Back to Journals » Journal of Pain Research » Volume 9
Effectiveness of low-dose intravenous ketamine to attenuate stress response in patients undergoing emergency cesarean section with spinal anesthesia
Authors Senapathi T , Widnyana IMG, Wiryana M, Aribawa IGNM , Aryabiantara IW , Hartawan IGAGU, Sinardja IK, Suarjaya IPP, Nada IKW, Jaya AGPS
Received 31 March 2016
Accepted for publication 20 May 2016
Published 20 September 2016 Volume 2016:9 Pages 689—692
DOI https://doi.org/10.2147/JPR.S109616
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Tjokorda Gde Agung Senapathi, I Made Gede Widnyana, Made Wiryana, I Gusti Ngurah Mahaalit Aribawa, I Wayan Aryabiantara, I Gusti Agung Gede Utara Hartawan, I Ketut Sinardja, I Putu Pramana Suarjaya, I Ketut Wibawa Nada, AA Gde Putra Semara Jaya
Department of Anesthesiology and Intensive Care, Faculty of Medicine, Udayana University, Sanglah Hospital, Bali, Indonesia
Purpose: Cesarean section is a surgical procedure. Surgical procedures will induce stress responses, which may have negative impact on postoperative recovery. Ketamine plays a role in the homeostatic regulation of inflammatory response in order to attenuate stress response. We tried to determine the effectiveness of low-dose intravenous ketamine to attenuate stress response in patients undergoing emergency cesarean section with spinal anesthesia.
Patients and methods: Thirty-six pregnant women undergoing emergency cesarean section with spinal anesthesia were randomly divided into two groups (n=18). Ketamine 0.3 mg/kg (KET group) or NaCl 0.9% (NS group) was administered intravenously before the administration of spinal anesthesia. C-reactive protein (CRP) and neutrophil levels were measured preoperatively and postoperatively.
Results: Elevation of CRP stress response was lower in the KET group and significantly different (P≤0.05) from that in the NS group. Neutrophil level was elevated in both the groups and hence not significantly different from each other (P>0.05). Postoperative visual analog scale pain score was not significantly different between the two groups (P>0.05), but there was a statistically significant (P≤0.05) positive and weak correlation between visual analog scale and CRP level postoperatively.
Conclusion: Low-dose intravenous ketamine effectively attenuates the CRP stress response in patients undergoing emergency cesarean section with spinal anesthesia.
Keywords: ketamine, stress response, pain, spinal anesthesia, cesarean section
Introduction
Cesarean section evokes stress response, which is associated with postoperative morbidity. Regional anesthesia can suppress neuroendocrine response but cannot suppress cytokine response.1 Interleukin (IL)-6 is a major cytokine responsible for inducing acute-phase response. One of the acute-phase responses is the production of acute-phase proteins by the liver (eg, C-reactive protein [CRP]).2,3 Elevation of CRP serum level will be affected by IL-6 level. Stress response is also characterized by an increase in the number of neutrophils that will undergo diapedesis to inflammation site through the vascular endothelium.4 In addition to tissue injury, postoperative pain can aggravate stress response.1
Ketamine is the drug of choice for induction of general anesthesia in patients undergoing a cesarean section. Ketamine results in less fetal depression. Ketamine has a rapid onset and short duration of action as well as provides analgesia and hypnosis of better quality. Ketamine is also an option in cases of severe fetal distress.5,9–11
Loix et al in their systematic review concluded that ketamine at a very low dose (0.25 mg/kg) may inhibit exacerbations of inflamation.5 Similarly, Dale et al in a systematic study and meta-analysis concluded that intraoperative ketamine significantly inhibited IL-6 postoperative stress response.6
Through this research, we tried to determine the effectiveness of low-dose intravenous ketamine 0.3 mg/kg in attenuating postoperative stress response, especially in patients undergoing emergency cesarean section.
Materials and methods
Patients
This is an experimental study with a double-blind randomized controlled trial design. A total of 36 pregnant women undergoing emergency cesarean section with spinal anesthesia in the emergency operating room at Sanglah Hospital (Joint Commission International – Accredited) from December 2015 to February 2016 were enrolled in the study (consecutive sampling). Patients were not enrolled in the study if any the following criteria were present: patient refusal, physical status ASA III or more, body mass index before pregnancy less than 18.5 or more than 24.9 kg/m2, hypertension during pregnancy, a history of chronic analgesic use, a history of coronary heart disease and stroke, and contraindications using ketamine or midazolam. The subjects were assigned into two groups by permuted-block randomization. The subject will be issued when such condition occur: bleeding more than 1,000 mL, changes in anesthetic techniques, and discharge against medical advice before 24 hours postoperatively. There is no loss of subject in this study.
