Back to Journals » International Journal of Women's Health » Volume 14
Effectiveness of Breathing Exercises, Foot Reflexology and Massage (BRM) on Maternal and Newborn Outcomes Among Primigravidae in Saudi Arabia: A Randomized Controlled Trial
Authors Baljon K , Romli MH, Ismail AH , Khuan L, Chew BH
Received 20 November 2021
Accepted for publication 8 February 2022
Published 25 February 2022 Volume 2022:14 Pages 279—295
DOI https://doi.org/10.2147/IJWH.S347971
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Marleen van Gelder
Kamilya Baljon,1,2 Muhammad Hibatullah Romli,3 Adibah Hanim Ismail,1 Lee Khuan,4 Boon-How Chew1,5
1Department of Family Medicine, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Serdang, 43400, Selangor, Malaysia; 2Department of Nursing, Nursing College, Umm, Al-Qura University, Makkah, Saudi Arabia; 3Department of Rehabilitation Medicine, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Serdang, 43400, Selangor, Malaysia; 4Department of Nursing, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, 43400, Malaysia; 5Clinical Research Unit, Hospital Pengajar Universiti Putra Malaysia (HPUPM Teaching Hospital), Serdang, 43400, Selangor, Malaysia
Correspondence: Boon-How Chew, Department of Family Medicine, Faculty of Medicine and Health Sciences, University Putra Malaysia, Serdang, 43400, Selangor, Malaysia, Tel +60 3-89472520, Fax +60 3-89472328, Email [email protected]; [email protected]
Background: Labor pain and anxiety are important concerns during labor, especially among the primigravidae. It may increase the duration of labor, increase stress hormones, and affect maternal and new-born related outcomes. This study examined the effectiveness of combined breathing exercises, foot reflexology, and massage (BRM) interventions on labor pain, anxiety, labor duration, stress hormone levels, maternal satisfaction, maternal vital signs, and the new-born’s APGAR scores.
Participants and Methods: This single-blind-parallel randomized controlled trial (RCT) was conducted at the Maternity and Children Hospital (MCH), Makkah, Saudi Arabia, by recruiting primigravidae aged 20 to 35 years, without any medical complications, and who were block-randomized at six-centimeter cervical dilation and stratified by intramuscular pethidine. The intervention is BRM compared to standard care. The labor pain was measured via present behavioral intensity (PBI) and visual analogue scale (VAS), and the anxiety was measured via Anxiety Assessment Scale for Pregnant Women in Labor (AASPWL). The secondary outcomes were duration of labor, maternal stress hormone levels, maternal vital signs, maternal satisfaction, fetal heart rate, and APGAR scores. All outcomes were measured at multiple time-points during and after contraction at baseline, during BRM intervention, at 60, 120, and 180 minutes post-intervention. Generalized linear mixed models were used to estimate the intervention effects over time.
Results: A total of 225 participants were randomized for the control (n = 112) and intervention group (113). BRM lowered the labor pain intensity at 60 minutes after intervention during (1.3 vs 3.5, F = 102.5, p < 0.001) and after contraction (0.4 vs 2.4, F = 63.6, p < 0.001) and also lowered anxiety (2.9 vs 4.2, F = 80.4, p < 0.001). BRM correspondingly lowered adrenocorticotropic (ACTH) (133 vs 209 pg/mL, p < 0.001), cortisol (1231 vs 1360 nmol/mL, p = 0.003), and oxytocin (159 vs 121 pg/mL, p < 0.001). It also shortened the labor duration (165 vs 333 minutes, p < 0.001), improved vital signs, which resulted in higher APGAR scores, and increased maternal satisfaction.
Conclusion: The labor unit management could consider adopting BRM as one of the non-pharmacological analgesia for healthy women in labor.
Trial Registration: ISRCTN87414969, registered 3 May 2019.
Keywords: breathing exercises, reflexology, massage, primigravidae, labor pain
Introduction
Labor is a normal physiological process.1 Labor pain is an individual experience and one of the most severe pains that a woman may experience during her life, which could be affected by different physiological, psychological, emotional, and environmental factors.2 Labor pain and anxiety are the chief problems of concerns, especially among the primigravida, which may increase the duration of labor, increase stress hormones, and affect maternal and new-born outcomes.3–5
Fear and anxiety are the negative consequences of labor pain that have prompted many women to refuse normal vaginal delivery.6 Intense pain, fear, anxiety, and prolonged labor increase the risk of assisted delivery and the maternal willingness to perform a cesarean delivery without medical indication.7 These have adverse consequences for mothers, such as hemorrhage, anesthetic complications, and wound infection. For neonates, such as transient tachypnea and depressed APGAR scores.5,8
A satisfactory labor process could be achieved by reducing the pain and anxiety during labor, which further helps in establishing a good relationship between the mother and her baby, and rendering positive maternal and new-born outcomes.9
Labor pain management using a pharmacological approach is common in mainstream medical practice. Pharmacological labor pain management includes opioids, narcotics, epidural analgesia, para-cervical block, spinal block, pudendal block, and nitrous oxide,10 which are widely used for labor analgesia. Among these, pethidine injection is the most commonly used opioid worldwide as it could be easily administered by the midwives, and it also provides significant pain relief.11 However, the majority of the pharmacological agents for labor pain are expensive and have certain adverse effects for mothers, such as hypotension, prolonging the second-stage of labor, and increase risk of assisted delivery. For new-borns, such as increased fetal hypoxia, fetal distress, and difficulty in lactation.11–13
Use of non-pharmacological approaches in managing labor pain is gaining popularity contemporarily. Examples of non-pharmacological therapies to relieve labor pain are water immersion, transcutaneous-electrical nerve stimulation, application of hot and cold pack, acupressure, reflexology, massage, guided imagery, relaxation, breathing exercises, aromatherapy, music therapy, positioning, physiotherapy, and hydrotherapy.10,14,15 Non-pharmaceutical methods of labor pain management are generally cost-effective, safe, and non-invasive. Which encourages women’s participation in their labor process, and helps increase their control over the childbearing experience.14,16 The use of non-pharmacological methods is gaining popularity contemporarily where around (56.5%) of women opted for non-pharmacological methods for pain management in a study conducted in Saudi Arabia.14
Several studies have reported the effectiveness of lower-back massage, hot and cold massage, breathing exercises, and water immersion for labor pain management as well as for shortening the duration of labor. An increase in maternal satisfaction with the labor process and normal APGAR scores was recorded as well.17–20 However, there is a lack of application of these non-pharmacological methods in the modern-day labor units reported in Saudi Arabia. There is also a lack of studies for those that use a combination of multiple non-pharmacological methods like breathing exercises, foot reflexology, and massage (BRM), especially for pregnant women in labor pain.
