Back to Journals » Risk Management and Healthcare Policy » Volume 15
Effect of a Regional Outbreak of Coronavirus Disease 2019 on Kawasaki Disease in Korea
Received 24 January 2022
Accepted for publication 5 April 2022
Published 19 April 2022 Volume 2022:15 Pages 739—745
DOI https://doi.org/10.2147/RMHP.S359781
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Soo In Jeong, Hyun Joo Jung
Department of Pediatrics, Ajou University School of Medicine, Suwon, Republic of Korea
Correspondence: Hyun Joo Jung, Department of Pediatrics, Ajou University School of Medicine, 164 World Cup-ro, Yeongtong-gu, Suwon, 16499, Korea, Tel +81 31 219 5160, Fax +81 31 219 5169, Email [email protected]
Purpose: The association between coronavirus disease 2019 (COVID-19) and Kawasaki disease (KD) remains controversial. Prior to the nationwide epidemic of COVID-19, there was a unique, large-scale, regional outbreak in Daegu and Gyeonsangbuk-do (DG) in Korea in the spring of 2020. We evaluated the impact of COVID-19 on KD by comparing the characteristics of KD incidence between epidemic and non-epidemic regions in Korea.
Patients and Methods: We analyzed nationwide Health Insurance Review and Assessment (HIRA) data to estimate KD incidence from February 2019 to July 2020. Patients below 18 years who were admitted with KD and administered both intravenous immunoglobulin and aspirin (ICD-10 code M303 for KD) were included in the study. We compared the incidence of KD in DG and other regions by analyzing the period-specific incidence from February to May before and after the COVID-19 era.
Results: A total of 4461 patients were identified to have KD nationwide from February 2019 to July 2020. The nationwide incidence of KD was significantly reduced during this period compared with the period from February 2018 to July 2019 (p < 0.001). In the DG region, within the 0– 4-years age group, there was no significant difference in the incidence of KD between periods (p = 0.714). In the 5– 9 years age group, a significant decrease in KD incidence was observed in the DG region and all other regions from February 2019 to July 2020.
Conclusion: There was a significant decrease in nationwide KD incidence during and until 2 months after the local epidemic in Korea. However, no significant decrease in KD incidence was observed in the 0– 4 years age group in the DG region where the local COVID-19 outbreak occurred. A larger study is necessary to determine the correlation between KD in this age group and the COVID-19 outbreak.
Keywords: mucocutaneous lymph node syndrome, seasonal incidence, SARS-COV-2, social distancing, Republic of Korea
Introduction
Kawasaki disease (KD) is an acute vasculitis that occurs during childhood and is the leading cause of acquired heart disease in children in the developed world.1 The etiology of KD is unknown; however, it is believed to be multifactorial, with some infectious triggers playing a role in genetically susceptible children.
Along with the global pandemic of coronavirus disease 2019 (COVID-19), there have been increasing reports of Kawasaki-like disease, including multi-system inflammatory syndrome in children (MIS-C) in the US, Europe, and other countries.2–7 As the global COVID-19 pandemic continued with social distancing, a reduced incidence of KD has been reported in many Asian countries with a historically high incidence of the disease.8–11 In Korea, the COVID-19 epidemic was not severe in early 2020 and the outbreak occurred only in certain regions for a certain period of time between February 2020 and March 2020.12 Given that asymptomatic infections are common in children and that hospital visits were restricted due to widespread infections in the community at the time, it would be difficult to rule out the possibility of undetected COVID-19 infections in children. Furthermore, Korea is a country with a large number of KD cases, and MIS-C is a new concept that has not yet been reported as at March 2019; we cannot rule out the possibility that MIS-C was treated as atypical KD or incomplete KD between February 2020 and March 2020. Therefore, by analyzing the epidemiologic features of patients diagnosed with KD during this period, we will be able to predict the impact of COVID-19 on KD and whether MIS-C played a role in KD incidence in Korea.
To evaluate the direct effect of COVID-19 on KD in Korea, we analyzed the change in KD incidence before and after the local COVID-19 outbreak by dividing it into the Daegu and Gyeonsangbuk-do (DG) region and other regions.
Materials and Methods
Data Source
We analyzed public health data provided by the Health Insurance Review and Assessment (HIRA) to predict whether there is a regional difference in KD incidence after the COVID-19 epidemic from February 2020 to March 2020. The HIRA is a government-affiliated organization created to build an accurate claims review and quality assessment system for the National Health Insurance, with databases open for all academic investigators. The HIRA database consists of claims of approximately 98% of the Korean population (nearly 50 million individuals). It includes the beneficiary’s information, including patient age, sex, address, and data on the health-care services provided, such as diagnosis, tests, prescriptions, and procedures.
