Back to Journals » Medical Devices: Evidence and Research » Volume 17
Effect of Back-Cut Point Needle Bevel Angle on Deterioration After Multiple Punctures in Central Vein Simulation
Authors Urimoto G , Suzuki T , Matsuda M, Ito K , Orihashi Y, Suzuki T
Received 10 November 2023
Accepted for publication 12 February 2024
Published 21 February 2024 Volume 2024:17 Pages 89—95
DOI https://doi.org/10.2147/MDER.S447188
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Genya Urimoto,1 Takeshi Suzuki,1 Mitsumasa Matsuda,1 Kenzi Ito,1 Yasushi Orihashi,2 Toshiyasu Suzuki1
1Department of Anesthesiology, Tokai University School of Medicine, Kanagawa, Japan; 2Division of Clinical Research, Kitasato University Hospital, Kanagawa, Japan
Correspondence: Takeshi Suzuki, Department of Anesthesiology, Tokai University School of Medicine, 143 Shimokasuya, Isehara, Kanagawa, 259-1193, Japan, Tel +81 463 93 1121, Email [email protected]
Background: Multiple needle punctures during central venous line insertion can lead to serious complications. Needle deterioration owing to repeated punctures may be a major cause. We hypothesized that there is an optimal bevel angle for a back-cut point needle that is resistant to deterioration. In this study, we examined the effect of bevel angle differences in a back-cut point needle on needle tip deterioration caused by multiple punctures.
Methods: The resin target was punctured perpendicularly using back-cut point needles with three bevel angles (15°, 17°, and 19°; n=8 for each angle) at a speed of 200 mm/min. The same needle was used for ten consecutive punctures at different locations on the target. The force applied to the needle was recorded as puncture force. The puncture force waveform is bimodal. The second peak values, which formed the maximum values of puncture force, were the focus of the main analysis. We considered a 5% elevation from the first to the 10th puncture force as needle deterioration, and the average slope value of the regression line between the puncture number and puncture force was used. When the upper limit of the 95% confidence interval (CI) of the slope value was less than 0.008889, the needle was considered to be resistant to deterioration.
Results: The slopes of the second peak values during 10 consecutive punctures for each bevel angle (15°, 17°, 19°) were 0.003011 ± 0.01085 [− 0.006056, 0.012077], 0.006116± 0.007431 [− 0.000096, 0.012328], and 0.001515 ± 0.005783 [− 0.003320, 0.006349], respectively (mean ± standard deviation [95% CI]). Only the 19° angle needle had a smaller upper limit of the 95% CI for a slope value of 0.008889.
Conclusion: The 19° bevel angle back-cut point needle was more resistant to deterioration than the 15° and 17° angle needles were.
Keywords: central venous line, repeated needle punctures, back-cut point needle, needle tip deterioration, complications
Introduction
In recent years, the insertion of a central venous catheter is usually performed under ultrasound guidance, ensuring safety during the procedure.1,2 Although ultrasound-guided central venous catheter insertion has been shown to reduce the incidence of complications, fatal complications have also been reported.3,4 Multiple needle puncture attempts have been reported to be associated with serious complications.5–8 Multiple punctures can cause minute scratches and irregularities on the needle tip and increase the puncture force.9 A degraded needle tip caused by repeated punctures may fail to cut the surface of the veins, collapse vessels due to pushing, and lead to difficulties in central venous puncture. Thus, resistance to degradation caused by repeated puncture is required for an ideal puncture needle. Smooth indwelling of the guidewire into the central vein through a puncture needle is also important for preventing serious complications related to central venous catheter insertion. Previous studies have recommended that the needle tip be short to prevent complications due to guidewire insertion.10 Therefore, an ideal metal needle for central vein puncture should have a short tip that is resistant to degradation by multiple punctures with a slight force. However, a larger bevel angle is required for a short needle tip, which may increase the force necessary to puncture the central vein and decrease procedural success rate. Despite these concerns regarding deterioration of the puncture needle, no previous studies have investigated how the bevel angle of the puncture needle affects the degree of needle tip deterioration caused by repeated punctures.
