Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Effect of ELOM-080 on exacerbations and symptoms in COPD patients with a chronic bronchitis phenotype – a post-hoc analysis of a randomized, double-blind, placebo-controlled clinical trial
Authors Beeh KM , Beier J , Candler H, Wittig T
Received 19 July 2016
Accepted for publication 10 October 2016
Published 23 November 2016 Volume 2016:11(1) Pages 2877—2884
DOI https://doi.org/10.2147/COPD.S117652
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Kai-Michael Beeh,1 Jutta Beier,1 Henning Candler,2 Thomas Wittig2
1Insaf Respiratory Research Institute, Wiesbaden, Germany; 2G. Pohl-Boskamp GmbH & Co KG, Hohenlockstedt, Germany
Background: Treating symptoms and preventing exacerbations are key components of chronic obstructive pulmonary disease (COPD) long-term management. Recently, a more tailored treatment approach has been proposed, in particular for two well-established clinical phenotypes, frequent exacerbators and chronic bronchitis-dominant COPD. ELOM-080 has demonstrated clinical efficacy in treating symptoms and preventing exacerbations in subjects with chronic bronchitis. However, little is known about the potential effects of ELOM-080 in COPD patients.
Aim: To evaluate the effect on exacerbation, cough sputum, and general state of health of long-term treatment with ELOM-080 in COPD patients with an exacerbation history and chronic bronchitis.
Methods: We performed a post-hoc analysis of a randomized, double-blinded, placebo-controlled parallel-group clinical trial of a 6-month treatment with ELOM-080 (3×300 mg) in patients with chronic bronchitis and concomitant COPD. The primary outcome was the proportion of subjects with at least one exacerbation over the 6-month study period. Secondary outcomes included the total number of exacerbations (ie, cumulative occurrence of exacerbations during the study period) and the proportion of acute exacerbations necessitating an antibiotic treatment, monthly evaluations of sputum and cough symptoms, and the general state of health and a safety analysis.
Results: Of 260 randomized subjects, 64 patients fulfilled the inclusion criteria for COPD (ELOM-080: 35, placebo: 29). Compared to placebo, ELOM-080 reduced the percentage of subjects with at least one exacerbation (29% versus 55%, P=0.031) and a reduction in the overall occurrence of exacerbations (ELOM-080: 10, placebo: 21, P=0.012) during the winter season. The percentage of asymptomatic or mildly symptomatic patients (sputum/expectoration and cough) was consistently higher in the ELOM-080 group compared to placebo, with statistical significant differences after 2 and 3 months of treatment (2 months: ELOM-080 25%, placebo 11%, P<0.005; 3 months: ELOM-080 26%, placebo 14%, P<0.05). Likewise the subjective rating of general health status was better in the ELOM-080 group with statistically significant superiority after 2 and 3 months of treatment (2-month treatment: P=0.015; 3-month treatment: P=0.024). Tolerability results were comparable between ELOM-080 and placebo.
Conclusion: ELOM-080 is efficacious in patients with COPD and a chronic bronchitis phenotype. Prophylactic use reduces the rate of exacerbations and improves the key symptoms of sputum and cough with a favorable long-term tolerability profile.
Keywords: COPD, exacerbations, winter, phytotherapy, myrtol, chronic bronchitis, sputum
Introduction
The term chronic obstructive pulmonary disease (COPD) has been established as an umbrella term to label a clinical syndrome characterized by chronic, poorly reversible airflow obstruction, airway inflammation in the presence of chronic bronchitis and/or pulmonary emphysema.1 It is, however, increasingly recognized, that distinct COPD phenotypes exist, and these may be prone to a more personalized, “targeted” management approach.2 In this regard, two important phenotypes have been described in recent years, the “frequent exacerbator” phenotype and the “bronchitic” (ie, sputum- or phlegm-producing) phenotype.