BRM could contribute a moderate enhancement to the therapeutic touch and conversation in the existing midwifery care in the labor room.21,22 Therapeutic touch is a form of complementary and alternative therapy which believes that energy can be channelled from the therapist to the client for healing purposes. In addition, therapeutic touch does not involve tissue manipulation, such as in a massage. It happens just by placing the hand onto the desired body location. Moreover, therapeutic touch helps by enhancing wellness and energy fields, and stimulates the patient’s natural healing abilities.23,24
The combination of BRM that was used in RCT would increase the acceptability of this therapy by health-care providers in the clinical units as the produced evidence would be of higher quality. BRM is a potential technique that can be used to influence the physiological and psychological factors that affect labor pain and anxiety.25,26 Touch and support during massage and reflexology improve the psychological status, and is highly appreciated by numerous Arab pregnant women.
There are several theories that support the mechanisms of BRM on pain and labor outcomes which we have elaborated in the protocol study.27 Briefly stating, the physiological mechanisms of deep-breathing exercises stimulate the parasympathetic nervous system which improves blood circulation, releases endorphin, and decreases the heart rate. It also helps pregnant women to focus on their breathing instead of their uterine contractions, thus helping them to keep calm.12,25
The mechanical action of reflexology and massage are based on energy theory postulating that an alternating pressure on the reflex points of the feet also stimulate the parasympathetic nervous system that bring about the same effects mentioned above.12,28 Additionally, serotonin, endorphin, and enkephalin hormones are released that help to reduce labor pain, and suppress the release of stress hormones, such as the cortisol, epinephrine, and norepinephrine hormones.26
Touching and pressing during a massage could stimulate the afferent impulses that block pain transmission that are based on the neuro-matrix pain theory.18,25 Skin-to-skin contact increases energy fluctuation between the pregnant woman and the therapist, and encourages the homeostatic balance posited by the sympathetic resonance theory,29 whereas the cutaneous mechanoreceptors theory decreases the receptors’ responsiveness to pain which increases the production of endorphin, and reduces adrenaline and noradrenaline.18,30
Labor pain and anxiety have negative consequences for both pregnant women and fetus outcomes.4,5 For pregnant women, the consequences are prolonged labor, an increased rate of cesarean sections,4–6 and stress hormone levels, as well as a decrease in the release of oxytocin hormone,4 along with increased fetal distress.31,32 Many studies have reported that pharmacological methods reduce labor pain and anxiety.17–33 Several studies have also reported side-effects for mothers, such as hypotension, prolonged second-stage of labor, and increased risk of assisted delivery. As well as their new-borns, such as decreased blood flow to the placenta, fetal-hypoxia, and difficulty in lactation for new-borns.13
In spite of many women opting for non-pharmacological methods34 for pain management, the evidence for them on labor pain management is still controversial.35 To the best of our knowledge, no study has been conducted previously using the combination of non-pharmacological therapies, such as BRM on labor pain and anxiety, and also assessing its effect on maternal and new-born outcomes during the first stage of labor.36,37
Accordingly, this study aimed to investigate the effectiveness of BRM intervention over standard care on managing labor pain, anxiety and maternal-related outcomes among primigravidae in active labor in Saudi Arabia.
Materials and Methods
This is a single-blind-parallel clinical trial block-randomized and stratified by intramuscular pethidine at six-centimeter cervical dilation which was conducted at the labor unit in Maternity and Children Hospital, Makkah, Saudi Arabia, from May to October 2019. A detailed description of the methodology has been published elsewhere.27
Study Participants
The eligible participants were primigravidae, aged 20–35 years, between the 37th to 41st week of gestation at recruitment, which had regular follow-ups at the antennal clinic, and had regular contractions38,39 (≥3 contractions per 10 minutes) where each contraction lasted for 40–55 seconds40,41 with cervical dilation at six-centimeter in the first stage of labor.
Sample Size
The required sample was determined with the independent t-test using G* power software free42 with an estimated effect size of 0.65 as the reduction in anxiety scores measured via the Spielberger State-trait Anxiety Inventory in the intervention group was compared to the control group.18,43–45 The total number was 184 with 92 in each group after an adjustment of (20%) for those who gave no response and/or dropped out. However, the sample size was further inflated when the primigravidae encountered, in the early recruitment, and expressed a high preference for pain relief, and thus a higher attrition rate was anticipated, and an increased possibility of participants that can turn into a cesarean section delivery was noted.
Recruitment
This was conducted at the antenatal clinic for five days a week for a period of six weeks. The recruitment preceded an educational session to draw the attention of the pregnant women and to explain both pharmacological and non-pharmacological types of labor pain management, and their effects on women and new-borns. We also invited participation in our research by explaining about the nature, the process, and the procedures of the research intervention. The eligible and consented participants had their follow-up card stamped. After their admission to the hospital’s labor unit, the eligibility of the participants and consent was reconfirmed. The participants’ confidentiality was maintained throughout the study.
Research Team Members Training
The principal investigator is a certified complementary therapist27 who designed and trained all research assistants (research coordinators, massage therapists, and outcome assessors) until they were found competent for their tasks in a pilot study. The research coordinators were to educate the pregnant women, explain the study, and obtain consent from the potential participants. The research coordinators were also made to reconfirm the eligible participants and organize the intervention sequence at the labor unit. The massage therapists were trained to perform the breathing exercises, foot reflexology, and Swedish and Malay massage techniques. The outcome assessors were trained in applying the questionnaire and in measuring the outcomes.
