Back to Journals » Risk Management and Healthcare Policy » Volume 16
Does the Implementation of a National Health Insurance Program Result in Rationing Care for Ischemic Stroke Management? Analysis of the Indonesian National Health Insurance Program
Authors Amalia L
Received 9 February 2023
Accepted for publication 22 March 2023
Published 27 March 2023 Volume 2023:16 Pages 455—461
DOI https://doi.org/10.2147/RMHP.S405986
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Lisda Amalia
Department of Neurology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Lisda Amalia, Department of Neurology, Faculty of Medicine, Universitas Padjadjaran, Jl. Eykman 38, Bandung, 40161, Indonesia, Email [email protected]
Background: There are 2.2 million stroke patients in Indonesia, and ischemic stroke represents 87% of all strokes. Ischemic stroke is one of the covered diseases (INA-CBGs) in the National Health Insurance (JKN). Based on the Indonesian Ministry of Health’s data, stroke uses up 1% of the yearly budget. This study compares clinical outcomes and treatment patterns before and during the JKN era.
Methods: A cross-sectional analytical study of ischemic stroke medical records treated at Hasan Sadikin Hospital in 2013 and 2015 as representatives of the before and during JKN era. Chi-Square is used for data processing relationship analysis.
Results: 164 ischemic stroke patients were treated, 75 before implementing the JKN program and 89 after implementing the JKN program. There was a significant difference between treatment patterns (p< 0.001) and clinical outcomes (p=0.046) of ischemic stroke patients before and after implementing The Indonesian National Health Insurance. There was no significant difference in length of stay (LOS).
Conclusion: There is significant different between treatment pattern and clinical outcome of ischemic stroke patients before and after implementing The Indonesian National Health Insurance. This program has improved clinical outcomes concerning the purpose of the JKN program to provide social protection and welfare in terms of health.
Keywords: ischemic stroke, treatment pattern, national health insurance, clinical outcome
Introduction
A stroke is an acute neurological dysfunction caused by ischemia or bleeding, persisting for more than 24 hours or until death. Based on the etiology, stroke can be classified into ischemic and hemorrhagic. Ischemic stroke is a neurological dysfunction caused by focal cerebral, spinal, or retinal infarction.1 Ischemic stroke cases account for 87% of all stroke cases.2 In Indonesia, the number of strokes medically diagnosed until 2018 is 2.2 million people, with a prevalence rate of 10.9%.3
The national health insurance in Indonesia, known as the National Health Insurance (JKN), was implemented in 2014 by the Health Insurance Management Agency (BPJS). The JKN program guarantees diseases included in the Indonesian Case-Based Groups (INA-CBGs) regulated in Minister of Health Regulation No. 59 of 2014, and ischemic stroke is one of the diseases listed. The allocation of health facilities is carried out prospectively using the case-mix method, which is expected to reduce unnecessary drug use and encourage efficient therapy. Drugs given to patients are regulated in a national formulary based on the List of Essential Medicines (DOEN).3
Based on data from the Ministry of Health, stroke is a catastrophic disease that uses up much of the JKN budget. Stroke uses about 1% of the total budget spending each year. Before the JKN era, ischemic stroke patients could be charged up to 4,290,000 rupiahs per patient. In a study conducted in North Sumatra by Mahulae, JX, and Ilyas J, 130 ischemic stroke patients spent IDR 1,305,844,880 for direct costs, including the drugs administered.4
Until now, no previous study compared the clinical outcomes of ischemic stroke patients based on the therapy pattern before and during the JKN era. Therefore, this study aims to compare the clinical outcomes and treatment patterns of ischemic stroke patients before and during the JKN era.
Research Methods
This study is an analytical study with a cross-sectional design, conducted on 164 ischemic stroke patients hospitalized at Hasan Sadikin Hospital in Bandung, using 2013 and 2015 as a representation of each period. Data were taken from available medical records at the Department of Neurology RSHS, with inclusion criteria, namely inpatients who had confirmed atherothrombotic ischemic stroke of the first attack through non-contrast brain computed tomography (CT scan). The exclusion criteria in this study were incomplete medical records (patient characteristics, treatment patterns, and clinical outcomes), patients with recurrent stroke, cardioembolic and hemorrhagic stroke. This study took the adult population. The 164 samples in this study used the total sampling method for all reachable populations and divided into 2 groups, before implementing the JKN program and after implementing the JKN program.
