Back to Journals » Clinical Ophthalmology » Volume 17
Early Clinical Experience with a New Hydrophobic Acrylic Single-Piece Monofocal Intraocular Lens
Authors Schallhorn SC, Teenan D , Venter JA, Schallhorn JM , Hannan SJ
Received 2 August 2023
Accepted for publication 5 October 2023
Published 13 November 2023 Volume 2023:17 Pages 3419—3427
DOI https://doi.org/10.2147/OPTH.S433530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Steven C Schallhorn,1– 3 David Teenan,2 Jan A Venter,2 Julie M Schallhorn,1,4 Stephen J Hannan2
1Department of Ophthalmology, University of California, San Francisco, CA, USA; 2Optical Express, Glasgow, UK; 3Carl Zeiss Meditec, Inc, Dublin, CA, USA; 4F.I. Proctor Foundation, University of California, San Francisco, CA, USA
Correspondence: Steven C Schallhorn, Tel +1 858-455-6800, Email [email protected]
Purpose: To evaluate early clinical outcomes and adverse events (AEs) in cataract patients following implantation of a monofocal hydrophobic acrylic IOL with a new optimized non-constant aberration-correcting design (CT LUCIA 621P).
Methods: This retrospective study included patients with visually significant cataracts who underwent implantation of the CT LUCIA 621P IOL. Refraction, corrected (CDVA) and uncorrected (UDVA) visual acuity of the last available visit were used in the analysis. Intraoperative and postoperative AEs of the cohort were reviewed.
Results: A total of 191 eyes of 133 patients with the mean age of 70.2± 11.2 years were included in this study. The mean follow-up time of the last available visit was 1.7± 1.3 months. The mean postoperative monocular UDVA was 0.09± 0.16 logMAR (≈20/25), and 74.9% (143/191) eyes achieved ≥ 20/25 UDVA. The percentage of eyes with manifest spherical equivalent (MSE) within ± 0.50D and ± 1.00D of emmetropia was 84.8% (162/191) and 98.4% (188/191), respectively. Linear regression of attempted vs achieved MSE showed a tight relationship, with the coefficient of determination close to 1 (R2=0.99), indicating a very predictable refractive correction. The reported AEs were those typically expected after cataract surgery. There were no AEs related to intraoperative manipulation with the IOL/injector or to postoperative stability of the IOL in the capsular bag. No eye lost ≥ 2 lines of CDVA.
Conclusion: The implantation of CT LUCIA 621P resulted in good refractive predictability and visual outcomes. No IOL-related adverse events were reported.
Keywords: monofocal IOL, non-constant aberration-correcting optic design, cataract surgery
Introduction
Monofocal IOLs remain the most commonly used lens types in cataract patients and are expected to meet certain standards in modern cataract surgery. These include refractive predictability and stability in the capsular bag, biocompatibility (minimal postoperative inflammation, long-term optical clarity with no material degradation over time, minimal posterior capsule opacification development), and possess optical properties that provide the best possible image quality.
To achieve the optimal quality of vision, various approaches and optical principles have been utilized in IOL designs. The human cornea has inherent positive spherical aberration. Conventional spherical IOLs increase the overall positive spherical aberration of the eye following cataract surgery, which impacts the quality of the retinal image.1 To overcome this issue, aspheric aberration-free or aberration-correcting IOLs have been introduced.2 Aberration-correcting IOLs typically have a constant amount of negative spherical aberration to compensate for the positive spherical aberration of the cornea. However, these IOLs are more sensitive to decentration or tilt due to the difference in optical power between the intermediate and peripheral optic of the lens.3,4
Another alternative is an aspheric non-constant aberration-correcting optic design. According to the manufacturer, these IOLs have a central zone with negative spherical aberration, which varies towards the periphery – A concept that should, in theory, provide higher tolerance to decentration.5 The aim of this study was to report our initial experience with a new hydrophobic aspheric non-constant aberration correcting IOL, CT LUCIA 621P (Carl Zeiss Meditec AG, Jena, Germany). The new IOL was derived from a hydrophobic single-piece IOL CT LUCIA 611P of the same manufacturer with minor changes to the optical design. The 611P IOL model has already exhibited great refractive predictability, biocompatibility, and stability in the capsular bag.6–10 Early clinical outcomes and adverse events of the 621P model will be presented in this study.