Exacerbations are considered key events in the clinical course of COPD, and the prevention of exacerbations is highlighted as a pivotal therapeutic goal and relevant outcome measure by current treatment strategies or guidelines. The distribution of exacerbations in COPD is not uniform, with seasonal3 or temporal4 clustering, in particular in a subset of COPD patients at high risk for exacerbations, where the individual’s history of prior exacerbations is a strong predictor of future events.5
In addition to frequent exacerbators, a clinical COPD phenotype characterized by increased sputum production and cough has been established over the past years.6 Mucus hypersecretion in COPD patients affects multiple important outcomes:7 mucus accumulation in small airways increases with COPD severity and is associated with decreased survival,8,9 chronic cough, and sputum production are associated with accelerated decline in forced expiratory volume in 1 second (FEV1),10 increased risk for pulmonary infections,11 and elevated frequency of exacerbations and hospitalizations.12
It has been demonstrated in well-controlled clinical trials, that COPD patients with the bronchitic phenotype may experience therapeutic benefits from anti-inflammatory treatment with a phosphodiesterase inhibitor, roflumilast, when added to standard inhaled therapy.13 In addition, a subset of patients with chronic sputum production and increased susceptibility to recurrent bacterial infections due to bacterial colonization may benefit from prophylactic long-term antibiotic treatment during the winter season,14 although results are conflicting.15 While some evidence supports the use of mucolytics in this indication,16–18 long-term treatment with both roflumilast and antibiotics is often limited by tolerability or safety issues. Hence, potential alternatives to prevent exacerbations in COPD patients with a “bronchitic” phenotype are needed.
ELOM-080 (trade name in Germany: GeloMyrtol® forte) is a distillate of a mixture of four rectified essential oils and approved for the treatment of acute and chronic bronchitis and sinusitis; in literature it is also denoted as Myrtol. There is a comprehensive knowledge about the mode of action. ELOM-080 is proven to have mucolytic, secretolytic, secretomotoric, anti-inflammatory, antioxidative, antimicrobial, and bronchospasmolytic effects.19–25 Preclinical evaluations in established COPD models demonstrated beneficial effects in rats, indicating an inhibition of proteins involved in mucus hypersecretion, eg, MUC5AC.26
A small-scale clinical trial in hospitalized COPD patients demonstrated beneficial effects of ELOM-080 versus placebo in terms of cough and dyspnea.27 In large-scale, clinical studies in placebo- or active-controlled settings of up to 6-month treatment duration, ELOM-080 significantly improved lead symptoms and signs of acute infectious bronchitis, and reduced the frequency of acute exacerbations in subjects with chronic bronchitis, with a favorable safety and tolerability profile.28–30 There exists, however, a significant overlap between chronic bronchitis and COPD, in particular in smokers.1 The authors therefore sought to evaluate the clinical efficacy of ELOM-080 treatment to prevent acute exacerbations by a post-hoc analysis in a subgroup of COPD patients with a chronic bronchitis phenotype, using the dataset of a previously published, randomized, placebo-controlled clinical trial of ELOM-080 in chronic bronchitis patients.29
Study design and methodology
The design and methods of the original study were reported in detail elsewhere.29 Briefly, eligible patients (n=260) with a diagnosis of chronic bronchitis were randomized to 6 months of treatment with ELOM-080 (3×300 mg daily) or matched placebo in a parallel-group, double-blinded, prospective clinical trial, performed in 19 practices (general practitioners, pulmonologists, and internal specialists) during the winter season in Germany. At screening, baseline conditions and eligibility were checked and medical history and demography including smoking habits recorded; physical examination, vital signs, and spirometry (FEV1) were performed and a safety lab sample was drawn. Subjects were originally eligible, if they fulfilled all of the following key inclusion criteria (for a full list of in- and exclusion criteria):29 A diagnosis of chronic bronchitis according to WHO definition,31 a screening pulmonary function result (forced expiratory volume in 1 second) of ≥50% predicted, and a history of at least one acute exacerbation in the past winter season.
Following randomization, follow-up visits were scheduled monthly to assess exacerbations, treatment compliance, change in concomitant medications, adverse events (AEs), and patient-rated overall efficacy of the study drug. Between visits, patients recorded the occurrence and impact of cough, sputum, and difficulty of expectoration in a diary card. Patients rated the occurrence of cough and sputum on a 4-point scale, where 1= constantly bothered, 2= often bothered, while 3= rarely bothered, and 4= never bothered at all. The general state of health was rated accordingly on a 4-point scale (1= very good; 2= good; 3= bad; 4= very bad).
