Back to Journals » Open Access Emergency Medicine » Volume 14
Effect of Structured Briefing Prior to Patient Arrival on Interprofessional Communication and Collaboration in the Trauma Team
Authors Iattoni M, Ormazabal M, Luvini G, Uccella L
Received 1 May 2022
Accepted for publication 13 July 2022
Published 30 July 2022 Volume 2022:14 Pages 385—393
DOI https://doi.org/10.2147/OAEM.S373044
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Martina Iattoni, Matias Ormazabal, Giorgia Luvini, Laura Uccella
Emergency Department, EOC - Ospedale Regionale di Lugano, Lugano, Switzerland
Correspondence: Laura Uccella, Emergency Department, EOC - Ospedale Regionale di Lugano, Canton Ticino, Lugano, Switzerland, Tel +41 91 8116657, Fax +41 91 811 6002, Email [email protected]
Purpose: Treating a multiple trauma patient is multidisciplinary team work. The performance of the trauma team is crucial to treating the patients safely and effectively. The fundamentals of the performance are the quality of interprofessional collaboration and the communication inside the team and its efficacy for patients’ safety and team’s well being. This is a prospective interventional study. The aim of this paper was to assess interprofessional collaboration and perceived efficacy inside the trauma team and to evaluate the effects of the implementation of a trauma team briefing tool before the arrival of the patient on perceived teamwork performance.
Participants and Methods: The study took place in the emergency department. Participants were members of the trauma team (emergency physicians and nurses). Two validated scales were selected that address interprofessional collaboration and team perceived efficacy: the TEAM survey (revised version) and the Mayo High Performance Teamwork Scale. A detailed and structured team briefing was used. The trauma team filled in the two scales (46 participants). Prior to every multiple trauma patient arrival, the briefing was then implemented for 3 months. At the end of the third month, the two scales were re-administered and the results analysed (31 participants). The main outcome was the variation of proportion of desirable answers. We considered significant only clearly separated confidence intervals (95% CI).
Results: All items in the questionnaires had better responses in the second round. In 16 items, the differences found were statistically significant with a 95% confidence interval and p< 0.05. The perceived communication and collaboration by healthcare professionals of the trauma team improved with the introduction of the tool.
Conclusion: A team briefing prior to the arrival of a multiple trauma patient enhances providers’ self perception of interprofessional collaboration in the management of multiple trauma patients.
Keywords: multiple trauma, critical care, communication, interprofessional collaboration, team briefing
Introduction
Treating a multiple trauma patient requires working in a multidisciplinary team consisting of physicians and nurses from different specialities. The performance of the team is crucial to treating the patient safely and effectively.1,2
The World Health Organization defines teamwork as two or more people who interact interdependently with a common purpose, working toward measurable goals that benefit from leadership that maintains stability while encouraging honest discussion and problem solving.3
Teamwork issues, and namely collaboration and communication are among the most contributory factors to good performance.4
A lack of communication/collaboration is often identified as a primary point of vulnerability for quality and safety of care even with a standardised and simple clinical approach such as the universally used ATLS (Advanced Trauma Life Support – American College of Surgeons). Improving communication and collaboration is therefore a top priority.5 There is a strong belief that effectiveness of healthcare teams can be improved by team interventions.6
Thus, interventions that address interprofessional collaboration problems have the potential to improve professional practice and healthcare outcomes.7,8
In the literature three types of interventions were distinguished: Training, either based on pre-defined principles or on general team training; Tools, interventions that structure, (ie, (de)briefing checklists), facilitate (ie, through communication technology), or trigger (through monitoring and feedback) teamwork; Organisational (re)design is about (re)designing structures to stimulate team processes and team functioning.9
As for the Emergency Department, there are numerous papers in the literature describing multiple interventions to improve interprofessional collaboration in various settings,9 but not much has been written on interprofessional collaboration in the trauma team.10,11 There is even less about the perception of interprofessional collaboration by the trauma team and about the possible changes that intervene and their measure. What we have is mainly in the nursing field, not in the medical field.12 Especially, prospective evidence remains rare and most data is obtained in a simulated setting.13
Our Emergency Department is a medium-size level 1 trauma centre in Switzerland, managing around 350 multiple traumas per year. In our department, all multiple trauma patients from all over the Ticino region are admitted. Ninety-three multiple trauma patients with an average ISS (Injury Severity Score) indicating a major trauma (predominantly head, thoracic, abdominal and long bone injuries) were referred to our centre during the 3 months covered by the study.
