Back to Journals » Open Access Emergency Medicine » Volume 15
Effective Coverage of Emergency Obstetric and Newborn Care Services in Africa: A Scoping Review
Authors Alemayehu M , Yakob B , Khuzwayo N
Received 12 January 2023
Accepted for publication 18 April 2023
Published 24 April 2023 Volume 2023:15 Pages 93—108
DOI https://doi.org/10.2147/OAEM.S403145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Mihiretu Alemayehu,1,2 Bereket Yakob,1,3 Nelisiwe Khuzwayo2
1School of Public Health, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 2School of Nursing and Public Health, Discipline of Public Health, University of Kwazulu-Natal, Durban, South Africa; 3School of Population and Public Health, the University of British Columbia, Vancouver, BC, Canada
Correspondence: Mihiretu Alemayehu, PO Box: 138, Wolaita Sodo, Ethiopia, Tel +251913213443, Fax +251465515113, Email [email protected]
Objective: This scoping review aimed to map the evidence of effective coverage (EC) of EmONC (Emergency Obstetric and Neonatal Care) services and associated factors in Africa.
Methodology: The review used PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews) checklist to select, appraise, and report the findings. We searched four databases (PubMed, Web of Science, Google Scholar, and Scopus) and grey literature published between Jan 01, 2011 – Dec 31, 2020. The search terms included “emergency”, “obstetric”, “newborn”, “effective coverage”, and “quality” with Boolean terms, AND and OR. The review was conducted using title, abstract, and full-article screenings. The results were analyzed thematically using NVivo v12 qualitative research data analysis software.
Results: Of the 1811 searched studies, 32 met the eligibility criteria for review. The majority of the studies were from East (56.3%) and Western (28.1%) Africa. Most studies were cross-sectional, had targeted health facilities, and combined two or more data collection techniques. The thematic analysis yielded three themes: EmONC service utilization, quality of EmONC service, and factors associated with the quality of EmONC services. The review showed a scarcity of evidence and variations regarding the crude coverage, quality of care, and factors affecting the quality of EmONC services in Africa.
Conclusion: The review reported that the utilization of EmONC services was below the WHO-recommended 100% in all studies, though some reported improvements over time. Disparities in EmONC services quality were paramount across studies and contexts. However, the methodological and analytical incongruity across studies brought difficulties in tracing and comparing the progress made in EmONC services utilizations.
Registration: This scoping review protocol was first registered on the Open Science Framework (OSF) on Aug 27, 2021 (https://osf.io/khcte/).
Keywords: maternal health, newborn health, obstetric care, perinatal care, emergency medicine
Introduction
Pregnancy is mothers’ riskiest experience while bringing new life to this world. It usually accompanies life-threatening complications such as severe bleeding, infection, unsafe abortion, hypertensive disorders, and delivery complications leading to death and disabilities.1 According to the 2019 WHO report, more than 810 mothers die daily during pregnancy or childbirth, causing 295,000 maternal deaths.2 Evidence shows that 94% of the estimated maternal deaths occurred in low-income countries.2 Compared to the developed world, the maternal mortality ratio was 40 times higher in the least developed countries.1 For instance, in Sub-Saharan Africa, there were 542 maternal deaths/100,000 live births, while there were only 7–10 maternal deaths/100,000 live births in Australia and Europe.1
Emergency obstetric and neonatal care (EmONC) is a package of care for mothers and neonates when severe life-threatening complications occur during pregnancy, child delivery, and postpartum. EmONC is believed to avert three-fourths of maternal mortality.3 Nevertheless, the effectiveness of EmONC depends on the health facilities’ readiness to provide care, quality of care, and the functionality, timeliness, and organization of referral systems in a given setting.4,5 In low-income countries, health systems have minimal resources and capacities, and women needing EmONC services often face challenges in accessing and utilizing them.5 Lack of evidence on the EC of EmONC services and factors affecting the utilization of quality service hinders the delivery of contextual solutions to maternal and child health problems in Africa.6
Several indicators have been defined to monitor maternal and child health.7 The third goal of the Sustainable Development Goals (SDGs) focuses on good health and well-being. The goal aims to improve maternal and child health by tracking the progress using indicators such as reducing global maternal mortality to less than 70/100,000 live births and neonatal mortality below 12/1000 live births. It also focuses on achieving universal health coverage and access to quality service by 2030.7 Recent studies of health systems have led to a proliferation of research that gives attention beyond access to the actual quality of care, highlighting the need for EC (a fraction of potential health gain delivered to the population in need). This concept combines the three widely used EC components: need, coverage/utilization, and quality of healthcare interventions.8–12 Though there are other ways to measure EC for health services, evidence suggests that quality-adjusted coverage is preferable to measuring maternal and child health services’ EC. It is believed to provide an overall impression of EC in global, regional, national, and local settings.12
The evidence stated EC as a fraction of potential health gain delivered through a health intervention by the health system, which is measured through the three components: need, use, and quality of healthcare service. The need is the population that needs a given health intervention (EmONC services). At the same time, use is the utilization of the intervention (EmONC services) among the people in need.13 The Donabedian framework of quality assessment remains the foundation of quality assessment today. The framework assesses service quality using the triads, namely, structure, process, and outcome of health care. “Structure” is defined as the setting, qualification of providers, and administrative system through which care (EmONC) is provided. “Process” is defined as the components of care (EmONC) delivered, while “outcome” is recovery, restoration of function, and survival (after EmONC services are provided).11,14
A scoping review was selected as the method of choice to study the EC of EmONC services and the factors affecting service quality. It is an appropriate method to map the evidence available in Africa, and no such study has been conducted to the authors’ knowledge. It helps to understand the existing knowledge gap in a broader context.15 Improving EC of EmONC services is among the major global priority health agenda.7,16 Hence, this review aimed to map evidence on EC of EmONC services and factors associated with quality service utilization in Africa. Therefore, this review will help policymakers, researchers, and stakeholders undertake evidence-based decisions on EmONC services to improve Africa’s maternal and neonatal health and well-being.
