Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Effectiveness of Heart Failure Checklist Management in Patients with Chronic Heart Failure: An Open-Label, Single-Center Controlled Study During 18 Months of Follow-Up
Authors Xu X , Cheng J, Zhang Y, Wang X , Chen M , Xu L, Zhao W
Received 9 August 2023
Accepted for publication 16 November 2023
Published 27 November 2023 Volume 2023:19 Pages 983—992
DOI https://doi.org/10.2147/TCRM.S417426
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Deyun Wang
Xiaorong Xu,* Jing Cheng,* Yeping Zhang, Xin Wang, Mulei Chen, Lin Xu, Wenshu Zhao
Heart Center and Beijing Key Laboratory of Hypertension, Beijing Chaoyang Hospital Affiliated to Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenshu Zhao; Lin Xu, Email [email protected]; [email protected]
Background: The efficacy of chronic heart failure (CHF) checklist management in reducing adverse outcomes of heart failure patients is still uncertain. This study explores whether CHF checklist management is more useful than usual care in reducing adverse health outcomes in the medium- and long-term among CHF patients.
Methods: In our prospective study, 132 patients with CHF were randomly assigned to CHF management group and usual care group by random number method. Patients in CHF management group were conducted through CHF checklist by cardiologists and general practitioner. Patients assigned to usual care were treated by non-stationary medical group without checklist. All groups were followed up for 18 months.
Results: There was no significant difference in overall mortality rate between management group and control group during 18 months (12.3% [8/65] vs. 11.7% [7/60], P = 0. 912]). The re-hospitalization rate of heart failure in management group (18.5% [12/65]) was significantly lower than that in usual care group (38.3% [23/60]) after 18 months of follow-up (P = 0.013). Median NT-proBNP level (632.3 ng/l vs. 1678 ng/l, p = 0.004) was lower in management group than that in usual care group. Cardiac ultrasonography was performed at 18 months between the management and usual care group. LVEDD (55.88± 7.11 mm vs. 60.92± 8.06 mm) and LVESD (43.25± 8.42mm vs. 48.41± 9.02mm) were decreased (P< 0.01). LVEF was increased (45.36± 10.64% vs. 39.96 ± 10.15%, P< 0.01). The utilization rate of ACEI/ARB/ARNI, β-blocker were high in management group.
Conclusion: CHF checklist management by cardiologists and general practitioners can significantly reduce the re-hospitalization and improve cardiac function. CHF management through heart failure checklist may improve prognosis in patients with CHF in the medium- and long-term.
Keywords: chronic heart failure, heart failure management, heart failure checklist, prognosis, re-hospitalization rate, CHF
Introduction
Chronic heart failure (CHF) is a major health challenge worldwide affecting approximately 26 million people all over the world.1 According to the most recent 2019 data in China, more than 13.7 million people of the Chinese adult population had CHF.2
It is still highly controversial whether or not CHF management programs can improve prognosis. CHF management interventions might reduce the risk of hospital readmission by providing ongoing, direct support to patients at home. Several studies showed that CHF management reduced all-cause hospital readmission rates and mortality among CHF patients.3,4 However, there were some studies that CHF management programs failed to improve clinical outcomes in CHF patients.5,6 The different results may be due to types of interventions of these programs, local medical model and process, patient characteristics, and quality of medical care given to patients with CHF.7
It is difficult to make individualized adjustment of medication for patients during limited hospitalization time. Moreover, there was no heart failure outpatient department to uniformly manage patients with CHF in most hospitals.
We develop CHF checklist as an important tool for long-term heart failure management, according to CHF management programs in previous projects and be involved in the new guidelines.8,9 The CHF management mainly included health mission, complications therapy, coordination of care, monitoring disease symptoms and medication taken, lifestyle advice, and management of body weight, blood pressure and heart rate, etc. CHF checklist can quantify disease management, which may make implement of CHF management simpler and easier. CHF checklist management also provides a basis for community management mode of CHF.
We hypothesized that using a simple checklist for HF may be associated with better quality of care and decreased readmissions for these patients.
Methods
Study Design
In our open-label randomized trial, we compared the effects of CHF checklist management versus usual care among ambulatory adult patients with CHF. Inclusion criteria: (1) Adult patients with CHF with moderate-to-severe CHF (New York Heart Association [NYHA] functional classes II to IV). Diagnosis of heart failure was based on typical signs and symptoms and abnormal cardiac structure and function: echocardiogram shows left ventricular ejection fraction (LVEF) ≤45% (echocardiogram results within half a year);10 (2) Patients aged 18–75 years; (3) Patients and family members sign informed consent.
