Back to Journals » Clinical Interventions in Aging » Volume 19
Effect of Continuous Positive Airway Pressure on Incident Frailty in Elderly Patients with Obstructive Sleep Apnea: A Study Based on Propensity Score Matching
Authors Xue X, Zhao LB, Zhao Z , Xu WH, Cai WM, Chen SH, Li TJ, Nie TY, Rui D, Qian XS, Liu L
Received 1 November 2023
Accepted for publication 4 February 2024
Published 16 February 2024 Volume 2024:19 Pages 255—263
DOI https://doi.org/10.2147/CIA.S446129
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Xin Xue,1,2 Li-Bo Zhao,3 Zhe Zhao,3 Wei-Hao Xu,4 Wei-Meng Cai,1 Shao-Hua Chen,1 Tian-Jiao Li,5 Ting-Yu Nie,5 Dong Rui,1 Xiao-Shun Qian,1 Lin Liu1
1Department of Pulmonary and Critical Care Medicine, Second Medical Center of Chinese PLA General Hospital, Beijing, People’s Republic of China; 2National Clinical Research Center for Geriatric Diseases, Chinese PLA General Hospital, Beijing, People’s Republic of China; 3Department of Vasculocardiology, Second Medical Center of Chinese PLA General Hospital, Beijing, People’s Republic of China; 4Department of Geriatrics, Guangdong Provincial Geriatrics Institute, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Southern Medical University, Guangzhou, People’s Republic of China; 5Medical College, Yan’ an University, Yan’ an, People’s Republic of China
Correspondence: Lin Liu; Xiao-Shun Qian, Department of Pulmonary and Critical Care Medicine, Second Medical Center of Chinese PLA General Hospital, Beijing, People’s Republic of China, Tel +86 132 6318 9578 ; +86 135 2127 9287, Email [email protected]; [email protected]
Background: The concomitant rise in the prevalence of obstructive sleep apnea (OSA) and frailty among the elderly population has been linked to an increase in mortality rates. Despite continuous positive airway pressure (CPAP) being the gold standard treatment for OSA, its impact on incident frailty remains inadequately explored.
Methods: In this cohort study, we analyzed data from 1290 patients diagnosed with OSA, aged 60 years and older. A subset of 71 patients who demonstrated high adherence to CPAP therapy were categorized as the CPAP group. Propensity score matching (PSM) was employed at a 1:4 ratio, matching for variables such as age, gender, body mass index (BMI), and sleep apnea-hypopnea index (AHI), to establish a non-CPAP group for comparison. The FRAIL scale was utilized to evaluate the frailty status of participants. Logistic regression analysis examined the relationship between CPAP therapy and incident frailty, as well as its individual components, in elderly patients with OSA.
Results: During a median follow-up period of 52 months, incident frailty was observed in 70 patients (19.7%). Patients with OSA receiving CPAP therapy exhibited a lower incidence of frailty compared to those not receiving CPAP (11.26% vs 21.83%, P=0.045). In the multivariate model, CPAP therapy was significantly correlated with a reduced risk of incident frailty (OR = 0.36, 95% CI, 0.15– 0.88; P = 0.025). Subcomponent analyses revealed that CPAP was associated with a lower risk of fatigue (OR=0.35, 95% CI, 0.19– 0.63; P < 0.001), resistance (OR = 0.32, 95% CI, 0.14– 0.74; P=0.008), and weight loss (OR = 0.38, 95% CI, 0.19– 0.75; P = 0.007).
Conclusion: CPAP therapy was associated with a reduced risk of incident frailty among elderly patients with OSA.