Two types of metal needles are used as introducers for central vein puncture: back-cut and lancet-point needles. One of the features of the back-cut point needle is the polished linear edge on the rear side of the blade surface, which creates a secondary blade surface. This secondary blade, opposite to the first blade surface, directly touches on the target skin (Figure 1). The inner lumen edge is not ground. The characteristics of the lancet point needle are curved edges polished on the front blade surface and the ground inner edge. Regarding these characteristics, it is likely that the back-cut point needle is superior to the lancet point needle in terms of safety because the back-cut point needle might be able to decrease the puncture force by making a shallower insertion angle compared to the lancet point needle11 and reduce guidewire trouble because of the lack of a sharpened inner edge.
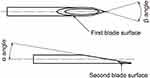 |
Figure 1 Structure of the back-cut point needle. This figure illustrates the definition of the α and β angles and two blade surfaces. |
In this study, we evaluated how the difference in the bevel angle of the back-cut point needle affected the degree of needle tip deterioration after multiple punctures and determined the optimal bevel angle of the back-cut point needle for central vein puncture.
Materials and Methods
Study Design
In this study, we used three types of back-cut point needles to evaluate the effect of the bevel angle on needle tip deterioration. Figure 1 presents the definition of each angle of the back-cut point needle. The 20-gauge stainless steel needles with three bevel angles (15°, 17°, and 19°) were prepared (Unisis Corporation, Tokyo, Japan). Angle β was required to be 55° ± 5° for all three angles. Before preparing the three different types of needles, we investigated the back-cut point needle included in the central venous catheter kit marketed in Japan to select the optimal angle. We referred to three products from three different companies, including the back-cut point needle in the central venous catheter kit; the α angles data were 15.8° (Arrow®, Teleflex, PA, USA), 21.5° (Legaforce®, TERUMO, Tokyo, Japan), and 16.5° (Seldinger kit, Medikit, Tokyo, Japan). We measured the needle angle of the arrow kit because there are no published data for this measurement. We refer to the 51.2° β angle in the arrow kit, which has the largest market share of the three products. The angles for the three types of needles were measured using a 50x magnified image from a digital microscope VHX-7000 version 1.3.13.4 (KEYENCE®, Osaka, Japan). The measured angles for the three needle types are listed in Table 1. The puncture target sheet was produced by TANAC (Gifu, Japan), which manufactures artificial organs to simulate the surgical procedures. The hardness and texture of the puncture target sheet were selected based on a previous report12 in which the average peak puncture force was 1.594 N during internal jugular vein puncture in a fresh frozen embalmed cadaver. The puncture target consisted of three layers: a 50 µm polyamide film on top of a 1 mm silicon sheet (Shore Durometer A40°) as a skin model, and two sheets of 5 mm urethane sheet (Shore Durometer E28°) as the muscle model (Figure 2).
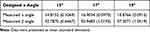 |
Table 1 Actual Measured α and β Angle for Three Different Needles |
 |
Figure 2 The puncture target consisted of three layers; 50 µm polyamide film on top of 1 mm silicon sheet for the skin model, and two 5mm urethane sheets for the muscle model. |
Measurements
The puncture force required for each needle to penetrate the puncture target sheet was measured using Autograph® (Shimadzu Corporation, Kyoto, Japan) (Figure 3). The puncture target sheet was set parallel to the ground, and the prepared back-cut point needle was inserted perpendicular to the target sheet for puncture at a speed of 200 mm/min, as previously reported,11 and was considered clinically relevant. The needle puncture procedure was performed ten times at different sites on the target sheet. Autograph® measured the force applied to the needle during the puncture procedure, and the results were recorded continuously by Trapezium X Version 1.5.2, an accessory software of Autograph®. The waveform of the puncture force was bimodal; the first peak was formed by the force applied at the tip level and the second peak was formed at the end of the blade surface.11 We focused on the second peak puncture force as the primary outcome, which indicates the maximum puncture force during the procedure. The slope of the regression line between the 10 puncture numbers and the second peak puncture forces was analyzed. The same analysis of the first peak puncture force was performed as the secondary outcome.
 |
Figure 3 The Autograph® configuration (Shimadzu Corporation, Japan). |
Ethic Approval
Ethical approval was waived by the ethics committee of the Tokai University School of Medicine because this study was performed without the use of human or animal resources.
