Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Effect of COVID-19 and Face Masks on the Condition of Rosacea – A Retrospective Analysis of 87 Patients
Authors Zhang T , Liu X , Yang F , Xu Y , Jiang X
Received 5 July 2023
Accepted for publication 3 October 2023
Published 13 October 2023 Volume 2023:16 Pages 2855—2862
DOI https://doi.org/10.2147/CCID.S429099
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Anne-Claire Fougerousse
Ting Zhang,1,* Xu Liu,1,* Fengjuan Yang,1 Yuanyuan Xu,1 Xian Jiang1,2
1Department of Dermatology, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Laboratory of Dermatology, Clinical Institute of Inflammation and Immunology, Frontiers Science Center for Disease-Related Molecular Network, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xian Jiang, Department of Dermatology, West China Hospital, Sichuan University, #37 Guoxue Alley, Wuhou District, Chengdu, Sichuan, 610041, People’s Republic of China, Tel +86-28-85423315, Fax +86-28-85422560, Email [email protected]
Introduction: The pathogenesis of COVID-19 includes systemic immune activation and endothelial dysfunction, which is closely related to the pathogenesis of rosacea. In order to investigate the influence of COVID-19 infection on the condition of rosacea patients, we retrospectively investigated the impact of COVID-19 infection and COVID-19-related masks on rosacea patients.
Methods: We collected the basic information from rosacea patients who had a long-term follow-up at West China Hospital of Sichuan University. Between January 2023 and March 2023, we recruited 87 rosacea patients for this survey.
Results: Our results showed that COVID-19 infection could aggravate the condition of rosacea patients, and the change in the symptoms was not related to fever, temperature, antipyretics use, and vaccination. In addition, we observed a significant association between the type of mask worn by rosacea patients and exacerbation, while the duration of mask usage did not exhibit a similar relationship.
Discussion: Considering the ongoing global utilization of masks due to the COVID-19 pandemic and the possible recurrence of COVID-19 infection, dermatologists should monitor the condition of rosacea patients infected with COVID-19 and adjust the treatment regimens accordingly.
Keywords: SARS-CoV-2, COVID-19 infection, rosacea, mask
Introduction
In late December 2019, an outbreak of unidentified pneumonia originated in Wuhan, China. The pathogen was isolated and identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), leading to Coronavirus Disease 2019 (COVID-19). Since the outbreak of the COVID-19 pandemic, understanding of COVID-19 symptoms has been progressively expanding. COVID-19 infection was initially described as a respiratory infection, which can cause severe pneumonia. However, as the number of clinical cases increases, it has been found that patients with COVID-19 also exhibit structural and functional impairments extending to various organs, including the skin.1,2 There are many mechanisms underlying the pathogenesis of COVID-19, encompassing systemic immune activation and endothelial dysfunction.3–5 Notably, patients afflicted with COVID-19 have been found to exhibit significantly elevated plasma concentrations of various proinflammatory cytokines, including interferon γ, tumor necrosis factor, Interleukin-6 (IL-6), IL-1β, IL-2, and IL-17A.6 Moreover, prior investigations have substantiated that COVID-19 can directly bind to angiotensin-converting enzyme 2 (ACE2) in vascular endothelial cells, causing endothelial damage and dysfunction.7–9
Rosacea is a common chronic inflammatory skin disease, affecting 3% of people over 30. It is characterized by frequent facial flushing, facial erythema, papules and telangiectasia.10,11 The exact etiology of rosacea is unknown, and it has been suggested that the pathogenesis of rosacea appears to be multifactorial.12,13 It may contain genetic components, innate immune system disorder, dysfunction of facial vascular regulation, neurogenic inflammation, skin barrier destruction, and increased Demodex level.14–16 The chitin released by the demodex can trigger an inflammatory response in keratinocytes through the TLR-2 pathway, which enhances the expression of IL-8, IL-1β, and TNF-α.17,18 IL-1β and TNF-α are additional angiogenic factors, which might cause vascular hyper-reactivity in rosacea.19 In addition, previous studies have found that IFN-γ and IL-17A are involved in the pathogenesis of rosacea.20 IL-17 has been proven to induce angiogenesis through VEGF and affect LL-37 expression.19 LL-37 can affect various processes, including immune modulation, neutrophil chemotaxis, and the induction of cytokine and chemokine release from mast cells, enhancing the expression of IL-1, IL-6, and MMP-9, thereby enhancing the inflammatory response to rosacea.21–23 On the other hand, LL-37 can affect angiogenesis by enhancing the proliferation of endothelial cells.24
As mentioned above, COVID-19 can cause systemic immune activation and endothelial dysfunction, which is related to the pathogenesis of rosacea. Nevertheless, our understanding of the specific influence of COVID-19 on rosacea remains limited. Consequently, we retrospectively investigated the impact of COVID-19 infection and COVID-19-related masks usage on rosacea patients.
