinal detachment,12–15 in bilateral cases16 and in cases refractory to other treatments.17–20 However, definite protocols to guide individualized treatment regimens are still lacking and decision-making is mainly based on experts’ opinions and consensus.21
Since 2015, all children diagnosed with retinoblastoma in Portugal, previously referred to international centers for management, started to be treated at the Portuguese National Reference Center for Ocular Tumors, located at Centro Hospitalar e Universitário de Coimbra. A multidisciplinary team, including pediatric ophthalmologists, pediatric oncologists and an interventional neuroradiologist, specialized in the management of retinoblastoma, having the capacity of performing all the modalities of treatment, namely, IVC, IAC, adjuvant treatments (transpupilar thermotherapy, cryotherapy and intravitreal chemotherapy), enucleation and, when necessary, orbital surgery. The aim of our study is to report our initial 5-years’ experience with IAC for the treatment of intraocular retinoblastoma.
Materials and Methods
Patients
We performed a 5-year retrospective study including children consequently diagnosed with intra-ocular retinoblastoma and selected to initiate IAC at the Portuguese National Reference Center, between October 2015 and October 2020. Our study was approved by the ethics committee of University of Coimbra and of Centro Hospitalar e Universitário de Coimbra. Parents of the included subjects have given their written informed consent for the data collection and analysis. The exclusion criteria were: extraocular invasion or metastatic disease (both considered contra-indication to IAC) and opacities of media precluding ocular fundus observation. Diagnosis and classification of retinoblastoma was made according to the International Classification of Intraocular Retinoblastoma (ICRB)22 by the multidisciplinary team, based on ophthalmological examination under general anesthesia, complemented with Retcam fundus photographs and magnetic resonance images. When considered necessary, fundus photographs were complemented with fluorescein angiography images performed with Retcam. The decision to initiate IAC was determined by the treatment team according to specialists’ recommendations.21
Treatment
All patients received one cycle of IAC, performed by an interventional neuroradiologist, every 4 weeks until the tumor was considered controlled by the multidisciplinary team, which observed the lesions under general anesthesia every 4 weeks (3 weeks after the last IAC session). The chemotherapeutic drugs used included melphalan (dose-adjusted to age, 3 mg between 6 to 12 months, 3.5 mg between 12 to 24 months, 4 mg after 24 months), topotecan 1 mg and/or carboplatin (40–70 mg). IAC was injected in the ostium of the ophthalmic artery via the femoral artery. Unilateral and bilateral retinoblastoma Group B, C and D, according to ICRB Classification, were considered for IAC. Group E eyes were enucleated and excluded from this study. In the case of bilateral retinoblastoma in which one of the eyes was Group E, IVC was preferred to IAC as the initial treatment of the fellow eye when the team considered high the risk of extraocular invasion.23 Patients elected to IAC but under 6 months and/or under 6 kg in weight started IVC (with a combination triple-drug regimen of carboplatin, etoposide and vincristine) until IAC could be performed, according to the bridge therapy regimen described by Abramson et al.24 Patients with bilateral retinoblastoma, when both eyes were eligible for IAC, were treated with melphalan in the worst eye and a combination of topotecan and carboplatin in the best eye, according to the tandem therapy regimen described by Abramson et al.25
The included patients were further divided into two groups: Group I included patients treated primarily with IAC and patients treated with bridge therapy and Group II included patients treated with IAC as a second-line treatment or salvage therapy, after IVC was first performed. In Group II patients, IVC was the first-line therapy due to bilateral disease with pathologic prognostic criteria to perform IVC.
Fundus examinations under anesthesia were performed using indirect ophthalmoscopy and images were recorded using RetCam. Local adjuvant treatments (laser transpupillary thermotherapy, cryotherapy and intravitreal chemotherapy with topotecan) were performed as needed during ophthalmological observations, according to the following indications: laser transpupillary thermotherapy in case of suspicious lesions located outside the posterior pole, cryotherapy in case of suspicious lesions located in the extreme periphery, not achieved correctly by laser treatment and intravitreal chemotherapy in case of vitreous seeding.