Statistics
A preliminary experiment was performed using three needles at an angle of 17°. The average second-peak puncture force during the first puncture was 1.712 N. The average value of the slope for the second peak puncture force, determined by the regression line of 10 punctures was −0.001148, standard deviation of 0.005865. Needle deterioration was defined as a > 5% increase in the second peak puncture force at the 10th puncture compared with that at the first puncture. If the first puncture force was 1.6 N with reference to the preliminary result, the 10th puncture force was 1.68 N after deterioration at a rate of 5%, and the slope of the regression line between the puncture number and puncture force was 0.008889. We defined needles as significantly resistant to deterioration when the upper limit of the 95% confidence interval (CI) of the slope value was less than 0.008889. The sample size was calculated using G*Power Version 3.1.9.6,13 with a two-sided type I error of 0.05 and a power of 0.9. The expected value of the slope was 0, with a standard deviation of 0.0065, and it was assumed based on a preliminary experiment. A sample size of eight was obtained. The slope of the regression line was obtained for the first peak puncture force in a secondary analysis. Analysis of variance (ANOVA) followed by a post-hoc test was performed to compare the slope values of the first and second peak puncture forces between the three angles of the needle. The 10 sequential first and second peak puncture forces were compared among the three needles at different angles using two-way repeated-measures ANOVA. SPSS ver. 26 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. Results are presented as mean ± standard deviation (SD) (95% confidence interval [CI]), and statistical significance was set at p < 0.05.
Result
The slope values for the second and first peak puncture forces after ten sequential punctures for the three angles of needles are listed in Table 2. The slope value of the second peak puncture forces for each α angle (15°, 17°, 19°) were 0.003011 ± 0.01085 [−0.006056, 0.012077], 0.006116 ± 0.007431 [−0.000096, 0.012328], and 0.001515 ± 0.005783 [−0.003320, 0.006349], respectively. The slope value of the first peak puncture forces for each α angle (15°, 17°, 19°) needle were 0.001896 ± 0.001731 [0.000449, 0.003343], 0.000521 ± 0.000733 [−0.000092, 0.001133], and 0.000447 ± 0.001318 [−0.001549, 0.000655], respectively. The results for the second and first puncture forces are shown in Figure 4. Regarding the slope formed by the second peak puncture force, the upper limit of the 95% CI for the slope value was significantly less than 0.008889 for the 19° α angle needle only (p=0.009), indicating this needle was the most resistant to deterioration among the three needle types. In the analysis of the slope formed by the first peak puncture force, there was a significant difference among the three angles (p=0.0071), and the post-hoc test showed that the slope value of the 19° angle needle was significantly smaller than that of the 15° angle needle. Although there was no statistically significant difference between the 19° and 17° angles, the slope value for the 19° angle needle tended to be smaller than that for the 17° angle needle. The results regarding the first peak puncture force also indicated that the needle with 19° α angle was the most resistant to deterioration.
 |
Table 2 The Slope Values for the Second and First Peak Puncture Forces |
For the puncture force itself, the second peak values tended to be 17°> 19°> 15° (Figure 4A); however, there was no significant difference between the three angles (p=0.056). There was no significant interaction between the angle and number of punctures (p=0.492) in the two-way repeated measures ANOVA for the second peak puncture force. Although the first peak puncture forces were 19°> 17°> 15°, as shown in Figure 4B, there was a significant interaction between the angle and number of punctures (p=0.008). The first peak puncture force was consistently 19°> 17°> 15° for the same puncture number in the Tukey’s multiple comparison test (p<0.05).