Randomization
In this study, stratified block-randomization (https://www.sealedenvelope.com/ simple-randomizer/v1/) was used by the principal investigator to achieve comparability of the intramuscular pethidine given by six-centimeter of cervical dilation.27
Allocation Concealment
After the eligibility of the participants who were admitted to the labor unit was reconfirmed, the allocation was done when the women achieved cervical dilation of six-centimeter. The sequence of allocation was maintained throughout the study until the estimated sample size was achieved. The research coordinators also organized and sent the massage therapists to all the participants’ labor room, and the timing to enter was set for the outcome assessors. It was arranged that every participant’s labor room was equipped with the BRM materials and was accompanied by a massage therapist. The massage therapist would stop the massage when the research coordinator’s timer rings, after which they would have to notify the outcome assessor to enter the labor room. This was maintained until all evaluations were completed and the new-born was delivered. All women in the intervention and control groups received routine midwifery care in the labor room.27
Study Intervention
The BRM intervention consists of five-minute breathing exercises, ten-minutes of foot reflexology per foot, and 35-minutes of leg-back massage on top of the standard labor care. The BRM technique applied breathing exercises which are deeply and rhythmically inhaled through the nose and slowly exhaled through the mouth during contractions. Foot reflexology applies direct pressure on specific areas of the foot. The massage techniques utilized a combination of Swedish and Malay traditional massages with five classical movements: effleurage, percussion, petrissage, friction, and vibration. The Swedish effleurage massage was applied on the legs, and the Malay traditional massage was applied on the lower and upper back. These were delivered by the principal investigator and trained research assistants.27
The control group received the standard midwifery care according to the hospital policy, which includes routine blood tests, setting up intravenous access, monitoring the mother’s vital signs, cervical dilation, uterine contractions, fetal heart rate, and charting the progress of labor on a partogram. The midwives provided routine labor pain management with physical support encouragement for mobilization, posture adoption, confirming up-right and side-lying positions, emotional support, such as positive talking, reassurance, and spiritual suggestion.46 Intramuscular pethidine was given before six-centimeter but is not allowed after.11,12,31
Study Outcomes
The labor pain and anxiety were the primary outcomes, while maternal stress hormones, vital signs, fetal heart rate, duration of labor, maternal satisfaction, and APGAR scores were the secondary outcomes.
Primary Outcome
The labor pain intensity was measured using Present Behavioral Intensity (PBI) scale and Visual Analogue Scale (VAS). PBI is a 5-point Likert scale that assesses the behavioral manifestations of pain by observing the patterns of respiration: normal respiration scores 0, the frequency changes of respiration during contractions score 1, gasping reactions that cease during contraction-relaxation scores 2, gasping that persists between contractions scores 3, and signs of agitation score 4. The PBI scores range from 0 (no pain) to 4 (most severe pain).47,48 The VAS scores range from 1 (no pain) to 6 (most severe pain).49,50 This assessment process was explained by the outcome assessors and research coordinator to all the primigravidae participants upon their admission to the labor unit before the commencement of the study. The pain intensity is measured by the PBI and VAS scales were assessed during and after contractions for six times: before intervention, then at 25 and 45 minutes during the intervention, then immediately after intervention, and at 120 minutes and 180 minutes after the intervention.27 The same times were used to assess the outcomes in the control group (Figure 1).
AASPWL was used to assess the anxiety level of women in labor. It has two sub-dimensions: The Birth Process Anxiety (BP - Anxiety) has six questions, and the Motherhood Constellation Anxiety (MC – Anxiety) has three questions. BP-Anxiety assesses the mother’s anxiety related to the birth process and MC-Anxiety assesses the mother’s feelings and concerns about the baby and its growth.51 Every question has an option in a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The total score ranges from 9 to 45, where higher scores indicate a higher level of anxiety. AASPWL has a content-validity index scale more than (0.80), and Kendall’s W between the opinions of the experts (W = 0.09; p = 0.08) with Cronbach’s alpha level of (0.77), significantly correlated (r = 0.36) with the Beck Anxiety Scale.51 The anxiety scores were evaluated four times in the trial: before intervention, then immediately after intervention, and at 120 minutes and 180 minutes after the intervention.27 (Figure 1).
Secondary Outcomes
The stress hormones ACTH, cortisol, and oxytocin levels were taken pre-intervention at baseline six-centimeter cervical dilation, and after intervention. The maternal vital signs were recorded from the maternal monitoring chart and the fetal heart rate was recorded from the cardiotocography, during pre-intervention at baseline, and also immediately after intervention. The duration of labor was obtained from the partogram in minutes. The maternal satisfaction regarding the labor and delivery was measured with the Six Simple Questions for Maternal Satisfaction Questionnaire, which has six items, and each item has a 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree). Higher total scores indicate a higher level of satisfaction.52 Its Cronbach alpha was (0.86), and correlated at (r = 0.51) with the Labor and Delivery Satisfaction Scale.53 The APGAR scores were recorded from a maternal medical record. All the secondary outcomes except Six Simple Questions were collected by health-care personnel as part of the standard routine care and the maternal satisfaction was measured by the trained outcome assessors after delivery. Demographic information was collected after the delivery of the new-born and before the participants leave the labor unit for the postnatal ward. This includes age, body mass index, education level, employment status, gestational age, having seen a birth, attended birth preparation classes, attended classes on methods to reduce pain, feeling towards childbirth, cervical dilation at admission, and intramuscular pethidine given (Figure 1).
Data Analyze
The data was entered by a blinded person and checked for accuracy by another person before analysis. A descriptive statistical analysis was reported according to the distribution: the means and standard deviations were reported for normal distribution data. The median and inter-quartile ranges were reported for non-normally distributed data. Categorical variables were reported in frequencies and percentages.
Since many variables (repeated measure) were not normally distributed, the correlation between PBI and VAS was estimated in Spearman correlation coefficient, and the Wilcoxon signed-rank test was used to assess the pairwise comparison across time.
The Mann–Whitney U-test was used to compare the control and intervention groups for ordinal variables and for interval scales. The effect sizes were estimated using SPSS version 25 and intention-to-treat analysis. The p value <0.05 was considered significant. The researcher used Generalized Linear Mixed Models to analyze the effectiveness of the intervention effects of the two groups and repeated the measurements that were non-normally distributed.
The variables that were entered as covariates were confounding factors, such as the sociodemographic variables of education and feeling towards childbirth. These variables were perceived to be different at baseline; the results were adjusted for the two factors.
The statistical assumptions of the non-constant variability of the residuals and correlated-repeated observations were verified. The sequential Bonferroni test was used to assess the effect of the intervention on the outcomes between the groups across time.