Nurses and physicians caring for such patients are a mix of specialised and in-training (residents) personnel not always used to work together (due to the rotation of the residents). This leads to a number of discontents with the perceived communication and cooperation. The dissatisfactions are perceptible, but difficult to formalise.
Hence, the feeling was that baseline interprofessional collaboration had to be assessed and one or more interventions had to be implemented.
Participants and Methods
Overall Study Design and Ethics
Prior to the beginning of this study, a request to the ethics committee of Canton Ticino was made to find out whether their authorisation was necessary. The Committee answered that it was not because the study did not involve patients.
All the participants volunteered to participate and received no reward for the participation. The inclusion criterion was to be part (doctor or nurse) of the trauma team.
In the first part of the study two questionnaires were administered to healthcare professionals (doctors and nurses) working on multiple trauma patients in our Emergency Department. Each participant agreed to participate and gave informed consent in the online form before completing the questionnaire. Providing consent was essential in order to start filling out the questionnaire. The questionnaires were filled out online anonymously and only a few personal data were requested such as type of profession and level of training.
In the second part of the study, the intervention aimed at improving interprofessional collaboration was implemented for a 3-month period. We judged that a duration of 3 months was sufficient for the team to familiarise with the instrument.
The intervention consisted of carrying out a structured briefing when the pre-hospital system announced the arrival of a multiple trauma patient. The briefing was based on the work of Purdy et al published in 2020.18
The structure of the briefing was as follows: introduction (thanks to team members and any introductions); details of pre-announcement by the pre-hospital system and approach to the patient on arrival at the hospital; what might change and what the priorities of care would become in this case; assignment of specific roles; request for suggestions, clarifications (Figure 1).
 |
Figure 1 Team briefing structure. Data from Purdy et al.18 |
Participants Description
The trauma team is composed of 52 professionals (34 nurses, 18 doctors).
The briefing was conducted by the team leader. The team leader was one of the nine senior emergency physicians of the trauma team (the one on duty). The need to always do the briefing before the arrival of the patient with multiple trauma was emphasised in meetings and by email and we verified that it was actually done. There were no difficulties nor deviations from protocol.
The briefing was always performed prior to the arrival of all patients with multiple trauma who presented during the examined period. We verified its execution. To prevent it from not being performed, we made an alert on the multiple trauma patient arrival announcement checklist, created action cards for team leaders and hung signs with the briefing questions in our shock room.
The intervention (about 5 minutes long) was carried out for 3 months to allow all the medical/nursing staff that played a role in the care of multiple trauma patients to be familiar with the tool.
In the third part of the study, the two questionnaires previously filled-in were re-administered and analysed for possible changes.
The administration of the questionnaires took place without the respondents being aware that the impact of the briefing was to be assessed. This is to avoid the potential bias of assessing the briefing and its perceived efficacy by team members instead of the interprofessional collaboration and communication.
Apart from the introduction of the briefing prior to the arrival of the multiple trauma patient, no other changes were made during the entire 3-month period, neither technical/non-technical nor in the composition of the team.
Primary End-Point Definition
The aim of this paper is to address the need for assessing and improving interprofessional collaboration and to evaluate the effects of the implementation of a trauma team briefing tool before the arrival of the patient on perceived collaboration/communication performance.
Our hypothesis was that the implementation of this tool would improve interprofessional collaboration and communication among team members.
The main outcome was the variation of proportion of desirable answers in the two selected questionnaires.
Measurement Tools
Before starting, a review of the literature was performed and two validated scales were selected:13
- The TEAM survey (revised version) assesses the efficacy of the team and the satisfaction of personnel.14 It consists of 46 items that can be rated on a scale from 1 to 5 where 1 is totally disagree and 5 is totally agree. Discriminant validity of the tool was good as was internal consistency with a Cronbach alpha of 0.94.14
- Mayo High Performance Teamwork Scale measures the overall perceived performance of the team.15 It consists of 16 items that can be rated on a scale from 0 to 2 where 0 is never or rarely and 2 is consistently. The scale showed satisfactory internal consistency and construct validity by Rasch (person reliability=0.77; person separation=1.85; item reliability=0.96; item separation=5.04) and traditional psychometric (Cronbach’s alpha=0.85) indicators.15
The choice fell on these scales because they best suit the work in multidisciplinary teams in the context of emergencies and multiple trauma.