Demographic characteristics reviewed in this study were gender, education, occupation, domicile, and patient age. This study analyzed the comparison of treatment patterns and clinical outcomes between the two periods. The era in which the patient was treated was compared with some of the drugs used by the patient and the clinical results in the form of a length of stay (LOS) or length of stay in the hospital and the clinical outcomes stated by the doctor. The drugs chosen are related to stroke therapy, including anti-cholesterol, antipyretic, antihypertensive, antiplatelet, anticoagulant, anti-lipid, and neuroprotectors.5 The independent variable in this study was the patient’s treatment era, and the dependent variable consisted of the length of stay (LOS), prognosis (morbidity and mortality), and drugs used.
Data collection and analysis in this study used IBM SPSS Statistics software version 28. Data processing was carried out by testing the normality of the data first with the Kolmogorov–Smirnov test on numerical data. The normality test’s significance limit is a p-value of <0.05. Categorical data are presented with frequency and proportion, while numerical data uses the mean and standard deviation. Comparison between era with LOS and age was analyzed using the Mann–Whitney test and comparisons between eras and other variables were analyzed using the Chi-Square test. A p-value < 0.05 was considered statistically significant. This research was conducted at RSUP Dr. Hasan Sadikin Bandung and carried out from February 2021 to December 2021 and has been approved by the Faculty of Medicine Ethics Committee Padjadjaran University (No. 77/UN6.KEP/EC/2021). This study complied with all relevant ethical regulations (including The Declaration of Helsinki) and covered patient data confidentiality. The correct ethics procedure was followed. Informed consent was obtained from the study participants before the study commencement.
Results
The population of this study consisted of 164 ischemic Stroke patients treated at Hasan Sadikin Hospital in Bandung from two groups, namely 75 patients before the JKN era and 89 patients during the JKN era. The ischemic stroke patients in this study were more female (94 women (57.3%), and 70 men (42.6%). The distribution of era, education, and hemispheric lesions was nearly even in this study. About two-thirds of the population live in cities. The mean age in this population was 57.7 (11.9) (Table 1).
 |
Table 1 Research Subjects Characteristic |
This study’s results showed no significant differences in gender, domicile, occupation, education, and hemisphere lesions between before and during the implementation of JKN. There was a significant difference in the subjects’ education level (p<0.001) (Table 2). In this study, there was significant difference between the drugs used in patients before and during the JKN era for neuroprotector drugs which were found to have statistical differences (p-value <0.001) after being tested using the Chi-Square method (Table 3). The comparison of clinical outcomes shows no significant difference in morbidity and length of stay (LOS), but there is a significant difference in mortality (p = 0.046) (Table 4).
 |
Table 2 Difference Characteristics of Research Subjects Before and During the JKN Era |
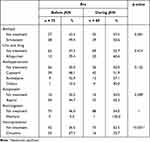 |
Table 3 Difference in Treatment Before and During JKN Era |
 |
Table 4 Differences in Clinical Outcomes Before and During the JKN Era |
Discussion
The results showed that in terms of educational level, the patient population was more in the category of not completing compulsory schooling (<12 years). The results of the analysis test show that there is a significant relationship between the era before and during JKN. Various factors can influence these results, such as low awareness of getting more information about stroke. Che, Shen et al conducted a study in China, with 3861 patients in the China Antihypertensive Trial in Acute Ischemic Stroke (a multicenter, single-blind randomized controlled clinical trial in patients with Acute Ischemic Stroke; stroke diagnosis, confirmed by CT scan or magnetic resonance imaging (MRI) within the first 48 hours of stroke). This prospective study concludes that low education correlates with increased mortality from subsequent strokes and the likelihood of experiencing cardiovascular problems.6 This seems similar to this study which also obtained data that the sample found more people with low education. Conversely, even though their education is low, their knowledge about stroke can also be influenced by various factors such as a family history of stroke, which can make their knowledge better during the JKN period due to exposure, so that they are more quickly aware of the impact of stroke on their health.7
The results showed that most patients live in cities. Based on the analysis test, there is no significant difference between before JKN and during the JKN period. This happened because the place of residence did not affect the incidence of stroke before the JKN period or after the JKN period.