Materials and Methods
Survey Subjects
In this study, patients with rosacea who had a long-term follow-up at West China Hospital of Sichuan University were enrolled as the subjects. Inclusion criteria include a) patients diagnosed with rosacea, b) being able to complete the questionnaire independently, and c) voluntary participation and informed consent. Conversely, exclusion criteria comprised patients with neurological or psychiatric disorders, unconsciousness, or communication impairments. The survey period spanned January 2023 to March 2023.
Survey Methods
In order to prevent the potential COVID-19 spread between respondents and investigators, all surveys were conducted by electronic questionnaires. Prior to conducting the survey, patients were informed of the purpose of the survey, and their informed consent was obtained. We informed every patient about the precautions for completing the questionnaires and explained the requirements for questionnaire completion under a uniform guideline to ensure consistency across responses.
Survey Content
The study collected basic information on rosacea patients, encompassing demographic characteristics, rosacea history, COVID-19 infection history, and mask use. The rosacea history comprises medical history, severity assessment of the condition, and treatment options. As for COVID-19 infection history, it encompassed relevant parameters such as infection status (presence or absence), infection duration, symptomatic manifestations, treatment approaches, and the consequential impact of COVID-19 infection on rosacea. Additionally, the use of masks includes the type of mask, the average duration of mask use per day, and the subsequent impact of mask use on rosacea.
Statistical Methods
IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY, USA) was used to analyze the data. The statistical descriptions of enumeration data were represented as numbers (percentage), while the statistical descriptions of measurement data were expressed as mean ± standard deviation. The Chi-square test was used for categorical variables, and the t-test was used for measurement data conformed to normal distribution. The difference was considered statistically significant at P < 0.05.
Results
A total of 121 questionnaires were collected in this study, with 87 valid questionnaires and a response rate of 71.90%. All patients were diagnosed with rosacea in the hospital. The mean age of the participants was 36.0 ± 10.8 years, comprising one male respondent (1.15%) and 86 female respondents (98.85%). The median duration of rosacea was 3 (2, 4) years. Furthermore, the distribution of rosacea severity within the studied population indicated that 18 cases were classified as mild (20.69%), 52 cases were classified as moderate (59.77%), and 17 cases were classified as severe (19.54%).
The treatment regimen for these patients was dominated by the use of phototherapy plus sonophoresis therapy in 52 cases (59.77%), minocycline in 33 cases (37.93%), hydroxychloroquine in 32 cases (36.78%), doxycycline in 23 cases (26.44%), compound glycyrrhizin in 27 cases (31.03%), antihistamines in 19 cases (21.84%), pregabalin in 15 cases (17.24%), alprazolam in 11 cases (12.64%), sodium bromide in 11 cases (12.64%), and untreated in 5 cases (5.75%). Among the cohort, a total of 55 patients with rosacea had redness and burning sensations in the ear, of which 25 patients (45.45%) reported symptoms lasting less than 1 hour per day, 26 patients (47.27%) had symptoms lasting 1 to 3 hours per day, 1 patient (1.82%) each had symptoms lasting 3 to 5 hours per day and 5 to 8 hours per day, and 2 patients (3.64%) had symptoms lasting more than 8 hours per day.