Patients and Methods
The study included patients who underwent cataract surgery with the implantation of the CT LUCIA 621P IOL between June 2022 and March 2023. All patients signed an informed consent document, including the description of the surgical procedure and complications, IOL information, and an agreement to use their de-identified records for research purposes. The study was a retrospective and de-identified analysis of data obtained during standard postoperative visits and was deemed exempt from full review by the Institutional Review Board at the University of California, San Francisco. The design of the study followed the tenets of the Declaration of Helsinki.
Preoperative and postoperative records of patients were extracted from Optical Express (United Kingdom) electronic medical record with the following requirements: cataract surgery with the implantation of the CT LUCIA 621P IOL, preoperative corneal astigmatism (as determined by IOLMaster 700, Carl Zeiss Meditec AG, Jena, Germany) ≤1.50 D, and attended a minimum of 1-month postoperative visit. The extracted variables included patient demographics, visual acuities and refraction, and IOL-related intraoperative and postoperative adverse events.
Prior to intraocular surgery, all patients underwent a full ophthalmic examination, including visual acuity testing, slit lamp examination, dilated fundus examination, non-contact tonometry, corneal tomography, endothelial cell count, biometry, and retinal optical coherence tomography.
The surgeries were performed with the standard phacoemulsification technique. Lens calculations were performed using the IOLMaster 700 (Carl Zeiss Meditec AG, Jena, Germany) utilizing the Haigis formula (formula constants a0 = −0.053, a1 = +0.290, a2 = +0.199). The refractive aim was postoperative emmetropic spherical equivalent. All surgeries were performed by three experienced surgeons in four surgical centers.
The fully preloaded CT LUCIA 621P IOL was implanted into the capsular bag in all cases using the BLUESERTTM (Carl Zeiss Meditec AG, Jena, Germany) injector through a 2.75 mm clear corneal incision. All patients received intracameral cefuroxime at the end of the surgery for postoperative endophthalmitis prophylaxis.
The standard postoperative drop regimen included topical antibiotic drops for 2 weeks (every two hours for the first 24 hours and then four times a day for the remaining 13 days) and topical steroid drops for four weeks (every two hours for the first 24 hours, four times a day for 13 days and two times a day for further 14 days).
Postoperative visits were recommended at 1 day, 1 week, 1 month, and 3 months. A routine postoperative visit consisted of slit lamp biomicroscopy, non-contact tonometry, refraction, and uncorrected (UCVA) and corrected (CDVA) distance visual acuity.
Intraocular Lens
The CT LUCIA 621P (Figure 1) is a monofocal aspheric hydrophobic acrylic IOL with a patented ZO (Zeiss Optic; Carl Zeiss Meditec AG, Jena, Germany) non-constant aberration-correcting asphericity concept. The lens has a 6.0 mm optic diameter and an overall length of 13.0 mm. The available diopter range is between 0.00 and 34.0 D in 0.50 D increments. The IOL is heparin-coated (a fragment of heparin used in IOL surface coating with no pharmacological, immunological, or metabolic action) and has a single-piece C-loop design. It is step-vaulted with 0° angulation and equipped with a 360° square edge design for posterior capsule opacification prevention.
 |
Figure 1 CT LUCIA 621P IOL. |
Compared to its predecessor, CT LUCIA 611P, the CT LUCIA 621P has optimized asphericity. As a result of a different asphericity profile, the 621P model has a different A constant (120.2 instead of 119.9 for the 611P model). The IOL comes fully preloaded in the new BLUESERTTM injector (Figure 2), which was improved for smoother injection force, better haptic tucking, and injection reproducibility.
 |
Figure 2 BLUESERTTM injector. |
The ZO non-constant aberration profile of the IOL is designed to represent the normal human eye’s aberration and imaging properties. Unlike traditional aberration-correcting IOLs that correct a constant value of spherical aberration, the ZO concept features a central zone that has negative spherical aberration and moving towards the periphery of the optic, the spherical aberration changes from negative to positive, creating a neutral effect and providing the IOL with better tolerance to decentration. The ZO concept was derived from Liou & Brennan’s eye model,11 which takes into consideration the anatomic misalignment of the eye, the anterior and posterior curvatures of the cornea, and the position of the macula. The concept is also optimized for pupil size above 3.5 mm.
Statistical Analysis
The outcomes of the last available visit of each patient were used in the analysis. Preoperative and postoperative variables were compared with paired analysis (Student’s t-test or Wilcoxon’s test, depending on the normality assumption). The incidence rate of intraoperative and postoperative adverse events was calculated. All calculations were performed using the Microsoft Office Excel program (Microsoft Corp.).