Results
A total of 253 pregnant women were eligible and 225 (response rate of 88.9%) agreed to participate, with 113 and 112 in the intervention and control groups, respectively (Figure 2). A total of 19 and 22 participants withdrew from the intervention and control group, respectively, which resulted in a 16.8% attrition rate in the intervention group and a 19.6% attrition rate in the control group (Figure 2). A total of 17 participants (7 in the intervention and 10 in the control) were excluded for having to undergo emergency cesarean section due to fetal and/or maternal distress, prolapsed umbilical cord, and maternal hemorrhage, and 15 (9 in the intervention and 6 in the control) were excluded due to complications during labor that had to be assisted with instrumental delivery, such as non-reassuring fetal status and prolonged second stage of labor. Otherwise, there were no serious adverse events, such as death recorded either in the intervention or control group, or minor complications from the massage, such as discomfort, redness of the skin, or muscle pain observed in the intervention group.
 |
Figure 2 CONSORT flow chart. Note: Adapted from Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010; 7(3):e1000251. Copyright: © 2010 Schulz et al. Creative Commons Attribution License.74 |
The demographics and obstetric characteristics of the study participants are shown in (Table 1). The mean age of the study participants was 26 years in both the intervention and the control groups at (25.9 ± 2.5) in intervention group and (25.9 ± 2.8) in the control group. The mean body mass index, of the study participants was below 30 kg/m2 in both groups. The mean gestational age of the study participants was about 40 weeks at full-term pregnancy when recruited, and slightly more than (40%) of the participants had tertiary education. More than half of the study participants were employed, and had seen the birth process. Most (>70%) of the study participants did not attend any classes on methods to ease pain. However, a majority of the participants from the intervention and control group had a positive feeling towards childbirth (90% vs 70%). Table 2 shows the outcome variables at baseline for both the intervention and control groups that were comparable except in the motherhood constellation-anxiety score and serum cortisol level.
 |
Table 1 Sociodemographic and Obstetric Characteristics of the Study Participants |
 |
Table 2 Comparing Median (Inter-Quartile) Ranges of the Outcome Variables in Intervention and Control Groups at Baseline |
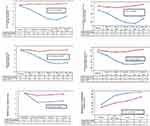
The BRM intervention lowered the scores of the pain (PBI and VAS scores), and anxiety (BP-Anxiety and MC-Anxiety scores) significantly across time during and after contractions (p < 0.001) (Figure 3). However, all contrast estimates of MC-Anxiety were positive, indicating that the scores of MC-Anxiety were significantly higher in the intervention groups. There were no significant changes in the pain and anxiety scores in the control group across time. The PBI and VAS scales correlated well during and after contraction over the six times of measurement where the correlation coefficient ranged from (0.48 to 0.87, p < 0.001). The intervention group reported lower pain scores in PBI and VAS scales compared to the control group (p < 0.001). The intervention group also reported lower anxiety scores in BP-Anxiety scale, but higher in MC-Anxiety scale when compared to the control group. There was a statistically significant difference in the anxiety scores between the intervention and control group (p < 0.001). There were also significant differences observed between the intervention and the control groups in all the secondary outcomes except in the maternal respiration rate (Table 3).
 |
Table 3 Comparison Between Intervention and Control Groups on Secondary Outcomes in Median Ranges at Baseline and After Delivery |
A significant decrease in cortisol and ACTH levels and a rise in oxytocin levels were observed in the intervention groups (Table 3). The maternal pulse rates, blood pressure, fetal heart rate, and duration of labor were significantly lower, and APGAR scores and maternal satisfactions were significantly higher in the intervention group compared to the control group (Table 3).
All variables were measured when the cervical dilation was at least six-centimeter (post-baseline and pre-intervention), and immediately post-intervention, while the APGAR scores, duration of labor, and maternal satisfaction were measured only post-intervention after the first 60 minutes of delivery of the baby. The detailed results of the comparison between pre-intervention and post-intervention in the intervention and control groups on secondary outcomes are shown in (Table 3). All the secondary outcomes showed a significant difference between the intervention and the control group except the maternal respiration rate beats per minute which showed no significant difference.
Discussion
BRM intervention reduced labor pain, improved labor experience, stress hormone levels and neonatal outcomes on top of intramuscular pethidine when compared to standard labor care in a public hospital in Saudi Arabia. This study is novel from the aspect of combining three non-pharmacological therapies’ mechanisms (BRM) into a singular mechanism to achieve reduced labor pain and anxiety, which are one of the most important problems that affect pregnant women during their first stage of labor.
This study recruited relatively healthy primigravidae, aged 20–35 years, between the 37th to the 41st week of gestation age, without medical complications from the antenatal clinics at MCH. The participants were randomized at six-centimeter cervical dilation at the labor unit because there would be no more intramuscular pethidine prescribed beyond this. The randomization strategy was successful and allows the BRM effect to be interpreted disregarding the effect of the analgesia, and ensuring homogeneity of the participants in both groups except in their MC-Anxiety scores, and cortisol levels at baseline. This indicates that the randomization was effective, and the differences were likely due to chance occurrences.