Keywords: obstructive sleep apnea, frailty, continuous positive airway pressure, elderly
Introduction
Obstructive sleep apnea (OSA) poses substantial health risks, particularly for the aging population.1 The condition leads to acute physiological disturbances such as intermittent hypoxia, sleep fragmentation, and variable heart rate, blood pressure, and intrathoracic pressure.2 Over time, these acute disturbances may evolve into chronic conditions, including hypertension, cardiovascular diseases,3 cognitive decline,4 impaired mood and quality of life,5 and even premature death.6
Frailty is an emerging public health issue with significant implications for clinical practice.7 As the aging population continues to grow, the prevalence of frailty is projected to rise.8 Geriatricians define frailty as a biologic syndrome of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiologic systems, and causing vulnerability to adverse outcomes. Those with frailty are at an elevated risk for adverse events such as falls, hospital admissions, and mortality.9–12
While numerous studies have separately investigated the risk factors for OSA and frailty,13–15 the gold standard treatment for OSA—continuous positive airway pressure (CPAP)—has not been examined for its potential impact on frailty. CPAP has been shown to substantially improve the quality of life in individuals with OSA.16 This study aims to explore whether CPAP therapy can mitigate the onset of frailty in patients with OSA, thereby offering valuable insights for personalized intervention strategies aimed at ameliorating frailty and enhancing quality of life.
Methods
Study Design and Participants
This study employed a multicenter cohort design, enrolling 1290 elderly patients aged 60 years and older with a confirmed diagnosis of OSA as assessed by PSG. Participants were recruited from several institutions: PLA General Hospital, the Affiliated Hospital of Gansu University of Traditional Chinese Medicine, Peking University People’s Hospital, Peking University International Hospital, Beijing Chaoyang Hospital, and the 960th Hospital of PLA. The recruitment period spanned from January 2015 to October 2017. At the beginning of the follow-up stage, we first identified 86 patients with high adherence to CPAP therapy (defined as a minimum of four hours of CPAP use per night for at least 70% of the treatment duration) and another with 344 patients who either did not undergo CPAP therapy or exhibited low adherence following PSM. During the entire follow-up, 15 patients in the CPAP group were excluded due to their insufficient adherence to CPAP therapy on two consecutive occasions, while 60 matched patients from the non-CPAP group were also excluded. Ultimately, we identified 71 cases in the CPAP group as well as 284 cases in the non-CPAP group. These cohorts were matched for age, gender, BMI, and AHI. The study methodology is outlined in Figure 1. The inclusion criteria specified individuals aged 60 years and older with OSA. After applying the exclusion criteria, 355 participants were included in the final analysis. Exclusion criteria were as follows: 1) a diagnosis of frailty based on one or more criteria from the FRAIL scale; 2) presence of Parkinson’s disease, stroke, or mental disorders that could interfere with frailty assessment; and 3) loss to follow-up or death (Figure 1).
 |
Figure 1 Study flowchart. Abbreviations: CPAP, continuous positive airway pressure; BMI, body mass index; AHI, apnea-hypopnea index. |
The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of the PLA General Hospital (S2022-366-01), and informed consent was obtained from all participants prior to study commencement.