The results showed that most patients with lesions were in the left hemisphere. Based on the analytical test, there was no significant relationship between the right, left, and vertebrobasilar hemispheres. This is supported by previous research by Bagaskoro YC and Pudjonarko D at Dr. Kariadi Semarang, who found that the location of the left and right hemisphere lesions had the same percentage.8
Treatment for acute ischemic stroke involves administering intravenous thrombolytics, optimizing blood sugar, controlling temperature, controlling blood pressure, reducing increased intracranial pressure, and administering neuroprotective drugs (Neuro-Protective-Drug=NPD).5 The results showed that the use of anti-cholesterol, antipyretic, antihypertensive, antiplatelet, and anti-lipid drugs did not show significant differences before and during the JKN era, while the use of neuroprotectors showed significant differences in the two eras (in the national formulary, neuroprotective drugs are not included in the drugs covered by JKN).9 In a previous study by Mehta et al, neuroprotective drugs were found to improve the functional outcomes of patients with acute stroke ischemia at 90 days. The neuroprotective agents that were found to be effective were citicoline, edaravone, and cerebrolysin.10 In the present study, citicoline was the neuroprotective drug used in both groups. A systematic review and Meta-Analysis of a Randomized Controlled Trial of 63 studies by Secades et al, obtained ten studies (double-blind, randomized, and placebo-controlled clinical trials) on the effect of citicoline on recovery in acute ischemic stroke patients. This study concludes that citicoline is beneficial in managing acute ischemic stroke.11 In Indonesia, for drugs other than neuroprotectors, there are guidelines issued by PERDOSSI in 2011 (pre-JKN era) and National Guidelines for Stroke Management Medical Services 2019 (during the JKN era), so there is no difference in the use of these drugs before and during the JKN era.12,13
In both eras, simvastatin was the treatment of choice for anticholesterol drugs. Statins are used in acute ischemic stroke patients for secondary stroke prevention by lowering lipid levels. In addition, statins have a pleiotropic effect of anti-inflammatory action, antioxidant effect, and antithrombotic action.14
Hypertension is one of the most common risk factors for ischemic stroke. In both groups, captopril was the most widely used antihypertensive drug (48.1% before the JKN era and 51.9% during the JKN era). In patients with acute ischemic stroke, blood pressure usually increases during the first 24–48 hours. The consensus is that antihypertensive agents should be given if the diastolic blood pressure is above 120 mm Hg or the systolic blood pressure is higher than 220 mm Hg. Captopril works by blocking the conversion of angiotensin I to angiotensin II, thereby preventing the degradation of vasodilating prostaglandins, thereby inhibiting vasoconstriction and increasing systemic vasodilation.15
Antiplatelets should be given to ischemic stroke patients to prevent stroke recurrence. Aspirin was used in both groups (44.7% and 55.3%, respectively). Previous studies suggest that the risk of mortality and morbidity decreases when aspirin is started within 48 hours after acute ischemic stroke.16 Some ischemic stroke patients are associated with hyperlipidemia. Gemfibrozil is the drug of choice in this population to treat hyperlipidemia by increasing plasma high-density lipoprotein (HDL) and lowering plasma triglycerides (TG) in various primary and secondary dyslipoproteinemias. In the present study, there was no statistically significant difference between gemfibrozil in the two groups.17
Length of stay (LOS) in a hospital is the main determinant of medical expenses that must be met by patients.18 Thus, LOS is an important factor related to patient financial responsibility, hospital operating costs, and health care management. Since 2000, treatment costs for stroke patients have increased faster than medical costs.19 When paying for hospitalization, the number of days spent in the hospital is an important indicator, accounting for 43% of medical costs.20 LOS increases for patients with stroke, a high-incidence disease mostly affecting the elderly, and increases the burden of medical expenses for stroke patients resulting in loss of benefit from treatment. Clinically this is also associated with a higher possibility of side