The MCH is the only public sector hospital that provides the obstetric services to the women of Makkah and its surrounding regions, and thus the participants recruited from the hospital should be a good representation of the primigravidae of Makkah. When we compare this study to another study by Azzeh et al54 among the subgroup of primigravidae women attending the antenatal care unit in the Medical Center of Umm Al-Qura University in Makkah City (n = 266), the mean age was (25.2 ± 4.1 years), and the mean body mass index was (24.5 ± 5.0 kg/m2). These were comparable to our study participants. However, being a non-experimental study conducted at a tertiary medical center, their primigravidae were higher educated (71% with a university degree; n = 188) and unemployed (n = 208).54
Generally, the trial recorded higher PBI and VAS scores in the control group compared to the intervention group, while the pain scores decreased significantly across time only in the intervention group. This shows that the breathing exercises, reflexology, and massage when combined and delivered as a package relaxed the primigravidae in labor and reduced pain perceptions. This positive impact on lowering the labor pain has also been observed in earlier studies.43,55–57 Different RCTs utilized massage, acupressure, massage plus acupressure, sacral massage, and Lamaze breathing as interventions and reported significantly lower VAS scores, ranging from (3.57 to 8.83) in the intervention group.43,55–57 Another study reported lower pain scores in the massage group that applied firm and rhythmic back massages PBI scored (1.73 ± 0.45) compared to the control group (2.17 ± 0.59).48 Studies that applied foot reflexology and Swedish massages during labor reported lower pain scores on the McGill Pain Scale in the intervention group.58,59
We used PBI and VAS as two complementary pain measures, and we observed consistent effects of BRM on labor pain but the effect sizes were larger on PBI than the VAS measure. It is evident that although different pain scales were used to measure the labor pain in the different RCTs, the lower pain scores were observed in the intervention group. Such similar findings strengthen the corpus of evidence that non-pharmacological therapies, such as BRM, help in reducing labor pain. This pain alleviation might be because of the apparent mechanism of action of the BRM intervention that stimulates the parasympathetic nervous system resulting in a state of calmness in the body, leading to reduced pain perceptions.27
The trial recorded higher BP-Anxiety scores in the control group compared to the intervention group, while the BP-Anxiety scores decreased significantly across time only in the intervention group. This shows that the anxiety assessed by birth process related questions that describe the pregnant woman’s feelings/emotions, and faintness. Wherein they felt they could possibly hurt themselves or their new-borns, and would feel they are weak or may cry at any time, as was usually experienced by the primigravidae during labor, was effectively reduced. This positive impact in lowering anxiety has also been observed in studies in Iran and Turkey in which foot reflexology was reported to decrease the anxiety on Spielberger State-Trait Anxiety Inventory.44,58
Similarly, other studies that used sacral massage, massage, and the presence of an attendant as an intervention also reported lower anxiety in the intervention group.43,56,60 The same mechanism of action via the stimulation of the parasympathetic nervous system, along with the release of endorphin, encephalin, and enkephalin, cumulatively decreases the heart rate and the release of stress hormones, and correspondingly increases feelings of calmness in the body.27
This study observed a larger effect size on the BP-Anxiety scale; however, the intervention group reported an increase in anxiety scores in the MC-Anxiety scale at all-time intervals. This means that despite the BRM intervention, the anxiety scores concerning the survival and growth of the baby were gradually increasing in the intervention group. It is not directly clear what could be the reason for this observation as these primigravidae were experiencing lower pain, anxiety, and shorter labor durations. This might be due to other unobserved factors that influenced the anxiety levels during the labor, such as socio-personal characters, personality traits, lack of family support, and negative beliefs about the childbirth process,61 or simply because of chance occurrence. This negative impact in the increase in anxiety scores has not been evident in any previous studies, and future studies could be conducted to explore these possible factors and similar interventions that could be modified to address and alleviate this anxiety. Additionally, validation studies for the AASPWL scale in the Saudi population are warranted.
This trial recorded a significant decrease in the levels of stress hormones, cortisol, and ACTH, and an increase in the level of oxytocin in the intervention group. In contrast, cortisol and ACTH hormones increased significantly in the control group. This positive impact in lowering stress hormonal levels has been evident in earlier studies that used massage, reflexology, yoga, and Swedish massage as an intervention.62–65
These observations are consistent with the effects on lowering pain and anxiety perceptions, and the mechanism of actions on the parasympathetic and sympathetic nervous systems. Touch is believed to affect the release of oxytocin and reduce the level of ACTH. Reflexology is known to be able to help in reorganizing and stabilizing the hormonal levels, and allowing the body system to work at its best. This trial included only cortisol, ACTH, and oxytocin levels, but future studies could be conducted by adding some others, such as beta-endorphin, epinephrine, and norepinephrine levels to better understand the effect of intervention across the broad range of hormones.66
This trial also reported improved vital signs including the fetal heart rate and high APGAR scores, shorter duration of labor, and high maternal satisfaction in the intervention group compared to the control group. These positive impacts are reassuring as they were also observed in earlier studies where sacral massage, foot massage, low back massage, reflexology, the presence of attendant, and Quran sound were used as interventions.18,30,60,67–71
In a quasi-experimental study, where Acu-Yoga was used as an intervention, a lower fetal heart rate was observed in the intervention groups.72 The positive impact of high APGAR scores has been evident in the earlier studies that used foot reflexology and massage as an intervention.58,62,73 However, another RCT used massage as an intervention and reported a non-significant difference in APGAR scores between the intervention and control groups.67 These inconsistent effects on the maternal and fetal vital signs might be due to the heterogeneity in the conduct of the studies and the intensity of the interventions. The same mechanism of parasympathetic nervous system activation that reduces resistance in the uterine arteries and facilitates blood flow to the placenta could result in an improved intrauterine fetal heart rate and improved health status of the new-born.72
Strengths and Limitations
This study included both the objective and subjective outcome measures that provided a more complete assessment of the BRM’s effect on the labor experience besides pain. It measured pain and anxiety at multiple times from the baseline at cervical dilation at six-centimeter, and at 25-, 40-, 60-, 120-, and 180-minutes post-intervention to examine the effect of intervention on different time intervals. However, there were limitations to the study which were exposed when clarifying the results. Firstly, the BRM intervention was interrupted by the routine midwifery care, such as the hourly vital signs, vaginal examination, and fetal heart monitoring. This might have caused a loss of effectiveness in the BRM intervention. Second, although the VAS is a common method in measuring the non-labor pain intensity, it is not a reference standard for assessing labor pain. However, it might still be a useful tool in the study participants if they are of the same general ethnic origin and if it was applied consistently over the different labor stages and compared to another pain measure.
Although optimal effort has been made to blind the research coordinators and outcome assessors, these might be compromised due to the nature and setting of the study. However, the impact is minimal as the whole sequence of tasks by all research assistants was pilot tested and was proven to have sufficient blinding on the research coordinators when allocating groups and on the outcome assessors. Furthermore, the principal investigator has conducted several audits to ensure the validity of the intervention flow and secure the collected data. The blinding of the primigravidae mothers was not possible in the study of this nature of the intervention as the performance biases (reactivity, compensatory rivalry and demoralization) in the participants and detection bias in the outcome assessors could not be fully avoided. However, we believe the performance biases were less substantial on the outcomes since labor is an intense process that can overwhelm women and their personal preferences.
Lastly, the study participants were primigravidae and at low risk, and therefore the results may not be generalized to either multigravidae, complicated labor, or in the second, third, and fourth stages of labor. Additionally, the risk of multiple testing and alpha error was possible but unlikely because even if two-sided alpha of (0.0125) were used to test significance for the pain and anxiety (twice; each during and after uterine contraction) to account for the 4 analyses, the observed effects were still significant at the (p < 0.001) (Figure 3).