Regarding COVID-19 infection, a notable proportion of rosacea patients, specifically 73 cases (83.91%), were found to have contracted the virus, while 14 cases (16.09%) remained uninfected. A total of 33 patients (45.20%) infected with COVID-19 were confirmed by self-purchased antigen reagent, 20 patients (27.40%) were confirmed by nucleic acid detection, and 20 patients (27.40%) were not detected but thought to be infected with COVID-19 (Figure 1A). A total of 14 cases (19.18%) were infected with COVID-19 for 1 to 3 days, 16 cases (21.92%) for 4 to 6 days, 22 cases (30.14%) for 7 to 9 days, and 11 cases (15.06%) for more than 9 days. The symptoms of patients with COVID-19 infection were mainly fever, with a total of 48 cases (65.75%), and the average temperature of patients with fever was 38.6 ± 0.7°C. There were 35 cases (47.95%) of malaise, 35 cases (47.95%) of dry cough, 27 cases (36.99%) of runny nose and nasal congestion, 26 cases (35.62%) of sore throat, 19 cases (26.03%) of abnormal smell and taste, 11 cases (15.07%) of nausea and vomiting, 9 cases (12.33%) of chest tightness, 8 (10.96%) cases of dyspnea, 6 cases (8.21%) of abdominal pain and diarrhea, and 4 (5.48%) cases of other symptoms (Figure 1B). The treatment of COVID-19 infection was mainly antipyretics in 43 cases (58.90%). A total of 17 patients (23.29%) took non-antipyretic drugs, 3 patients (4.11%) were hospitalized in the general ward, and 11 patients (15.07%) had no treatment.
 |
Figure 1 (A) The number of patients with rosacea infected with COVID-19. (B) The post-infection symptoms of patients with rosacea infected with COVID-19. |
Among 73 rosacea patients infected with COVID-19, 25 (34.25%) had exacerbations. Among the 25 patients, 22 of them experienced exacerbations without any change in the treatment regimen. The exacerbation of the disease was mainly reflected in 23 cases (92.00%) of facial flushing, 17 cases (68.00%) of facial burning sensation, 14 cases (56.00%) of telangiectasia, 14 cases (56.00%) of persistent facial erythema and 7 cases (28.00%) of facial itching. Among 73 rosacea patients infected with COVID-19, 45 patients (61.64%) had a treatment regimen that had no effect, and 3 patients (4.11%) had remission. Nine patients (12.33%) changed their treatment during COVID-19 infection. Furthermore, infection with COVID-19 had a psychological impact on 18 patients (24.66%).
This study also studied the relationship between the changes in symptoms in rosacea patients after infection with COVID-19 and fever, usage of antipyretic drugs, vaccination, type of mask, and duration of mask usage. As shown in Table 1, the changes in symptoms in rosacea patients after COVID-19 infection were unrelated to fever, antipyretics usage, and vaccination (P>0.05).
 |
Table 1 Changes of Rosacea Patients Infected with COVID-19 |
During the COVID-19 pandemic, masks aggravated the condition of 53 patients (72. 60%), mainly manifested in 51 patients (98. 08%) experiencing aggravated facial flushing, 24 patients (45. 28%) experiencing aggravated facial erythema, 23 patients (43. 40%) experiencing aggravated facial burning sensation, and 16 patients (30. 19%) experiencing aggravated papules and pustules. The type of mask worn by patients was related to the exacerbation of rosacea (χ 2 = 7. 145, P = 0. 025), while the duration of mask usage was not associated with the exacerbation of rosacea (χ 2 = 0. 013, P = 0. 908) (Table 2). The details are shown in Figure 2.