Diagnosis of OSA
Portable laboratory-based polysomnography (PSG) serves as the gold standard for OSA diagnosis. In this study, each participant underwent a comprehensive PSG assessment conducted in the sleep laboratories of affiliated hospitals. OSA diagnosis and sleep tests were first scored according to the Guideline of the American Academy of Sleep Medicine (2012). Data collection was facilitated using the Compumedics system, a technology originating from Melbourne, Australia. This evaluation encompassed a wide array of sleep metrics, including electroencephalography, electrooculography, electrocardiography, nasal-oral airflow, thoracic and abdominal movements, oxygen saturation (SpO2), and body orientation. Data were subjected to automatic computer analysis followed by manual correction by two sleep technologists and a senior physician. OSA was defined as AHI ≥5 events/hour. AHI was calculated as the total number of apnea and hypopnea events divided by the sleep duration (in hours). The severity of OSA was stratified into mild (AHI 5–15), moderate (AHI 15–30), and severe (AHI ≥30) based on PSG findings.17
Diagnosis of Frailty
The assessment of frailty was conducted using the FRAIL scale, which consists of five criteria: (1) fatigue, measured by asking respondents how much time during the past 4 weeks they felt tired; (2) resistance difficulty, indicated by challenges in ascending a 10-step staircase; (3) reduced ambulatory ability, demonstrated by an incapacity to walk one block (several hundred yards); (4) presence of multiple comorbidities, specified as having five or more from a list including hypertension, diabetes, cancer (excluding minor skin cancer), chronic lung disease, myocardial infarction, congestive heart failure, angina, asthma, arthritis, stroke, and kidney disease; and (5) unintentional weight loss, defined as a decrease exceeding 5.0% within the past year. Participants were categorized as frail if they met three or more criteria, pre-frail if they met fewer than three, and non-frail if they met none. For the aims of this study, participants who met three or more criteria were classified as frail, while those meeting 0–2 criteria were considered non-frail.18
Demographic and Clinical Characteristics
Baseline demographic variables included age, sex, smoking status (categorized as regular smoker, occasional smoker, or non-smoker), and drinking status (defined as drinking or not drinking in the past 30 days). BMI was computed using the formula: body weight (in kilograms) divided by the square of height (in meters). These demographic variables were collected through face-to-face interviews. Information on specific chronic diseases, such as hypertension, diabetes, and hyperlipidemia, was obtained from the participants as well as their spouses and children and was further verified by a comprehensive review of medical records.
Follow-Up
The follow-up phase began after the comprehensive collection of validated data and was initiated by diagnosing OSA in study participants via PSG. Our research team underwent specialized training to conduct follow-up activities through telephone, WeChat, and in-person hospital visits. During the initial stage of follow-up, we separated patients into two groups: those with high CPAP compliance and those with poor compliance or refusal of CPAP. We then matched patients with high CPAP compliance using PSM. In the subsequent stage, we evaluated patients’ frailty using various communication methods, including telephone and WeChat, based on the frailty questionnaire proposed by Morley et al, which is also endorsed by Chinese experts.18 All patients were evaluated at 1 month, 3 months, 6 months, 12 months and then every 6 months thereafter (at least 3 months and up to 1 years), with an average follow-up duration of 52 months. Patients unable to provide information during the follow-up were considered lost to follow-up. The follow-up period concluded in December 2022.
Statistical Analysis
Propensity score matching (PSM) was performed using R software (version 4.2.1). In order to generate the PSM, three frailty-associated confounders (age, sex and BMI) and one OSA-associated confounder (AHI) were considered. We matched each patient in the non-CPAP group to a counterpart in the CPAP group based on the closest propensity score, utilizing a nearest-neighbor matching algorithm. The specific instructions for the matching procedure were as follows: matching = matchit (CPAP ~ age + sex + BMI + AHI, data = a, method = “nearest”, ratio = 4). Statistical analyses were conducted using SPSS 25.0 statistical software (version 25.0, SPSS Inc., Chicago, Illinois, USA). Initially, tests for normality and variance homogeneity were performed. Data that followed a normal distribution were presented as mean ± standard deviations and subjected to t-test analysis. Non-normally distributed data were displayed as quartiles [M(P25, P75)]. Categorical data were expressed as proportions and analyzed using the chi-square test. Logistic analyses were used to determine the risk factors linked to frailty and the association between CPAP therapy and frailty components, with a statistical significance threshold set at P < 0.05.