Results
A total of 191 eyes of 133 patients were included in the analysis (58 bilateral surgeries and 75 unilateral surgeries). Patients with unilateral surgeries either required cataract surgery only in one eye or already had the fellow eye treated prior with a different monofocal IOL. Of the patients who had bilateral implantation of CT LUCIA 621P, 38 patients had immediate sequential, and 20 patients had delayed sequential bilateral cataract surgery.
Forty-eight eyes in the cohort (25.1% or 48/191) had accompanying ocular pathology (other than cataracts) noted preoperatively: 39 eyes had signs of dry age-related macular degeneration, and 9 eyes had an epiretinal membrane. The mean age of the study group was 70.2 ± 11.2 years (range 40 to 96 years), and the mean follow-up of the last available visit was 1.7 ± 1.3 (range 1 to 8 months). The demographics of the study group, as well as the basic preoperative and postoperative outcomes, are summarized in Table 1. The power of the implanted IOL ranged between 10 and 32 D (mean 22.2 ± 3.8 D).
 |
Table 1 Preoperative and Postoperative Outcomes (n = 191 Eyes) |
Visual Outcomes
Figure 3 depicts cumulative postoperative uncorrected distance visual acuity vs postoperative corrected distance visual acuity. Postoperatively, 74.9% (143/191) and 93.2% (178/191) of eyes achieved UDVA of 20/25 or 20/40 or better, respectively. Corrected visual acuity of 20/25 or 20/40 or better was achieved in 91.1% (174/191) and 99.5% (190/191) of eyes. On average, there was a 5 Snellen line gain between preoperative CDVA (0.51 ± 0.51 logMAR, ≈20/60) and postoperative CDVA (0.00 ± 0.11 logMAR; 20/20). The mean postoperative monocular UDVA was 0.09 ± 0.16 logMAR (≈20/25). No eye in the study lost two or more lines of corrected distance visual acuity.
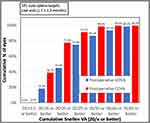 |
Figure 3 Cumulative postoperative uncorrected distance visual acuity (UDVA) vs cumulative postoperative corrected distance visual acuity (CDVA). |
Refractive Outcomes
The scattergram of attempted vs achieved manifest spherical equivalent is depicted in Figure 4. The linear regression shows a very tight correlation with the coefficient of determination close to 1 (R2 = 0.99).
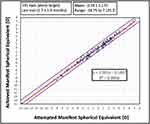 |
Figure 4 Scattergram of attempted vs achieved manifest spherical equivalent (D – diopter). |
Figure 5 shows the distribution of postoperative manifest spherical equivalent. The percentage of eyes within ±0.50 D and ±1.00 D of emmetropia was 84.8% (162/191) and 98.4% (188/191), respectively. The mean manifest spherical equivalent (MSE) changed from −0.59 ± 3.17 D (range: −14.75 to + 7.125 D) preoperatively to +0.15 ± 0.38 D (range: −1.00 to +1.125 D) postoperatively, p < 0.01.
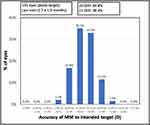 |
Figure 5 Distribution of postoperative manifest spherical equivalent (MSE – manifest spherical equivalent, D – diopter). |
Adverse Events
There were no intraoperative adverse events recorded in our cohort.
Postoperative adverse events included 3 cases of corneal edema persisting for longer than one month (3 eyes of 2 patients, per-eye incidence 1.57% or 1 in 64 eyes), but they all resolved within the first three postoperative months. Eight cases of postoperative cystoid macular edema were observed (8 eyes of 6 patients, per-eye incidence 4.19% or 1 in 24 eyes), and they all responded well to the treatment with topical steroid drops, non-steroidal anti-inflammatory drops, and oral acetazolamide.
Five eyes of four patients were noted to have signs of posterior capsule opacification (per-eye incidence 2.62% or 1 in 38 eyes). In all cases, patients had dense preoperative cataracts with poor visual acuity, and PCO was noted at the early postoperative visits: three eyes at the day one visit and two eyes (bilateral case) at the 1-month visit. The PCO was noted to be minor and did not require any intervention during the available follow-up. All five eyes had postoperative CDVA between 20/30 and 20/20.