Exclusion criteria: Patients with severe comorbidity (pericardial effusion, constrictive pericarditis and other extra-cardiac diseases, Malignant tumor, severe liver and kidney insufficiency, severe blood disease), functional or cognitive impairment, participate in any other relevant research, Unwilling to join this study, and substance abuse.
A total of 200 patients with definite diagnosis of CHF admitted to the Heart Center of Beijing Chaoyang Hospital Affiliated to Capital Medical University from June 30, 2017 to June 30, 2018 were selected. Three were 68 participants were excluded, of whom 30 participants were found non-eligible because of exclusion criteria, and 38 participants refused participation. There were 132 patients diagnosed with CHF were included in our study, they were randomly assigned to CHF checklist management or usual care, using random number method (Randomization: 1:1 ratio). This study was approved by the Ethics Committee of Beijing Chaoyang Hospital, Capital Medical University. All the patients provided written informed consent before study entry. We have registered on the clinical registration website, ChiCTR2300073962. Our study complies with the Declaration of Helsinki. Flowchart of the study was shown in Figure 1.
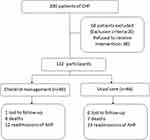 |
Figure 1 Patient Flow Chart. |
CHF Checklist Management
A CHF checklist was shown in Figure 2. CHF checklist management programs included appropriate medication use, relevant health education, complications therapy, and standardized treatment: (1) Health education: conduct health education on knowledge related to CHF for patients and their families during treatment and management, teach patients and their families to measure blood pressure, pulse and body quality, urge patients to control risk factors and change adverse lifestyle. Patients should maintain a balanced or slightly negative daily intake. Educate patients on self-management, including guidance on how to detect and respond to heart failure symptoms as early as possible; (2) Complications therapy: including the management of hypertension, diabetes mellitus (DM), coronary heart disease (CHD) and other complications. Blood pressure was controlled at <130/80mmHg (1mmHg = 0.133kPa) to reach the standard. Blood glucose: fasting blood glucose (FBG) 3.9~7.2mmol/L, HbA1c <7%. Blood lipid: Total cholesterol (TC) and low density lipoprotein cholesterol (LDL-C) were determined according to risk stratification; and11 (3) Standardized treatment: guide patients to take ACE inhibitors (ACEI)/ARB/ARNI, β-blockers, aldosterone receptor antagonists and other heart failure guidelines to recommend medication, including detailed explanation of medication list, drug name, dosage, time, frequency, purpose of medication, adverse reactions, precautions to improve patients’ medication compliance.
 |
Figure 2 Chronic heart failure discharge checklist. |
Follow-Up Arrangements
CHF checklist managements group: telephone or outpatient follow-up was conducted for patients once a month, including patients’ basic condition after discharge, complication control, medication compliance through comprehensive management. In addition to general follow-up, routine blood tests, blood biochemical tests (including blood glucose, LDL-C, liver function, renal function, electrolytes), brain natriuretic peptide (BNP), electrocardiogram, and echocardiography were performed for patients with NYHA cardiac function grade III-IV or patients with disease changes. Chest X - ray, dynamic electrocardiogram and other examinations were performed when necessary. Usual care group: telephone or outpatient follow-up was conducted for patients once a month with identical team of general practitioners. Mortality and re-hospitalization rate were compared between the managed and unmanaged groups.
Study Assessments
All patients were evaluated at the heart center in Beijing chaoyang hospital of capital medical university at baseline and 18-month intervals thereafter. The assessments included: fasting blood NT-pro BNP levels, echocardiography, CHF standardized drug use rates. Mortality and heart failure readmission rates (readmissions from the beginning of the program to follow-up/total number of participants in each group ×100%) were recorded.
Statistical Analysis
If variables conforming to normal distribution, differences of continuous variables between groups were performed by independent sample t-test or Mann–Whitney U-test. Differences of categorical variables were analyzed by χ2 test. If variables of non-normal distribution, the rank sum test was used for comparison. Logistic regression was performed to assess the relation between failure checklist management and re-hospitalization rate. The odds ratios (OR) with 95% confidence intervals (CI) were presented. P < 0.05 was considered statistically significant. SPSS 19.0 software was used for statistical analysis.
