Back to Journals » Patient Preference and Adherence » Volume 17
Drug Attitude and Medication Adherence of Patients with Early Psychosis in South Korea: Mediating Effect of Medication Adherence Self-Efficacy
Received 16 February 2023
Accepted for publication 6 May 2023
Published 12 May 2023 Volume 2023:17 Pages 1247—1255
DOI https://doi.org/10.2147/PPA.S408781
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Yoon-A Choi,1 Young-Ran Kweon2
1Department of Nursing, Chonnam National University Hospital, Gwangju, South Korea; 2Department of Nursing, Chonnam National University, Gwangju, South Korea
Correspondence: Young-Ran Kweon, Department of Nursing, Chonnam National University, P.O. Box 61469, 60 Baekseo-ro, Dong-gu, Gwangju, South Korea, Tel +82 62 530 4966, Fax +82 62 220 4544, Email [email protected]
Purpose: This study examined the mediating effect of medication adherence self-efficacy (MASE) on the relationship between drug attitude (DA) and medication adherence (MA) in patients with early psychosis.
Patients and Methods: A total of 166 patients, aged 20 years or older, and who had received treatment within 5 years of their initial psychotic episode at a University Hospital outpatient center, participated in the study. Data were analyzed using descriptive statistics, t-tests, one-way analysis of variance, Pearson’s correlation coefficients, and multiple linear regression. Additionally, a bootstrapping test was conducted to determine the statistical significance of the mediating effect. All study procedures adhered to Strengthening the reporting of observational studies in epidemiology (STROBE) guidelines.
Results: This study found a significant correlation between MA and DA (r=0.393, p< 0.001), and between MA and MASE (r=0.697, p< 0.001). MASE had a partial mediating effect on the association between DA and MA. The model that integrated both DA and MASE accounted for 53.4% of the variation in MA. Bootstrapping analysis indicated that MASE was a significant partial parameter (lower limit confidence interval [CI] 0.114; upper limit CI 0.356). Further, 64.5% of the study participants were either currently enrolled in college or had higher levels of education.
Conclusion: These findings could potentially lead to a more personalized approach to medication education and adherence, considering the unique DA and MASE of each patient. By identifying the mediating effect of MASE on the relationship between DA and MA, healthcare providers could tailor interventions to enhance the ability of patients with early psychosis to adhere to prescribed medication regimens.
Keywords: drug attitude, early psychosis, mediating effect, medication adherence, self-efficacy
Introduction
Mental illnesses are conditions that occur mainly in puberty, with exacerbations and remission, and difficulties in maintaining independence and social life. Schizophrenia, for example, is characterized by worsening symptoms within the first 5 years of onset, followed by chronic symptoms during subsequent periods.1 Therefore, providing appropriate interventions for functional restoration during the early stages of psychosis is crucial to prevent functional deterioration.2 In recent years, there has been growing recognition of the critical period in the treatment of psychosis. Early detection and intervention within 5 years of the initial psychotic episode positively impact patient prognosis. This critical period is characterized by high levels of vulnerability and opportunities for maximum recovery.3
However, despite the importance of early intervention, previous studies have shown that many patients with schizophrenia experience relapse, with 53.7% of patients relapsing after 2 years and 81.9% relapsing after 5 years, largely due to discontinuation of drug treatment.4,5 Therefore, one of the main concerns during the early treatment of psychosis is whether patients receive sufficient drug therapy. Typically, nonadherence with drug therapy is reported as 40% within 1 year, and 75% within 2 years.6 Such nonadherence leads to significant social and psychological consequences and to a major influence on the disease;7–9 therefore, it is particularly important to help patients with early psychosis engage in successful drug therapy to prevent remission and chronicity.
Medication adherence (MA) is a behavioral outcome that reflects the degree to which patients follow the prescribed medication regimen, and is a significant predictor of treatment outcomes among individuals with early psychosis.8 The most effective treatment for early psychosis is long-term maintenance therapy with antipsychotic drugs, and patients who follow their medication regimens consistently experience marked symptom improvement (55–81% decrease in symptoms).10–12 However, even after experiencing high response rates to early drug therapy, patients with early psychosis tend to overlook the importance of long-term maintenance therapy.13 Therefore, managing patients’ attitudes towards drug therapy is crucial to improve MA rates.