Other questionnaires (eg, AITCS II or the Jefferson scale)16,17 have some items relevant to our context but contain sections that are more adaptable to a ward context or are only validated on students. There are very few tools in the literature that address the evaluation of collaboration and communication within a team.
Data Collection Process
The questionnaires were completed online for the first part between the 27th of February and 14th of March 2021. We received 46 responses (88%).
The implementation phase of the briefing took place between 15th of March and 15th of June 2021. During this period, the trauma team treated 93 multiple trauma patients.
The same questionnaires were then re-administered online to the same participants between the 16th of June and the 1st of July 2021, and we received 31 responses.
The second round of questionnaires was administered during a summer holiday period. In addition, some members of the trauma team (six residents and two senior) ended their rotation in the emergency department between the first and second rounds and left the hospital for another Swiss Canton. This led to a decrease in the number of respondents.
All respondents filled in the questionnaires completely.
Statistical Procedures
Statistical analysis was performed using the open-source packages “Pandas”, “NumPy”, “SciPy”, “Seaborn” and “PyMC” for Mac Os X versions 0.23.0, 11.1.3, 1.1.0, 0.8.1 and 2.3.6, respectively. Statistical significance was considered achieved based on highly credible intervals of parameter estimates.19 Confidence intervals (CI) were calculated at 95%.
We used a Bayesian methodology (albeit with uninformative a-priori) as the number of respondents was small and it does not have the sample size limitations that frequentist methods relying on asymptotics do, and addresses uncertainty be producing “fatter” confidence intervals. We calculated a P-value only as a usual reference.
The problem with measuring the difference in scores was that the reconstructed scores (assigning a numerical score to a qualitative judgment such as “totally agree” or “not at all agree”) is arbitrary. Averaging the values obtained in this way is not meaningful because variables that are nor quantitative nor metric are measured. We decided, for each item of the questionnaires, to divide the scores into “desirable” and “non-desirable”. We considered as “desirable” a response in which collaboration/communication was good by the respondent and as “undesirable” a response in which collaboration/communication was not considered good. For the positive items (eg, I am proud of being part of this team), the highest scores were evaluated as desirable (4 and 5 for the Team scale and 2 for the Mayo scale), while for the negative items (eg, I do not feel part of this team), the lowest scores were evaluated as desirable (1 and 2 for the Team scale and 0 for the Mayo scale). We then measured the proportion of people who gave a desirable answer in the first questionnaire and compared it with the proportion of people who gave a desirable answer in the second questionnaire.
Results
The sociodemographic data of the respondents are summarised in Table 1. Grossly, two-thirds of the respondents were nurses, reflecting the composition of the trauma team in the emergency department. All but one dedicated physicians responded to the first questionnaire, and the vast majority of nurses (29/34). The number of trauma team members responding to the second questionnaire decreased slightly.
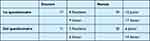 |
Table 1 Sociodemographic Data of Respondents |
For the Team Survey, the answers were divided into the categories indicated by its authors:
- Team identification
- Team potency
- Team interaction models
- Team models (subcategories: knowledge of team members and utilisation of team members)
- Meta-cognitions
- Communication
- Perspectives
- Valuing others
Team interaction models and team models are part of what the authors called “shared mental models” while the last three categories (communication, perspectives and valuing others) represent what the authors called “team orientation”.
Shared mental models are intended as a shared understanding of the structure of the team, its tasks and the roles of its members in patient care.
Statistical analysis concentrated on differences in the answers’ rating between the first and second questionnaire (Figures 2 and 3).
 |
Figure 2 Confidence intervals (CI) of the most statistically relevant answers to the TEAM scale. |
 |
Figure 3 Confidence intervals (CI.of the most statistically relevant answers to the Mayo High Performance Teamwork Scale. |
Team identification: no statistically significant differences were noted.