There were no serious complications, such as endophthalmitis, toxic anterior segment syndrome, persistent inflammation, or retinal detachment, observed in this study. No IOL-related postoperative adverse events (eg, IOL dislocation, clinically significant decentration, or tilt) were recorded. Likewise, no case of postoperative glistening was observed in the current study.
Discussion
The implantation of the CT LUCIA 621P IOL in the current study resulted in good visual acuity and predictable refractive outcomes. Of all eyes, 84.8% were within 0.50 D of emmetropia, and almost all eyes (98.4%) were within 1.00 D of emmetropia. The correlation between attempted and achieved manifest spherical equivalent (Figure 4) was tight, with only three outliers outside of the ±1.00 D guidelines, but no eye in the study had ametropia of more than +1.125 D. To date, there is only one study reporting clinical outcomes with this particular IOL in a cohort of 86 patients (90 eyes).12 The authors report 73.33% of eyes within 0.50 D of emmetropia, but the postoperative MSE of their cohort was slightly myopic (−0.18 ± 0.55 D) compared to our MSE which was slightly hyperopic (+0.15 ± 0.38 D). This could simply be the difference in the surgeon’s preference for postoperative aim or optimization of the lens constant.
Unfortunately, the short follow-up time precluded us from calculating the refractive stability of MSE over time. The predecessor of CT LUCIA 621P, the CT LUCIA 611P model, which shares a very similar platform, was found to have excellent postoperative refractive stability as well as axial stability in the capsular bag. In the Investigation Device Exemption (IDE) CT LUCIA 611P study for the US Food and Drug Administration (FDA) approval, there was no statistically significant change in MSE between 1 week, 1 month, 6 months, and 1 year exams in a consecutive cohort of 308 patients.6 In a smaller study, Hienert et al9 measured postoperative anterior chamber depth change using a swept-source optical coherence tomography device (IOLMaster 700) and found that CT LUCIA 611P exhibited minimal movement dynamics within the first 6 postoperative months. Overall, the mean anterior chamber depth (ACD) change between the first postoperative visit (1 week) and the last visit (4 to 6 months) was only −0.06 ± 0.16 mm. In a bench study13 comparing the geometry of five commercially available hydrophobic acrylic single-piece IOLs, all haptic dimensions (length, thickness, surface area, volume) and all optic-haptic junction dimensions (surface area and volume) were greatest for the CT LUCIA 621PY IOL (blue-light filtering equivalent of our study IOL), suggesting these features could be advantageous for biomechanical stability of this IOL.
In the current study, no adverse events related to intraoperative surgical manipulation or postoperative stability of the IOL in the capsular bag were noted. There was no case of postoperative clinically significant intraocular lens tilt, decentration, or IOL displacement. In fact, in a small case series,8 the previous CT LUCIA 611P lens model was used in complicated cataract cases susceptible to lens dislocation or decentration. Authors postulated that robust design with thicker and wider optic-haptic junction, as well as the overall IOL length of 13 mm, likely contributed to the overall stability of the IOL in the capsular bag in eyes prone to IOL dislocation.8 Considering CT LUCIA 621P has a very similar haptics configuration as CT LUCIA 611P, the same stability should be expected.
Biocompatibility of IOL materials has been the subject of intense scrutiny in recent years. We have not observed any major adverse events that could potentially be related to the biocompatibility of the lens material, such as persistent inflammation, toxic anterior segment syndrome, postoperative glistening, or excessive posterior capsule opacification. However, the follow-up of our cohort was too short to address some of these events. The hydrophobic material with the same composition of polymers as CT LUCIA 621P has been used in a few other lens models for almost two decades and has not been associated with significant cases of glistening. For example, in the large IDE study of CT LUCIA 611P,6 which is also made of the same material, there was no case of glistening over the one-year follow-up. Likewise, in another long-term prospective study,7 no glistening at all was reported for the CT LUCIA 611P model over a one-year period. Nevertheless, inconsistent degrees of glistening have been observed for CT LUCIA 611P14 IOL and a similar model made of the same material (CT LUCIA 601P15,16) in the laboratory (in-vitro) settings using accelerated aging simulation. However, laboratory-based testing methods and the temperature shock the lenses are exposed to during testing might not always resample the performance of the IOL in-vivo. In clinical practice, glistening has not been a significant issue with the material of the study IOL.