Results
Baseline Characteristics
A total of 1290 elderly patients diagnosed with OSA were initially screened for inclusion in this study. The mean duration of follow-up was 52 months. After applying matching criteria based on age, gender, BMI, and AHI, 335 of these patients were ultimately included in either the CPAP or non-CPAP treatment groups (Figure 1). Table 1 provides a comprehensive comparison of baseline characteristics between the two groups. There is marginally significant between the smoking status (11.26% vs 21.21%, P = 0.059) and drinking status (2.81% vs 9.85%, P = 0.056) between the CPAP-treated and non-CPAP-treated cohorts.
 |
Table 1 Baseline Characteristics of Research Subjects |
Association Between CPAP Therapy and Frailty Incidence in Patients with OSA
Our data indicate that OSA patients receiving CPAP treatment exhibited a significantly reduced incidence of frailty compared to those not receiving CPAP treatment (11.26% vs 21.83%, P = 0.045, Figure 2). Further analysis using an unadjusted logistic regression revealed that CPAP treatment was significantly associated with a reduced risk of developing individual components of frailty. Specifically, the OR for experiencing fatigue was 0.35 (95% CI, 0.19–0.63; P < 0.001), for resistance was 0.32 (95% CI, 0.14–0.74; P = 0.008), and for unintentional weight loss was 0.38 (95% CI, 0.19–0.75; P = 0.007, Table 2).
 |
Table 2 Association Between CPAP Therapy and Incidence of Frailty Components |
 |
Figure 2 Divergent Incidence of Frailty between Two Groups. |
Association Between Frailty and Risk Factors in Patients with OSA
The unadjusted logistic regression demonstrated a significant correlation between frailty and multiple risk factors. Specifically, the OR was 1.18 for age (95% CI, 1.12–1.25; P < 0.001), 1.95 for smoking (95% CI, 1.07–3.61; P = 0.027), 1.18 for BMI (95% CI, 1.00–1.39; P = 0.003), and 1.87 for diabetes (95% CI, 1.05–3.33; P = 0.032). After adjusting for confounding variables such as age, AHI, smoking, diabetes, and CPAP therapy, the adjusted OR was 1.20 for age (95% CI, 1.13–1.28; P < 0.001), 1.01 for AHI (95% CI, 1.00–1.03; P = 0.010), and 0.36 for CPAP therapy (95% CI, 0.15–0.88; P = 0.025; Table 3).
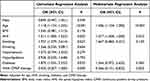 |
Table 3 Results of Logistic Analysis |
Discussion
To the best of our knowledge, this study is the first to investigate the potential of CPAP therapy to mitigate frailty in older individuals with OSA. Our primary findings suggest two key points: (i) CPAP therapy is effective in delaying the onset of frailty in older OSA patients; (ii) severe OSA is a significant risk factor for frailty.
Frailty has been strongly correlated with factors such as gender, AHI13 and BMI.19 In the present study, we controlled for these variables to minimize their impact on the outcomes. Frailty is an age-related syndrome characterized by reduced biological reserves, which in turn can lead to negative outcomes like disability, institutionalization, hospitalization, and mortality.20 Notably, frailty is often a reversible condition, and early identification of associated risk factors could help in reducing its prevalence.21 Previous research has already recognized OSA as a risk factor for frailty.13 The biological mechanisms underpinning OSA include the generation, metabolism, and abnormal activation of reactive oxygen species, as well as the initiation of inflammatory responses; these factors are also implicated in the onset of frailty.22–25 Our data further confirmed that individuals with severe OSA have a higher likelihood of being frail, although this was not significant. Additionally, we found no evidence of independent associations between frailty and gender or BMI. However, the existence of an ethnic or cultural factor that explains this discrepancy cannot be ruled out, and further studies are required in this regard.