effects.21,22 An increase in LOS indicates that health services in hospitals have decreased or inefficiencies have occurred in service delivery, whereas a decrease in LOS indicates an increase in the quality and efficiency of health services provided by hospitals.23 The results showed that LOS in this study had an average value of 6 days. This is supported by previous research, which stated that the result of a 15-day hospitalization was 8.43% (7 patients). The length of stay is also related to medical complications in stroke patients during the treatment period, affecting the improvement of the patient’s clinical condition and the patient’s length of stay.24 In this study, LOS was not significantly significant before the JKN era and after JKN. This could be due to the absence of differences in the length of stay before and during the JKN era, where in a study conducted by Herminawati A. at Tugurejo Hospital, Semarang, in 2014, the average LOS for ischemic stroke patients was 6.05 days, which was the same as the LOS in the study during the JKN era.25
Prognosis means estimating or predicting the likely future clinical outcome of a patient. Prognosis is usually related to a person’s risk of developing a certain health condition over a certain time, based on their clinical and non-clinical profiles. Outcomes are often specific events and complications or death, but they can also be changes, such as disease progression, pain, or quality of life.26
Concerning the purpose of the JKN program to provide social protection and welfare in terms of health, in this study, there was no significant difference between functional prognoses, so there was no significant difference between the functional outcomes of the two groups. On the other hand, there was a significant difference in mortality before and during the JKN era, thus indicating a significant difference in life expectancy between the two groups, which is in accordance with the objectives of the JKN era. After implementing the national health insurance program, the mortality of ischemic stroke patients has decreased. Increasing the capacity of human resources involved in managing stroke patient services is an effort that is no less important. Neurologists could be better distributed throughout all islands of Indonesia. Knowledge update regarding the stroke management protocol or guideline is obligatory. The Indonesian Neurologist Association (PERDOSSI), the national neurological professional organization, is already doing this.
The limitation of this study is that there needed to be more information about the clinical condition of the patients or co-morbidities among patients so that further analysis of the drug of choice could be carried out only a short time. Another area for improvement is the need for more adequate information about using JKN, so this study only compares the two eras.
Conclusion
There is a significantly difference between the treatment pattern (neuroprotector agent) and clinical outcome (mortality) of ischemic stroke patients before and after implementing The Indonesian National Health Insurance. This program has improved clinical outcomes concerning the purpose of the JKN program to provide social protection and welfare in terms of health and national health insurance results in rationing of stroke care services.
Funding
No funding was received for this study.
Disclosure
The author reports no competing interest in this work.
References
1. Katan M, Luft A. Global Burden of Stroke. Thieme Medical Publishers; 2018:208–211.
2. Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Lippincott Williams and Wilkins; 2020:E139–596.
3. Kemenkes RI. Laporan nasional riskesdas 2018. Jakarta: Kemenkes RI; 2018:154–166.
4. Mahulae JX, Ilyas J. Determinan variasi klaim penyakit stroke peserta jaminan kesehatan nasional rumah sakit X sumatera utara. J Ekonomi Kesehatan Indones. 2017;2:2. doi:10.7454/eki.v2i2.2147
5. Kaur H, Prakash A, Medhi B. Drug therapy in stroke: from preclinical to clinical studies. Pharmacology. 2013;92(5–6):324–334. doi:10.1159/000356320
6. Che B, Shen S, Zhu Z, et al. Education level and long-term mortality, recurrent stroke, and cardiovascular events in patients with ischemic stroke. J Am Heart Assoc. 2020;9(16):16671. doi:10.1161/JAHA.120.016671
7. Putri I, Tedjasukmana R, Mesina D, Pasaribu R. Hubungan antara tingkat pendidikan dengan pengetahuan deteksi dini tentang stroke di universitas Kristen Krida Wacana. J Kedokteran Meditek. 2017;23:63.