Methodology
This scoping review followed Arksey and O’Malley’s proposed scoping review framework. The framework consists of six steps: (a) identifying the research question and eligibility criteria, (b) identifying relevant studies, (c) selecting the studies and appraising the quality, (d) charting the data, (e) collating, summarizing, and reporting the results, and (f) consultation.17
Identifying the Research Question
This scoping review had the following research questions:
- What is the level of EC of EmONC services in Africa?
- What is the level of quality of EmONC services in Africa?
- What are health facility-related factors associated with the utilization of quality EmONC services in Africa?
- What are maternal behavioral factors related to using quality EmONC services in Africa?
- What sociodemographic factors are associated with utilizing quality EmONC services in Africa?
Eligibility of the Research Question
This study involved the core elements of the Population, Concept, and Context (PCC) suggested by the 2015 Joanna Briggs Institute methodology for scoping review guideline to determine the eligibility of the research question.18 (Table 1)
 |
Table 1 The PCC Framework of JBI Methodology for Scoping Review for Defining the Eligibility of the Research Question |
Identifying Relevant Studies
This review comprehensively identified relevant studies by searching published and unpublished (grey) literature databases. The investigators used PubMed, Web of Science, Google Scholar, and Scopus to search for published evidence. The WHO, Demographic and Health Survey (DHS) report, and other international organizations’ websites were searched for relevant grey literature. We used the following key terms in combination and appropriate Medical Subject Heading (MeSH) terms to search for relevant studies from the electronic databases: “Emergency Service”, “Emergency Medical Services”, “Emergenc*”, “Obstetric*”, “Labor Complication*”, “Pregnancy Complication*”, “Obstetric care service*”, “obstetric service*”, “Neonatal Nursing”, “Neonatal service*”, “Neonatal care”, “Newborn”, “Effective coverage”, “Quality of Health Care”, “quality service*”, ‘quality-adjusted delivery care”, “Risk Factors”, “Factors associated”, and “Africa”. (Table 2)
 |
Table 2 Data Charting (Studies Included in the Scoping Review) |
We used the Boolean terms’ AND’ and “OR” to separate keywords. We also used truncation and field codes/tags of title, MeSH terms, and text words/keywords for filtering. We limited the selection of studies based on their publication date. Accordingly, studies published in Africa from Jan 01, 2011, to Dec 31, 2020, were considered for review. The investigators also searched the reference list of all identified grey literature and published articles for additional studies. The authors have tried contacting the authors of the identified studies for further information and support.
Selecting the Studies and Appraising the Quality
Eligibility Criteria
This review included studies that fulfilled the following inclusion criteria:
- Studies presenting evidence of EC of Emergency Obstetric and Neonatal Care (EmONC) services
- Studies showing evidence of the quality of EmONC services
- Studies conducted in African countries
- Studies published in the English language
- Studies published on or after Jan 01, 2011 (Jan 01, 2011 – Dec 31, 2020)
- Studies published in peer-reviewed journals or grey literature with extractable primary research data with qualitative research, randomized controlled trials, non-randomized studies, quantitative descriptive studies, and mixed methods studies.
This review was conducted using the three stages. In the first stage, the principal investigator did a title screening, removed the duplicates, and exported the studies to Endnote 20. Two independent reviewers used the eligibility criteria in the second and third stages to do abstract and full-article screenings. When the studies were not accessible, investigators attempted to contact the authors and the University of KwaZulu-Natal library service. The third reviewer’s decision was accepted to resolve any disagreement at the abstract screening stage. The investigators described the screening using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.19 (Figure 1)
 |
Figure 1 PRISMA 2009 Flow Diagram for selection of studies. Note: Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG; The, Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097.19 |
Quality Appraisal
The selected studies’ quality was assessed using the Mixed Methods Appraisal Tool (MMAT) 2018 version.20 This tool helped the investigators evaluate the quality of different study designs in terms of appropriateness of the study’s aim, methods, study design, study participant selection, data collection, analysis, discussion, and conclusion.
Charting the Data
A customized data charting table was developed and used for the review (Table 2) and piloted by two independent investigators using a random sample of 10 included studies for consistency. It was used to extract information from the included data sources/documents. The table was modified as required based on the investigators’ feedback and was updated continuously throughout the review. After data extraction, the comparison was made, and any disagreement was resolved through discussion. The third investigator was consulted in cases of disputes to reach a consensus. The review used NVivo version 12 software (QSR International Pty Ltd, Burlington, MA, USA) to classify, sort, arrange, examine, and extract the relevant outcomes through thematic analysis.
Collating, Summarizing, and Reporting the Results
This scoping review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews (PRISMA-ScR) checklist (Supplementary File). 21 The review presented a numerical summary description at each stage of the PRISMA flow diagram. The charting and appraisal tools’ findings were summarized and presented in tabular form using the respective tools’ categories.
The investigators presented a summarized diagrammatic presentation of eligible articles’ major characteristics, such as the study’s characteristics, including geographic location, design, data collection techniques, and target populations. The relevancy of data for the research question on factors affecting the quality of EmONC services was presented for each evidence source and sorted by the data’s perspective. The investigators have also undergone thematic analysis to summarize the results based on themes from the extracted data.
Consultation
Investigators consulted the key stakeholder groups (health system leaders/decision-makers, healthcare providers, and service users). Investigators also consulted non-governmental organizations involved in the EmONC services delivery and obtained relevant inputs on the literature gap and understanding for the review.