Team potency: statistically significant differences were noted on item 2 (“this team feels it can provide a high-quality service”) in the sense of improvement (confidence interval (CI) before the implementation of the briefing 54.0–80.2%, after the implementation of the briefing 79.1–98.1%, p<0.001).
Shared mental models: a statistically significant difference was noted on item 1 (“if asked I could explain all of the roles in the team and how they overlap”) in the sense of improvement (CI before 63.8–87.4% after 84.0–94.8%; p<0.001). There was also a significant difference in items 6 and 7, positive and negative, respectively (“all team members are aware of where to go for information when they need it” and “it is not always obvious where we should go for information when we need it”) (CI item 6 before 37.4–64.9% after 66.8–92.6%; p<0.001; CI item 7 before 46.3–78.9% after 28.9–56.9%; p<0.005). As for team models, item 6 (“the team takes into consideration the capabilities of its members”) scored significantly higher (CI before 45.7–73% after 71.3–94.7%; p<0.001).
Metacognition: no statistically significant differences were observed.
Team orientation: of the six communication items, three were statistically significant, namely items 1, 3 and 4 (“team members act upon the information I communicate to them”, “this team has agreed methods for communication” (Figure 1) and “communication between team members is unclear”). Respectively, higher scores were observed in items 1 and 3 and a lower score in item 4 (negative item) (CI item 1 before 32.3–61.3% after 56.5–86.3%; p<0.001; item 3 before 32.8–60.7% after 63.4–91%; item 4 before 70.9–94.6% after 44.7–73.1%; p<0.001). In the two sections of perspectives and valuing others no statistically significant differences were observed.
The Mayo High Performance Teamwork Scale takes into consideration four categories of behaviours:
- Cooperation/communication
- Leadership/management
- Situation awareness
- Decision-making
The items that differed in a statistically significant way were
- 1 and 2 (concerning leadership and namely “a leader is clearly recognised by all team members” (Figure 2) and “ the team leader assures maintenance of an appropriate balance between command authority and team member participation”) (CI item 1 before: 40.8–68.8% after 74.6–96.7%; p<0.001; item 2 before 28.8–56.6% after 56.3–86%; p<0.001),
- 3, 4 and 10 (concerning role management, namely “each team member demonstrates a clear understanding of his or her role” (Figure 3), “the team prompts each other to attend to all significant clinical indicators throughout the procedure/intervention” and “when appropriate, roles are shifted to address urgent or emergent events”) (CI item 3 before 43.8–71.1% after 71.1–94.9%; p<0.001; item 4 before 38.8–67% after 60.1–88.5%; item 10 before 35.0–63.5% after 67.3–92.6%; p<0.001),
- 8, 9 and 15 (concerning cooperation, namely “all members of the team are appropriately involved and participate in the activity”, “disagreements or conflicts among team members are addressed without a loss of situation awareness” and “when statements directed at avoiding or containing errors or complications do not elicit a response to avoid or contain the error, team members persist in seeking a response”) (CI item 8 before 29.0–57.0% after 56.4–86.4%; p<0.001; p<0.001; item 9 before 32.8–60.4% after 47.4–79%; p<0.001; item 15 before 31.3–58.8% after 60.5–88.6%; p<0.005).
Discussion
The present study is one of the few studies in the literature that addresses the evaluation of the effect of using a specific tool (the pre-arrival briefing of the multiple trauma patient) to improve collaboration and communication within a team. Even fewer studies assess the effect of such tools on trauma team.13
In this paper, we have shown how the use of a briefing before the arrival of multiple trauma is able to increase in several areas (team potency, shared mental models, team orientation, role identification and perception of cooperation and communication within the team) the team’s perception of its own communication and cooperation.
The issues that were assessed by the questionnaires are of high importance and are likely to impact on the well-being of health workers. It could be inferred that they also may impact on the real effectiveness of the care provided to the patient, although this cannot be stated, because it was not the aim of this study and it was not measured.
In this field, as said before, prospective evidence is rare and most data is obtained in a simulated setting.8,9,11,13 Our paper provides prospective data from real-life experience.