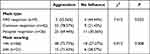 |
Table 2 The Relationship Between Mask Use and Disease Change in Rosacea Patients |
 |
Figure 2 The relationship between mask usage and disease change in rosacea patients. |
Discussion
To our knowledge, this is the first study to investigate the effect of COVID-19 infection on individuals with rosacea. Notably, our investigation revealed that 34.25% of rosacea patients had exacerbations subsequent to contracting COVID-19. We also found that the changes in symptoms of rosacea patients following COVID-19 infection were unrelated to fever, antipyretics usage, and vaccination status. In addition, we conducted an in-depth exploration of the correlation between the type of mask worn by rosacea patients and the duration of mask usage, and the rosacea exacerbation. However, our results found that the type of mask worn by rosacea patients was related to the exacerbation of rosacea, while the duration of mask usage was not associated with the exacerbation of rosacea.
Our findings indicate that 34.25% of rosacea patients experienced exacerbation after COVID-19 infection. The aggravation primarily manifested as the aggravation of facial flushing (92.00%), facial burning sensation (68.00%), telangiectasia (56.00%), persistent facial erythema (56.00%) and facial itching (28.00%). Indeed, previous studies have documented a case study delineating amelioration in rosacea subsequent to acyclovir intervention for herpes simplex type 1 manifestations.25 Moreover, Sezer et al expounded upon a Wolf’s isotopic response, wherein rosacea manifested at the site of healed herpes zoster.26 Concomitantly, instances of rosacea post HIV infection have been documented. These observations posit a potential linkage between rosacea and viral infections.27,28 Previous studies have hypothesized that viral IgM and IgG can cross-react with mast cell IgE, subsequently triggering degranulation of mast cells.29 It has been documented that SARS CoV-2 specific IgM and IgG can be detected in affected patients.30 Consequently, we speculated that the cross-reaction between the SARS CoV-2 antibody and mast cell IgE might lead to mast cell degranulation.31 In addition, significantly elevated plasma concentrations of pro-inflammatory cytokines, such as interferon γ, tumor necrosis factor, IL-6, IL-1β, IL-2, and IL-17A, were reported in patients with COVID-19.6 These inflammatory mediators, along with the release of inflammatory factors from mast cell degranulation, can serve as endogenous vasoactive agents, inducing superficial vasodilation and resulting in facial flushing. Repeated flushing can lead to the development of persistent facial erythema, accompanied by telangiectasia. Additionally, it should be noted that the administration of nonsteroidal anti-inflammatory drugs in rosacea patients following COVID-19 infection may also provoke flushing.32,33 The facial itching symptoms can also be attributed to the release of various itch-inducing molecules or pruritogens triggered by mast cell degranulation.34
Unexpectedly, our research revealed no significant correlation between the alteration of symptoms in rosacea patients following COVID-19 infection and factors such as fever, body temperature, antipyretics usage, and vaccination. We speculate that this may be attributed to the patients’ adherence to their established treatment regimens even during the course of COVID-19 infection. It is plausible that this ongoing treatment may have prevented exacerbation of rosacea, thereby obscuring the potential impact of fever, body temperature, antipyretics usage, and vaccination on rosacea outcomes subsequent to COVID-19 infection.