A negative attitude towards drug therapy is the main reason why patients with psychosis often discontinue treatment.14 However, a previous study in patients with schizophrenia admitted to hospital within 2 years of initial diagnosis reported a treatment success rate of 64.3% for patients with a positive DA and who consistently received drug treatment.7 In addition, Hsieh et al reported that DA directly affects MA in individuals with schizophrenia residing in the community,15 and previous several studies suggest that a positive DA can increase MA rates.8,16 Thus, to improve MA in patients with schizophrenia, healthcare professionals should adopt a personalized medication education approach that considers individual DA, and health providers for patients with early psychosis should aim to increase DA to raise MA and ultimately improve patients’ quality of life.
Medication adherence self-efficacy (MASE) reflects a patient’s confidence in taking medications regularly and correctly, despite potential barriers or challenges.17 Although there has been limited research on MASE in patients with psychosis, MASE is a significant factor that affects MA, particularly in patients with conditions such as hypertension and diabetes.18,19 According to Beebe et al, there was a strong correlation between MASE and MA in patients with psychosis.20 The study found that patients who could self-administer medication had a higher likelihood of following a prescribed medication regimen. Also, in the planned behavior theory, attitudes are manifested into behaviors through beliefs as a mediator.21 Therefore, it is necessary to investigate whether MASE affects between DA and MA in patients with early psychosis.
The goal of the current study was to explore whether MASE acts as a mediator between DA and MA in individuals with early psychosis. The results of the study will be used as basic data to develop strategies to improve MA in patients with early psychosis.
Materials and Methods
Study Design and Participants
This study applied a descriptive, cross-sectional, quantitative design, with a self-reported survey (including a Likert-scale questionnaire), in patients with early psychosis using outpatient services.
Patients were aged ≥20 years and were using outpatient services at the Chonnam National University Hospital, South Korea. The patients had a first psychotic episode and had been diagnosed with a schizophrenia spectrum disorder (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) by a psychiatrist. The onset of psychotic symptoms, and subsequent treatment, occurred within a 5-year period.
Specific inclusion criteria comprised patients: currently undergoing outpatient treatment after being diagnosed with schizophrenia following first-episode psychosis; taking antipsychotic drugs; and capable of understanding, writing, and responding to the questionnaire independently. Exclusion criteria comprised: a score of ≥4 on the Clinical Global Impression (CGI) scale,22 as assessed by the case manager, to evaluate symptom severity and functional impairments; any relationship between current symptoms and substance use or substance use disorder; other mental or neurologic diseases; severe somatic diseases; difficulties in understanding and participating in the study due to cognitive dysfunction; and long-term injectable antipsychotic therapy.
The sample size was calculated using the G*Power 3.1.9 program. A minimum sample size of 160 was required for regression analysis using a significance level (α) of 0.05, power (1–β) 0.85, effect size (medium) 0.15, and nine predictor variables. The study collected a total of 190 data sets, including dropouts.
Procedure for Data Collection
Data were collected from June 1, 2019 to August 16, 2019. Patients with early psychosis at the outpatient center at Chonnam National University Hospital were given the study rationale and provided written consent for voluntary participation. The time taken to complete the study questionnaire was about 10–15 minutes, during the waiting period before outpatient attention.
The questionnaire was provided to 190 patients. Overall, 24 patients were excluded for the following reasons: receiving long-term injectable antipsychotic therapy (n=15); declined to participate (n=8); or not receiving drug therapy, but continuing outpatient counselling (n=1). Thus, the total data set for the final analysis was 166 patients.
Survey Instruments
Previous research has shown that socio-demographic factors, such as educational, insurance, socioeconomic, and marital status, and family relationships, are related to MA in patients with schizophrenia.23 Therefore, in this study, we investigated 11 socio-demographic characteristics. To collect data, we used three self-reported instruments: DA, MASE, and MA. Before using these instruments, we obtained permission from the original authors and translators via email.
Drug Attitude
DA was measured using the DA Inventory-10, translated into Korean.24,25 This scale asks about attitudes towards drugs. It comprises six items that evaluate subjective positive feelings regarding antipsychotic drugs, and four items that evaluate subjective negative feelings. Questions answered “yes” are assigned one point, and those answered “no” are assigned minus one point. The scores from the two sections are totaled and the final score is calculated. A positive final score indicates a subjective positive response to the drug, and a negative score indicates a subjective negative response. In this study, the Kuder-Richardson Formula 20 (KR-20) value was 0.70.