Ethics
This study was approved by the Human Investigation Review Board of Ajou University Hospital (IRB No. AJIRB-MED-EXP-20-464). Informed consent was not obtained because patient records/information was anonymized and de-identified prior to analysis.
Study Population and Statistical Analyses
For our analysis, the definition of KD was as follows: (1) the International Classification of Disease-10 diagnostic code for KD (M30.3), (2) the prescription code for intravenous immunoglobulin (IVIG) and aspirin together during hospitalization. There have been reports of MIS-C onset within 2 to 6 weeks of an illness compatible with acute COVID-19 infection, up to 8 weeks.13 We targeted the period from the beginning of the disease outbreak in February 2020 to May 2020, ie, eight weeks after the end of the outbreak in March 2020. The annual mean incidence rate was calculated as the number of patients who developed KD divided by the relevant population of the relevant period. Data of the total South Korean population in the relevant year were estimated from the resident registration population available from the Korean Statistical Information Services. The mean and standard deviation were calculated in the analysis of monthly changes.
To determine the change in KD incidence before and after the local outbreak, we compared the KD incidence in different age groups and regions during the same period of the year. Based on the data obtained in February 2020, when the regional epidemic occurred in the DG region, each region was divided into period 1 (February to May 2019) and period 2 (February to May 2020). The incidence of each region was compared during the same months to limit seasonal variation bias.
Results
The Nationwide Incidence of KD Decreased After the COVID-19 Pandemic in Korea
A total of 4461 KD cases treated with IVIG and aspirin were identified nationwide during our study period, from February 2019 to July 2020. In Korea, the COVID-19 epidemic was sparse until January 2020; however, a localized large-scale outbreak related to a religious group occurred in the DG region, which persisted for about 3 months and then rapidly disappeared. Since then, the nationwide spread of COVID-19 has occurred, which led to the start of nationwide social distancing in mid-February 2020 and has since been strengthened. The incidence of KD in Korea decreased significantly after the onset of the COVID-19 epidemic, and seasonal variation was eliminated during the study period (Figure 1).
The Regional Outbreak of COVID-19 Induced Differences in KD Incidence Between Different Age Groups
To determine the change in KD incidence in different age groups before and after the local outbreak, we compared the KD incidence by age group and region during the same period of the year. During period 1, a total of 1158 patients were diagnosed with KD, the majority of whom were males. The mean age of patients was 2.62±1.90 years. During period 2, there were 697 cases of KD, and there was no difference in age and sex during periods 1 and 2 nationwide. However, the mean age of patients with KD in the DG region was significantly lower during period 2 than during period 1 (2.56±2.33 vs 2.12±1.48, p = 0.025) (Table 1).
 |
Table 1 Number of Kawasaki Disease Cases in Children by Region |
The nationwide incidence of KD decreased significantly in period 2, which was after the COVID-19 epidemic, compared with period 1, before the COVID-19 epidemic. However, the rate of decline varied with age; in the 0–4 years age group, the nationwide KD incidence was 154.6 per 100,000 during period 1 and 97.08 per 100,000 during period 2 (RR, 0.66 [95% CI 0.66–0.73], p < 0.001). In the 5–9 years age group, KD incidence was 19.5 per 100,000 during period 1 and 10.6 per 100,000 during period 2 (Table 2). In the DG region, KD incidence in the 0–4 years age group was 124.0 per 100,000 in period 1 and 131.7 per 100,000 in period 2 (RR, 1.06 [95% CI 0.77–1.47], p = 0.714). In other regions, KD incidence in the 0–4 years age group was 157.8 per 100,000 in period 1 and 98.7 per 100,000 in period 2 (RR, 0.63, 95% CI 0.56–0.71, p < 0.001). In the 5–9 years age group, KD incidence in the DG region was 26.3 per 100,000 in period 1 and 5.6 per 100,000 in period 2 (RR, 0.21 [95% CI 0.07–0.62], p = 0.002). In other regions, KD incidence in the 5–9 years age group decreased during period 2 (18.8 per 100,000 in period 1 and 11.1 per 100,000 in period 2 (RR, 0.59 [95% CI 0.45–0.78], p < 0.001)) (Figure 2). When analyzing KD incidence subdivided by age for subjects below 5 years of age at which KD is most prevalent, there was no significant change in KD incidence between the two periods in all age groups in the DG region, unlike in other regions (Table 3). In our study, 11 children were prescribed inotropics during period 1; 10 children nationwide, and no children in the DG region were administered inotropics during period 2.