Result
The database search yielded 1787 studies, and the grey literature search yielded 24 studies, of which 31 duplicates were removed. Next, 1655 studies were removed during the title and abstract screening because they did not meet the inclusion criteria, and 93 were removed during the entire article screening stage (as they were either not specific to EmONC or PCPs). Finally, 32 studies were included in the study. The steps used to select studies for the review are provided in the PRISMA flow diagram (Figure 1).
Characteristics of Included Studies
The Studies’ Location and Types
Most studies were from East and Western African countries (Figure 2). A variety of studies were included in the review, including 18 cross-sectional studies,22–39 seven qualitative studies,40–46 one prospective before-after study,47 one forthcoming chart review study,48 two retrospective studies,49,50 one mixed method study,51 one interventional study,52 and one observational study.53
 |
Figure 2 Geographic distribution of included studies, 2022. |
The Studies’ Focus
Most included studies targeted health facilities and a combination of at least two target populations (representing a combination of health facilities, women, care providers, stakeholders, and others). However, only six and four studies targeted only service users (women and newborns) and care providers (Figure 3).
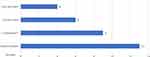 |
Figure 3 Population of included studies, 2022. |
The Studies’ Methods
Besides, 19 studies combined two or more data collection techniques. The most commonly used method was record review followed by interview and observation of the facility for infrastructure availability. However, only one study directly observed care provision (clinical skill). (Figure 4)
 |
Figure 4 Data collection methods of included studies, 2022. |
Key Findings
The thematic analysis of included literature yielded three themes: EmONC service utilization, quality of EmONC services, and factors linked with the quality of EmONC services.
Utilization/Crude Coverage of EmONC Services
Of the 32 reviewed studies, 13 reported the crude coverage (use) of the EmONC services.25,27,29,31,32,34–39,47,49 It ranged from 3% in 2011 in Ethiopia32 to 73% in 2016 in Togo.27 Studies from Ethiopia and Nigeria reported a high unmet need for EmONC services in which 3%,11 and 3.9%10 of women with obstetric complications were treated at fully functional EmONC facilities in Ethiopia and Nigeria, respectively, varied significantly by the sub-national administrative structures. The national EmONC assessments from Ethiopia,36 Sierra Leone,35 Ghana,39 Malawi,37 and Gambia38 reported that 18%, 20%, 34%, 51%, and 56%% of women with obstetric complications were treated at health facilities, with a significant disparity by the sub-national administrative structures.
Four studies have also shown a progressive improvement in EmONC service utilization. A study from Mozambique reported that the EmONC service utilization increased from 20% in 2007 to 26% in 2012.25 A Nigerian study also reported a threefold increase in EmONC service utilization (3.3% to 9.9%) within three years (2012 to 2015). In the same study, the percentage of women who sought care outside health facilities dropped significantly from 8.3% to 3.2%.47 Furthermore, studies from Cameroon49 and Burkina Faso29 also reported an increasing trend in EmONC service utilization.
Quality of EmONC Services
We also found evidence of the quality of EmONC services measured in various ways. Of the 32 included studies, 27 reported the quality of EmONC services and used a single index or a combination of indices to measure the Quality of EmONC services. The most commonly used methods in the included studies were structure, process quality, perceived quality, and case fatality rates (CFRs) as measurements of EmONC service quality. Most studies reported providing quality EmONC services as the primary challenge, though some reported a progressive improvement.
Structure/Input Quality
Of four articles that assessed the structure/input quality of EmONC services, three reported that none of their facilities performed at the expected level of EmONC service quality (measured using checklist-guided assessment).22,24,34 One of the studies said that the quality of EmONC services was inadequate (based on documentation) though some indices indicated excellent and sound levels.30
A study from South Africa reported a 56.7% average drug availability with complete unavailability of some drugs, including parenteral antibiotics, ergometrine, and diazepam.24 Similarly, the essential drugs were unavailable or poorly available in facilities with good infrastructure in a study from Kenya.30 In a study from DRC, the structural quality of EmONC services was 41%, in which face mask, Manual Vacuum Aspiration (MVA), and magnesium sulfate were the least available elements, with a prevalence of 4%, 6%, and 10%, respectively.22 Besides, in a study from Tanzania, facilities did not perform at the expected level for EmONC services, mainly due to the unavailability of essential drugs and the inability to perform vacuum extraction and blood transmission.34
Process/Observed Quality
Only two studies30,53 reported the quality of EmONC services using process indicators through direct observation of activities occurring in the clinical setting and documentation of process indicators. An observational study from Egypt reported poor quality of EmONC services (with particular attention on third delay and blood transfusion), ie, only 62% of patient’s vital signs were checked, and 93% of patients who needed resuscitation received it. The same study also reported that the average time between physical examination and medical or surgical intervention was three hours, the time spent was not justified on medical grounds by obstetricians in 60% of the cases, and anesthesia was initiated late in >50% of cases.53
However, a multi-site cross-sectional study from Kenya stated a wide interquartile range (IQR) of process indicators, suggesting variable process indicators. The record review revealed that the obstetric history was adequately documented (when documented in >75% of the cases). Still, parity and previous deliveries were graded as moderately adequate (recorded in 51–74%) and inadequate (recorded in <50%), respectively.30
Perceived Quality
Of the 32 included studies, five23,28,42–44 reported the quality of EmONC services based on care providers’ or receivers’ (patients’) perspectives on facility infrastructure, care providers’ respectful care, or satisfaction with the overall EmONC services. Two studies reported that the average perceived quality ranged from 66.7% in Adigrat, Northern Ethiopia,23 to 79.4% in Jimma, Western Ethiopia.28
Three studies reported the high quality of EmONC services from participants’ perspectives (care receivers or providers).28,42,44 For instance, women in a qualitative study in Kenya reported that they experienced improvements in the quality of EmONC services provided after the care providers received training on the EmONC services.42 However, in a study from Ethiopia, only 41.2%, 45.2%, and 34.7% of women stated the input, process, and outcome (satisfaction) components as good quality.23 Besides, a study from Tanzania reported a “good” perceived quality regarding the structure quality of EmONC services but discouraging responses regarding communication with care providers.44