Enucleation was performed in the case of potential tumor spread, uncontrolled disease or media opacities that precluded fundus observation.
After the decision to stop IAC, patients continued to be followed every 4 weeks under general anesthesia for 6 to 8 months, after which visits started to be gradually spaced. When collaboration of the children permitted, usually after 4 years of age, observations started to be performed at a regular outpatient clinic.
A new tumor was defined as the development of a tumor concurrent with or after IAC that was not observed at initial diagnosis. Recurrence was defined as the regrowth of retinal tumors, subretinal or vitreous seeds after a satisfactory initial response to IAC. New tumors and recurrences were treated with IAC when possible, consolidated with transpupillary thermotherapy and cryotherapy. Alternative treatment strategies included intravitreal chemotherapy (in case of vitreous seeding), plaque brachytherapy and enucleation.
Data Collection and Statistical Analysis
Patients were characterized in terms of demographics (age at diagnosis, sex, clinical signs at presentation and family history), tumor characteristics (eye stage according to ICRB and laterality) and treatment protocol (number of IAC cycles, drugs used in each cycle and additional treatments performed). During follow-up visits each eye was assessed for regression of retinoblastoma, vitreous seeds and subretinal seeds. Tumor recurrence or relapses, systemic metastasis and deaths were documented. Relevant ocular and systemic complications were recorded. Data was recorded using an electronic registration system and posteriorly an electronic database was created. Main efficacy outcome included ocular salvage and recurrence-free survival rates estimated using the Kaplan–Meier method. As a secondary efficacy outcome of IAC, visual acuity was measured according to age (preferential looking before 2 years of age, Lea chart between 2 and 4 years of age; Tumbling “E” after 4 years old).
Follow-up time was considered the time, in months, between the last treatment (the treatment after which the team decided the tumor was inactive and IAC were stopped) and the last follow-up evaluation. For survival analysis, recurrence-free time was considered the time between the last treatment and the last follow-up evaluation. Ocular salvage time was calculated between the time of inclusion in the study and the last follow-up visit.
All statistical analysis was performed using IBM SPSS Statistics 26 for Windows. Chi-square tests were used for categorical variables and the non-parametric Mann–Whitney to continuous variables. A p-value under 0.05 was considered as statistically significant.
Results
Patient Characteristics
From October 2015 to October 2020, a total of 28 eyes from 23 children were eligible to initiate IAC at our center, as a primary or secondary treatment for intraocular retinoblastoma. From the included children, 12/23 (52.2%) were males and the median age at diagnosis was 14.35 months (range 3–50). Thirteen (13/23, 56.5%) patients were diagnosed with heritable retinoblastoma (from whom two presented with unilateral retinoblastoma and heritability was confirmed with a positive genetic test for a pathogenic mutation of RB) and only 3/23 (13%) had a positive family history of retinoblastoma. Clinical characteristics of the included patients can be found in Table 1.
 |
Table 1 Clinical Characteristics of the Included Participants |
At presentation, 16/23 (69.6%) reported leukocoria and 10/23 (43.5%) strabismus (3/23 children presented concomitantly leukocoria and strabismus). The classification of the included eyes according to the ICRB Classification was as follows: 4/28 (14.3%) eyes were considered Group B, 7/28 (25%) Group C and 17/28 (60.7%) Group D. Pineal involvement was not reported in any of the patients. Subretinal seeding was present in 17/28 (60.7%) eyes, vitreous seeding in 8/28 (28.6%) eyes, macular involvement in 17/28 (60.7%) eyes and multifocal lesions in 17/28 (60.7%) eyes (Table 1).