The post-hoc analysis compared the effect of ELOM-080 versus placebo in a subset of the safety analyzable population of chronic bronchitis patients who additionally fulfilled diagnostic criteria for COPD. For this purpose, subjects were considered as COPD patients when they either a) had a documented physician diagnosis of COPD, or b) fulfilled all of the following three criteria: prescription of concomitant bronchodilator treatment (inhaled or oral beta-2-agonists, inhaled anticholinergics, oral theophylline); smoking history of at least 10 years; spirometric evidence of airflow obstruction, FEV1 ≤80% of the predicted value.
The original study was conducted in accordance with the Declaration of Helsinki, Good Clinical Practice and German Drug Law (Arzneimittelgesetz, AMG). The protocol was approved by the Regional Medical Chamber of Baden-Wurttemberg Ethics Committee as well as by independent local ethics committees and all patients gave informed written consent to participation prior to any study-related activities.
Outcomes
The primary outcome of the original study was the effect of study drug on the proportion of exacerbation-free subjects versus placebo over the whole treatment period of 6 months. Secondary parameters were the frequency of exacerbation, days of treatment with antibiotics, frequency and duration of inability to work, number and duration of hospitalizations, occurrence of AE, patients’ subjective assessment of the course of disease, investigator’s assessment of the therapeutic result, and the occurrence of clinically relevant changes of laboratory parameters.
The primary efficacy parameter of the present post-hoc analysis was the proportion of subjects experiencing at least one acute exacerbation of chronic bronchitis (AECB) during the study period. An acute exacerbation was defined by the presence or considerable increase of mucopurulent and purulent sputum and cough plus at least one of the following symptoms: increased sputum thickness, increased difficulty of expectoration, increased breathlessness, impairment of general health, cold-like symptoms, and increased body temperature (≥38°C). Exacerbations were considered as separate events only if they were separated by at least 2 weeks during which the patients symptoms had recovered.
Secondary outcomes included
- the total number of exacerbations after completion of the study period, ie, the cumulative occurrence of exacerbations over the 6-month period),
- the number of subjects with clinically relevant impairment due to cough and sputum for each month,
- the number of subjects with an at least good state of health for each month,
- safety/tolerability.
Statistical analysis
For the present post-hoc analysis, the sponsor of the study provided the full access to the complete original data set. Descriptive data analyses were performed using the Analysis Tool Pack of Microsoft Excel 2013. Categorical outcomes were contrasted by appropriate inferential statistics (chi-squared test), counts of items or events were compared with chi-square goodness of fit test.
Results
Patients
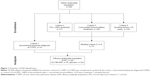
Of 260 enrolled patients, 64 had a confirmed diagnosis or fulfilled diagnostic criteria of COPD. The selection of the efficacy analyzable population is outlined in Figure 1. Distribution of single criteria for COPD diagnosis is listed only for subjects without a physician diagnosis of COPD. However, any of these criteria could have been present also in the physician diagnosis group. Of these, 35 patients were treated with ELOM-080, 300 mg three times daily orally, whereas 29 patients were treated with placebo.
The demographic characteristics of selected subjects are listed in Table 1. Patients in both groups were comparable, although ELOM-080-treated patients were on average slightly younger than subjects on placebo. Both treatment groups included predominantly male subjects. The median FEV1% predicted was 70.0 (interquartile range [IQR]: 61.1–77.0) in ELOM-080-treated patients versus 68.1 (IQR: 62.0–78.0) in the placebo group.
Exacerbations
Over the 6 months of treatment period, 29% (10 of 35) of ELOM-080-treated patients experienced at least one exacerbation, versus 55% (16 of 29) in the placebo group, the difference reaching statistical significance (P=0.031, compare Figure 2).
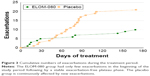
In addition, the total number of exacerbations during the study period was significantly lower with ELOM-080 versus placebo (10 events versus 21 events, P=0.012). The cumulative numbers of exacerbations are shown in Figure 3.
In the ELOM-080 group, 6 of 35 subjects (17%) had an acute exacerbation requiring an antibiotic treatment versus 10 of 29 subjects (34%) in the placebo group. Given the overall reduced absolute occurrence of exacerbations with ELOM-080, the percentage of exacerbations requiring treatment with antibiotics was comparable between the groups (60% versus 48%). The median antibiotic treatment duration was 5.5 days (range 5–14 days; mean 7.3±3.6 days) in the ELOM-080 group compared to 10 days (range 9–12 days; mean 10.7±1.49 days) in the placebo group.