Case Fatality
Fifteen of the 32 included studies25–27,31,33–39,47–50 used the CFR as a means of the EmONC service quality assessment method. The CFR in the included studies ranged from 1.3% in Togo27 to 11% in Cameroon.49 It exceeded the UN-recommended maximum of less than 1% in all the studies except grey literature. Studies from Togo,27 Ethiopia,50 Tanzania,31 and Nigeria31 reported relatively lower direct obstetric CFR, ie, 1.3%, 1.9%, 3%, and 3.2%, respectively. However, studies from DRC,26 Mozambique,25 and Cameroon49 reported higher direct obstetric CFR, amounting to 5.1%, 5.2%, and 11%, respectively. However, the Gray literature review of national surveys reported lower CFRs, ranging from 0.8% in Ethiopia36 to 3% in Sierra Leone.35
Ten studies also reported intrapartum and very early neonatal deaths,25,27,31,35–39,47,49 ranging from 19.3 per 1000 deliveries in Mozambique25 to 83.7 in Togo.27 The studies reported significant disparities across districts and regions. However, the national surveys of five countries reported relatively similar intrapartum and very early neonatal deaths ranging from 20 per 100 deliveries in Malawi37 to 27 in Gambia.38
The included studies reported improved and worsened CFR trends with varying extent/levels over time. For instance, in Mozambique, the direct obstetric CFR decreased by half (5.2% to 2.8%,) and the stillbirth rate dropped by one-third (29.3 to 19.3/1000 births) in five years.25 However, studies from Nigeria and Cameroon reported a deteriorating trend in quality service. Accordingly, the direct obstetric CFR in a study from Nigeria increased from 3.1% in 2012 to 4.1% in 2015.47 Similarly, in a study from Cameroon, the direct CFR and intrapartum neonatal death rate increased by 3% in three years.49
Factors Associated with Utilization of Quality EmONC Service
Seventeen of the 32 studies reported the aspects of using Quality EmONC services. The studies reported the sociodemographic factors, maternal behavioral and health service utilization-related factors, and health facility and health system-related factors associated with the utilization of quality EmONC services.
Sociodemographic Factors
Four studies reported that patients’ residence, educational status, and age were associated with using quality EmONC service.23,43–45 Three studies particularly underlined that the sociodemographic factors were the vital predisposing factors to adverse maternal outcomes, far exceeding the health system’s failure.23,43,45 For instance, in a study from Tanzania, women’s tendency to express their feeling and pain was highly affected by their educational status; only educated women said their emotions and pain during medical/surgical procedures and other obstetric service provisions.44 Young age, unemployment, poverty, distance, and residence were reported as barriers to perceived quality EmONC service utilization.23,43
A qualitative exploratory study from Ethiopia also reported very high maternal mortality (>4%) from remotely located facilities.41 Besides, qualitative research from Ghana indicated that the financial burden exerted on women resulted in maternal death due to inadequate transportation.46 A companion’s presence was also reported as a facilitating factor, where such mothers (accompanied by their relatives) had a seven times higher risk of obtaining quality EmONC service.23,43
Maternal Behavioral and Health Service Utilization-Related Factors
A qualitative study from Nigeria reported that mothers who visited traditional or religious delivery places come to health facilities lately and face a higher risk of complications and adverse health outcomes. Ignorance, preference for traditional birth attendants, and the cultural preference for vaginal delivery increased the risk.23,43 On the contrary, ANC follow-up had higher odds of quality of basic EmONC services.23 The quality of EmONC service was also associated with women’s preference for care providers’ sex.43
Health Facility and Health System-Related Factors
The need for more efficiency in resource allocation, particularly scarcity of beds, rooms, supplies, and ambulances, challenged the provision of quality obstetric services in Burundi and Uganda,45 Ethiopia,41 Kenya,40 and Nigeria.47 This was further explained by a study from Ethiopia, where a unit decrease in satisfaction with the availability of medical supplies decreased the overall clients’ satisfaction by 0.23 units.28 Besides, the absence of stationary was a major causal factor for the deficiency of partograph usage in Tanzania.34 The shortage of qualified staff and the increased workload were also reported as barriers to quality EmONC service provision.40,42,45–47
Effective communication was reported as one of the determining factors for delivering quality EmONC services. A study from Ghana reported that a lack of communication hampered pre-referral communication between facilities.46 A qualitative explanatory study from Ethiopia also reported that the language barrier affected midwives’ ability to provide quality EmONC services.41 Another study from Ethiopia and Tanzania reported that women’s satisfaction was associated with healthcare providers’ communication.28,44
Transportation and referral system-related challenges were also raised as determining factors for the delivery of quality EmONC services. Using vehicles other than ambulances was mentioned as a quality-compromising circumstance because of the inability to ensure appropriate care, such as vital sign follow-up and provision of intravenous drips.46 Besides, late arrival (as a result of transportation-related challenges) resulted in CFRs in Northern Nigeria.47
Healthcare workers’ clinical skill gap and training were also identified as factors determining the provision of quality EmONC services. In some contexts, patients presented with advanced complications because of the referring facility’s clinical skill gap in recognizing the danger signs on time.46 Women’s obstetric complications were also poorly managed at the appropriate facility level.43 The insufficient pre-service and in-service training also contributed to poor-quality EmONC services.40,47 Besides, the role of training in providing quality EmONC services was also reported in studies from Kenya, Burundi, and Uganda.42,45,48
The absence of supervision and coordination was also a critical barrier to providing quality emergency obstetric care.40,41,45 Nevertheless, the effectiveness of the supervisory role was identified as a controversial issue in cases of routine “traditional” supervision that did not result in the provision of the needed supplies.46 Furthermore, poor curriculum,45 treatment protocol,41 policies, and specific action plans43 were reported as factors influencing the delivery of quality EmONC services.