Considering the study groups, 19/28 (67.9%) eyes were included in Group I and were treated with IAC as a first-line treatment. In this group were included 3 eyes treated with bridge therapy (IVC until IAC could be initiated) and 4 eyes (from 2 patients) treated with tandem therapy (melphalan in the worst eye and association of carboplatin with topotecan in the best eye).
Nine eyes (9/28, 32.1%) were included in Group II: in 4/9 (44%) eyes, IAC was used after 6 cycles of IVC to consolidate the treatment and, in 5/9 (56%) eyes, IAC was used due to a recurrence in an eye that was previously treated with IVC. All included eyes corresponded to bilateral and hereditary retinoblastoma. Patients included in this group were diagnosed with retinoblastoma at a significantly younger age compared to eyes included in Group I (p=0.012). In this group, 4/9 (44%) eyes underwent tandem therapy.
Treatment Characterization
A total of 130 IAC procedures were performed, with a median number of 4 sessions (range 1–8) for each treated eye. No catheterization failures were reported.
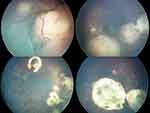
Nineteen (19/28, 67.9%) eyes were treated only with melphalan; 4/28 (14.3%) eyes were treated with topotecan and carboplatin (corresponding to the better eye of a bilateral retinoblastoma treated with tandem therapy); 4/28 (14.3%) were treated with melphalan and topotecan; and 1/28 (3,6%) was treated with the 3 agents (melphalan, topotecan and carboplatin) (Table 2 and Figure1)
 |
Table 2 Treatment Characteristics and Outcomes |
Twenty-one (21/28, 75%) of the included eyes underwent treatment consolidation with transpupillary thermotherapy (median 2 sessions, range 1–6), 2/28 (7.1%) eyes underwent cryotherapy and 2/28 (7.2%) eyes were submitted to intravitreal injection of topotecan due to vitreous seeding.
In Group I the median number of IAC cycles was 4 (1–8) compared to 3 (2–4) in Group II (p=0.035).
The median follow-up after treatment was 25.79 months (range 6–57), specifically 30.95 (range 6–57) in Group I and 14.89 (range 6–45) in Group II (p=0.02).
Anatomical and Functional Outcomes
Of the included eyes, 22/28 (78.6%) were preserved. From the 6/28 (31.6%) enucleated eyes, all from Group I, 2 corresponded to the worst eye of a child diagnosed with bilateral retinoblastoma. Considering their ICRB classification, 5 eyes were Group D and 1 eye was Group C (which was enucleated after developing a vitreous hemorrhage that precluded observation of the fundus) (Table 2).
Six (6/28, 21.4%) eyes had recurrence of the tumoral activity, diagnosed during the follow-up visits. From the eyes with recurrence (3 from Group I and 3 from Group II), 4 corresponded to patients with heritable retinoblastoma. All recurrences responded to IAC, which was performed by associating 2 or 3 drugs, and no recurrence resulted in enucleation. Globe salvage and recurrences during the follow-up period were not statistically significantly different between the two groups (p-value of 0.057 and 0.678, respectively). No metastases were detected during the follow-up period and an overall survival of 100% was achieved.
Considering the survival analysis of recurrence, the overall free recurrence was 78.6% (84.2% in Group I and 66.7% in Group II) at 60 months of follow-up. The mean recurrence-free time in Group I was 54.91 ± 4.81 months versus 34.33 ± 6.93 months in Group II, which was not statistically significant (p=0.134). Recurrences occurred between 3 and 14 months after treatment (Figure 2A).
 |
Figure 2 Kaplan–Meier survival curves for IAC in heritable and sporadic retinoblastoma. Overall globe survival (A) and recurrence-free survival of Group I (blue line) and Group II (red line) (B). |
The overall globe survival was 78.6% (68.4% in Group I and 100% in Group II, p=0.07) at 60 months of follow-up. The mean globe survival time was 51.46 ± 4.53 months (enucleations occurred between 2 and 8 months of follow-up) and groups could not be compared in terms of this measure as no events were registered during the follow-up period in Group II (Figure 2B).