Rating of symptoms and well-being
The percentage of subjects rating their impairment by cough and sputum as “rarely bothered” or “never bothered”, was higher with ELOM-080 versus placebo at all post-randomization visits, with a statistically significant difference observed after 2 months of treatment at visit 3 (P<0.005) and after 3 months of treatment at visit 4 (P<0.05). The rating of cough and sputum is shown in Figure 4.
More subjects rated their own health status as “good” or “very good” with ELOM-080 versus placebo, with a statistical significance after 2 and 3 months of treatment. During the whole treatment period, the general state of health was better in subjects randomized in the ELOM-080 group. A statistically significant difference was observed after 2 (P=0.015) and 3 months (P=0.024) of treatment (Figure 5).
Safety
Both treatments were well tolerated over the treatment of 6 months. A total of 96 AE were recorded (ELOM-080: 53 AE; placebo 43 AE). No serious AEs occurred. The causal relationship of at least “possible” (considered as adverse drug reaction, ADR) was rated in 16 events in 8 patients (ELOM-080: 5 patients; placebo: 3 patients) without any statistically significant difference between both treatment groups. Gastrointestinal ADRs were reported in 7 patients (ELOM-080: 4 patients; placebo: 3 patients), again without any statistically significant difference between the two treatment groups. The gastrointestinal ADRs of the ELOM-080 group were only reported within the first treatment month, while the ADRs of the placebo group had no obvious temporal relationship to the treatment duration. In the ELOM-080 group two patients discontinued prematurely versus one patient in the placebo group.
Discussion
Current treatment strategies and recommendations do not routinely recommend the use of mucolytics for the treatment of COPD, mainly due to a lack of consistent data from well-controlled clinical trials.1 The present post-hoc analysis suggests that treatment with ELOM-080 is a safe and effective treatment option in COPD subjects with the chronic bronchitis phenotype. This phenotype affects a significant proportion of the overall COPD population and is clinically associated with an increased risk for exacerbations and disease progression.6 In addition, COPD patients with the bronchitic phenotype appear to be at greater risk for experiencing mucopurulent exacerbations during the winter period.32
Importantly, in our post-hoc analysis, treatment with ELOM-080 over 6 months during the winter season was associated with a reduction in the exacerbation rate versus placebo and numerically or statistically significant improvements of symptoms of cough, expectoration, and sputum, and subjectively rated general health status over the course of 6 months. While health status benefits may be difficult to fully interpret in their clinical significance due to the use of a rather simple, not validated questionnaire, consistent effects on acute exacerbations were observed for both the reduced percentage of subjects experiencing at least one exacerbation, as well as the cumulative overall occurrence of exacerbations during the study period. Thus, the beneficial effects observed with ELOM-080 over the comparator arm were not driven by few patients experiencing multiple exacerbations under placebo. The reduction in acute exacerbations with ELOM-080 also led to fewer and shorter treatments of acute episodes with antibiotics. While the final decision to prescribe antibiotics – as in other published studies33,34 – was based on the treating physicians’ clinical judgment using criteria described in the methods section, the frequency of antibiotics usage may nonetheless serve as a crude estimate for the number of exacerbations caused by bacteria. The mechanism, by which ELOM-080 leads to a reduction in winter episodes of acute exacerbations in our post-hoc analysis of COPD patients is likely linked to the secretolytic properties, but may involve additional mechanisms. It is well documented that infection with common cold viruses, for example, rhinovirus, during the winter season promotes growth and spread of resident bacteria such as haemophilus influenzae, in particular in patients with significant chronic colonization.35 Thus, effects of ELOM-080 on mucociliary clearance may improve local lower respiratory tract host defense resulting in decreased virus-mediated flare-up of bacterial exacerbations. This is supported by the reduced occurrence of sputum/expectoration and cough symptoms under ELOM-080 versus placebo in our post-hoc analysis. However, as the nature of our data do not allow us to draw firm conclusions on whether these symptomatic improvements actually preceded the effect on exacerbations, it is also possible that the observed symptomatic effects are rather a consequence of than a cause of reduced exacerbations. In this regard, it is also possible that the effect of ELOM-080 on symptoms increased the threshold for a symptomatic “breakthrough” during an acute event, thus reducing the overall number of detected exacerbations.36 Importantly, the results on the efficacy of ELOM-080 in the COPD subgroup did not differ from the results in the overall population,29 where 28% of patients experienced at least one exacerbation versus 47% with placebo (P<0.01).