The number of respondents to the questionnaire is representative of the team, as we obtained many responses, well above the majority of the members. It could therefore be said that the results obtained are representative of the perception of the team about its own communication and collaboration.
The number of respondents in the second round of questionnaires was lower than in the first round due to contingent reasons explained in the results section. We do not believe that this could have affected our results, since the statistical analysis was designed to evaluate small samples and its significance is very robust. In addition, after the research closed, we conducted unstructured interviews with trauma team members, and all members confirmed to us how good the introduction of the briefing was. The briefing, after the study, has become part of our clinical practice and no trauma team member would think of doing without it, currently.
The internal coherence of the questionnaires was respected: positive items and their negative counterparts had a high internal coherence (all the changes observed in positive items are then observed in negative items with opposite sign).
Moreover, all the items underwent a variation in the sense of improvement of the perception of the evaluated themes, even when this variation was not statistically significant.
There was no variation (either significant or non-significant) in the sense of a worsening of the perception of the assessed performances in the questionnaires.
The items that were found to be statistically significant were in the areas of team potency, shared mental models, team orientation, role identification and perception of cooperation and communication within the team.
On the other hand, there were no significant variations in team identification and metacognition. These are identity and cognitive competence issues that were not addressed by the briefing, which focused rather on practical aspects of role and competence allocation and information sharing. In the literature, team identification and metacognition are instances that improve support between members and act as a buffer system for stress and could thus theoretically influence collaboration and communication. However, very little data exists in this regard.20,21
Thus, it seems possible to say that it was most likely the introduction of the briefing that improved our team’s perception of performance effectiveness. This is in agreement with the literature, although the evidence reported refers to mostly nursing experience only.12,17
The two scales we chose measure many elements of the perception of effectiveness with good internal consistency and psychometric validity (communication, coordination, collaboration, utilisation of the expertise of all members, respect, knowledge and responsibility for roles, shared objectives, etc) although metacognition and team identification are missing.13 A broader discussion of the literature seems difficult, as the goodness of the use of briefing, although often postulated, presents very little evidence.
We thought of anything else that may have occurred during the 3-month study period that may have influenced interprofessional collaboration and communication, but we could not identify any factor that may have done this.
The structured briefing prior to the arrival of the multiple trauma patient appears as a simple tool for improving clinical practice, at least in terms of the trauma team’s perception of its own communication/collaboration, if not also in terms of its actual effectiveness. We had no difficulties implementing the routine use of the tool.
The study is easily reproducible as the intervention was structured and the scales validated.
Strengths and Limitations
We could have chosen to divide the staff into two groups (team briefing implemented and not implemented) and conduct a prospective study comparing the two groups. Or we could have randomised the patients before arrival (briefing and non-briefing). Instead, we chose to compare two periods (before and after the team briefing) because we wanted to assess perceived effectiveness and interprofessional collaboration without the team being aware of the intervention we wanted to examine. Had they been aware of it, this could have led to evaluation biases, which we tried to exclude as much as possible. Choosing the first solution (staff divided into two groups) would have raised the question of how to select the groups, given that the degree of experience, perceived effectiveness and well-being of the workers is heterogeneous.
Our study has also some non-negligible limitations:
- The subjects interviewed, although representative of our trauma team, are numerically few. The statistical significance achieved is solid, but our situation may be dissimilar to that of other centres.
- The actual effectiveness of the care provided to the patient was not assessed. To say that the introduction of the briefing was the reason for the improvement in the team’s perception of their own performance is an arbitrary inference. Other factors may have intervened that are not apparent to the authors of this study, who tried not to influence colleagues. The fact that colleagues were not told that the briefing was the subject of the evaluation does not mean that some of them may not have understood it, although the authors of this paper have kept this strictly confidential.
- The choice of re-evaluation period (after 3 months) is arbitrary. We have found no literature on the subject. A future re-evaluation is probably necessary to understand whether the effects will be long-lasting.
Conclusion
In conclusion, a structured team briefing prior to the arrival of a multiple trauma patient can be a valuable tool to improve self reported perception of interprofessional collaboration, communication and the perception of effectiveness within the trauma team, at least in the areas of team potency, shared mental models, team orientation, role identification and perception of cooperation and communication within the team.