Medication Adherence Self-Efficacy
MASE was measured using the drug-related self-efficacy scale developed by Seo, revised by patients with mental illness, and supplemented by Lee & Kim.26,27 This scale measures the type of drugs and administration times, the degree of drug-dosage adherence, side effects, economic burden, and confidence in adhering to drug therapy despite its long-term nature. This scale comprises a total of eight items measured on a five-point Likert scale from one point (“not at all”) to five points (“always”), and the total score ranges from 8–40, where higher scores indicate higher MASE; Cronbach’s α was 0.83.
Medication Adherence
MA measured the extent of adherence to medication by patients with mental illness, using the tool initially developed by Thompson et al and translated and supplemented by Chang et al28,29 The scale comprises seven items, and questions are measured on a five-point Likert scale, ranging from 7–35, where a higher score indicates higher MA; Cronbach’s α was 0.85.
Statistical Analyses
Data were analyzed using IBM SPSS version 25.0 (SPSS Inc.; Chicago, IL, USA). First, frequency analysis was performed to identify demographic and clinical characteristics. Second, analysis of descriptive statistics was conducted to identify the mean and standard deviation of research variables and skewness and kurtosis. Third, the t-test and one-way ANOVA were used to examine differences in MA by demographic characteristics. Fourth, Pearson’s correlation coefficient analysis was conducted to assess the relationship between study variables. Fifth, to determine whether MASE served as a mediator between DA and MA, multiple linear regression analysis was performed according to the method proposed by Baron and Kenny.30
Finally, the statistical significance of the mediating effect of MASE was verified using a bootstrapping method with the SPSS Process Macro (model 4, version 3.4, written by Andrew F. Hayes).31 The bootstrapping method had a higher statistical power and more accurate type I error rate than the Sobel test, even in small samples. Bootstrapping, as used in mediation, simply resamples data naively with replacement of several times (eg 5000) and, for each sample, estimates of the indirect effect are obtained. Specifically, we calculated a 95% confidence interval (CI) with 5000 bootstrap resamples to determine if MASE helped to explain the association between DA and MA in patients with early psychosis.
Ethical Considerations
This study was approved by the Institutional Review Board at Chonnam National University Hospital (IRB no. CNUH-2019-156). The questionnaire was administered after obtaining written informed consent from all patients to participate. All procedures were conducted in accordance with ethical standards of the Helsinki Declaration.
Results
Demographic Characteristics
Demographic characteristics for the study participants are shown in Table 1. Overall, 47.6% of participants were male, mean age was 27.8 years, and 64.5% of participants were either currently enrolled in college or had higher education levels. Regarding relationship with the family, 127 participants (76.5%) responded “good”, and MA improved with higher ratings (F=7.64, p<0.001). Mean age of the first psychotic episode was 25.4 years; 68 patients (41.0%) had never been hospitalized, and 98 (59.0%) had been hospitalized once or more. A total of 115 patients responded that they managed medication by themselves (69.3%), which was significantly greater than the proportion who did not self-manage their medication (t=–3.16, p<0.01).
 |
Table 1 Participant Characteristics, and Differences in Medication Adherence by Characteristics |
Descriptive Statistics for Major Variables
Descriptive statistics for the major research variables are shown in Table 2. Mean scores for DA, MASE, and MA were 4.18, 33.44, and 30.27 points, respectively. All variables did not exceed an absolute value for skewness of 3.0, and an absolute value for kurtosis of 10.0, thus satisfying univariate normality.