Considering the preserved eyes, the overall median decimal visual acuity achieved at the last visit was 0.15 (range 0.02–0.8). Final median visual acuity was 0.2 in Group I compared to 0.06 in Group II (p=0.21).
Local IAC complications, including erythema, ptosis and hair loss, were transitory and were not reported. Three patients from Group I had permanent adverse events related to IAC, specifically one case of cataract (who after one year of being recurrence-free was submitted to surgery), one case of vitreous hemorrhage (in this case the eye was enucleated) and one choroidal ischemia (with consequent loss of functionality of the eye). Only one patient from Group II presented complications, a transient femoral artery thrombosis during an IAC procedure. Major systemic events, including grade IV neutropenia, were not reported.
Discussion
Our study’s results reflect the initial experience with IAC in the one Portuguese reference center for retinoblastoma treatment. During these 5 years, we gained experience in the treatment of different staging-groups and with vast treatment modalities, including tandem therapy, bridge therapy and adjuvant local treatments such as transpupillary thermotherapy, cryotherapy and intravitreal chemotherapy, achieving a global globe preservation of 78.6%. Patients that would have previously been treated abroad were successfully managed in our country, lowering the cost and burden of the treatment for the children and their parents. Considering the preserved eyes, we also achieved a favorable functional outcome with a median decimal visual acuity of 0.15, which corresponds to a preliminary value that can possibly be improved in the future with improved collaboration of older children allied to amblyopia management of vision-deprived eyes. We did not experience severe systemic complications associated with IAC and believe this treatment presents a good safety profile. This study is therefore important to demonstrate that IAC is an effective treatment that can be successfully applied in centers with a moderate number of patients when a multidisciplinary team is available.
In terms of globe preservation and recurrence-free survival, our study shows similar results to previously published literature.2,6,8,9 Our median number of IAC sessions per eye was 4, which is slightly superior to the median number of 3 sessions per eye reported by other groups.2,10 We believe that in our results some patients were possibly over-treated. However, with these results, in future the treatment-committee group will be able to make the decision to stop IAC earlier with more confidence.
All the 5 eyes that presented recurrences during the follow-up period, and that otherwise would have been enucleated, were successfully treated with multi-drug IAC. This confirms the previously reported efficacy of IAC in the treatment of recurrent and relapsing cases.9,17
Comparing the two study groups, we found a superior proportion of recurrences in Group II, although not statistically significant. We think this might be associated with the fact that Group II included more advanced and resistant cases (bilateral cases that needed systemic chemotherapy first and then consolidation with IAC or cases of recurrence after initial treatment with systemic chemotherapy), as both bilateral and advanced cases have been associated with higher recurrence rates and global resistance to treatment.26–28 However, a definite conclusion cannot be extrapolated due to the small number of cases and consequently no statistically significant results. We also found a superior proportion of enucleation in Group I; however, no definite conclusions can be made about this result as Group II included only bilateral cases and, in many, the other eye had already been enucleated due to advanced disease, therefore biasing the decision of enucleation, which was possibly less performed as we preferred alternative rescue therapies.
Considering the time until recurrence, when comparing to previously published papers from other groups, we found that apparently our sample had earlier recurrences (at a mean of 6.33 months). A recently published paper reported that recurrences and new tumor development after intravenous chemotherapy occurred at a mean time of 10.7 months and that risk factors for recurrence included heritable retinoblastoma, tumor base diameter > 12 mm and presence of subretinal seeding.29 We cannot fully explain the difference in our sample, but we think it can be related to the high number of heritable retinoblastoma and advanced cases and also possibly with an inferior number of IAC sessions than needed, as we tend to stop treatment as soon as lesions seem stable, to avoid toxicity of IAC, preferring to maintain monthly surveillance during the first 6 months after IAC. However, the overall recurrence rate found in our sample was similar to that reported recently in two different cohorts, where a recurrence rate of approximately 25% was described.30,31
Compared to systemic chemotherapy, IAC demonstrated an excellent safety profile. In our series, no severe systemic complications were found and only one transient femoral arterial thrombosis was reported. Local complications were mostly transitory except for a vitreous hemorrhage resulting in globe enucleation (posteriorly, the pathological report described a complete calcification of the tumor), a cataract and the occurrence of severe choroidal ischemia in one eye.