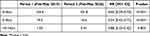 |
Table 2 Nationwide Incidence of Kawasaki Disease by Age |
 |
Table 3 The Periodic Changes of Incidence of Kawasaki Disease by Age |
 |
Figure 2 Comparison of changes in Kawasaki disease (KD) incidence between regions by age group. |
Discussion
As the global COVID-19 pandemic continued, with social distancing, a reduced incidence of KD has been reported, and a similar result was observed in our study.8–11 In Korea, a localized, large-scale, unique, short-term outbreak of COVID-19 related to a religious group occurred in the DG region from the end of January 2020. However, the COVID-19 epidemic in the DG region has been controlled, partially through the enforcement of social distancing measures, after April 2020, and the number of KD cases has also decreased nationwide. The incidence of KD in Korea decreased significantly after the onset of the COVID-19 epidemic, and seasonal variation was also eliminated during the study period. However, the decrease in KD incidence appeared in accordance with the initiation and strengthening of social distancing measures, rather than with the COVID-19 outbreak in the DG region, which was the same across the country (Figures 1 and 2). In a Japanese study that analyzed KD incidence throughout the COVID-19 epidemic, age and sex distributions did not significantly differ between 2016–2019 and 2020.8 In our study, there was no significant difference in the age and gender distribution of KD nationwide before and after the COVID-19 outbreak (Table 1). Therefore, it can be considered that the overall decrease in infectious diseases caused by social distancing had a greater impact on the KD outbreak in Korea than COVID-19 did itself. However, the fact that the occurrence of KD did not decrease in the DG region where there was a local outbreak of COVID-19 may implicate the possibility of COVID-19 as the cause of a decrease in KD incidence. Further research is needed to confirm this implication.
To determine the change in KD incidence in different age group before and after the local outbreak, we compared the KD incidence by age group and region during the same period of the year. In period 2, although nationwide enforcement of social distancing policies was implemented in the DG region, the COVID-19 epidemic still occurred, which implies that by comparing the difference in the change of KD incidence between periods 1 and 2 observed in the DG and other regions, the effect of COVID-19 itself on the KD incidence in Korea could be evaluated. The KD incidence across the nation, including in all other regions, was significantly reduced in period 2 for both the 0–4 years age group and the 5–9 years age group (p < 0.001). In the DG region, the KD incidence in the 5–9 years age group was significantly decreased (p = 0.002); however, no significant reduction in KD incidence was observed in the 0–4 years age group (p = 0.714) (Table 2 and Figure 2). Analysis of KD incidence confined to the 0–4 years age group, at which KD is most prevalent, revealed no significant change in the KD incidence in period 1 and period 2 in all ages below 5 years in the DG region. However, in other regions where there was no COVID-19 outbreak during period 2, the incidence of KD significantly decreased in period 2 in all age groups below 5 years. Interestingly, in other regions, the decrease in KD incidence was small between period 1 and period 2 in the 0 to 1-year-old group (RR = 0.81, CI [0.66–1.00], p = 0.045) (Table 3).
In this study, we observed a unique phenomenon in which the decrease in KD incidence was offset in the 0–4-years age group in the region where COVID-19 was most prevalent, unlike the nationwide KD incidence, due to the reduction of respiratory infectious diseases as a result of social distancing.14 Therefore, it can be considered that the overall reduction in infectious disease caused by social distancing and improved personal hygiene had a greater impact on the KD outbreak in Korea than COVID-19 itself. However, the fact that the occurrence of KD in certain age groups did not significantly decrease in the DG region where there was a local outbreak of COVID-19 may implicate the possibility of COVID-19 itself as the cause of KD, and further research is necessary to evaluate this implication. In addition, for the 0–1 year age group who had a relatively low extent of decrease in the incidence of KD, despite the rapid increase in social distancing caused by the COVID-19 outbreak, active research regarding etiology other than respiratory infections is necessary.
It is unknown whether the cause of KD in the 0–4-years age group is more affected by causes other than respiratory infections or whether KD-like syndromes, such as MIS-C, are mistaken for KD; thus, further research is needed. While MIS-C or KD-like syndrome has been reported in Europe, Latin America, and the United States, only a few cases have been reported in Asian countries where KD is more prevalent.15 The clinical spectrum of MIS-C associated with COVID-19 is variable, overlapping with KD symptoms, myocarditis, and acute heart failure.6,16 Since MIS-C is a very rare disease and has not been reported before April 2020, MIS-C might be misidentified and treated as KD shock syndrome or atypical KD in Asian countries. In our study, there were only 5 cases of KD in patients over 5 years in the DG region in period 2, and no patients received inotropic agents, suggesting that MIS-C cases are unlikely. No significant MIS-C cases were reported in several retrospective studies conducted in Japan on KD during the COVID-19 pandemic.8,17 Hence, the authors suggested that the lack of MIS-C reports in Asia might be related to racial differences and a lower incidence of COVID-19 in Asia than in Europe, causing fewer children to have the disease.17 Alternatively, it could be that MIS-C is such a rare condition that it has only been observed in countries with a very large number of COVID-19 cases, such as Italy, Spain, France, the UK, and the United States.