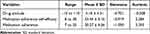 |
Table 2 Descriptive Statistics for Major Variables |
Correlations Between Major Variables
The relationships between major variables are shown in Table 3. MA showed a significant correlation with all variables. Specifically, MA was positively correlated with DA (r=0.393, p<0.001) and MASE (r=0.697, p<0.001). Also, DA was positively correlated with MASE (r=0.334, p<0.001).
 |
Table 3 Correlations Among Major Variables |
Mediating Effects of MASE Between DA and MA
The results of the mediating effects of MASE on the DA and MA relationship in patients with early psychosis are shown in Table 4. The regression analysis included variables that influenced MA, such as patient relationship with the primary caregiver, as a covariate. The Durbin-Watson statistic ranged from 1.973–2.028, which was close to 2, and considered appropriate for the independence of residual assumption; further, the variance inflation factor was <10, eliminating the issue of multicollinearity. The three-step method was used to analyze the mediating effect. In the first step, we analyzed the effect of DA on MASE as a mediating variable. This confirmed that DA had a significant effect on MASE (β=0.334, p<0.001). In step two, we analyzed the effect of DA on MA as a dependent variable, and DA had a significant effect on MA (β=0.386, p<0.001). In the third step, MASE was added as an independent variable, along with DA, and MA was added as a dependent variable: DA had a statistically significant effect on MA (β=0.172, p<0.01), and MASE also had a significant effect on MA (β=0.660, p<0.001). These results suggest that DA and MA are partially mediated by MASE. DA explained 14.4% of the variance in MA, and the model including DA and MASE explained 53.4% of the variance in MA.
 |
Table 4 Mediating Effects of MASE on the Relationship Between DA and MA |
Table 5 shows the direct and indirect effects of the mediating variable. As a result of the mediating-effect test, the indirect effect of MASE on the relationship between DA and MA did not include zero between the lower limit value (0.124) and the upper limit value (0.361) of the confidence level; therefore, this effect was statistically significant.
 |
Table 5 Verification of the Bootstrapping Mediation Effect |
Discussion
This study attempted to explore the role of MASE in the relationship between DA and MA in patients with early psychosis, and to critically examine relevant literature and empiric evidence to provide a comprehensive suggestion of strategies to enhance treatment adherence.
The mean age of study participants was 27.8 years, which is similar to findings in previous studies in patients with early psychosis.32 Patients were residing with their parents, with a significant proportion of patients having education levels greater than high school. In 200 patients who participated in an early psychosis program in Calgary, Canada for 3 years, 87% of participants were single, 78% resided with their families, and mean age was 23.6 years.33 Thus, it is necessary to provide mental health services to manage early psychotic symptoms, medication, and issues pertinent to young adults, such as employment and family relationships. In addition, appropriate customized services are required to meet patients’ needs regarding developmental stage, improved quality of life, and treatment outcomes.
This study showed high levels of DA and MA in patients with early psychosis: in particular, the mean score for DA was 4.18 points, which was high compared to patients with chronic schizophrenia treated for more than 5 years (mean 2.99 or 3.96 points).34,35 Also, the mean score for MA was 30.27 points, which was slightly higher than the score inpatients with chronic schizophrenia treated in hospital (mean 29.49 points).25 These results were considered attributable to symptom remission and stable rates of maintenance therapy in most of the patients with early psychosis who participated in the study. Our results also suggested a favorable effect for family support on MA in patients with first-episode psychiatric problems.36,37 Our study findings may have been influenced by the young age of the participants and their reliance on family support. However, Quach et al found that patients controlling versus not controlling their own medication management had better MA.36 This suggests that patients who are actively involved in their own healthcare, and who take responsibility for their own medication management, may be more likely to adhere to their medication regimens. In addition, interventions that focus on supportive counseling and motivational treatment could be effective in improving MA in patients with early psychosis who manage their own medication. Therefore, we recommend that healthcare providers encourage both family support and self-management of medication to enhance MA in this population.
Our study also revealed strong correlations between DA and MA in patients with early psychosis, which agrees with a previous study.38 Patients’ negative DAs during first-episode psychosis are reportedly the most powerful predictors of poor MA at 1 and 2 years of follow-up.39 The most frequent reasons for negative DAs are denial of illness, rejection of the need for medication, no perceived benefit from medication, and fear of stigma and substance abuse.40 Nevertheless, to some extent, the beneficial effects of antipsychotic drugs have changed patients’ views and made it easier for patients to adhere to drug therapy.41 Thus, to improve MA among patients with schizophrenia, healthcare professionals should adopt for a personalized medication education approach that considers individual DA.