Results
Characteristics of the Study Population
A total of 132 patients diagnosed with CHF with moderate-to-severe CHF were included in our study. The characteristics of patients in our study were shown in Table 1. There were no significant differences in gender, age, blood pressure, heart rate, hemoglobin (Hb), NT-proBNP, glycosylated hemoglobin, serum creatinine (SCr), aspartate aminotransferase (AST), Alanine aminotransferase (ALT), NYHA class, LVEF, use of angiotensin converting enzyme inhibitors (ACEI) / angiotensin II receptor antagonist (ARB), beta-blockers, aldosterone receptor antagonists between two groups in admission. One hundred and twenty-five patients were finished follow up. There were 65 cases in management group and 60 cases in usual care group.
 |
Table 1 Clinical Parameters at Baseline of the Study Population |
Overall Mortality and Re-Hospitalization Rate of HF
There was no significant difference in overall mortality rate between management group and control group during 18 months (12.3% [8/65] vs. 11.7% [7/60], χ2 = 0.012, P = 0. 912). The heart failure re-hospitalization rate was significantly lower among patients in management group (18.5% [12/65]) compared to those in control group (38.3% [23/60]) after 18 months of follow-up (Table 2). There was no significant difference in coronary events (6.2% [4/65] vs. 6% [10/60]) and arrhythmias (4.6% [3/65] vs. 3.3% [2/60]) between two groups.
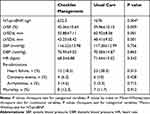 |
Table 2 Re-Admissions, Mortality, NT-proBNP and Echocardiography After follow-Up |
Kaplan–Meier Survival Curves for heart failure re-hospitalization showed heart failure re-hospitalization rate was significantly lower in the checklist management group than control group (Log rank test; p = 0.045) (Figure 3).
Study Assessments
As shown in Table 2, median NT-proBNP level (632.3 ng/l vs. 1678 ng/l, p = 0.004) was lower in management group than that in usual care group. Cardiac ultrasonography was performed 18 months between the management and usual care group. LVEDD (55.88±7.10 mm vs. 60.92±8.06 mm) and LVESD (43.25±8.42mm vs. 48.41± 9.02mm) were decreased (P<0.01). LVEF was increased (45.36±10.64% vs. 39.96 ±10.15%, P<0.01).
HF Medication Use
The utilization rate of standardized medications were higher in management group than that in usual care group (ACEI/ARB/ARNI: 73.8% vs. 61.7%, P<0.05; β-blocker: 72.3% vs. 63.3%, P<0.05). However, there was no significant difference in the utilization rate of spironolactone between the two groups (spironolactone: 69.2% vs. 65%, P>0.05), (Table 3). Although There were significant difference in the utilization rate of standardized medications, systolic blood pressure (116.22±13.98 vs. 117.28±12.99, p = 0.756), diastolic blood pressure (70.95±9.02 vs. 70.58±14.87, p = 0.865) and heart rate (68.5±6.88 vs. 71.64±15.02, p = 0.343) were no significant difference between two groups, (Table 2).
 |
Table 3 Standardized Medications Taken During Follow-Up |
Discussion
CHF is the severe and terminal stage of various cardiovascular diseases, mortality remains high, especially in patients with HFrEF. Standardized treatment and management of high-risk groups and patients with CHF can delay the occurrence of heart failure and the deterioration of heart function, significantly improve their exercise endurance and quality of life, reduce rehospitalization of heart failure and mortality rate.12
The guidelines recommend the management of CHF after discharge should be strengthened, due to the varying levels of expertise of general practitioners and cardiologists.13 The use of heart failure checklist is conducive to the establishment of heart failure management team. We can strengthen the contact and cooperation between different doctors, through the list of supervision and tips, which is convenient and coherent.
Cardiac Function Assessment
Our results show that NT-proBNP, cardiac function classification, LVEF, LVEDD and LVESD in the management group were better than the control group after 18 months of follow-up, indicating that long-term systematic management can improve the heart function of patients, improve the quality of life.
Previous research reported the use of a HF management programmes (HFMP) was found to have beneficial effects in terms of reducing the number of healthcare contacts and hospital admissions, and improving cardiac function in patients with systolic HF.10
First of the reason, the management group focused on guiding patients to adjust drug dosage according to heart rate and blood pressure, adhere to long-term standardized use of targeted doses of the RAS inhibitors /ARNI and β-blockers, as well as aldosterone receptor antagonists to improve medication compliance, significantly enhance therapeutic effect, reverse ventricular remodeling, and thus better improve cardiac function.13 Secondly, the continuous management of patients in the management group in this study can increase patients’ compliance and establish a good doctor-patient relationship, thus improving symptoms and cardiac function.