Conclusion
BRM intervention has shown benefits in labor pain and experience on top of intramuscular pethidine measured by different subjective and objective tools including the maternal and new-born health status. Primigravidae who received BRM intervention during the first stage of labor experienced significantly reduced labor pain, anxiety, and labor duration, and improved maternal outcomes (vital signs, maternal satisfaction, higher oxytocin levels, reduced cortisol and ACTH levels). As well as the new-born outcome (higher APGAR scores at the 1st and 5th minute).
This study supports the effectiveness of BRM as an essential tool to address obstetric, psychological, and new-born outcomes in relatively healthy primigravidae. It provides good evidence for midwifery care to consider BRM as one of the non-pharmacological interventions in the labor unit.
Abbreviations
AASPWL, anxiety assessment scale for pregnant women in labor; ACTH, Adrenocorticotropin; APGAR scores, appearance, pulse, grimace, activity and respiration; BP-Anxiety, birth process anxiety; BRM, breathing exercises, reflexology, and massage; MCH, maternity and children hospital; MC-Anxiety, motherhood constellation anxiety; PBI, present behavioral intensity; RCT, randomized controlled trial; VAS, visual analogue scale.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Ethics Approval and Consent to Participate
This study was conducted under the ethical guidelines of the Declaration of Helsinki. It was approved by Ethical Committee for Research Involving Human Subjects of the Ministry of Health in Saudi Arabia with reference number H-02-K-076-0319-109 and from the Ethics Committee for Research Involving Human Subjects (JKEUPM) Universiti Putra Malaysia with reference number JKEUPM-2019-169 as a requirement for all international student’s research projects. Informed written consent was obtained from participants before participating in the study. Confidentiality of all the study participants’ information was observed and maintained.
Acknowledgments
I would like to express my sincere gratitude to Um-Al-Qura University, Universiti Putra Malaysia, Research Department in the Directorate of Health Affairs, Makkah Region, Saudi Arabia, Ethics Committee for Research Involving Human Subjects (JKEUPM) Universiti Putra Malaysia, and Maternity and Children Hospital in Makkah, Saudi Arabia. I would like to thank Dr. Danaee from Faculty of Medicine, University of Malaya, Malaysia, for assisting in the statistical analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
The authors received no financial support for the research, authorship, or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Aziato L, Acheampong AK, Umoar KL. Labor pain experiences and perceptions: a qualitative study among post-partum women in Ghana. BMC Pregnancy Childbirth. 2017;17:73. doi:10.1186/s12884-017-1248-1
2. Boryri T, Noori NM, Teimouri A, Yaghobinia F. The perception of primiparous mothers of comfortable resources in labor pain (a qualitative study). Iran J Nurs Midwifery Res. 2016;21:239. doi:10.4103/1735-9066.180386
3. Cicek S, Basar F. The effects of breathing techniques training on the duration of labor and anxiety levels of pregnant women. Complement Ther Clin Pract. 2017;29:213–219. doi:10.1016/j.ctcp.2017.10.006
4. Demšar K, Svetina M, Verdenik I, et al. Tokophobia (fear of childbirth): prevalence and risk factors. J Perinat Med. 2018;46:151–154. doi:10.1515/jpm-2016-0282
5. Levy I, Attias S, Lavee TS, et al. The effectiveness of foot reflexology in reducing anxiety and duration of labor in primiparas: an open-label randomized controlled trial. Complement Ther Clin Pract. 2020;38:101085. doi:10.1016/j.ctcp.2019.101085
6. Aksoy M, Aksoy AN, Dostbil A, et al. The relationship between fear of childbirth and women’s knowledge about painless childbirth. Obstet Gynecol Int. 2014;2014:1–7. doi:10.1155/2014/274303
7. Stoll KH, Hauck YL, Downe S, et al. Preference for cesarean section in young nulligravid women in eight OECD countries and implications for reproductive health education. Reprod Health. 2017;14:1–9. doi:10.1186/s12978-017-0354-x
8. Aljohani AA, Al-Jifree HM, Jamjoom RH, Albalawi RS, Alosaimi AM. Common complications of cesarean section during the year 2017 in King Abdulaziz Medical City, Jeddah, Saudi Arabia. Cureus. 2021;13:e12840. doi:10.7759/cureus.12840
9. Wilde-larsson B, Hildingsson I, Angeby K, Sandin-Bojö A-K. Prevalence of prolonged latent phase and labor outcomes: review of birth records in a Swedish population. J Midwifery Womens Health. 2018;63:33–44. doi:10.1111/jmwh.12704
10. Simkin P, Klein M. Nonpharmacological approaches to management of labor pain, parts 1 and 2. UpToDate. 2015;17:1–11.
11. Smith LA, Burns E, Cuthbert A, Mori R, Dowswell T. Parenteral opioids for maternal pain management in labor. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.CD007396.pub2
12. Mathew AM, Francis F. Effectiveness of foot reflexology in reduction of labor pain among mothers in labor admitted at PSG Hospital, Coimbatore. Int J Nurs Educ. 2016;8:11–15. doi:10.5958/0974-9357.2016.00081.7
13. Abd El-Aziz SN, Mansour SES, Hassan NF. Factors associated with fear of childbirth: it’s effect on women’s preference for elective cesarean section. J Nurs Educ Pract. 2017;7:133–146. doi:10.5430/jnep.v7n1p133
14. Almushait M, Ghani RA. Perception toward non-pharmacological strategies in relieving labor pain: an analytical descriptive study. J Nat Sci Res. 2014;4:5–12.
15. Ghiasi A, Bagheri L, Haseli A. A systematic review on the anxiolytic effect of aromatherapy during the first stage of labor. J Caring Sci. 2019;8:51–60. doi:10.15171/jcs.2019.008
16. Kavosi Z, Keshtkaran A, Setoodehzadeh F, et al. A comparison of mothers’ quality of life after normal vaginal, cesarean, and water birth deliveries. Int J Community Based Nurs Midwifery. 2015;3:198–204.