The briefing could perhaps prove useful both for the training of new trauma team professionals and for the performance of the team itself. In this regard, however, further studies are needed.
We are planning a multi-centre study in order to understand whether our results are generalisable.
Acknowledgments
Thanks to Lorenzo Emilitri, for all the time you have dedicated to us with statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cottey L, Roberts T, Blair G, et al. Need for recovery and physician well-being in emergency departments: national survey findings. Eur J Emerg Med. 2021;28(5):386–393. doi:10.1097/MEJ.0000000000000850
2. Cinar O, Ak M, Sutcigil L, et al. Communication skills training for emergency medicine residents. Eur J Emerg Med. 2012;19(1):9–13. doi:10.1097/MEJ.0b013e328346d56d
3. World Health Organization. Interprofessional collaborative practice in primary health care: nursing and midwifery perspectives; 2013. World Health Organization. Available from: https://apps.who.int/iris/handle/10665/120098.
4. Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaest Scand. 2008;53:143–151. doi:10.1111/j.1399-6576.2008.01717.x
5. Weller J, Boyd M, Cumin D, Berggren I. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. J Adv Nurs. 2019;75(3):585–593. doi:10.1136/postgradmedj-2012-131168
6. Jung HS, Warner-Hillard C, Thompson R, et al. Why saying what you mean matters: an analysis of trauma team communication. Am J Surg. 2018;215(2):250–254. doi:10.1016/j.amjsurg.2017.11.008
7. Lingard L, Whyte S, Espin S, Baker GR, Order B, Doran D. Towards safer interprofessional communication: constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483. doi:10.1080/13561820600921865
8. Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6(6):CD000072. doi:10.1002/14651858.CD000072.pub3
9. Müller M, Jürgens J, Redaelli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018;23(8):e022202. doi:10.1136/bmjopen-2018-022202
10. Bleetman A, Sanusi S, Dale T, Brace S. Human factors and error prevention in emergency medicine. Emerg Med J. 2012;29(5):389–393. doi:10.1136/emj.2010.107698
11. Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;8(3):CD000072. doi:10.1002/14651858.CD000072.pub2
12. Steinemann S, Bhatt A, Suares G, et al. Trauma team discord and the role of briefing. J Trauma Acute Care Surg. 2016;81(1):184–189. doi:10.1097/TA.0000000000001024
13. Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16–30. doi:10.1097/MLR.0b013e31827feef6
14. Millward LJ, Jeffries N. The team survey: a tool for health care team development. J Adv Nurs. 2001;35(2):276–287. doi:10.1046/j.1365-2648.2001.01844.x
15. Malec JF, Torsher LC, Dunn WF, et al. The mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills. Simul Health. 2007;2(1):4–10. doi:10.1097/SIH.0b013e31802b68ee
16. Orchard C, Pederson L, Read E, Mahler C, Laschinger H. Assessment of interprofessional team collaboration scale (AICTS): further testing and instrument revision. J Contin Educ Health Prof. 2018;38(1):11–18. doi:10.1097/CEH.0000000000000193
17. Hojat M, Ward J, Spanjorer J, Arenson C, Van Winkle LJ, Brett W. The Jefferson scale of attitudes toward interprofessional collaboration (JeffSATIC): development and multi-institution psychometric data. J Interprof Care. 2015;29(3):238–244. doi:10.3109/13561820.2014.962129
18. Purdy E, Alexander C, Shaw R, Brazil V. The team briefing: setting up relational coordination for your resuscitation. Clin Exp Emerg Med. 2020;7(1):1–4. doi:10.15441/ceem.19.021
19. Kruschke JK. Bayesian estimation supersedes the t-test. J Exp Psychol Gen. 2013;142(2):573. doi:10.1037/a0029146
20. McCarthy A, Garavan TN. Team learning and metacognition. A neglected area of HRD research and practice. Adv Dev Hum Resour. 2008;10(4):509–524. doi:10.1177/1523422308320496
21. Jimmieson NL, McKimmie BM, Hannam RL, Gallagher J. An investigation of the stress-buffering effects of social support in the occupational stress process as a function of team identification. Group Dynamics. 2010;14(4):350–367. doi:10.1037/a0018631
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