Exacerbations in COPD are recognized as heterogeneous events, and different interventions may impact on different exacerbation drivers, depending on their mechanism.37–39 In clinical practice, these drivers are often difficult to identify and no reliable biomarker exists this far to support characterization of exacerbations in routine care. Thus, it appears tempting to combine interventions with distinct modes of action in an attempt to maximize the potential for exacerbation prevention in an individual patient.40 Our results described herein with ELOM-080, in light of concurrent results of other mucosecretolytics in defined COPD populations16,17 and the well-documented safety of these agents, suggest that it is worthwhile to reconsider the potential role of these medicines in both the symptomatic and preventative treatment of COPD. In any case, the results presented herein may serve as a hypothesis for a future prospective clinical trial in this COPD phenotype using an appropriate clinical setting, eg, add-on treatment to bronchodilators.41
ELOM-080 was well tolerated in our study. The pattern of AE was typical for a COPD population and the occurrence of events not differed to placebo. Gastrointestinal AEs were rare and the temporal distribution immediately after initiation of treatment provides evidence of a habituation effect, so that these events do not limit a long-term use.
Limitations
Our analysis has some important limitations. First, the post-hoc nature of the study does not allow to draw any firm conclusions about the “true” effectiveness of ELOM-080 in a broader COPD population. However, the positive results of the current analysis nonetheless provided important data for hypothesis-generation for future trials in this population. Taking into account the drug’s mode of action, the observed effects were not unexpected and lend further support to the potential adjunct use of this class of medication in chronic therapy.42 Second, the target population recruited into the original study were chronic bronchitis, not COPD patients. However, there is significant clinical overlap between chronic bronchitis and COPD,6 particularly in smokers, and in fact, chronic bronchitis is an essential part of the umbrella diagnosis COPD. We used standard diagnostic criteria or a physician-based diagnosis of COPD to identify reliably those patients with concomitant COPD, ie, patients with a chronic bronchitic phenotype of COPD. In fact, a large proportion of the subjects included in the original study had concomitant bronchodilator therapy and presence of airflow limitation, evident by pre-bronchodilator FEV1 values between 62% and 78% (IQR) of predicted. While this criterion differs from current GOLD classification strategies (based on post-bronchodilator FEV1 values), the spirometric criteria were at the time of study conduct in line with the American Thoracic Society/European Respiratory Society criteria published in 1995.43 Therefore, we believe that the spirometric criteria we used – among others – were sufficient to reliably identify COPD patients.
Third, the definition of an exacerbation used in the present trial is suitable for AECB, while there are subtle differences from defining COPD exacerbations, although there are overlapping criteria.44,45 Further, we did not differentiate exacerbations into mild, moderate, and severe. As we did not observe any hospitalizations for COPD, it is possible to conclude that the exacerbations observed corresponded to mild-moderate exacerbations, with a substantial proportion necessitating additional medical treatment. However, our study design did not allow to capture steroid-treated exacerbation, as this was not part of the prespecified definition. In large-scale COPD exacerbation trials, the majority (up to 80%) of exacerbations are treated with antibiotics, either alone, or in combination with steroids.33,34 While there is evidence, that COPD subjects with chronic bronchitis phenotype may be more prone to recurrent bacterial exacerbations than subjects without this phenotype, the results of our post-hoc analysis cannot be generalized to exacerbations of other suspected causes, necessitating the introduction of systemic corticosteroid bursts. However, the authors are convinced that the demonstrated reductions in mucopurulent exacerbation with ELOM-080 versus placebo are meaningful and clinically relevant in this population.
Finally, our analysis did not include subjects with severe or very severe COPD, who have been shown to be at particular risk for exacerbations. However, the underlying mechanisms of exacerbations are not necessarily different in more severe stages of COPD, therefore it is possible that the observed effects with ELOM-080 on winter period exacerbations may also be replicated in these subjects.
Conclusion
This post-hoc analysis provides evidence of a beneficial effect of the mucosecretolytic ELOM-080, in preventing mucopurulent exacerbations and improving symptoms of chronic sputum production (sputum, phlegm, cough) in COPD patients with a “chronic bronchitic” phenotype. In light of the documented tolerability profile, reconsideration of this class of medicine as a potential maintenance or seasonal treatment in this subset of COPD patients appears justified.