Studies also reported the lack of regulation and monitoring as contributing factors to poor quality service delivery.22,41,45 On the contrary, in a study from Nigeria, the increase in CFR was associated with better record keeping.47 Studies also revealed that poor staff motivation influenced the provision of quality EmONC services.41 For instance, in a qualitative study conducted in Burundi and Uganda, demoralization and lack of recognition resulted in staff absenteeism.45
Effective Coverage of EmONC Service
The included studies reported evidence on coverage, use, and Quality of EmONC services. Out of the 32 included studies, 13 said both utilization and Quality of EmONC services, whereas 14 reported only the quality of EmONC services. However, none of the studies reported the combined result of EC of EmONC services.
Discussion
This review mapped evidence of EC of EmONC services and factors affecting the quality of services. It revealed a great diversity in the availability of evidence on crude coverage, quality of care, and associated factors. Furthermore, the findings indicated that the evidence of the EC of EmONC services lacked comprehensiveness in Africa.
The estimates of EC are highly relevant since they can show the bottlenecks in achieving better impact.54 Despite the EC’s growing and direct relevance in tracking the progress towards SDG 3,55 the evidence on EC for the EmONC services lacks, though it exists for other health interventions.56 Though studies focusing on the comprehensive estimate for EC of EmONC services were lacking in Africa, the review identified evidence of crude coverage and the quality of EmONC services.
The crude coverage (utilization) of EmONC services was a prioritized topic in the reviewed articles, with 40% reporting it. In addition, wide variations are observed by study time, methods, and country. Although progressing improvements were documented, universal coverage of EmONC services was not achieved in all studies,25,29,47,49 only to remain below the WHO’s target. For instance, most of the needed EmONC services are unmet in some countries, ie, 97% in Ethiopia32 and 96.1% in Nigeria31 were not addressed. National EmONC assessments, ie, in Ethiopia,36 Sierra Leone,35 Ghana,39 Malawi,37 and Gambia,38 showed significant variations in the EmONC services utilization by the sub-national administrative structures. Unless tailored, contextualized, and accelerated interventions are implemented, it is imminent that most countries will face challenges in achieving the SDG goal of improving maternal and newborn health.
The scoping review showed that providing quality EmONC services remained one of the continent’s most challenging interventions and unattained goals. Few studies.11,14 have shown an improvement in the quality of EMONC services over time, and most (84%) studies relied on one or more of the Donabedian quality triads. The input and process components were less emphasized in the reviewed studies, while the majority (62.5%) focused on the outcome indicators. Despite the relevance of the facilities’ settings, care providers’ qualification, and administration,11 the current review revealed that evidence on the structural quality of EmONC service is limited in Africa. Furthermore, the review showed poor structural quality. It has also demonstrated poor adherence to the standards of care, including inadequate documentation of the patient’s past medical history30 and inadequate clinical actions.53 Despite its relevance to evaluating the content of care,14 the review underlined that the process component of EmONC services quality is overlooked in Africa.
On the contrary, the outcome quality of EmONC services was more researched and had a variable level. However, the review identified the methodological and analytical inconsistencies across studies as a primary challenge to the comparability of the results, implying the need for uniform (harmonized) techniques. The direct obstetric case fatality rate (DOCFR), the proportion of women admitted to an EmONC facility with major direct obstetric complications or who develop such complications after admission, and die before discharge, is one of the proxy measures to assess the quality of EmONC services.8 Although CFR’s methodological approach is relatively consistent among the included studies, the findings vary. Besides, though evidence underlined complementing it with other valid indicators (since the absence of case fatality in primary health care facilities does not necessarily indicate higher quality),8 the review revealed that the included studies lacked triangulation of their findings to render a better understanding of EmONC service quality. Nonetheless, most reviewed articles exceeded the UN-recommended minimum level, implying the tension behind the progress toward achieving SDG goal 3.7
The review also identified the factors linked with providing quality EmONC services. The sociodemographic characteristics (patients’ residence, educational status, age, unemployment, poverty, distance, and place) and maternal behavioral and health service utilization-related factors (ignorance, preference for traditional birth attendants, culture, ANC follow-up, and care providers’ sex preference) impacted the provision of quality EmONC services. Besides, the health facility and health system-related factors such as resource allocation, staff motivation, transportation and referral system, training, curriculum and treatment protocol, policies, and specific action plans have positively or negatively influenced the provision of quality EmONC services. Hence, interventions pointing at the identified factors could help improve the EC of EmONC services. For instance, staff motivation was cited in the reviewed articles as an essential factor influencing the provision of quality EmONC services.40,54 Interventions, including most Results-Based Financing (RBF), positively impacted the motivation of care providers to improve their performance.54,57,58 Similar evidence from LMICs supported the application of such interventions to improve care providers’ commitment and feelings of professionalism, which subsequently lead to receivers’ satisfaction.57,58
Limitation
This study only includes studies published in English on Jan 01, 2011 – Dec 31, 2020, so studies published in other languages were excluded from the review despite their significance to the study’s scope.