In our study, we observed that patients with OSA who adhered to CPAP therapy experienced less fatigue compared to those in the non-CPAP group. This finding aligns with earlier research demonstrating that three weeks of CPAP therapy substantially mitigated fatigue and enhanced energy levels in OSA patients.26 Our results are also consistent with those of Lianne, particularly after a median follow-up period of 52 months. One plausible explanation for the observed fatigue reduction is that CPAP diminishes inflammation in OSA patients, thereby mitigating fatigue. Moreover, our study revealed that CPAP therapy significantly enhanced exercise tolerance in elderly patients with OSA. The improvement in exercise performance could be attributed to multiple factors. For instance, CPAP is known to enhance left ventricular function and cardiac index, subsequently improving arterial oxygen content. These physiological changes provide a rationale for the observed benefits in patients with heart failure. Additionally, some researchers propose that CPAP might modulate the autonomic nervous system, which could further contribute to improved exercise performance. It has also been hypothesized that CPAP enhances oxygen volume by reducing the production of reactive oxygen species like interleukin-8, TNF-α, and IL-6, thus leading to advancements in cardiovascular, ventilatory, and musculoskeletal systems.27 In relation to unintentional weight loss—a condition associated with increased morbidity and mortality in individuals over 65 years old28 —our findings indicated that the CPAP group was at a lower risk. Previous research by Chin found that leptin levels, which are involved in regulating body weight and fat distribution, declined significantly after 3 to 4 days of CPAP therapy in OSA patients.29 Furthermore, energy expenditure during sleep has been found to increase in individuals with sleep apnea, particularly those with severe forms, and to decrease upon CPAP treatment.30
CPAP, a standard treatment for OSA, not only alleviates upper airway obstruction during sleep but also diminishes stress-induced inflammation and corrects alveolar hypoxia by promoting unobstructed airflow into the alveoli. A meta-analysis has corroborated the ability of CPAP therapy to significantly reduce inflammatory markers such as C-reactive protein (CRP), IL-6, and TNF-α in patients with OSA.31 Additionally, CPAP therapy has been found to elevate serum vitamin D levels in individuals diagnosed with OSA.32 A growing body of evidence points to a strong correlation between vitamin D levels and frailty,33–36 which could account for the observed effectiveness of CPAP in mitigating frailty in OSA patients. Moreover, frailty has a significant association with hypertension and diabetes.20 Previous studies have indicated that CPAP therapy leads to reductions in blood pressure37 and improvements in glycemic control and insulin resistance.38 Hence, it is plausible to posit that CPAP may mitigate the occurrence of frailty by means of an intermediary influence. This may explain the relatively strong effectiveness of CPAP in preventing frailty, despite the limited link between the severity of AHI and frailty.
Our results demonstrate that CPAP therapy significantly attenuates the onset of frailty in elderly individuals diagnosed with OSA. These findings indicate that CPAP may serve as a strategic intervention for both the prevention and mitigation of frailty, consequently enhancing the quality of life in aging populations. Notable strengths of our study are its multicenter cohort design and long-term follow-up, which add rigor and reliability to our conclusions. To our knowledge, this is the first investigation to establish a link between CPAP therapy and reduced incidence of frailty among elderly individuals with OSA. However, our study is not without limitations. A major limitation of this study is the apparent reliance on telephone surveillance data rather than on objective measurement to assess CPAP compliance. Despite thorough investigation by my colleagues, the potential for residual confounding cannot be eliminated. Furthermore, we made considerable efforts to match the non-CPAP group. However, other factors that could impact frailty in the elderly, such as smoking, drinking, economic status were not included in the PSM. This could potentially introduce some bias into the results. Additionally, the demographic homogeneity of our study population, consisting mainly of Asian individuals, limits the generalizability of our findings to other ethnic groups. Future studies should aim to include more ethnically diverse cohorts to ascertain the global applicability of our conclusions.
Conclusion
In this multicenter cohort study conducted in an Asian population, we found that CPAP treatment independently reduces the risk of the onset of frailty in elderly patients with OSA. Furthermore, age, severe OSA, and the absence of CPAP treatment were identified as significant risk factors for frailty. Given these findings, we advocate for the initiation of CPAP therapy in all suitable elderly patients diagnosed with OSA, whenever feasible. However, further studies are warranted to elucidate the specific mechanisms by which CPAP treatment mitigates frailty.