Heart Failure Readmission and Mortality
Our trail showed that CHF management by general practitioners or cardiologists with checklist can reduce re-admission rate. As we noted in the methods, patients in control group were treated by routine outpatient management without checklist at hospital or community clinic of their choice.
After discharge, readmission is common in patients with heart failure (HF), with a rate ranging from 15% at 30 days, to 50% at 6 months and is associated with significant medico-economic impact and poor prognosis. Most of the readmissions occurring in the post-discharge period could be avoided.11
The earlier OPTIMIZE-HF study enrolled 259 hospitals and 48,612 patients with CHF in the United States. This study showed the use of heart failure assessment tools can improve quality of life, reduce readmission rates,14 our study show similar results. Some other studies reported that CHF management programs were effective in decrease of re-admissions and mortality for heart failure.15,16 However, there were some studies that HF management programs failed to improve clinical outcomes in acute heart failure patients.5,6 Differences in results may be due to different study subjects and the length of follow-up.
The results of our study showed that the 18-month re-hospitalization rate was 15.4% in the management group and 36.7% in the control group. The results indicate that the application of the heart failure checklist can reduce the rate of heart failure re-hospitalization in the management group. But there was no significant difference in overall mortality rate between management group and control group during 18 months.
Most preventable causes for hospitalization can be reduced through appropriate medication up-titration and effective discharge instructions.10 We suggested that CHF management by checklist may be an efficient way to instruct patients.
ACEI/ARB/ARNI, beta-blockers and aldosterone receptor antagonists were frequently under dosed in CHF patients. The management by checklist can direct to adjust the drug dosage to the target dose of ACEI/ARB/ARNI, beta-blockers and aldosterone receptor antagonists more earlierly. Appropriate medication up-titration of those cornerstone drugs may improve ventricular remodeling and cardiac function.17,18
Self-care behaviors can reduce re-hospitalization rate of heart failure and improve the quality of life.19 The checklist management may instruct patients to know how to manage themselves. Researchers urged patients to improve their lifestyle, helped patients identify risk factors for heart failure. We believed that our CHF management using a more comprehensive intervention resulted in less adverse events in medium and long term.
This simple tool for heart failure management may be more simplified and practical, easy to promote, and can also be combined with the Internet model of chronic disease management in the future.
Heart Failure Medication Compliance
It has been demonstrated that the administration of HF therapies, including β-blockers and RAS inhibitors, is associated with better survival of HF patients with a low LVEF.20
According to the comparison between the two groups after management in this study, the utilization rate of ACEI/ARB/ARNI, β-blocker were high in management group.
Studies show that CHF patients often complicated with a variety of chronic diseases, patients with CHF did not take the standardized treatment or taking insufficient doses.21
Other clinical studies have shown that community management of patients with CHF can improve the rate of standardized drug use for CHF. And more importantly, upward titration of ACE inhibitor, ARNI, and β-blocker therapies after discharge leads to reduced hospital re-admission rates and improved functional capacity and quality of life.10
Limitation
This study had some limitations: This was a single-center research. The sample size was small which may lead to inaccurate results. Effect evaluation was relatively simple. There was no significant difference in mortality after discharge between two groups, which may be related to small sample size. This is open-label randomized trial, thus contamination of intervention may be possible. More large-scale clinical randomized controlled trials are needed to perform.
Conclusion
First, checklist management of heart failure can make the management items clear, organized and facilitate the communication between general practitioners and cardiologists. Second, it will strengthen the patient’s own management consciousness
In summary, heart failure checklist management by cardiologists and general practitioners can significantly reduce the re-hospitalization and improve cardiac function. Management through heart failure checklist may improve prognosis in patients with CHF in medium and long term.
Data Sharing Statement
The datasets generated and analyzed are not publicly available because of the policies of the Beijing Chaoyang Hospital regarding individual confidentiality; however, they are available from the corresponding author upon reasonable request. If necessary, some data results can be made public on the website of the clinical study registry.
Ethics and Consent Statements
The study protocol was approved by the Ethics Committee of Capital Medical University Beijing Chao-Yang Hospital, Beijing, China. All participants provided written informed consent prior to admission into the study. The clinical trial registration was not a requirement at the time the study was conducted, we have retrospectively register our clinical trial to the Chinese Clinical Trial Registry.