MASE in patients with early psychosis had a positive correlation with DA and MA in this study. Consequently, the higher the MASE, the higher the DA and MA, which is similar to previous studies,17,41 in which MA and MASE scores were significantly correlated. These results provide evidence of planned behavior, whereby adherence intent is determined, in part, by perceived behavioral control, which reflects the level of confidence in one’s own ability to modify behavior.42 Perceived behavioral control was “operationalized” as MASE in this study. That is, the higher a patient’s MASE, the higher was MA. Thus, we should encourage MA in patients with early psychosis by increasing MASE.
Finally, the main contribution of this study is to highlight that DA may affect MA in patients with early psychosis via a mediating mechanism of MASE. Our study suggests that DA explained 14.4% of the variance in MA, and the model including DA and MASE explained 53.4% of the variance in MA. We found that DA directly affects MA, and MASE indirectly affects MA. DA level was a unique predictor of MA in patients with mental health problems. Unequivocally, DA and MA are closely related.43 Adherence studies in schizophrenia also consistently reported that service users’ beliefs about MASE had primacy over side effects in influencing MA.44 Above all, MASE will have a positive effect in patients with early psychosis who are in a critical period of clinical treatment. Importantly, MASE will likely contribute to improvements in the quality of psychiatric nursing care and patient-centered nursing. Our findings emphasize the importance of developing patients’ MASE in fostering improvements in patient quality of care.
These study findings reveal a noteworthy association between DA, MASE, and MA, whereby MASE partially mediated the relationship between DA and MA. These results suggest that interventions aimed at enhancing MASE may indirectly augment the impact of DA on MA. However, it is crucial to devise and implement education and intervention strategies for promoting MASE, and to verify the effectiveness of such strategies through randomized controlled trials. Such trials could facilitate the establishment of causal relationships between DA, MASE, and offer insights for developing effective interventions to improve MA in patients with early psychosis.
A limitation of our research is the cross-sectional study design, which allows relationships between variables to be identified at one timepoint only and does not allow causal relationships among variables to be established. Therefore, to better understand adherence in patients with early psychosis, longitudinal designs are recommended for future studies. In addition, data from the analyses in this study were excluded for 12.6% of participants. As missing data may have affected the study results, careful interpretation is required.
Conclusion
In this study, MASE was identified as a major predictor of MA, and also had a partial mediating effect on DA and MA, in patients with early psychosis. Therefore, to improve MA in patients with early psychosis, MASE should be improved by developing and implementing appropriate intervention programs. Education on medication should be provided to build an internal motivation to promote MASE.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to respondents’ confidentiality but are available from the corresponding author on reasonable request.
Informed Consent Statement
Informed consent was obtained from all study participants before participation in this study. All participants were informed that no personal identifying information was collected.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board at Chonnam National University Hospital (IRB no. CNUH-2019-156).
Acknowledgments
The authors would like to thank all participants who volunteered their time to participate in the study. Also, we would like to thank the collaborating authors for their contributions.
Author Contributions
All authors made a significant contribution to the work reported, whether in conception, study design, execution, data acquisition, analysis, and interpretation, or in all these areas; or in drafting, revising, or critical review of the article. All authors approved the final version to be published, agreed on the journal for article submission, and agreed to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest.
References
1. Coentre R, Levy P, Figueira ML. Early intervention in psychosis: first-episode psychosis and critical period. Acta Med Port. 2011;24(1):117–126. doi:10.20344/amp.336
2. Onitsuka T, Hirano Y, Nakazawa T, et al. Toward recovery in schizophrenia: current concepts, findings, and future research directions. Psychiatry Clin Neurosci. 2022;76(7):282–291. doi:10.1111/pcn.13342
3. Shah JL, Jones N, van Os J, McGorry PD, Gülöksüz S. Early intervention service systems for youth mental health: integrating pluripotentiality, clinical staging, and transdiagnostic lessons from early psychosis. Lancet Psychiatry. 2022;9(5):413–422. doi:10.1016/S2215-0366(21)00467-3
4. Gilbert PL. Neuroleptic withdrawal in schizophrenic patients: a review of the literature. Arch Gen Psychiatry. 1995;52(3):173–188. doi:10.1001/archpsyc.1995.03950150005001
5. Robinson D, Woerner MG, Alvir JMJ, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56(3):241–247. doi:10.1001/archpsyc.56.3.241
6. Leucht S, Heres S. Epidemiology, clinical consequences, and psychosocial treatment of nonadherence in schizophrenia. J Clin Psychiatry. 2006;67(suppl 5):3–8.