Our initial functional evaluation in preserved globes treated with IAC reflects a good visual function. We believe that in the future the best visual acuity results can be obtained. In our sample, patients with poorer functional results presented macular tumors and the results were not directly related to the therapy, except for the eye that presented with severe choroidal ischemia after an IAC session. Few groups have reported functional results after IAC due to the difficulty in visual function assessment in infants, so we hope our results can contribute to the global awareness of visual preservation after IAC.15
Patients included in Group II were previously treated with IVC and represent cases of recurrence after the systemic treatment and cases in which IVC was not considered sufficient to control the lesions. Moreover, in this group 100% of patients had heritable retinoblastoma and in most cases the worst eye had already been enucleated, and the eye included in this study was the better eye, which explains the higher rate of globe salvage in this group.
Limitations of our study include the small sample size, which is related to retinoblastoma being a rare tumor with a mean incidence in our country of 4 to 6 cases per year and with a significant proportion of cases not eligible for IAC due to advanced disease. We also recognize a bias effect related to the learning curve as these results represent our initial experience. We also recognize our follow-up period is insufficient to evaluate long-term results and complications and we hope that in the future this information can be also evaluated. Furthermore, we did not include results of IAC used in intraocular tumors from Group E, which has already been described in the literature as an effective option in some cases.11,18 Shields et al reported a global 5-year globe salvage of 76% for primary therapy with IAC, however with values of 100% for Groups B and C, 86% for group D, and only 55% for group E.11 They concluded that intra-arterial chemotherapy is now most often used for unilateral retinoblastoma, for eyes in Groups B, C, and D, and occasionally E. Furthermore, we emphasize that there is great variability in the different classifications of intraocular retinoblastoma and there are different Group E patients, including from tumors that involve more than 50% of the vitreous cavity to patients with anterior chamber invasion and neovascular glaucoma. So, although in our sample we did not include Group E patients, we think that in some less advanced Group E patients IAC would be a reasonable possibility. We hope that with our growing experience we will start to use IAC in more advanced disease, including some Group E patients.
Conclusion
IAC has been shown to be an effective and safe treatment for children with intraocular retinoblastoma in our center. Our gained experience and favorable results with this treatment modality will allow us to broaden the use of IAC to more advanced stages of retinoblastoma and also in the treatment of recurrent and relapsing tumors. In the future, more globes will be preserved in our country, possibly with a good visual function.
Statement of Ethics
Research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. This study protocol was reviewed and approved by Ethics Committee of Centro Hospitalar e Universitário de Coimbra (CE-CHUC). Written informed consent was obtained from participants’ parents or legal guardians to participate in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was supported by the Portuguese national funding agency for science, research and technology (FCT) (UID/4950/2020).