A previous research conducted by Damiani et al has indicated that wearing masks has the potential to exacerbate rosacea.35 However, it has been noted that the duration of mask usage was not associated with exacerbation. Our study further investigated the impact of masks on rosacea patients while considering their adherence to prior treatment protocols. Interestingly, our results also showed that the duration of mask usage was not associated with exacerbations but the type of mask was associated with exacerbations. Our research aligns with previous research findings,36–38 but contradicts the observations from Yaqoob et al, in which there is no association between the frequency and duration of mask usage and skin symptoms.39 Notably, during the prevalence of COVID-19, wearing masks exacerbated symptoms in 72.60% of rosacea patients. The aggravation primarily reflected in the aggravation of facial flushing (98.08%), facial erythema (45.28%), facial burning sensation (43.40%), and papules and pustules (30.19%). Previous studies have revealed that masks can induce changes in the skin microenvironment through dehydration, increased sebum, and elevated pH levels.40 Dehydration and sebum imbalance can promote the proliferation of Propionibacterium acnes, triggering innate immune responses and inflammatory lesions such as papules and pustules.41 In addition, increased sebum and inflammatory skin lesions can facilitate the colonization of Demodex folliculorum, thereby promoting the development of rosacea.17,42
Our study also has some limitations. Firstly, the sample size of patients in our analysis is relatively small, which warrants further verification in a more extensive data set. Secondly, our research was carried out via an electronic questionnaire survey, lacking data such as VISIA results of rosacea patients.
Conclusion
In conclusion, this retrospective study showed that COVID-19 infection could aggravate the condition of rosacea patients, and the change in the symptoms was not related to fever, temperature, antipyretics usage, and vaccination. In addition, we observed a significant association between the type of mask worn by rosacea patients and exacerbation, while the duration of mask usage did not exhibit a similar relationship. Considering the ongoing global utilization of masks due to the COVID-19 pandemic, as well as the likelihood of rosacea patients experiencing repeated infections, it is advisable for dermatologists to remain vigilant in monitoring rosacea patients with COVID-19 infections and adjusting treatment regimens accordingly. Additional interventions may be incorporated, including the utilization of ivermectin, minocycline, or doxycycline.43,44 In addition, further understanding of the pathophysiological mechanisms underlying the effects of COVID-19 infection and mask usage on rosacea patients is needed in the future to evaluate the best treatment to counteract the pro-inflammatory effects of COVID-19 infection and masks.
Ethics Approval and Consent for Publication
The patients described in this manuscript gave informed consent to the publication of their case details. The research was conducted in accordance with the ethical guidelines outlined in the Declaration of Helsinki and was approved by the Medical Ethics Committee of the West China Hospital of Sichuan University (approval number: 2019-248).
Acknowledgments
There are no acknowledgments.
Funding
This study was supported by the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYJC21036) and the National Natural Science Foundation of China (82073473) and the National Natural Science Foundation of China (82273559).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–875. doi:10.1016/j.dsx.2021.04.007
2. Wollina U, Karadağ AS, Rowland-Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID-19 patients: a review. Dermatol Ther. 2020;33(5):e13549. doi:10.1111/dth.13549