Discussion and Conclusion
To the best of our knowledge, this is the first study to quantitatively evaluate back-cut point needle deterioration due to repeated punctures and to demonstrate that it differs depending on the angle of the blade surface. In this study, the needle with 19° α angle was more resistant to needle tip deterioration after repeated punctures compared with the 15° and 17° angle needles. This result is likely to contribute to the development of an ideal puncture needle that can enable easier and safer central venous line insertion. We analyzed the deterioration of the back-cut point needle by comparing the slope value of the second peak puncture forces during 10 consecutive punctures at three different angles (15°, 17°, and 19°) and determined that the needle was resistant to deterioration when the upper limit of the 95% CI of the slope value was < 0.008889, which was based on a preliminary study. By using the upper limit of the 95% CI as the cut-off value, we were able to evaluate the deterioration of the back-cut point needles more strictly. Owing to this statistical method, only 19° α angle needles were considered resistant to deterioration following repeated punctures. Analysis of the first peak puncture force showed that the slope of the 19° angle needle was significantly smaller than that of the 15° α angle needle. Given that the slope values of the first peak tended to be 15° > 17° > 19°, these results also suggest that needles with an angle of 19° α angle are the most resistant to deterioration induced by repeated punctures. A larger sample size may be required to detect a statistically significant difference between the first peak slope values of the 19° and 17° angle needles.
In this experimental study, we selected the slope value of the second peak puncture force as the primary outcome for evaluating the resistance of the needle against repeated punctures, rather than the first peak puncture force. Although the effects of the angle might be more predominant in the first peak force than in the second one, we chose the second peak force as the primary outcome because the second peak force was greater than the first one. A greater puncture force must be more influential in the deviation of the tissues surrounding the central veins, which could reduce the success rate of central vein puncture because it deforms the veins and causes contact between the anterior and posterior walls.14 Regarding the puncture force itself, the 19° α angle needle had the highest first peak puncture force among the three angles, which may have caused difficulty in puncturing the central vein. However, the difference was too small, and the aim of this study was to evaluate needle deterioration by analyzing the second peak force.
We were able to capture needle deterioration after repeated punctures by using a highly reproducible puncture target. The ideal puncture target should have two characteristics: the capacity to detect minute changes in each puncture force, and adequate and sufficient hardness to induce needle deterioration. Initially, we selected pig or sheep leather layered with pork meat as the puncture target model. However, we could not evaluate the deterioration of the needle because experimental factors other than the effect of needle deterioration by multiple punctures affected the measured puncture force, the thickness of the leather was not uniform, the hair root indentations were randomly located, and leather moisture was not even due to muscle water absorption. The puncture targets were clamped using porous metal plates (reference number: ISO7864:2016; International Organization for Standardization, Geneva, Switzerland) to fix needle punctures. We could not stabilize the pressure applied to the targets in this setting, because the greater the tension applied to the puncture target, the lower the puncture force.15 Therefore, we designed a puncture target model made of resin to address these issues. Because the virtual skin layer was sufficiently fixed on top of the 10 mm virtual muscle layer without any stabilizer, we did not need to adjust the tension applied to the target material.
The needles used in this experiment were manufactured especially for this experiment by the Unisis Corporation. The α angles of all needles were precise, and the errors within each angle were negligible. However, there were some concerns regarding β angles of the three types of needles. The β angle of the 19°needle was slightly larger than those of the 15° and 17°needles, which could have influenced the results. This difference in the β angles is a technical issue in the production of back-cut point needles. The larger the α angle, the closer the distance between the lumen and blade linear edge shaped by the second blade surface (Figure 1) is, if the β angle is narrow. This indicates that the needle metal thickness limits the production of needles with a narrow β-angle and a large angle. Although this difference may have influenced the results of this study, our final goal was to pursue an ideal puncture needle with resistance to deterioration following repeated punctures.
This study has several limitations that should be considered when interpreting the results. First, only three angles (15°, 17°, and 19°) were evaluated. However, given that most needles used for central venous line insertion are within this angle range, this choice of three angles seems reasonable. Furthermore, we demonstrated the differences among these three angles in the deterioration caused by repeated punctures. Second, the needle puncture was performed perpendicular to the target sheet, which is unrealistic in actual clinical situations. The value of the puncture force might be different if the needle punctures the target sheet at an angle of 30–45°, which is practical in clinical situations. Considering that the aim of this study was to compare needle deterioration among three different angles, it is likely that we accomplished this aim. Third, we used an artificial target sheet instead of human skin. Because the artificial target sheet used in this study was quite imitative of human skin and highly reproducible, we believe that we precisely evaluated needle deterioration. Finally, the standard deviation of the second peak puncture force, which was analyzed for the primary outcome, was greater than that of the first peak, and the second peak puncture force itself did not differ significantly among the three angles. However, considering that the experiment was performed under the same conditions for each angle, and that the evaluation of the slope value after 10 repeated punctures was unlikely to be influenced by the absolute value of the second peak puncture force itself, we believe that these issues have little impact on the results of the study.