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Seregard S, Lundell G, Svedberg H, Kivelä T. Incidence of retinoblastoma from 1958 to 1998 in Northern Europe: advantages of birth cohort analysis. Ophthalmology. 2004;111(6):1228–1232. doi:10.1016/j.ophtha.2003.10.023
2. Manjandavida FP, Stathopoulos C, Zhang J, Honavar SG, Shields CL. Intra-arterial chemotherapy in retinoblastoma – a paradigm change. Indian J Ophthalmol. 2019;67(6):740–754. doi:10.4103/ijo.IJO
3. Yamane T, Kaneko A, Mohri M. The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol. 2004;9(2):69–73. doi:10.1007/s10147-004-0392-6
4. Abramson DH, Dunkel IJ, Brodie SE, Kim JW, Gobin YP. A Phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma. Initial results. Ophthalmology. 2008;115(8):1398–1405. doi:10.1016/j.ophtha.2007.12.014
5. Abruzzo TA, Geller JI, Kimbrough DA, et al. Adjunctive techniques for optimization of ocular hemodynamics in children undergoing ophthalmic artery infusion chemotherapy. J Neurointerv Surg. 2015;7(10):770–776. doi:10.1136/neurintsurg-2014-011295
6. Abramson DH, Dunkel IJ, Brodie SE, Marr B, Gobin YP. Superselective ophthalmic artery chemotherapy as primary treatment for retinoblastoma (chemosurgery). Ophthalmology. 2010;117(8):1623–1629. doi:10.1016/j.ophtha.2009.12.030
7. Aziz HA, Boutrid H, Murray TG, et al. Supraselective injection of intraarterial melphalan as the primary treatment for late presentation unilateral multifocal stage VB retinoblastoma. Retina. 2010;30(4SUPPL. 4):63–65. doi:10.1097/IAE.0b013e3181cbda0f
8. Shields CL, Bianciotto CG, Jabbour P, et al. Intra-arterial chemotherapy for retinoblastoma: report no. 1, control of retinal tumors, subretinal seeds, and vitreous seeds. Arch Ophthalmol. 2011;129(11):1399–1406. doi:10.1001/archophthalmol.2011.150
9. Thampi S, Hetts SW, Cooke DL, et al. Superselective intra-arterial melphalan therapy for newly diagnosed and refractory retinoblastoma: results from a single institution. Clin Ophthalmol. 2013;7:981–989. doi:10.2147/OPTH.S43398
10. Gobin YP. Intra-arterial chemotherapy for the management of retinoblastoma. Arch Ophthalmol. 2011;129(6):732. doi:10.1001/archophthalmol.2011.5
11. Shields CL, Dockery PW, Yaghy A, et al. Intra-arterial chemotherapy for retinoblastoma in 341 consecutive eyes (1292 infusions): comparative analysis of outcomes based on patient age, race, and sex. J AAPOS. 2021;25(3):150.e1–e150.e9. doi:10.1016/j.jaapos.2020.12.006
12. Peterson EC, Elhammady MS, Quintero-Wolfe S, Murray TG, Aziz-Sultan MA. Selective ophthalmic artery infusion of chemotherapy for advanced intraocular retinoblastoma: initial experience with 17 tumors. J Neurosurg. 2011;114(6):1603–1608. doi:10.3171/2011.1.JNS10466
13. Abramson DH, Marr BP, Dunkel IJ, et al. Intra-arterial chemotherapy for retinoblastoma in eyes with vitreous and/or subretinal seeding: 2-Year results. Br J Ophthalmol. 2012;96(4):499–502. doi:10.1136/bjophthalmol-2011-300498
14. Shields CL, Kaliki S, Shah SU, Bianciotto CG, Jabbour P. Effect of intraarterial chemotherapy on retinal detachment. Retina. 2012;32(4):799–804.