Acknowledgments
We are grateful to all patients who participated in the study. We also thank Prof. Chang-Lin Lu for advice and assistance.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1:4–25. doi:10.1002/ehf2.12005
2. Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China hypertension survey, 2012–2015. Eur J Heart Fail. 2019;21:1329–1337. doi:10.1002/ejhf.1629
3. Frederick SR, Wai C, Ly H, et al. Using a discharge readiness checklist to reduce heart failure readmissions. Heart Lung. 2016;45:378–379. doi:10.1016/j.hrtlng.2016.05.020
4. Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160:774–784. doi:10.7326/M14-0083
5. Legallois D, Chaufourier L, Blanchart K, et al. Improving quality of care in patients with decompensated acute heart failure using a discharge checklist. Arch Cardiovasc Dis. 2019;112:494–501. doi:10.1016/j.acvd.2019.05.003
6. Allain F, Loizeau V, Chaufourier L, et al. Usefulness of a personalized algorithm-based discharge checklist in patients hospitalized for acute heart failure. ESC Heart Fail. 2020;7:1217–1223. doi:10.1002/ehf2.12604
7. Kalter-Leibovici O, Freimark D, Freedman LS, et al. Disease management in the treatment of patients with chronic heart failure who have universal access to health care: a randomized controlled trial. BMC Med. 2017;15:90. doi:10.1186/s12916-017-0855-z
8. Wahbi-Izzettin O, Hopper I, Ritchie E, Nagalingam V, Aung AK. United we stand, divided we conquer: pilot study of multidisciplinary general medicine heart failure care program. Intern Med J. 2018;48:178–183. doi:10.1111/imj.13647
9. McDonagh TA, Metra M, Adamo M, et al; ESC Scientific Document Group. 2023 focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023;44:3627–3639. doi:10.1093/eurheartj/ehad195
10. Agvall B, Alehagen U, Dahlström U. The benefits of using a heart failure management programme in Swedish primary healthcare. Eur J Heart Fail. 2013;15:228–236. doi:10.1093/eurjhf/hfs159
11. Desai AS. Intensive management to reduce hospitalizations in patients with heart failure. Circulation. 2016;133(17):1704–1707. doi:10.1161/CIRCULATIONAHA.115.017594
12. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi:10.1002/ejhf.592
13. McDonagh TA, Metra M, Adamo M, et al; Authors/Task Force Members; ESC Scientific Document Group. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24:4–131. doi:10.1002/ejhf.2333
14. Fonarow GC, Abraham WT, Albert NM, et al. Influence of a performance-improvement initiative on quality of care for patients hospitalized with heart failure: results of the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF). Arch Intern Med. 2007;167:1493–1502. doi:10.1001/archinte.167.14.1493
15. Marano PJ, Steverson AB, Chen C, et al. Effect of a novel, evidence-based, standardized discharge checklist on 30-day all-cause readmissions in patients hospitalized for heart failure in an urban safety net hospital. Am J Cardiol. 2022;182:40–45. doi:10.1016/j.amjcard.2022.06.058
16. Cañon-Montañez W, Duque-Cartagena T, Rodríguez-Acelas AL. Effect of educational interventions to reduce readmissions due to heart failure decompensation in adults: a systematic review and meta-analysis. Invest Educ Enferm. 2021;39:e05. doi:10.17533/udea.iee.v39n2e05
17. Di Lenarda A, Di Tano G, Cipriani M, et al. ANMCO position paper: double, triple or quadruple therapy for heart failure with reduced ejection fraction. Current evidence and new strategies. G Ital Cardiol. 2021;22:861–868.
18. Masarone D, Martucci ML, Errigo V, Pacileo G. The use of β-blockers in heart failure with reduced ejection fraction. J Cardiovasc Dev Dis. 2021;8. doi:10.3390/jcdd8090101
19. Uchmanowicz I, Jankowska-Polańska B, Mazur G, Sivarajan Froelicher E. Cognitive deficits and self-care behaviors in elderly adults with heart failure. Clin Interv Aging. 2017;12:1565–1572. doi:10.2147/CIA.S140309
20. Gayat E, Arrigo M, Littnerova S, et al. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur J Heart Fail. 2017;20:345–354.1. doi:10.1002/ejhf.932
21. DeVore AD, Granger BB, Fonarow GC, et al. Effect of a hospital and postdischarge quality improvement intervention on clinical outcomes and quality of care for patients with heart failure with reduced ejection fraction: the CONNECT-HF randomized clinical trial. JAMA. 2021;326:314–323. doi:10.1001/jama.2021.8844
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.