Data Sharing Statement
Our research is conducted collaboratively, with a focus on teamwork. In the event that all team members are in agreement to share the data, the corresponding author can be contacted to request access to the information.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of the PLA General Hospital (S2022-366-01), and informed consent was obtained from all participants prior to study commencement.
Acknowledgments
We express our sincere appreciation to the six sleep centers and 355 patients who graciously participated in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Military Health Care Project (22BJZ52, 23BJZ27), Military Equipment Construction Application Research Project (LB20211A010013) and Military experimental animal special research project (SYDW_KY[2021]04). The funders had not directly role in the design.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Johnson KG, Johnson DC. When will it be time? Evaluation of OSA in stroke and TIA patients. Sleep Med. 2019;59:94–95. doi:10.1016/j.sleep.2018.10.016
2. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52(8):686–717. doi:10.1016/j.jacc.2008.05.002
3. Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290(14):1906–1914. doi:10.1001/jama.290.14.1906
4. Targa ADS, Benítez ID, Moncusí-Moix A, et al. Breathing cessation events that compose the apnea-hypopnea index are distinctively associated with the adverse outcomes in Alzheimer’s disease. Alzheimer’s Res Ther. 2023;15(1):123. doi:10.1186/s13195-023-01266-x
5. Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166(16):1709–1715. doi:10.1001/archinte.166.16.1709
6. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078. doi:10.1002/14651858.CD001106.pub3
7. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A. 2001;56(3):M146–M156. doi:10.1093/gerona/56.3.m146
8. Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol Biol Sci Med Sci. 2017;73(1):102–108. doi:10.1093/gerona/glx098
9. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi:10.1016/s0140-6736(19)31786-6
10. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Biol Sci Med Sci. 2004;59(3):255–263. doi:10.1093/gerona/59.3.m255
11. Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surgeons. 2012;215(4):453–466. doi:10.1016/j.jamcollsurg.2012.06.017
12. Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54(6):991–1001. doi:10.1111/j.1532-5415.2006.00745.x
13. Mehawej J, Saczynski JS, Kiefe CI, et al. Association between risk of obstructive sleep apnea and cognitive performance, frailty, and quality of life among older adults with atrial fibrillation. J Clin Sleep Med. 2022;18(2):469–475. doi:10.5664/jcsm.9622
14. Piovezan RD, Abucham J, Dos Santos RV, Mello MT, Tufik S, Poyares D. The impact of sleep on age-related sarcopenia: possible connections and clinical implications. Ageing Res Rev. 2015;23(Pt B):210–220. doi:10.1016/j.arr.2015.07.003
15. Moreno-Tamayo K, Manrique-Espinoza B, Guerrero-Zúñiga S, Ramírez-García E, Sánchez-García S. Sex differences in the association between risk of obstructive sleep apnea, insomnia, and frailty in older adults. Nat Sci Sleep. 2021;13:1461–1472. doi:10.2147/nss.S320192
16. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE Assessment. J Clin Sleep Med. 2019;15(2):301–334. doi:10.5664/jcsm.7638
17. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi:10.5664/jcsm.2172
18. Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
19. Jayanama K, Theou O, Godin J, Mayo A, Cahill L, Rockwood K. Relationship of body mass index with frailty and all-cause mortality among middle-aged and older adults. BMC Med. 2022;20(1):404. doi:10.1186/s12916-022-02596-7
20. Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–1386. doi:10.1016/s0140-6736(19)31785-4