15. Chen Q, Zhang B, Dong Y, et al. Intra-arterial chemotherapy as primary or secondary treatment for infants diagnosed with advanced retinoblastoma before 3 months of age. BMC Cancer. 2019;19(1):1–8. doi:10.1186/s12885-019-5844-5
16. Abramson DH, Marr BP, Francis JH, et al. Simultaneous bilateral ophthalmic artery chemosurgery for bilateral retinoblastoma (tandem therapy). PLoS One. 2016:1–11. doi:10.1371/journal.pone.0156806
17. Say EAT, Iyer PG, Hasanreisoglu M, et al. Secondary and tertiary intra-arterial chemotherapy for massive persistent or recurrent subretinal retinoblastoma seeds following previous chemotherapy exposure: long-term tumor control and globe salvage in 30 eyes. J AAPOS. 2016;20(4):337–342. doi:10.1016/j.jaapos.2016.05.009
18. Li J, Jing C, Hua X, et al. Outcome of salvage intra-arterial chemotherapy for recurrent retinoblastoma. Eye. 2021. doi:10.1038/s41433-021-01693-w
19. Mirzayev I, Gündüz AK, Yavuz K, et al. Secondary intra-arterial chemotherapy and/or intravitreal chemotherapy as salvage treatment for retinoblastoma. Eur J Ophthalmol. 2021;31(5):2692–2698. doi:10.1177/1120672120957587
20. Hua J, Gang S, Yizhou J, Jing Z. Intra-arterial chemotherapy as second-line treatment retinoblastoma: a 2-year single-center study in China for advanced. J Cancer Res Ther. 2019;1:106–110.
21. Abramson DH, Shields CL, Munier FL, Chantada GL. Treatment of retinoblastoma in 2015: agreement and disagreement. JAMA Ophthalmol. 2015;133(11):1–7. doi:10.1001/jamaophthalmol.2015.3108
22. Shields CL, Shields JA. Basic understanding of current classification and management of retinoblastoma. Curr Opin Ophthalmol. 2006;17(3):228–234. doi:10.1097/01.icu.0000193079.55240.18
23. Brodie SE, Abramson DH, Navarro BV. Success of intra-arterial chemotherapy (chemosurgery) for retinoblastoma. J Proteom. 2015;130(2):180–185. doi:10.1016/j.jprot.2015.09.027
24. Gobin YP, Dunkel IJ, Marr BP, Francis JH, Brodie SE, Abramson DH. Combined, Sequential Intravenous and Intra-Arterial Chemotherapy (Bridge Chemotherapy) for Young Infants with Retinoblastoma. PLoS One. 2012;7(9):e44322. doi:10.1371/journal.pone.0044322
25. Abramson DH, Dunkel IJ, Brodie SE, Marr B, Pierre Gobin Y. Bilateral superselective ophthalmic artery chemotherapy for bilateral retinoblastoma: tandem therapy. Archiv Ophthalmol. 2016;128(3):370–372.
26. Michaels ST, Abruzzo TA, Augsburger JJ, Correˆa M, Lane A, Geller JI. For advanced intraocular retinoblastoma: cchmc early experience. J Pediatr Hematol/Oncol. 2016;38(1):65–69. doi:10.1097/MPH.0000000000000471
27. Abramson DH, Fabius AWM, Issa R, et al. Advanced Unilateral retinoblastoma: the impact of ophthalmic artery chemosurgery on enucleation rate and patient Survival at MSKCC. PloS One. 2015;2009:1–9. doi:10.1371/journal.pone.0145436
28. Ravindran K, Dalvin LA, Pulido JS, Brinjikji W. Intra-arterial chemotherapy for retinoblastoma: an updated systematic review and meta-analysis. J Neurointerv Surg. 2019;11(12):1266–1272. doi:10.1136/neurintsurg-2019-014909
29. Gündüz AK, Mirzayev I, Dinçaslan H, Özalp Ateş FS. Recurrence and new tumor development after frontline intravenous chemotherapy for retinoblastoma: risk factors and treatment results. Eur J Ophthalmol. 2022;32(3):1795–1803. doi:10.1177/11206721211023311
30. Francis JH, Roosipu N, Levin AM, et al. Current treatment of bilateral retinoblastoma: the impact of intraarterial and intravitreous chemotherapy. Neoplasia. 2018;20(8):757–763. doi:10.1016/j.neo.2018.05.007
31. Francis JH, Levin AM, Zabor EC, Gobin YP, Abramson H. Ten-year experience with ophthalmic artery chemosurgery: ocular and recurrence-free survival. PLoS One. 2018;13(5):1–17.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.