Procedures
In the preparation room of emergency operating theater, basal blood pressure and heart rate of the subjects were measured, intravenous access was obtained, blood samples for preoperative CRP and neutrophil were collected, and ringer lactate 10 mL/kg and midazolam 0.03 mg/kg were administered intravenously. In the operating room, the subjects received oxygen supplementation of 2 L/min through a nasal cannula. Three milliliters of ketamine 0.3 mg/kg (KET group) or 0.9% NaCl (NS group) was administered within 30 seconds at the disinfection step of spinal anesthesia. Spinal anesthesia was performed with Quincke type needle G27 using 0.5% hyperbaric bupivacaine 12.5 mg at the rate of 0.2 mL/sec. Pin-prick test was performed to assess the height of the block based on skin dermatome. Apgar scores of newborns were evaluated. Postoperative patients received fentanyl 0.25 µ/kg/h and ketorolac 30 mg every 8 hours intravenously as analgesia. Postoperative CRP, neutrophil, and visual analog scale (VAS) were measured after 24 hours.
Statistical analysis
Data analysis was done using Statistical Package for Social Sciences for Windows (IBM Corporation, Armonk, NY) software version 20. Numerical variables were expressed as mean ± standard or median (minimum–maximum). Test for normality was performed using Shapiro–Wilk test and homogeneity test using Levene’s test. Mean tests were compared using independent t-test if data distribution was normal or using nonparametric Mann–Whitney U test if data were not distributed normally. The level of significance was α=0.05.
Ethics statements
This study was approved by the Research Ethics Committee of Faculty of Medicine, Udayana University, Sanglah Hospital (1852/UN.14.2/Litbang/2015). Written informed consent was obtained from all the subjects.
Results
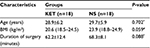
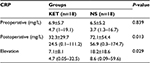
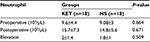
As shown in Table 1, subject characteristics (age, body mass index, and duration of surgery) were not significantly different in the two groups (P>0.05). Table 2 presents the perioperative CRP levels. Preoperative CRP levels were not significantly different in the two groups (P>0.05), with a median of 4.7 mg/L in the KET group and 3.7 mg/L in the NS group. There were significant differences in postoperative CRP levels in both the groups (P≤0.05), with a mean of 32.3±29.7 mg/L in the KET group and 72.1±54.4 mg/L in the NS group. Statistical analysis of the elevation of CRP resulted in median value of 4.7 times in the KET group and 8.6 times in the NS group, with significant difference (P≤0.05). Neutrophil level was not significantly different for preoperative and postoperative levels as well as for the elevation. Table 3 shows a mean preoperative neutrophil level of 9.6±4.4 103/µL in the KET group and 9.08±3 103/µL in the NS group, with P>0.05. The increase in neutrophil level in both the groups did not differ significantly.
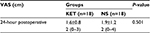
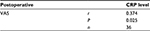
As shown in Table 4, postoperative pain scores did not differ significantly in both the groups (P>0.05). The mean VAS for the KET group was 1.6±0.8 and 1.9±1.2 for the NS group. The maximum VAS value was 3 cm in the KET group and 4 cm in the NS group.
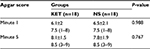
Based on Spearman test between postoperative VAS value and postoperative CRP level (Table 5), there was a weak positive correlation with a correlation coefficient of 0.374, which was statistically significant (P≤0.05). Table 6 presents the Apgar score. Apgar scores of 1 and 5 minutes in both the groups were not significantly different with P>0.05.
Discussion
Surgery or trauma will evoke a stress response. Stress response is a physiological response that arises to protect the body from injury and to survive. There is growing evidence that there is a stress response associated with postoperative morbidity. Neuroendocrine response stimulated by pain stimulus afferent fibers to the central nervous system can be reduced or eliminated through a regional nerve block anesthesia. Cytokine responses that are stimulated by local tissue damage at the site of surgery cannot be inhibited by regional anesthesia.1,8
Cytokine response begins with the release of IL-1 and tumor necrosis factor-α on the activation of macrophages and monocytes from the damaged tissue. This will stimulate the production and release of other cytokines, particularly IL-6 as it is the major cytokine responsible for the systemic change known as the acute-phase response. Acute-phase protein (ie, CRP, fibrinogen, α2-macroglobulin) produced by the liver. This protein acts as mediator of inflammation, anti-proteinase, and scavengers, and affect tissue repair. Elevation of CRP serum level will be affected by IL-6 levels.2
Injury to nerve tissues in the skin layer can cause severe pain due to peripheral and central sensitization. Peripheral sensitization occurs due to the release of local inflammatory mediators. Central sensitization occurs due to recurrent pain stimulation. Pain will aggravate stress response.1,12
Cytokine response can be suppressed by the administration of ketamine. According to a review by Golubovskiy and Vanags, the addition of a low dose of ketamine before the induction of general anesthesia produces a decrease in the secretion of proinflammatory cytokines IL-6 and tumor necrosis factor-α, as well as maintains the production of IL-2.7 In a review of ketamine and peripheral inflammation, De Kock et al summarized that ketamine acts as a homeostatic regulator of acute inflammatory reactions and stress-induced immune disturbances.8 Ketamine prevents the exacerbations and extension of local inflammation, without blunting local process and delaying the resolution of inflammation. In vitro studies have clearly shown that ketamine can significantly reduce the number of proinflammatory cytokines without affecting the production of anti-inflammatory cytokines. Ketamine reduces the expression of adhesion molecules on the surface of immune cells, thereby limiting diapedesis of neutrophils to inflammation sites and attenuating increased production of superoxide anions by neutrophils.5,8,14 The regulatory role of ketamine is more pronounced when administered before the injury.8
Ketamine provides powerful analgesic effects, which last until postoperative period.10 There is growing evidence that low-dose ketamine plays an important role in improving the management of postoperative pain when used as an adjuvant opioid or a local anesthesia.7 In a study by Hassan, it was concluded that low-dose intravenous ketamine prior to spinal anesthesia, showed some preventive or preemptive analgesic properties, prolonging spinal block, delaying the onset of pain, reducing the need for analgesia, and resulted in lower pain scores in the early few hours (up to 8 hours) postoperatively. Analgesic properties of ketamine are achieved through inhibition of N-methyl-D-aspartate receptors.