This study had a limitation. The clinical information of individual patients is lacking because the study data was gathered using HIRA data. In this study, we compared the KD incidence by region at the time of the COVID-19 epidemic limited to a specific region and observed that it is impossible to determine whether severe acute respiratory syndrome coronavirus 2 infection is present in children in the relevant community.
Conclusion
During and until 2 months after the local COVID-19 epidemic in Korea, KD incidence nationwide significantly decreased in children below 10 years. However, there was no significant decrease in KD incidence in the 0–4-years age group in the DG region where local COIVD-19 outbreaks occurred. A larger study is necessary to determine the correlation between KD in this age group and the COVID-19 outbreak.
Acknowledgments
We would like to thank Editage for English language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
1. McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi:10.1161/CIR.0000000000000484
2. Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395(10239):1771–1778. doi:10.1016/S0140-6736(20)31103-X
3. Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324(3):259–269. doi:10.1001/jama.2020.10369
4. Toubiana J, Poirault C, Corsia A, et al. Kawasaki-like multi-system inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. doi:10.1136/bmj.m2094
5. Pouletty M, Borocco C, Ouldali N, et al. Paediatric multi-system inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020;79(8):999–1006. doi:10.1136/annrheumdis-2020-217960
6. Belhadjer Z, Meot M, Bajolle F, et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of Global SARS-CoV-2 pandemic. Circulation. 2020;142(5):429–436. doi:10.1161/CIRCULATIONAHA.120.048360
7. Cheung EW, Zachariah P, Gorelik M, et al. Multisystem Inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York City. JAMA. 2020;324(3):294–296. doi:10.1001/jama.2020.10374
8. Iio K, Matsubara K, Miyakoshi C, et al. Incidence of Kawasaki disease before and during the COVID-19 pandemic: a retrospective cohort study in Japan. BMJ Paediatr Open. 2021;5(1):e001034. doi:10.1136/bmjpo-2021-001034
9. Shulman S, Geevarghese B, Kim KY, Rowley A. The impact of social distancing for COVID-19 upon diagnosis of Kawasaki disease. J Pediatric Infect Dis Soc. 2021;10(6):742–744. doi:10.1093/jpids/piab013
10. Hwangbo J, Lee JS, Choe SA, Choe YJ. Impact of social distancing on Kawasaki disease-associated hospitalization, South Korea. Pediatr Infect Dis J. 2021;40(10):e383–e384. doi:10.1097/INF.0000000000003202
11. Kang JM, Kim YE, Huh K, et al. Reduction in Kawasaki disease after nonpharmaceutical interventions in the COVID-19 era: a nationwide observational study in Korea. Circulation. 2021;143(25):2508–2510. doi:10.1161/CIRCULATIONAHA.121.054785
12. Central Disaster Management Headquarters K. Coronavirus Disease-19, Republic of Korea. Korea. Available from: http://ncov.mohw.go.kr/en/ Accessed April 17, 2022.
13. Martinez OM, Bridges ND, Goldmuntz E, Pascual V. The immune roadmap for understanding multi-system inflammatory in children: opportunities and challenges. Nat Med. 2020;26(12):1819–1824. doi:10.1038/s41591-020-1140-9
14. Yum S, Hong K, Sohn S, Kim J, Chun BC. Trends in viral respiratory infections during COVID-19 pandemic, South Korea. Emerg Infect Dis. 2021;27(6):1685–1688. doi:10.3201/eid2706.210135
15. Rowley AH. Understanding SARS-CoV-2-related multi-system inflammatory syndrome in children. Nat Rev Immunol. 2020;20(8):453–454. doi:10.1038/s41577-020-0367-5
16. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607–1608. doi:10.1016/S0140-6736(20)31094-1
17. Iio K, Uda K, Hataya H, et al. Kawasaki disease or Kawasaki-like disease: influence of SARS-CoV-2 infections in Japan. Acta Paediatr. 2021;110(2):600–601. doi:10.1111/apa.15535
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