17. Czech I, Fuchs P, Fuchs A, et al. Pharmacological and non-pharmacological methods of labor pain relief—establishment of effectiveness and comparison. Int J Environ Res Public Health. 2018;15:2792. doi:10.3390/ijerph15122792
18. Erdogan SU, Yanikkerem E, Goker A. Effects of low back massage on perceived birth pain and satisfaction. Complement Ther Clin Pract. 2017;28:169–175. doi:10.1016/j.ctcp.2017.05.016
19. Nehbandani S, Koochakzaei M, Keikhaie F, Jahantigh F. Comparison of the effect of hot and cold massage at spleen 6 on pain relief during active labor phase: a clinical trial. Medsurg Nurs J. 2019;8:e97075. doi:10.5812/msnj.97075
20. Yuksel H, Cayir Y, Kosan Z, Tastan K. Effectiveness of breathing exercises during the second stage of labor on labor pain and Medicine. J Integr Med. 2017;15:456–461. doi:10.1016/S2095-4964(17)60368-6
21. Simkin PP, O’hara M. Nonpharmacologic relief of pain during labor: systematic reviews of five methods. Am J Obstet Gynecol. 2002;186:S131–S159. doi:10.1016/S0002-9378(02)70188-9
22. Pinar SE, Demirel G. The effect of therapeutic touch on labor pain, anxiety and childbirth attitude: a randomized controlled trial. Eur J Integr Med. 2021;41:101255. doi:10.1016/j.eujim.2020.101255
23. Turan N. The importance of therapeutic touch in intensive care unit. Acibadem Univ Health Science J. 2015;6:134–139.
24. Cheraghi M, Hosseini A, Gholami R, et al. Therapeutic touch efficacy: a systematic review. Medsurg Nurs J. 2017;5:e67946.
25. Embong NH, Soh YC, Ming LC, Wong TW. Perspectives on reflexology: a qualitative approach. J Tradit Complement Med. 2017;7:327–331. doi:10.1016/j.jtcme.2016.08.008
26. Taheri H, Naseri-Salahshour V, Abedi A, Sajadi M. Comparing the effect of foot and hand reflexology on pain severity after appendectomy: a randomized clinical trial. Iran J Nurs Midwifery Res. 2019;24:451–456. doi:10.4103/ijnmr.IJNMR_85_18
27. Baljon KJ, Romli MH, Ismail AH, et al. Protocol: effectiveness of breathing exercises, foot reflexology and back massage (BRM) on labor pain, anxiety, duration, satisfaction, stress hormones and newborn outcomes among primigravidae during the first stage of labor in Saudi Arabia: a study protocol for a randomised controlled trial. BMJ Open. 2020;10:e033844. doi:10.1136/bmjopen-2019-033844
28. Sripongngam T, Eungpinichpong W. Effects of different duration of traditional Thai massage on parasympathetic nervous system. Int J Geomate. 2016;11:2883–2887. doi:10.21660/2016.28.1343
29. McCullough JEM, Liddle SD, Sinclair M, Close C, Hughes CM. The physiological and biochemical outcomes associated with a reflexology treatment: a systematic review. Evid Based Complement Alternat Med. 2014;2014. doi:10.1155/2014/502123
30. Bolbol-Haghighi N, Masoumi SZ, Kazemi F. Effect of massage therapy on duration of labor: a randomized controlled trial. J Clin Diagn. 2016;10:12–15. doi:10.7860/JCDR/2016/17447.7688
31. Ahmadi Z, Torkzahrani S, Roosta F, Shakeri N, Mhmoodi Z. Effect of breathing technique of blowing on the extent of damage to the perineum at the moment of delivery: a randomized clinical trial. Iran J Nurs Midwifery Res. 2017;(22):62–66. doi:10.4103/1735-9066.202071
32. AlSheeha MA. Epidemiology of cesarean delivery in Qassim, Saudi Arabia. Open Access Maced J Med Sci. 2018;6:891. doi:10.3889/oamjms.2018.213
33. Boateng EA, Kumi LO, Diji AKA. Nurses and midwives’ experiences of using non-pharmacological interventions for labor pain management: a qualitative study in Ghana. BMC Pregnancy Childbirth. 2019;19:168. doi:10.1186/s12884-019-2311-x
34. Thomson G, Feeley C, Moran VH, Downe S, Oladapo OT. Women’s experiences of pharmacological and non-pharmacological pain relief methods for labor and childbirth: a qualitative systematic review. Reprod Health. 2019;16:71. doi:10.1186/s12978-019-0735-4
35. Levett KM, Smith CA, Bensoussan A, Dahlen HG. The complementary therapies for labor and birth study making sense of labor and birth–experiences of women, partners and midwives of a complementary Medicine antenatal education course. Midwifery. 2016;40:124–131. doi:10.1016/j.midw.2016.06.011
36. Mohamed MA, El Bigawy AF. Effect of back massage and relaxation training on the act of labor: a randomized controlled clinical trial. Int J Chemtech Res. 2017;10:243–252.
37. Alrowais NA, Alyousefi NA. The prevalence extent of Complementary and Alternative Medicine (CAM) use among Saudis. Saudi Pharm J. 2017;25:306–318. doi:10.1016/j.jsps.2016.09.009
38. Maeda K. Uterine contractions in normal labor developed by a positive feed-back and oscillation. J Health Med. 2013;4:10–4172. doi:10.4172/2157-7420.1000130
39. Desai JA, Thejavathy GV. Normal labor and vaginal delivery. A practical guide to third trimester of pregnancy & puerperium. 2016.
40. Mola G. Caring for PNG Women and Their Newborns: A Manual for Nurses and Community Health Workers in Papua New Guinea. University of Papua New Guinea Press; 2014.
41. King TL, Brucker MC, Kriebs JM, Fahey JO. Varney’s Midwifery. Jones & Bartlett Publishers; 2013.
42. Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Method. 2007;39:175–191. doi:10.3758/BF03193146
43. Lamadah SM, Nomani I. The effect of aromatherapy massage using lavender oil on the level of pain and anxiety during labor among primigravida women. Am J Nurs Sci. 2016;5:37–44. doi:10.11648/j.ajns.20160502.11
44. Yılar Erkek Z, Aktas S. The effect of foot reflexology on the anxiety levels of women in labor. J Altern Complement Med. 2018;24:352–360. doi:10.1089/acm.2017.0263
45. Sadat HZ, Forugh F, Maryam H, Nosratollah MN, Hosein S. The impact of manual massage on intensity and duration of pain at first phase of labor in primigravid women. Int J Med. 2016;1:16–18.