In conclusion, the 19° α angle needle was more resistant to deterioration after repeated punctures than the 15° and 17° α angle needles were. Further studies are warranted to develop an ideal needle that can puncture with a slight force and does not deteriorate after repeated punctures.
Data Sharing Statement
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors thank Yoshikazu Matsumoto for assistance with the experiments. We also thank Akihiro Saruya for the design and production of needles used in this study. We are grateful to the Unisis Corporation for lending us all the equipment.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors received no financial support for this study.
Disclosure
The authors declare no potential conflicts of interest regarding the research, authorship, or publication of this article.
References
1. Lalu MM, Fayad A, Ahmed O, et al. Ultrasound-guided subclavian vein catheterization: a systematic review and meta-analysis. Crit Care Med. 2015;43(7):1498–1507. doi:10.1097/CCM.0000000000000973
2. Brass P, Hellmich M, Kolodziej L, et al. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015. Availabe from: http://www.thecochranelibrary.com.
3. Henry TCL, Huei TJ, Yuzaidi M, et al. Unexpected complication of arteriovenous fistula of the left common carotid to internal jugular vein following central venous catheterization. Chin J Traumatol. 2020;23(1):29–31. doi:10.1016/j.cjtee.2019.10.001
4. Japan Medical Safety Research Organization. Recommendations for the prevention of recurrence of medical accidents analysis of deaths related to the complications of “Central Venous Catheterization” Analysis of deaths related to the complications of “Central Venous Catheterization”; 2017. Availabe from: https://www.medsafe.or.jp/modules/advocacy/index.php?content_id=49.
5. Bo-Linn G, Anderson DJ, Anderson KC, et al. Percutaneous central venous catheterization performed by medical house officers: a prospective study. Cathet Cardiovasc Diagn. 1982;8(1):23–29. doi:10.1002/ccd.1810080105
6. Lefrant J, Muller L, De J, et al. Risk factors of failure and immediate complication of subclavian vein catheterization in critically ill patients. Intensive Care Med. 2002;28(8):1036–1041. doi:10.1007/s00134-002-1364-9
7. Eisen LA, Narasimhan M, Berger JS, et al. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21(1):40–46. doi:10.1177/0885066605280884
8. Kusminsky RE. Complications of central venous catheterization. J Am Coll Surg. 2007;204(4):681–696. doi:10.1016/j.jamcollsurg.2007.01.039
9. Owen K, Blackie N, Gibson TJ. The effect of needle reuse on piglet skin puncture force. Vet Sci. 2022;9(2):90. doi:10.3390/vetsci9020090
10. Kim E, Kang P, Song IS, et al. Straight-tip guidewire versus J-tip guidewire for central venous catheterisation in neonates and small infants: a randomised controlled trial. Eur J Anaesthesiol. 2022;39(8):656–661. doi:10.1097/EJA.0000000000001695
11. Suzuki T, Tanaka A, Fukuyama H, et al. Differences in penetration force of intravenous catheters: effect of grinding methods on inner needles of intravenous catheters. Tokai J Exp Clin Med. 2004;29(4):175–181.
12. Pepley DF, Yovanoff MA, Mirkin KA, et al. Integrating cadaver needle forces into a haptic robotic simulator. J Med Devices. 2018;12(1):0145011–0145015. doi:10.1115/1.4038562
13. The G*Power team, Allgemeine Psychologie und Arbeitspsychologie, Heinrich-Heine-Universität Düsseldorf. G*Power; 2020. Available from: https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower.html.
14. Suzuki T, Kanazawa M, Kinefuchi Y, et al. A pilot/introducer needle for central vein cannulation. Tokai J Exp Clin Med. 1995;20(4–6):223–226.
15. Aoyagi S, Izumi H, Fukuda M. Biodegradable polymer needle with various tip angles and consideration on insertion mechanism of mosquito’s proboscis. Sens Actuat A Phys. 2008;143(1):20–28. doi:10.1016/j.sna.2007.06.007
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