Disclosure
The institution where KMB and JB are employed has received lecture fees, advisory honoraria, and compensation for design and conduct of clinical trials from various pharmaceutical companies in the past 5 years, including honoraria from G. Pohl-Boskamp GmbH&Co KG. HC and TW are full-time employees of G. Pohl-Boskamp GmbH & Co KG. The authors report no other conflicts of interest in this work.
References
Decramer M. GOLD: Global strategy for the diagnosis, management, and prevention of COPD; 2016 [Updated, 2016]. Available from: www.goldcopd.com | ||
Han MK, Agusti A, Calverley PM, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182(5):598–604. | ||
Rabe KF, Fabbri LM, Vogelmeier C, et al. Seasonal distribution of COPD exacerbations in the prevention of exacerbations with tiotropium in COPD trial. Chest. 2013;143(3):711–719. | ||
Hurst JR, Donaldson GC, Quint JK, Goldring JJ, Baghai-Ravary R, Wedzicha JA. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179(5):369–374. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. | ||
Kim V, Criner GJ. The chronic bronchitis phenotype in chronic obstructive pulmonary disease: features and implications. Curr Opin Pulm Med. 2015;21(2):133–141. | ||
Ramos FL, Krahnke JS, Kim V. Clinical issues of mucus accumulation in COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:139–150. | ||
Hogg JC, Chu FS, Tan WC, et al. Survival after lung volume reduction in chronic obstructive pulmonary disease: insights from small airway pathology. Am J Respir Crit Care Med. 2007;176(5):454–459. | ||
Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–2653. | ||
Vestbo J, Prescott E, Lange P. Association of chronic mucus hypersecretion with FEV1 decline and chronic obstructive pulmonary disease morbidity. Copenhagen City Heart Study Group. Am J Respir Crit Care Med. 1996;153(5):1530–1535. | ||
Pistelli R, Lange P, Miller D. Determinants of prognosis of COPD in the elderly: mucus hypersecretion, infections, cardiovascular comorbidity. Eur Respir J Suppl. 2003;21(40 suppl):10s–14s. | ||
Burgel PR, Nesme-Meyer P, Chanez P, et al. Cough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjects. Chest. 2009;135(4):975–982. | ||
Martinez FJ, Calverley PM, Goehring UM, Brose M, Fabbri LM, Rabe KF. Effect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy (REACT): a multicentre randomised controlled trial. Lancet. 2015;385(9971):857–866. | ||
Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish COPD Guidelines (GesEPOC): pharmacological treatment of stable COPD. Arch Bronconeumol. 2012;48(7):247–257. | ||
Han MK, Tayob N, Murray S, et al. Predictors of chronic obstructive pulmonary disease exacerbation reduction in response to daily azithromycin therapy. Am J Respir Crit Care Med. 2014;189(12):1503–1508. | ||
Vogelmeier C, Buhl R, Criee CP, et al. [Guidelines for the diagnosis and therapy of COPD issued by Deutsche Atemwegsliga and Deutsche Gesellschaft fur Pneumologie und Beatmungsmedizin]. Pneumologie. 2007;61(5):e1–e40. German. | ||
Zheng JP, Kang J, Huang SG, et al. Effect of carbocisteine on acute exacerbation of chronic obstructive pulmonary disease (PEACE Study): a randomised placebo-controlled study. Lancet. 2008;371(9629):2013–2018. | ||
Poole P, Chong J, Cates CJ. Mucolytic agents versus placebo for chronic bronchitis or chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;7:Cd001287. | ||
Beuscher N, Kietzmann M, Bien E, Champeroux P. Interference of myrtol standardized with inflammatory and allergic mediators. Arzneimittelforschung. 1998;48(10):985–989. | ||
Beuscher N, Bien E, Elstner E, Kietzmann M, Amon U. Myrtol standardized in treatment of sinusitis and bronchitis–Pharmacodynamics and pharmacokinetics. Z Phytotherapie Abstractband. 1997;8:9–10. | ||
Grassmann J, Hippeli S, Dornisch K, Rohnert U, Beuscher N, Elstner EF. Antioxidant properties of essential oils. Possible explanations for their anti-inflammatory effects. Arzneimittelforschung. 2000;50(2):135–139. | ||