Ketamine attenuates postoperative CRP level through several mechanisms. Elevated CRP level reflects stress response or inflammation reaction. CRP is one of the acute-phase proteins produced by the liver, which is involved in acute-phase response. Elevation of CRP serum level will be affected by IL-6 level (a proinflammatory cytokine).
Conclusion
Low-dose intravenous ketamine effectively attenuates CRP stress response in patients undergoing emergency cesarean section with spinal anesthesia. Pain scores did not differ significantly in both the groups. There was a weak positive correlation between postoperative VAS score of pain and CRP level, which was statistically significant. Low-dose intravenous ketamine does not affect the Apgar scores of newborns.
Disclosure
The authors report no conflicts of interest in this work.
References
Deakin CD. Metabolism, the stress response to surgery and perioperative thermoregulation. In: Aitkenhead AR, Moppett IK, Thompson JP, editors. Smith & Aitkenhead’s Textbook of Anaesthesia. 6th ed. China: Elsevier; 2013:180–198. | ||
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–117. | ||
Burton D, Nicholson G, Hall G. Endocrine and metabolic response to surgery. Continuing Ed Anaesthesia Crit Care Pain. 2004;4(5):144–147. | ||
Cole DS, Watts A, Scott-Coombes D, Avades T. Clinical utility of peri-operative C-reactive protein testing in general surgery. Ann R Coll Surg Engl. 2008;90(4):317–321. | ||
Loix S, De Kock M, Henin P. The anti-inflammatory effects of ketamine: state of the art. Acta Anaesthesiol Belg. 2011;62(1):47–58. | ||
Dale O, Somogyi AA, Li Y, Sullivan T, Shavit Y. Does intraoperative ketamine attenuate inflammatory reactivity following surgery? A systematic review and meta-analysis. Anesth Analg. 2012;115(4):934–943. | ||
Golubovska I, Vanags I. Anaesthesia and stress response to surgery. Proc Latv Acad Sci. 2008;62(5):141–147. | ||
De Kock M, Loix S, Lavand’homme P. Ketamine and peripheral inflammation. CNS Neurosci Ther. 2013;19(6):403–410. | ||
Kuczkowski KM, Reisner LS, Lin D. Anesthesia for cesarean section. In: Chestnut DH, editor. Obstetric Anesthesia: Principles and Practice. 5th ed. Philadelphia: Mosby; 2014:545–603. | ||
Dershwitz M, Rosow CE. Pharmacology of intravenous anesthetics. In: Longnecker DE, Brown DL, Newman MF, Zapol WM, editors. Anesthesiology. 2nd ed. New York: McGraw-Hill; 2012:687–702. | ||
Rathmell JP, Rosow CE. Intravenous sedatives and hypnotics. In: Flood P, Rathmell JP, Shafer S, editors. Stoelting’s Pharmacology & Physiology in Anesthetic Practice. 5th ed. Illinois: Wolters Kluwer Health; 2015. | ||
Singh M. Stress response and anaesthesia. Altering the peri and post-operative management. Indian J Anaesth. 2013;47(6):427–434. | ||
Hassan AA. Pre-emptive analgesic effect of low dose N-methyl-D-aspartate receptor antagonists: ketamine and magnesium in conjunction with spinal anesthesia. Alexandria J Anaesth Intensive Care. 2006;9:18–25. | ||
Zilberstein G, Levy R, Rachinsky M, et al. Ketamine attenuates neutrophil activation after cardiopulmonary bypass. Anesth Analg. 2002;95:531–536. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.