21. Marcucci M, Damanti S, Germini F, et al. Interventions to prevent, delay or reverse frailty in older people: a journey towards clinical guidelines. BMC Med. 2019;17(1):193. doi:10.1186/s12916-019-1434-2
22. Teixeira-Gomes A, Lage B, Esteves F, et al. Frailty syndrome, biomarkers and environmental factors - a pilot study. Toxicol Lett. 2020;330:14–22. doi:10.1016/j.toxlet.2020.04.023
23. Kane AE, Sinclair DA. Frailty biomarkers in humans and rodents: current approaches and future advances. Mech Ageing Dev. 2019;180:117–128. doi:10.1016/j.mad.2019.03.007
24. Furtado GE, Uba Chupel M, Minuzzi L, et al. Exploring the potential of salivary and blood immune biomarkers to elucidate physical frailty in institutionalized older women. Exp Gerontol. 2020;129:110759. doi:10.1016/j.exger.2019.110759
25. Kheirandish-Gozal L, Gozal D. Obstructive sleep apnea and inflammation: proof of concept based on two illustrative cytokines. Int J Mol Sci. 2019;20(3):459. doi:10.3390/ijms20030459
26. Tomfohr LM, Ancoli-Israel S, Loredo JS, Dimsdale JE. Effects of continuous positive airway pressure on fatigue and sleepiness in patients with obstructive sleep apnea: data from a randomized controlled trial. Sleep. 2011;34(1):121–126. doi:10.1093/sleep/34.1.121
27. Fletcher HV, Cho PSP, Loong SL, et al. Effect of continuous positive airway pressure on maximal exercise capacity in patients with obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2020;16(11):1847–1855. doi:10.5664/jcsm.8686
28. Gaddey HL, Holder KK. Unintentional Weight Loss in Older Adults. Am Fam Phys. 2021;104(1):34–40.
29. Chin K, Shimizu K, Nakamura T, et al. Changes in intra-abdominal visceral fat and serum leptin levels in patients with obstructive sleep apnea syndrome following nasal continuous positive airway pressure therapy. Circulation. 1999;100(7):706–712. doi:10.1161/01.cir.100.7.706
30. Stenlöf K, Grunstein R, Hedner J, Sjöström L. Energy expenditure in obstructive sleep apnea: effects of treatment with continuous positive airway pressure. A J Physiol. 1996;271(6 Pt 1):E1036–E1043. doi:10.1152/ajpendo.1996.271.6.E1036
31. Xie X, Pan L, Ren D, Du C, Guo Y. Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med. 2013;14(11):1139–1150. doi:10.1016/j.sleep.2013.07.006
32. Liguori C, Romigi A, Izzi F, et al. Continuous positive airway pressure treatment increases serum vitamin D levels in male patients with obstructive sleep apnea. J Clin Sleep Med. 2015;11(6):603–607. doi:10.5664/jcsm.4766
33. Gutiérrez-Robledo LM, Ávila-Funes JA, Amieva H, et al. Association of low serum 25-hydroxyvitamin D levels with the frailty syndrome in Mexican community-dwelling elderly. Aging Male. 2016;19(1):58–63. doi:10.3109/13685538.2015.1105796
34. Trevisan C, Veronese N, Maggi S, et al. Factors influencing transitions between frailty states in elderly adults: the Progetto Veneto Anziani longitudinal study. J Am Geriatr Soc. 2017;65(1):179–184. doi:10.1111/jgs.14515
35. Rybchyn MS, Abboud M, Puglisi DA, et al. Skeletal muscle and the maintenance of vitamin D status. Nutrients. 2020;12(11):3270. doi:10.3390/nu12113270
36. Sutherland JP, Zhou A, Hyppönen E. Muscle traits, sarcopenia, and sarcopenic obesity: a vitamin D Mendelian randomization study. Nutrients. 2023;15(12):2703. doi:10.3390/nu15122703
37. Feldstein CA. Blood pressure effects of CPAP in nonresistant and resistant hypertension associated with OSA: a systematic review of randomized clinical trials. Ann Clin Exp Hypertens. 2016;38(4):337–346. doi:10.3109/10641963.2016.1148156
38. Martínez-Cerón E, Barquiel B, Bezos AM, et al. Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes. a randomized clinical trial. Am J Respir Crit Care Med. 2016;194(4):476–485. doi:10.1164/rccm.201510-1942OC
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