Conclusion
Evidence of EC of EmONC services lacks comprehensiveness (with regard to the three components: need, use, and quality) in Africa. However, the review explored evidence on crude coverage and quality of EmONC services with a wide variability across studies, study period, and sub-national administrative structures. The utilization of EmONC services was lower than the WHO-recommended 100% in all studies, though some reported a progressive improvement. The variation in the quality of EmONC services and assessment techniques was observed in the review, which has shown wide disparity across studies. In addition to the scarcity of evidence on the structural quality of EmONC services in Africa, the review explored the inadequacy of structural quality, particularly essential drugs and equipment. Furthermore, despite their drawbacks, the perceived quality and CFRs were widely researched in the review, while very few studies assessed the content of care for EmONC service quality.
The perceived quality of EmONC services has shown a variable level (very low to high) in the continent. However, the methodological and analytical inconsistencies across studies ultimately resulted in difficult comparability of the results, implying the need for uniform (harmonized) techniques. The high CFRs in the review indicated the low outcome quality of EmONC services. However, studies did not complement their results with other assessment techniques since lower CFRs do not necessarily mean better quality. The review further explored and identified sociodemographic, maternal behavioral, and health service utilization-related factors influencing the utilization of quality EmONC services in Africa.
Recommendation
The incongruity of EmONC service quality assessment methods needs to be harmonized to trace and compare the progress toward achieving the SDG goals in the continent. We also recommend robust data collection systems and incorporating indicators that better reveal the quality of EmONC services, mainly content of care components. Furthermore, a comprehensive (that encompasses all its components) study is suggested to understand the EC of EmONC services in Africa.
Abbreviations
BEmONC, Basic Emergency Obstetric and Newborn Care; CEmONC, Comprehensive Emergency Obstetric and Newborn Care; CFR, Case Fatality Rate; DHS, Demographic and Health Survey; DOCFR, Direct Obstetric Case Fatality Rate; DRC, Democratic Republic of Congo; EC, Effective Coverage; EmONC, Emergency Obstetric and Newborn Care; EmOC, Emergency Obstetric Care; FGD, Focus Group Discussion; IDI, Individual In-depth Interview; IQR, Inter-quartile Range; JBI, Joanna Briggs Institute; KII, Key-Informant Interview; LMIC, Low and Middle-income Country; MMAT, Mixed Methods Appraisal Tool; MeSH, Medical Subject Heading; OSF, Open Science Framework; PCC, Population, Concept, and Context; PRISMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews; SDG, Sustainable Development Goal; UNICEF, United Nations Children’s Fund; WHO, World Health Organization.
Data Sharing Statement
All data used for this study are cited and presented as references.
Acknowledgment
Our gratitude goes to the School of Nursing and Public Health, Discipline of Public Health, University of KwaZulu-Natal, and Wolaita Sodo University for assistance with the protocol and provision of necessary resources.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division. Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division. Geneva: World Health Organization; 2019. Available athttps://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/.
2. WHO. Maternal Mortality in 2017: Estimates Developed by WHO, UNICEF, UNFPA, and the World Bank. Geneva: World Health Organization; 2019. Available athttps://www.who.int/en/news-room/fact-sheets/detail/maternal-mortality.
3. WHO. Managing Newborn Problems: A Guide for Doctors, Nurses, and Midwives. Geneva: World Health Organization; 2003. Available athttps://www.who.int/maternal_child_adolescent/documents/9241546220/en/.
4. Souza JP, Gülmezoglu AM, Vogel J, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross-sectional study. Lancet. 2013;381(9879):1747–1755. doi:10.1016/S0140-6736(13)60686-8
5. Illias K, Paswan B, Anand A, Mondal NA. Praying until death: revisiting three delays model to contextualize the socio-cultural factors associated with maternal deaths in a region with high prevalence of eclampsia in India. BMC Pregnancy Childbirth. 2019;19(1):314. doi:10.1186/s12884-019-2458-5
6. Holmer H, Oyerinde K, Meara JG, Gillies R, Liljestrand J, Hagander L. The global met need for emergency obstetric care: a systematic review. BJOG. 2015;122(2):183–189.
7. UN. About the Sustainable Development Goals; 2015. Available from: https://www.un.org/sustainabledevelopment/sustainable-development-goals/.
8. WHO, UNFPA, UNICEF, AMDD. Monitoring Emergency Obstetric Care: A Handbook. Geneva: Switzerland; 2009
9. Campbell J, Buchan J, Cometto G, et al. Human resources for health and universal health coverage: fostering equity and effective coverage. Bull World Health Organ. 2013;91(11):853–863. doi:10.2471/BLT.13.118729
10. Admasu K, Haile-Mariam A, Bailey P. Indicators for availability, utilization, and quality of emergency obstetric care in Ethiopia, 2008. Int J Gynaecol Obstet. 2011;115(1):101–105. doi:10.1016/j.ijgo.2011.07.010
11. Ayanian JZ, Markel H. Donabedian’s Lasting Framework for Health Care Quality. N Engl J Med. 2016;375(3):205–207. doi:10.1056/NEJMp1605101
12. Marsh AD, Muzigaba M, Diaz T, Requejo J, Jackson D. Effective coverage measurement in maternal, newborn, child, and adolescent health and nutrition: progress, future prospects, and implications for quality health systems. Lancet Global Health. 2020;8(5):e730–e6. doi:10.1016/S2214-109X(20)30104-2
13. Shengelia B, Tandon A, Adams OB, Murray CJL. Access, utilization, quality, and effective coverage: an integrated conceptual framework and measurement strategy. Soc Sci Med. 2005;61(1):97–109. doi:10.1016/j.socscimed.2004.11.055
14. Berwick D, Fox DM. “Evaluating the Quality of Medical Care”: donabedian’s Classic Article 50 Years Later. Milbank Q. 2016;94(2):237–241. doi:10.1111/1468-0009.12189
15. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi:10.1186/s12874-018-0611-x
16. WHO, HRP, UNICEF, UNFPA, USAID, FIGO. Strategies toward ending preventable maternal mortality (EPMM) 2015. Available from: https://data.unicef.org/resources/strategies-toward-ending-preventable-maternal-mortality/.
17. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616
18. Peters M, Godfrey C, McInerney P, et al. The Joanna Briggs Institute Reviewers’ Manual: Methodology for JBI Scoping Reviews. Adelaide, SA Australia: The Joanna Briggs Institute; 2015:1–24.
19. Moher D, Liberati A, Tetzlaff J, Altman DG; The, Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097
20. Quan N, Pierre P, Sergi F, et al. Mixed methods appraisal tool (MMAT) version 2018. Dep family med. 2018;3:354–371.
21. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and Explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850
22. Mpunga Mukendi D, Chenge F, Mapatano MA, Criel B, Wembodinga G. Distribution and quality of emergency obstetric care service delivery in the Democratic Republic of the Congo: it is time to improve regulatory mechanisms. Reprod Health. 2019;16(1). doi:10.1186/s12978-019-0772-z
23. Berhane B, Gebrehiwot H, Weldemariam S, Fisseha B, Kahsay S, Gebremariam A. Quality of basic emergency obstetric and newborn care (BEmONC) services from patients’ perspective in Adigrat town, Eastern zone of Tigray, Ethiopia. 2017: a cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):6534.
24. Pearl Thwala SB, Blaauw D, Ssengooba F. Measuring the preparedness of health facilities to deliver emergency obstetric care in a South African district. PLoS One. 2018;13(3):324.
25. Augusto O, Keyes EE, Madede T, et al. Progress in Mozambique: changes in the availability, use, and quality of emergency obstetric and newborn care between 2007 and 2012. PLoS One. 2018;13(7):e0199883. doi:10.1371/journal.pone.0199883
26. Ntambue AM, Malonga FK, Cowgill KD, Dramaix-Wilmet M, Donnen P. Emergency obstetric and neonatal care availability, use, and quality: a cross-sectional study in the city of Lubumbashi, Democratic Republic of the Congo, 2011. BMC Pregnancy Childbirth. 2017;17(1). doi:10.1186/s12884-017-1224-9
27. Ouédraogo AM, Nikiema L, Meda IB, N’Tapi K, Kouanda S. Indicators of availability, use, and quality of emergency obstetric and neonatal care in Togo in 2012. Int J Gynecol Obstet. 2016;135(S1):S7–S10. doi:10.1016/j.ijgo.2016.08.014
28. Kumsa A, Tura G, Nigusse A, Kebede G. Satisfaction with emergency obstetric and new born care services among clients using public health facilities in Jimma Zone, Oromia Regional State, Ethiopia; a cross-sectional study. BMC Pregnancy Childbirth. 2016;16(1). doi:10.1186/s12884-016-0877-0
29. Kouanda S, Ouédraogo AM, Ouédraogo GH, Sanon D, Belemviré S, Ouédraogo L. Emergency obstetric and neonatal care needs assessment: results of the 2010 and 2014 surveys in Burkina Faso. Int J Gynecol Obstet. 2016;135:S11–S5. doi:10.1016/j.ijgo.2016.08.008
30. Kosgei RJ, Gathara D, Kamau RK, et al. Quality of comprehensive emergency obstetric care through the lens of clinical documentation on admission to labour ward. East Afr Med J. 2016;93(2):82–90.
31. Abegunde D, Kabo IA, Sambisa W, et al. Availability, utilization, and quality of emergency obstetric care services in Bauchi State, Nigeria. Int J Gynecol Obstet. 2015;128(3):251–255. doi:10.1016/j.ijgo.2014.09.029
32. Admasu K, Haile-Mariam A, Bailey P. Indicators for availability, utilization, and quality of emergency obstetric care in Ethiopia, 2008. Int J Gynecol Obstet. 2011;115(1):101–105.
33. Maswanya E, Muganyizi P, Kilima S, Mogella D, Massaga J. Practice of emergency obstetric care signal functions and reasons for non-provision among health centers and hospitals in Lake and Western zones of Tanzania 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Health Serv Res. 2018;18(1). doi:10.1186/s12913-018-3685-6
34. Solnes Miltenburg A, Kiritta RF, Bishanga TB, van Roosmalen J, Stekelenburg J. Assessing emergency obstetric and newborn care: can performance indicators capture health system weaknesses? BMC Pregnancy Childbirth. 2017;17(1). doi:10.1186/s12884-017-1282-z
35. Government of Sierra Leone UNFPA, UNICEF, WHO, UKAID. Sierra Leone Rapid Emergency Obstetric and newborn Care (EmONC) Assessment 2017; 2017. Available from: https://sierraleone.unfpa.org/en/publications/sierra-leone-rapid-emergency-obstetric-and-newborn-care-emonc-assessment-2017.
36. Ethiopian Public Health Institute FMoH, Averting Maternal Death and Disability. Ethiopian Emergency Obstetric and Newborn Care (EmONC) Assessment. 2016; 2017. Available from: https://www.ephi.gov.et/images/pictures/download2010/FINAL-EmONC-Final-Report-Oct25-2017.pdf.
37. Malawi Health Ministry, UNFPA, UNICEF, Clinton Health Access Initiative, Save the Children. Malawi Emergency Obstetric and Newborn Care Needs Assessment, 2014; 2015. Available from: https://www.healthynewbornnetwork.org/resource/malawi-emergency-obstetric-newborn-care-needs-assessment-2014/.