3. Rudnicka L, Glowacka P, Goldust M, et al. Cyclosporine therapy during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(2):e151–e152. doi:10.1016/j.jaad.2020.04.153
4. Tufan A, Avanoğlu Güler A, Matucci-Cerinic M. COVID-19, immune system response, hyperinflammation and repurposing antirheumatic drugs. Turkish J Med Dci. 2020;50(Si–1):620–632. doi:10.3906/sag-2004-168
5. Nägele MP, Haubner B, Tanner FC, Ruschitzka F, Flammer AJ. Endothelial dysfunction in COVID-19: current findings and therapeutic implications. Atherosclerosis. 2020;314:58–62. doi:10.1016/j.atherosclerosis.2020.10.014
6. Zhong J, Tang J, Ye C, Dong L. The immunology of COVID-19: is immune modulation an option for treatment? Lancet Rheumatol. 2020;2(7):e428–e436. doi:10.1016/S2665-9913(20)30120-X
7. Monteil V, Kwon H, Prado P, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181(4):905–913.e907. doi:10.1016/j.cell.2020.04.004
8. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi:10.1002/path.1570
9. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi:10.1016/S0140-6736(20)30937-5
10. Yamasaki K, Kanada K, Macleod DT, et al. TLR2 expression is increased in rosacea and stimulates enhanced serine protease production by keratinocytes. J Invest Dermatol. 2011;131(3):688–697. doi:10.1038/jid.2010.351
11. Xie HF, Huang YX, He L, et al. An observational descriptive survey of rosacea in the Chinese population: clinical features based on the affected locations. PeerJ. 2017;5:e3527. doi:10.7717/peerj.3527
12. Woo YR, Lim JH, Cho DH, Park HJ. Rosacea: molecular mechanisms and management of a chronic cutaneous inflammatory condition. Int J Mol Sci. 2016;17(9):1562. doi:10.3390/ijms17091562
13. Jeon HW, Na EY, Yun SJ, Lee SC, Lee JB. Citron essential oils alleviate the mediators related to rosacea pathophysiology in epidermal keratinocytes. Ann Dermatol. 2018;30(6):653–661. doi:10.5021/ad.2018.30.6.653
14. Steinhoff M, Buddenkotte J, Aubert J, et al. Clinical, cellular, and molecular aspects in the pathophysiology of rosacea. J Invest Dermatol Sympos Proce. 2011;15(1):2–11. doi:10.1038/jidsymp.2011.7
15. Addor FA. Skin barrier in rosacea. An Bras Dermatol. 2016;91(1):59–63. doi:10.1590/abd1806-4841.20163541
16. Roihu T, Kariniemi AL. Demodex mites in acne rosacea. J Cutan Pathol. 1998;25(10):550–552. doi:10.1111/j.1600-0560.1998.tb01739.x
17. Casas C, Paul C, Lahfa M, et al. Quantification of Demodex folliculorum by PCR in rosacea and its relationship to skin innate immune activation. Exp Dermatol. 2012;21(12):906–910. doi:10.1111/exd.12030
18. Turgut Erdemir A, Gurel MS, Koku Aksu AE, Falay T, Inan Yuksel E, Sarikaya E. Demodex mites in acne rosacea: reflectance confocal microscopic study. Australas J Dermatol. 2017;58(2):e26–e30. doi:10.1111/ajd.12452
19. Gerber PA, Buhren BA, Steinhoff M, Homey B. Rosacea: the cytokine and chemokine network. J Invest Dermatol Sympos Proce. 2011;15(1):40–47. doi:10.1038/jidsymp.2011.9
20. Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135(9):2198–2208. doi:10.1038/jid.2015.141
21. Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Invest Dermatol Sympos Proce. 2011;15(1):12–15. doi:10.1038/jidsymp.2011.4
22. Zheng Y, Niyonsaba F, Ushio H, et al. Cathelicidin LL-37 induces the generation of reactive oxygen species and release of human alpha-defensins from neutrophils. Br J Dermatol. 2007;157(6):1124–1131. doi:10.1111/j.1365-2133.2007.08196.x
23. Muto Y, Wang Z, Vanderberghe M, Two A, Gallo RL, Di Nardo A. Mast cells are key mediators of cathelicidin-initiated skin inflammation in rosacea. J Invest Dermatol. 2014;134(11):2728–2736. doi:10.1038/jid.2014.222
24. Schwab VD, Sulk M, Seeliger S, et al. Neurovascular and neuroimmune aspects in the pathophysiology of rosacea. J Invest Dermatol Sympos Proce. 2011;15(1):53–62. doi:10.1038/jidsymp.2011.6