7. Perki P, Faivre N, Urbach M, et al. Relationships between neuropsychological performance, insight, medication adherence, and social metacognition in schizophrenia. Schizophr Res. 2023;252:48–55. doi:10.1016/j.schres.2022.12.037
8. Raghavan V, Mohan G, Gopal S, Ramamurthy M, Rangaswamy T. Medication adherence in first-episode psychosis and its association with psychopathology. Indian J Psychiatry. 2019;61(4):342–346. doi:10.4103/psychiatry.IndianJPsychiatry_148_17
9. Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114:169–179. doi:10.1093/bmb/ldv017
10. Bola JR, Kao D, Soydan H, Adams CE. Antipsychotic medication for early episode schizophrenia. Cochrane Database Syst Rev. 2011;6. doi:10.1002/14651858.CD006374.pub2
11. Lieberman JA, Tollefson G, Tohen M, et al. Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry. 2003;160(8):1396–1404. doi:10.1176/appi.ajp.160.8.1396
12. Merlo MC, Hofer H, Gekle W, et al. Risperidone, 2 mg/day vs. 4 mg/day, in first-episode, acutely psychotic patients: treatment efficacy and effects on fine motor functioning. J Clin Psychiat. 2002;63(10):18580.2002, 63, 885–891. doi:10.4088/jcp.v63n1006
13. Kim J, Park Y, Shin K, Jung Y. Pharmacotherapeutic strategies to prevent relapse in schizophrenia. J Korean Neuropsychiatr Assoc. 2018;57:225–229. doi:10.4306/jknpa.2018.57.3.225
14. Mutsatsa SH, Joyce E, Hutton S, et al. Clinical correlates of early medication adherence: west London first episode schizophrenia study. Acta Psychiatr Scand. 2003;108(6):439–446. doi:10.1046/j.0001-690x.2003.00193
15. Hsieh WL, Yeh ST, Liu WI, Li IH, Lee SK, Chien WT. Improving medication adherence in community-dwelling patients with schizophrenia through therapeutic alliance and medication attitude: a serial multiple mediation model. Patient Prefer Adherence. 2022;13:1017–1026. doi:10.2147/PPA.S351
16. Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. 2020;9. doi:10.1186/s13643-020-1274-3
17. Fernandez S, Chaplin W, Schoenthaler AM, Ogedegbe G. Revision and validation of the medication adherence self-efficacy scale (MASES) in hypertensive African Americans. J Behav Med. 2008;31(6):453–462. doi:10.1007/s10865-008-9170-7
18. Shahin W, Kennedy GA, Cockshaw W, Stupans I. The role of medication beliefs on medication adherence in Middle Eastern refugees and migrants diagnosed with hypertension in Australia. Patient Prefer Adherence. 2020;3:2163–2173. doi:10.2147/PPA.S27433
19. Huang YM, Shiyanbola OO, Chan HY. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ Couns. 2018;101(11):1906–1913. doi:10.1016/j.pec.2018.06.010
20. Beebe LH, Smith K, Phillips C. Descriptions and correlates of medication adherence, attitudes, and self-efficacy in outpatients with schizophrenia spectrum disorders (SSDs). Arch Psychiat Nurs. 2016;30(3):400–405. doi:10.1016/j.apnu.2016.01.010
21. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
22. Guy W ECDEU assessment manual for psychopharmacology. US Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976.
23. Acosta FJ, Hernández JL, Pereira J, Herrera J, Rodríguez CJ. Medication adherence in schizophrenia. World J Psychiatry. 2012;2(5):74. doi:10.5498/wjp.v2.i5.74
24. Phan SV. Medication adherence in patients with schizophrenia. Int J Psychiatry Med. 2016;51:211–219. doi:10.1177/00912174166366
25. Yoon B, Park W, Lee K, Hong C, Ahn J, Kim M. The psychometric characteristics of the Korean version of the drug attitude inventory(KDAI-10). Korean J Psycho Pha. 2005;16:480–487.