38. Gambia Ministry of Health & Social Welfare, UNICEF, WHO, AMDD, Program/Mailman School of Public Health/Columbia University. Gambia National Assessment for Emergency Obstetric and Newborn Care, 2012; 2012. Available from: https://gambia.unfpa.org/en/publications/national-assessment-emergency-obstetric-and-newborn-care.
39. Ghana Ministry of Health, UNICEF, UNFPA, WHO, AMDD. National Assessment for Emergency Obstetric and Newborn Care Ghana; 2011.
40. Hirai M, Morris J, Luoto J, Ouda R, Atieno N, Quick R. The impact of supply-side and demand-side interventions on use of antenatal and maternal services in western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):453. doi:10.1186/s12884-020-03130-4
41. Geleto A, Chojenta C, Taddele T, Loxton D. Perceptions of midwives on the quality of emergency obstetric care at hospitals in Ethiopia: a qualitative explanatory study. Midwifery. 2020:90.
42. Banke-Thomas A, Maua J, Madaj B, Ameh C, Van Den Broek N. Perspectives of stakeholders on emergency obstetric care training in Kenya: a qualitative study. Int Health. 2019;12(1):11–18. doi:10.1093/inthealth/ihz007
43. Okonofua F, Randawa A, Ogu R, et al. Views of senior health personnel about quality of emergency obstetric care: a qualitative study in Nigeria. PLoS One. 2017;12(3):e0173414. doi:10.1371/journal.pone.0173414
44. Stal KB, Pallangyo P, van Elteren M, van den Akker T, van Roosmalen J, Nyamtema A. Women’s perceptions of the quality of emergency obstetric care in a referral hospital in rural Tanzania. Trop Med Int Health. 2015;20(7):934–940. doi:10.1111/tmi.12496
45. Chi PC, Bulage P, Urdal H, Sundby J. Barriers in the delivery of emergency obstetric and neonatal care in post-conflict Africa: qualitative case studies of Burundi and Northern Uganda. PLoS One. 2015;10(9):e0139120. doi:10.1371/journal.pone.0139120
46. Afari H, Hirschhorn LR, Michaelis A, Barker P, Sodzi-Tettey S. Quality improvement in emergency obstetric referrals: qualitative study of provider perspectives in Assin North district, Ghana. BMJ Open. 2014;4(5):e005052. doi:10.1136/bmjopen-2014-005052
47. Kabo I, Orobaton N, Abdulkarim M, et al. Strengthening and monitoring health system’s capacity to improve availability, utilization and quality of emergency obstetric care in northern Nigeria. PLoS One. 2019;14(2):e0211858. doi:10.1371/journal.pone.0211858
48. Spitzer RF, Steele SJ, Caloia D, et al. One-year evaluation of the impact of an emergency obstetric and neonatal care training program in Western Kenya. Int J Gynecol Obstet. 2014;127(2):189–193. doi:10.1016/j.ijgo.2014.05.023
49. Kadia RS, Kadia BM, Dimala CA, Aroke D, Vogue N, Kenfack B. Evaluation of emergency obstetric and neonatal care services in Kumba Health District, Southwest region, Cameroon (2011-2014): a before-after study. BMC Pregnancy Childbirth. 2020;20(1). doi:10.1186/s12884-020-2774-9
50. Girma M, Yaya Y, Gebrehanna E, Berhane Y, Lindtjørn B. Lifesaving emergency obstetric services are inadequate in south-west Ethiopia: a formidable challenge to reducing maternal mortality in Ethiopia. BMC Health Serv Res. 2013;13(1). doi:10.1186/1472-6963-13-459
51. Austin A, Gulema H, Belizan M, et al. Barriers to providing quality emergency obstetric care in Addis Ababa, Ethiopia: healthcare providers’ perspectives on training, referrals and supervision, a mixed methods study. BMC Pregnancy Childbirth. 2015;15(1). doi:10.1186/s12884-015-0493-4
52. Mirkuzie AH, Sisay MM, Reta AT, Bedane MM. Current evidence on basic emergency obstetric and newborn care services in Addis Ababa, Ethiopia; a cross sectional study. BMC Pregnancy Childbirth. 2014;14(1). doi:10.1186/1471-2393-14-354
53. Nada KH, Barakat AA, Gipson R. Quality of care for obstetric emergencies in 4 general hospitals in Egypt: an observational study of delays in receiving care and blood bank services. East Mediterr Health J. 2011;17(1):19–25. doi:10.26719/2011.17.1.19
54. Walque D, Kandpal E, Wagstaff A, et al. Improving Effective Coverage in Health: Do Financial Incentives Work? World Bank Group; 2022.
55. Marsh AD, Muzigaba M, Diaz T, et al. Effective coverage measurement in maternal, newborn, child, and adolescent health and nutrition: progress, future prospects, and implications for quality health systems. Lancet Global Health. 2020;8(5):e730–e6.
56. Amouzou A, Leslie HH, Ram M, et al. Advances in the measurement of coverage for RMNCH and nutrition: from contact to effective coverage. BMJ Global Health. 2019;4(Suppl 4):e001297. doi:10.1136/bmjgh-2018-001297
57. Zitti T, Gautier L, Coulibaly A, Ridde V. Stakeholder Perceptions and Context of the Implementation of Performance-Based Financing in District Hospitals in Mali. Int J Health Policy Manag. 2019;8(10):583–592. doi:10.15171/ijhpm.2019.45
58. Bertone MP, Meessen B. Studying the link between institutions and health system performance: a framework and an illustration with the analysis of two performance-based financing schemes in Burundi. Health Policy Plan. 2013;28(8):847–857. doi:10.1093/heapol/czs124
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