8. Bagaskoro YC, Pudjonarko D. Hubungan lokasi lesi stroke non-hemoragik dengan tingkat depresi pasca stroke (Studi Kasus Di Poli Saraf RSUP Dr. Kariadi Semarang). Diponegoro Med J. 2017;6(2):1383–1393.
9. Tentang Formularium Nasional. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MENKES/6485/2021 tentang formularium nasional; 2021.
10. Mehta A, Mahale R, Buddaraju K, Javali M, Acharya P, Srinivasa R. Efficacy of neuroprotective drugs in acute ischemic stroke: is it helpful? J Neurosci Rural Pract. 2019;10(4):576. doi:10.1055/s-0039-1700790
11. Secades JJ, Alvarez-Sabín J, Castillo J, et al. Citicoline for acute ischemic stroke: a systematic review and formal meta-analysis of randomized, double-blind, and placebo-controlled trials. J Stroke Cerebrovasc Dis. 2016;25(8):1984–1996. doi:10.1016/j.jstrokecerebrovasdis.2016.04.010
12. Guideline Stroke Tahun. Pokdi Stroke Perhimpunan Dokter Spesialis Saraf Indonesia (PERDOSSI). Guideline Stroke Tahun; 2011.
13. Tentang Pedoman Nasional Pelayanan Kedokteran Tata Laksana Stroke. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MENKES/394/2019 tentang pedoman nasional pelayanan kedokteran tata laksana stroke; 2019.
14. Hong KS, Lee JS. Statins in acute ischemic stroke: a systematic review. J Stroke. 2015;17(3):282. doi:10.5853/jos.2015.17.3.282
15. Rabinstein AA. Update on Treatment of Acute Ischemic Stroke. Continuum. 2020;26(2):268–286. doi:10.1212/CON.0000000000000840
16. Rabinstein AA. Treatment of Acute Ischemic Stroke. Continuum. 2017;23(1):62–81. doi:10.1212/CON.0000000000000420
17. Menet R, Bernard M, ElAli A. Hyperlipidemia in stroke pathobiology and therapy: insights and perspectives. Front Physiol. 2022;2022:488.
18. Kim SM, Hwang SW, Oh EH, Kang JK. Determinants of the length of stay in stroke patients. Osong Public Health Res Perspect. 2013;4(6):329–341. doi:10.1016/j.phrp.2013.10.008
19. Kwon YD, Chang H, Choi YJ, Yoon SS. Nationwide trends in stroke hospitalization over the past decade. J Korean Med Assoc. 2012;55(10):1014–1025. doi:10.5124/jkma.2012.55.10.1014
20. Yoon SS, Chang H, Kwon YD. Itemized hospital charges for acute cerebral infarction patients influenced by severity in an academic medical center in Korea. J Clin Neurol Neurosurg. 2012;8(1):58–64. doi:10.3988/jcn.2012.8.1.58
21. Song H-J, Jeong HS, Kim J. Integrated acute stroke unit care. J Neurocrit Care. 2012;5:8–16.
22. Kim S-M, Kim Y, Lee S-A. Propensity score matching analysis on inpatient period differences of hemorrhagic stroke survivors depending on medical insurance coverage. Phys Ther Rehabil Sci. 2019;8(2):67–73. doi:10.14474/ptrs.2019.8.2.67
23. Dian A. Deskripsi Karakteristik Penderita, Lama Dirawat (Los) Dan Epidemiologi Penyakit Diabetes Mellitus Pada Pasien Jkndi RSUD Tugurejo Semarang Triwulan I Tahun 2014; 2014.
24. Poana NL, Wiyono WI, Mpila DA. Pola Penggunaan Obat Pada Pasien Stroke Hemoragik Di RSUP Prof. Dr. R.D. Kandou Manado Periode Januari-Desember 2018. Pharmacon. 2020;9(1):90–99. doi:10.35799/pha.9.2020.27469
25. Herminawati A, Suryani M. Perbedaan lama rawat inap antara stroke hemoragik dan stroke non hemoragik Di RSUD Tugurejo Semarang. Karya Ilmiah. 2013;1:1.
26. Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13(1):1–10. doi:10.1186/s12916-014-0241-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