25. Badieyan ZS, Hoseini SS. Improvement of rosacea during acyclovir treatment: a case report. Am J Clin Dermatol. 2017;18(6):845–846. doi:10.1007/s40257-017-0315-8
26. Sezer E, Koseoglu RD, Filiz N. Wolf’s isotopic response: rosacea appearing at the site of healed herpes zoster. Australas J Dermatol. 2006;47(3):189–191. doi:10.1111/j.1440-0960.2006.00270.x
27. Vin-Christian K, Maurer TA, Berger TG. Acne rosacea as a cutaneous manifestation of HIV infection. J Am Acad Dermatol. 1994;30(1):139–140. doi:10.1016/S0190-9622(08)81905-6
28. Yamaoka T, Murota H, Tani M, Katayama I. Severe rosacea with prominent Demodex folliculorum in a patient with HIV. J Dermatol. 2014;41(2):195–196. doi:10.1111/1346-8138.12352
29. Imbalzano E, Casciaro M, Quartuccio S, et al. Association between urticaria and virus infections: a systematic review. Allergy Asthma Proce. 2016;37(1):18–22. doi:10.2500/aap.2016.37.3915
30. Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20(5):269–270. doi:10.1038/s41577-020-0308-3
31. Meixiong J, Anderson M, Limjunyawong N, et al. Activation of mast-cell-expressed mas-related G-protein-coupled receptors drives non-histaminergic itch. Immunity. 2019;50(5):1163–1171.e1165. doi:10.1016/j.immuni.2019.03.013
32. Lafont E, Sokol H, Sarre-Annweiler ME, et al. Étiologies et orientation diagnostique devant un flush [Causes and differential diagnosis of flush]. La Revue de medecine interne. 2014;35(5):303–309. French. doi:10.1016/j.revmed.2013.08.015
33. Ray D, Williams G. Pathophysiological causes and clinical significance of flushing. Br J Hosp Med. 1993;50(10):594–598.
34. Yang TB, Kim BS. Pruritus in allergy and immunology. J Allergy Clin Immunol. 2019;144(2):353–360. doi:10.1016/j.jaci.2019.06.016
35. Damiani G, Gironi LC, Grada A, et al. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): multi-center, real-life, telemedical, and observational prospective study. Dermatol Ther. 2021;34(2):e14848. doi:10.1111/dth.14848
36. Lan J, Song Z, Miao X, et al. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215–1216. doi:10.1016/j.jaad.2020.03.014
37. Szepietowski JC, Matusiak Ł, Szepietowska M, Krajewski PK, Białynicki-Birula R. Face mask-induced itch: a self-questionnaire study of 2315 responders during the COVID-19 pandemic. Acta Derm Venereol. 2020;100(10):adv00152. doi:10.2340/00015555-3536
38. Zuo Y, Hua W, Luo Y, Li L. Skin reactions of N95 masks and medial masks among health-care personnel: a self-report questionnaire survey in China. Contact Dermatitis. 2020;83(2):145–147. doi:10.1111/cod.13555
39. Yaqoob S, Saleem A, Jarullah FA, Asif A, Essar MY, Emad S. Association of acne with face mask in healthcare workers amidst the COVID-19 outbreak in Karachi, Pakistan. Clin Cosmet Investig Dermatol. 2021;14:1427–1433. doi:10.2147/CCID.S333221
40. Hua W, Zuo Y, Wan R, et al. Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermatitis. 2020;83(2):115–121. doi:10.1111/cod.13601
41. Jusuf NK, Putra IB, Sari L. Differences of microbiomes found in non-inflammatory and inflammatory lesions of acne vulgaris. Clin Cosmet Investig Dermatol. 2020;13:773–780. doi:10.2147/CCID.S272334
42. Moran EM, Foley R, Powell FC. Demodex and rosacea revisited. Clin Dermatol. 2017;35(2):195–200. doi:10.1016/j.clindermatol.2016.10.014
43. Trave I, Micalizzi C, Cozzani E, Gasparini G, Parodi A. Papulopustular rosacea treated with ivermectin 1% cream: remission of the demodex mite infestation over time and evaluation of clinical relapses. Dermat Pract Concept. 2022;12(4):e2022201. doi:10.5826/dpc.1204a201
44. van Zuuren EJ, Arents BWM, van der Linden MMD, Vermeulen S, Fedorowicz Z, Tan J. Rosacea: new concepts in classification and treatment. Am J Clin Dermatol. 2021;22(4):457–465. doi:10.1007/s40257-021-00595-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