46. Akhavan S, Edge D. Foreign-born women’s experiences of community-based doulas in Sweden—a qualitative study. Health Care Women Int. 2012;33:833–848. doi:10.1080/07399332.2011.646107
47. Bonnel AM, Boureau F. Labor pain assessment: validity of a behavioral index. Pain. 1985;22:81–90. doi:10.1016/0304-3959(85)90150-2
48. Chang MY, Wang SY, Chen CH. Effects of massage on pain and anxiety during labor: a randomized controlled trial in Taiwan. J Adv Nurs. 2002;38:68–73. doi:10.1046/j.1365-2648.2002.02147.x
49. Bahammam MA, Hassan MH. Validity and reliability of an Arabic version of the modified dental anxiety scale in Saudi adults. Saudi Med J. 2014;35:1384.
50. Taghinejad H, Delpisheh A, Suhrabi Z. Comparison between massage and music therapies to relieve the severity of labor pain. Womens Health. 2010;6:377–381. doi:10.2217/WHE.10.15
51. Durat G, Çulhacik GD, Doğu Ö, et al. The development of an anxiety assessment scale for pregnant women in labor. Saudi Med J. 2018;39:609–614. doi:10.15537/smj.2018.6.22266
52. Harvey S, Rach D, Stainton MC, et al. Evaluation of satisfaction with midwifery care. Midwifery. 2002;18:260–267. doi:10.1054/midw.2002.0317
53. Sawyer A, Ayers S, Abbott J, et al. Measures of satisfaction with care during labor and birth: a comparative review. BMC Pregnancy Childbirth. 2013;13:1–10. doi:10.1186/1471-2393-13-108
54. Azzeh F, Refaat B. Iodine adequacy in reproductive age and pregnant women living in the Western region of Saudi Arabia. BMC Pregnancy Childbirth. 2020;20:1–12. doi:10.1186/s12884-020-03057-w
55. Gönenç IM, Terzioglu F. Effects of massage and acupressure on relieving labor pain, reducing labor time, and increasing delivery satisfaction. J Nurs Res. 2020;28:e68. doi:10.1097/jnr.0000000000000344
56. Akköz Çevik S, Karaduman S. The effect of sacral massage on labor pain and anxiety: a randomized controlled trial. Jpn J Nurs Sci. 2020;17:e12272. doi:10.1111/jjns.12272
57. Jhala A. a study to assess the effectiveness of lamaze breathing on labor pain and anxiety towards labor outcome among primigravida mothers during labor in community health center, Kolar Road, Bhopal (MP). Indian J Obstet Gynecol. 2017;5:19–22. doi:10.21088/ijog.2321.1636.5117.2
58. Hanjani SM, Tourzani ZM, Shoghi M. The effect of foot reflexology on anxiety, pain, and outcomes of the labor in primigravida Women. Acta Med Iran. 2014;53:507–511.
59. Janssen P, Shroff F, Jaspar P. Massage therapy and labor outcomes: a randomized controlled trial. Int J Ther Massage Bodywork. 2012;5:15–20. doi:10.3822/ijtmb.v5i4.164
60. Mortazavi SH, Khaki S, Moradi R, et al. Effects of massage therapy and presence of attendant on pain, anxiety and satisfaction during labor. Arch Gynecol Obstet. 2012;286:19–23. doi:10.1007/s00404-012-2227-4
61. Madhavanprabhakaran GK, D’Souza MS, Nairy KS. Prevalence of pregnancy anxiety and associated factors. Int J Africa Nurs. 2015;3:1–7. doi:10.1016/j.ijans.2015.06.002
62. Hosseini E, Asadi N, Zareei F. Effect of massage therapy on labor progress and plasma levels of cortisol in the active stage of first labor. Zahedan J Res Med Sci. 2013;15:35–38.
63. Polis RL, Gussman D, Kuo YH. Yoga in pregnancy: an examination of maternal and fetal responses to 26 yoga postures. Obstet Gynecol. 2015;126:1237–1241. doi:10.1097/AOG.0000000000001137
64. McCullough JE, Liddle SD, Close C, et al. Reflexology: a randomized controlled trial investigating the effects on beta-endorphin, cortisol and pregnancy related stress. Complement Ther Clin Pract. 2018;31:76–84. doi:10.1016/j.ctcp.2018.01.018
65. Morhenn V, Beavin LE, Zak PJ. Massage increases oxytocin and reduces adrenocorticotropin hormone in humans. Altern Ther Health Med. 2012;18:11–18.
66. Karakaya BK, Moraloglu O, Findik RB, et al. Evaluation of maternal and fetal stress hormones during the process of birth. Obstet Gynaecol Reprod Med. 2018;24:65–70. doi:10.21613/GORM.2017.753
67. Gallo RBS, Santana LS, Ferreira CHJ, et al. Massage reduced severity of pain during labor: a randomized trial. J Physiother. 2013;59:109–116. doi:10.1016/S1836-9553(13)70163-2
68. Vahedian-Azimi A, Ebadi A, Jafarabadi MA, et al. Effect of massage therapy on vital signs and GCS scores of ICU patients: a randomized controlled clinical trial. Trauma Mon. 2014;19(3):e17031. doi:10.5812/traumamon.17031
69. Supa’At I, Zakaria Z, Maskon O, et al. Effects of Swedish massage therapy on blood pressure, heart rate, and inflammatory markers in hypertensive women. Evid Based Complement Alternat Med. 2013;2013:1–8. doi:10.1155/2013/171852
70. Maghfiroh T, Setiani O, Sumarni S, et al. The effect of stimulus cutaneous slow stroke back massage to beta endorphin levels and blood pressure changes among pregnant women with preeclampsia in Demak, Indonesia.
71. Ermiati E, Setyawati A, Emaliyawati E. Foot massage modification to reduce blood pressure in pregnant woman with Preeclampsia. Padjadjaran Nurs J. 2018;6:131–138. doi:10.24198/jkp.v6i2.625
72. Hudzaifah HM, Widyawati MN. The effect of acuyoga on fetal heart among pregnant women with hypertension. J Nurs Healthc Res. 2020;3:573–579. doi:10.35654/ijnhs.v3i1.192
73. Bayrami R, Ebrahimipour H. Effect of the Quran sound on labor pain and other maternal and neonatal factors in nulliparous women. J Res Health. 2014;4:898–902.
74. Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010; 7(3):e1000251.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.