In our case series, five eyes showed minor PCO signs, but these were likely related to the surgery and dense preoperative cataract rather than the IOL not providing an adequate barrier for lens epithelial cells migration because the PCO was mostly present from postoperative day one. The follow-up of our cohort was not sufficient to elucidate long-term PCO development. CT LUCIA 611P and CT LUCIA 621P share the same geometric features for PCO prevention. These include the same IOL material and haptic configuration, step-vaulted design for better contact with the posterior capsule, and the 360-degree posterior square edge (with no interruption at the optic/haptic junction). In laboratory studies, IOLs from the CT LUCIA range have been found to have some superior qualities in terms of PCO protection. For instance, a study by Nanavaty17 showed that CT LUCIA had the sharpest posterior edge among fourteen commercially used hydrophobic and hydrophilic IOLs. Additionally, the aforementioned bench study of five hydrophobic IOLs13 used a range of compression well diameters (9 to 11.5 mm) to simulate the potential behavior of these lenses in a shrinking capsular bag. The study found that CT LUCIA 621PY had the greatest angle of contact and capsular bag contact values for all well sizes and the smallest percentage change in angle of contact and capsular bag contact between the 9- and 11.5-mm compression wells. Additionally, in a laboratory study of Wormstone et al,10 using a human capsular bag model, CT LUCIA 611PY remained stable in the capsular bag despite the expected postoperative distortion of the capsular bag and the optic edge of the IOL showed an enhanced barrier function.
To date, there are only three studies that evaluate long-term (cumulative one-year incidence) PCO rates with the CT LUCIA 611P IOL. In a prospective study of 96 eyes,7 two cases of Nd:YAG capsulotomy were reported within the first year (both had mature white cataracts and primary PCO requiring capsulotomy at 8–10 weeks), and one eye required Nd:YAG capsulotomy after the one year visit. The CT LUCIA 611P IDE study6 reported a 3.5% Nd:YAG capsulotomy rate at 1 year, but most of the patients still had reasonable CDVA ahead of capsulotomy. A study by Ling et al18 found PCO-related Nd:YAG capsulotomy rates of 3.5% at one year and 8.5% at 2 years in 200 real-world unselected cataract patients with a variety of conditions that could exacerbate PCO development. Further, long-term studies are required to assess the real clinical rate of PCO development with IOLs from the CT LUCIA range.
Unfortunately, this study was not able to address the non-constant aberration-correcting feature of this IOL. A previous study by Liu et al4 found that a non-constant aberration IOL had significantly better postoperative intraocular stray light and a lower value of total ocular coma than two aberration-correcting IOLs with a constant value of negative spherical aberration. The optical concept of the IOL was derived from a theoretical eye model, and more studies are required to assess its advantages in real patients, especially its presumed higher tolerance to postoperative IOL decentration.
The current study has several limitations. The data used in the analysis were collected retrospectively, and the follow-up time was relatively short. Adverse events, biocompatibility, or refractive stability require long-term evaluation. Assessment of postoperative higher-order aberrations, contrast sensitivity, visual symptoms, or visual symptoms change in cases of IOL decentration would be valuable, however, this analysis was not possible in our current retrospective study.
Conclusion
Despite the limitations outlined, our initial experience with the CT LUCIA 621P IOL in terms of surgical workflow and refractive outcomes was positive. Some features of the IOL warrant further research, ideally in a larger prospective study.
Disclosure
Steven Schallhorn is a chief medical officer for Carl Zeiss Meditec and a chairman of medical advisory board for Optical Express. Stephen Hannan, Jan Venter, and David Teenan are employees of Optical Express. Julie Schallhorn received personal fees from Carl Zeiss Meditec, Allergan, Long Bridge, and Forsight V6 and has a financial interest in Journey 1, Neurotrigger, and Novus Vision. The authors report no other conflicts of interest in this work.
References
1. Taketani F, Yukawa E, Yoshii T, Sugie Y, Hara Y. Influence of intraocular lens optical design on high-order aberrations. J Cataract Refract Surg. 2005;31(5):969–972. doi:10.1016/j.jcrs.2004.10.064
2. Schuster AK, Tesarz J, Vossmerbaeumer U. Ocular wavefront analysis of aspheric compared with spherical monofocal intraocular lenses in cataract surgery: systematic review with metaanalysis. J Cataract Refract Surg. 2015;41(5):1088–1097. doi:10.1016/j.jcrs.2015.04.005
3. Lawu T, Mukai K, Matsushima H, Senoo T. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J Cataract Refract Surg. 2019;45(5):662–668. doi:10.1016/j.jcrs.2018.10.049
4. Liu Y, Zhao J, Hu Y, Li B, Wang J, Zhang J. Comparison of the visual performance after implantation of three aberration-correcting aspherical intraocular lens. Curr Eye Res. 2021;46(3):333–340. doi:10.1080/02713683.2020.1798467
5. Schmid R. Early experience with the aspheric CT LUCIA 621P IOL. Host of design features add up to reliable optical performance. Ophthalmology Times. Available from: https://europe.ophthalmologytimes.com/microsites/zeiss-cataract-laser-vision-correction-cases/assets/f130cd99d6f6af815c3e70991df9b147-zeiss_case_of_the_month_10-20_en_32_025_0053i_screen.pdf.