26. Seo YM. Factors influencing medication adherence in hypertensive patients. J Korean Acad Comm Health Nurs. 2010;21:82–91. doi:10.12799/jkachn.2010.21.1.82
27. Lee D, Kim S. The effects of group motivational interviewing compliance therapy on drug attitude, medicine application self-efficacy and medicine application in psychiatric patients. J Korean Acad Psychiatr Ment Health Nurs. 2017;26:391–401. doi:10.12934/jkpmhn.2017.26.4.391
28. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new medication adherence rating scale (Mars) for the psychoses. Schizophr Res. 2000;42:241–247. doi:10.1016/s0920-9964(99)00130-9
29. Chang JG, Roh D, Kim CH. The reliability and validity of the Korean version of medication adherence rating scale. Korean J Psychopharmacol. 2015;26:43–49.
30. Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psycho. 1986;51(6):1173. doi:10.1037/0022-3514.51.6.1173
31. Hayes AF, Scharkow M. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: does method really matter? Psychol Sci. 2013;24(10):1918–1927. doi:10.1177/0956797613480187
32. Addington J, Young J, Addington D. Social outcome in early psychosis. Psychol Med. 2003;33(6):1119–1124. doi:10.1017/S0033291703007815
33. Coldham EL, Addington J, Addington D. Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand. 2002;106(4):286–290. doi:10.1034/j.1600-0447.2002.02437.x
34. Lim H, Kim S, Kim J, Ha K, Park H. Factors related to medication adherence in outpatients with schizophrenia under more than 5 years of treatment. J Korean Neuropsychiatr Assoc. 2016;55(4):397–406. doi:10.4306/jknpa.2016.55.4.397
35. Bozzatello P, Giordano B, Montemagni C, Rocca P, Bellino S. Real-world functioning in psychiatric outpatients: predictive factors. J Clin Med. 2022;11(15):4400. doi:10.3390/jcm11154400
36. Quach PL, Mors O, Christensen TØ, et al. Predictors of poor adherence to medication among patients with first‐episode schizophrenia‐spectrum disorder. Early Interv Psychiatry. 2009;3(1):66–74. doi:10.1111/j.1751-7893.2008.00108.x
37. Rabinovitch M, Béchard-Evans L, Schmitz N, Joober R, Malla A. Early predictors of nonadherence to antipsychotic therapy in first-episode psychosis. Can J Psychiatry. 2009;54(1):28–35. doi:10.1177/070674370905400106
38. Yeisen RA, Bjornestad J, Joa I, Johannessen JO, Opjordsmoen S. Experiences of antipsychotic use in patients with early psychosis: a two-year follow-up study. BMC Psychiatry. 2017;17(1):1–10. doi:10.1186/s12888-017-1425-9
39. Jonsdottir H, Opjordsmoen S, Birkenaes AB, et al. Predictors of medication adherence in patients with schizophrenia and bipolar disorder. Acta Psychiatr Scand. 2013;127(1):23–33. PubMed PMID: 22900964. doi:10.1111/j.1600-0447.2012.01911.x
40. Ferretti F, Goracci A, Laurenzi PF, et al. Neuroticism and conscientiousness moderate the effect of oral medication beliefs on adherence of people with mental illness during the pandemic. Brain Sci. 2022;12(10):1315. PMID: 36291250; PMCID: PMC9599797. doi:10.3390/brainsci12101315
41. Baloush-Kleinman V, Levine SZ, Roe D, Shnitt D, Weizman A, Poyurovsky M. Adherence to antipsychotic drug treatment in early-episode schizophrenia: a six-month naturalistic follow-up study. Schizophr Res. 2011;130(1–3):176–181. PMID: 21636254. doi:10.1016/j.schres.2011.04.030
42. McGuckin C, Prentice GR, McLaughlin CG, Harkin E. Prediction of self-monitoring compliance: application of the theory of planned behaviour to chronic illness sufferers. Psychol Health Med. 2012;17(4):478–487. PMID: 22111866. doi:10.1080/13548506.2011.630399
43. Kikkert MJ, Schene AH, Koeter MW, et al. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2006;32(4):786–794. PMID: 16887889; PMCID: PMC2632275. doi:10.1093/schbul/sbl011
44. Löffler W, Kilian R, Toumi M, Angermeyer MC. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105–112. PMID: 12806568. doi:10.1055/s-2003-39985
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