App EM. Stellenwert der Mukusclearance für das Bronchialsystem – Pathophysiologie und therapeutische Ansätze. Entzündliche Erkrankungen des Bronchialsystems: Springer; 2000:27–53. | ||
Begrow F, Bockenholt C, Ehmen M, Wittig T, Verspohl EJ. Effect of myrtol standardized and other substances on the respiratory tract: ciliary beat frequency and mucociliary clearance as parameters. Adv Ther. 2012;29(4):350–358. | ||
Christoph F, Kaulfers PM, Stahl-Biskup E. In vitro evaluation of the antibacterial activity of beta-triketones admixed to Melaleuca oils. Planta Med. 2001;67(8):768–771. | ||
Lai Y, Dilidaer D, Chen B, et al. In vitro studies of a distillate of rectified essential oils on sinonasal components of mucociliary clearance. Am J Rhinolo Allergy. 2014;28(3):244–248. | ||
Cao L, Chen Y, Zhao Y, et al. Effect of myrtol standardized on mucus hypersecretion and clearance of Pseudomonas aeruginosa in a rat model of chronic obstructive pulmonary disease. Arzneimittelforschung. 2011;61(12):685–692. | ||
Ulmer W, Schött D. Chronisch-obstruktive Bronchitis. Wirkung von Gelomyrtol® forte in einer plazebokontrollierten Doppelblindstudie. Fortschr Med. 1991;109(27):547–550. German. | ||
Gillissen A, Wittig T, Ehmen M, Krezdorn H, de Mey C. A multi-centre, randomised, double-blind, placebo-controlled clinical trial on the efficacy and tolerability of GeloMyrtol® forte in acute bronchitis. Drug Res (Stuttg). 2013;63(01):19–27. | ||
Meister R, Wittig T, Beuscher N, de Mey C. Efficacy and tolerability of myrtol standardized in long-term treatment of chronic bronchitis. a double-blind, placebo-controlled study. Study Group Investigators. Arzneimittelforschung. 1999;49(4):351–358. | ||
Matthys H, de Mey C, Carls C, Rys A, Geib A, Wittig T. Efficacy and tolerability of myrtol standardized in acute bronchitis. a multi-centre, randomised, double-blind, placebo-controlled parallel group clinical trial versus cefuroxime and ambroxol. Arzneimittelforschung. 2000;50(8):700–711. | ||
WHO. Report of an expert committee: Definition and diagnosis of pulmonary disease with special reference to chronic bronchitis and emphysema. WHO Techn Rep Ser. 1961;213(1961):14–19. | ||
Santos S, Marin A, Serra-Batlles J, et al. Treatment of patients with COPD and recurrent exacerbations: the role of infection and inflammation. Int J Chron Obstruct Pulmon Dis. 2016;11:515–525. | ||
Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26. | ||
Vogelmeier C, Hederer B, Glaab T, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364(12):1093–1103. | ||
Molyneaux PL, Mallia P, Cox MJ, et al. Outgrowth of the bacterial airway microbiome after rhinovirus exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(10):1224–1231. | ||
Vestbo J, Lange P. Prevention of COPD exacerbations: medications and other controversies. ERJ Open Res. 2015;1(1):00011–2015. | ||
Seemungal T, Harper-Owen R, Bhowmik A, et al. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(9):1618–1623. | ||
Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117(6):1638–1645. | ||
Bafadhel M, McKenna S, Terry S, et al. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med. 2011;184(6):662–671. | ||
Wedzicha JA, Decramer M, Seemungal TA. The role of bronchodilator treatment in the prevention of exacerbations of COPD. Eur Respir J. 2012;40(6):1545–1554. | ||
Calverley PM, Rabe KF, Goehring U-M, Kristiansen S, Fabbri LM, Martinez FJ. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet. 2009;374(9691):685–694. | ||
Poole P, Black PN, Cates CJ. Mucolytic agents for chronic bronchitis or chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;8:CD001287. | ||
Society AT. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;152(5 Pt 2):S78–S121. | ||
Anthonisen N, Manfreda J, Warren C, Hershfield E, Harding G, Nelson N. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106(2):196–204. | ||
Effing TW, Kerstjens HA, Monninkhof EM, et al. Definitions of exacerbations: does it really matter in clinical trials on COPD? Chest. 2009;136(3):918–923. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.