6. Schallhorn SC, Bonilla M, Pantanelli SM. Outcomes of a multicenter U.S. clinical trial of a new monofocal single-piece hydrophobic acrylic IOL. J Cataract Refract Surg. 2022;48(10):1126–1133. doi:10.1097/j.jcrs.0000000000000943
7. Borkenstein AF, Borkenstein EM. Long-term clinical results and scanning electron microscopic analysis of the aspheric, hydrophobic, acrylic intraocular lens CT LUCIA 611P(Y). Clin Ophthalmol. 2018;12:1219–1227. doi:10.2147/OPTH.S167895
8. Borkenstein AF, Borkenstein EM. Surgical experience with a redesigned, fully preloaded, hydrophobic acrylic intraocular lens in challenging cases of pseudoexfoliation syndrome, phacodonesis, and small pupils. Clin Ophthalmol. 2019;13:199–206. doi:10.2147/OPTH.S194420
9. Hienert J, Hirnschall N, Ruiss M, Ullrich M, Zwickl H, Findl O. Prospective study to compare axial position stability after fellow-eye implantation of 2 distinct intraocular lens designs. J Cataract Refract Surg. 2021;47(8):999–1005. doi:10.1097/j.jcrs.0000000000000557
10. Wormstone IM, Damm NB, Kelp M, Eldred JA. Assessment of intraocular lens/capsular bag biomechanical interactions following cataract surgery in a human in vitro graded culture capsular bag model. Exp Eye Res. 2021;205(108487). doi:10.1016/j.exer.2021.108487
11. Liou HL, Brennan NA. Anatomically accurate, finite model eye for optical modeling. J Opt Soc Am Opt Image Sci Vis. 1997;14(8):1684–1695. doi:10.1364/josaa.14.001684
12. Hernandez-Martinez A, Diaz-Del-Rio MA, Ruiz-Santos M, Ruiz-Mesa R, Tana-Rivero P. Refractive and visual outcomes of a monofocal non-constant aberration aspheric intraocular lens. Clin Ophthalmol. 2022;16:2521–2530. doi:10.2147/OPTH.S373587
13. Borkenstein AF, Borkenstein EM. Geometry of acrylic, hydrophobic IOLs and changes in haptic-capsular bag relationship according to compression and different well diameters: a bench study using computed tomography. Ophthalmol Ther. 2022;11(2):711–727. doi:10.1007/s40123-022-00469-z
14. Yildirim TM, Schickhardt SK, Wang Q, Friedmann E, Khoramnia R, Auffarth GU. Quantitative evaluation of microvacuole formation in five intraocular lens models made of different hydrophobic materials. PLoS One. 2021;16(4):e0250860. doi:10.1371/journal.pone.0250860
15. Labuz G, Knebel D, Auffarth GU, et al. Glistening formation and light scattering in six hydrophobic-acrylic intraocular lenses. Am J Ophthalmol. 2018;196:112–120. doi:10.1016/j.ajo.2018.08.032
16. Tandogan T, Auffarth GU, Son HS, Merz P, Choi CY, Khoramnia R. In-vitro glistening formation in six different foldable hydrophobic intraocular lenses. BMC Ophthalmol. 2021;21(1):126. doi:10.1186/s12886-021-01879-6
17. Nanavaty MA, Zukaite I, Salvage J. Edge profile of commercially available square-edged intraocular lenses: part 2. J Cataract Refract Surg. 2019;45(6):847–853. doi:10.1016/j.jcrs.2018.12.004
18. Ling R, Borkenstein EM, Borkenstein AF. Evaluation of Nd:YAG laser capsulotomy rates in a real-life population. Clin Ophthalmol. 2020;14:3249–3257. doi:10.2147/OPTH.S276329
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
