Back to Journals » Clinical Epidemiology » Volume 10
Does low risk of infections as a marker of effective immunity predict increased risk of subsequent giant cell arteritis or polymyalgia rheumatica? A Danish population-based case–control study
Authors Brault C, Riis AH , Mor A, Duhaut P , Thomsen RW
Received 28 November 2017
Accepted for publication 12 May 2018
Published 16 October 2018 Volume 2018:10 Pages 1533—1543
DOI https://doi.org/10.2147/CLEP.S158293
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Irene Petersen
Clément Brault,1,2 Anders H Riis,1 Anil Mor,1 Pierre Duhaut,2 Reimar W Thomsen1
1Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark; 2Department of Internal Medicine and RECIF, Amiens-Picardie University Hospital, Amiens, France
Objective: It has been suggested that a hyper-effective immune system (“hyper-immunity”) is central to the pathogenesis of giant cell arteritis and polymyalgia rheumatica (GCA/PMR). We examined if a low risk of infections, as a marker of hyper-immunity, can predict increased subsequent risk of GCA/PMR.
Patients and methods: We conducted a population-based case–control study including all patients aged ≥50 years with incident GCA/PMR diagnosed between 1997 and 2012 in Northern Denmark. For each case, we selected 10 population controls matched on gender, age, place of residence, and time spent in the region. Complete history of hospital-treated infections and community-based anti-infective prescriptions was assessed in population-based registries. We used conditional logistic regression to compute OR of GCA/PMR associated with infections while adjusting for comorbidities, immunosuppressive treatment, and other potential confounders.
Results: We included 7,225 GCA/PMR cases and 72,250 controls. When excluding all infections occurring within the last year before GCA/PMR diagnosis, there was no decreased risk for GCA/PMR in people with a history of hospital-treated infection (adjusted OR=1.04, 95% CI: 0.98–1.10) or community anti-infective treatment (adjusted OR=1.07, 95% CI: 0.99–1.16). Within the last year preceding the GCA/PMR index date, patients with hospital-treated infections (adjusted OR=1.59, 95% CI: 1.44–1.75) or community anti-infective treatment (adjusted OR=1.63, 95% CI: 1.48–1.79) had a greatly increased risk of a GCA/PMR diagnosis.
Conclusion: These results do not support the hypothesis of “hyper-immunity” leading to GCA/PMR. Instead, incident GCA/PMR is preceded by a slightly increased risk of infection, which may be related to protopathic bias or support theories that infections may be directly involved in the pathogenesis of GCA/PMR.
Keywords: giant cell arteritis, polymyalgia rheumatica, infection, immune system
Introduction
Giant cell arteritis (GCA) is a vasculitis involving large- and medium-size vessels, especially the cranial branches derived from the carotid artery.1 GCA is relatively common in adults aged over 50 years with an incidence of 1/10,000 person-years and may lead to severe ischemic complications like visual loss, aortic aneurism, or stroke.1,2 Polymyalgia rheumatica (PMR) is present in up to 50% of patients with GCA and may begin before, simultaneously, or after the clinical manifestations of GCA, suggesting they are different spectrums of the same disease process.3
The pathophysiology of GCA is not fully understood, but the role of cellular actors has been investigated in recent years. Schematically, an unknown antigen present in the vascular wall appears to activate dendritic cells in the adventitia. Consequently, recruitment and activation of CD4 T cells and then the macrophages lead to vascular inflammation and remodeling. As for other vasculitis, it is suspected that an antigen of infectious origin may trigger GCA by interacting with an appropriate genetic condition in an individual.4
It has been suggested that a hyper-effective immune system or “hyper-immunity” is central to the pathogenesis of GCA/PMR.5,6 This concept, recent and not yet well defined, refers to a state of over-activation of the innate immune system. Dendritic cells are highly efficient in sensing bacterial products and facilitating T-cell recruitment.5 A hyper-effective immune system might thus protect against infections in general and, on the other hand, lead to increased risk of GCA/PMR.
Several previous studies have examined infection risks following a diagnosis of GCA/PMR. Most of them reported an increased subsequent risk of incident infections or mortality due to infectious diseases.7–12 For example, Schmidt et al found that severe infections were more common in GCA patients compared to subjects without GCA during the first year of follow-up (incidence rate ratio=2.1; 95% CI: 1.2–3.4).11 However, such increased infection risk may be related to corticosteroid treatment and other acute therapy, increased surveillance and healthcare contacts, and other comorbid conditions.12 One recent matched case–control study from the UK examined the association between previous infections and incident GCA. This study found a modest positive association, thus not supporting the hypothesis of hyper-immunity.13
To examine if a decreased risk of infection, as a marker of hyper-immunity, can predict an increased subsequent risk of GCA/PMR in the Danish population, we conducted a large population-based case–control study.
Patients and methods
Study setting
The source population was all inhabitants of the Central and the North Denmark Region (~1.8 million individuals).14
Data sources
We used three databases: the Danish National Patient Registry (DNPR), the Danish Pathology Registry (DPR), and the Aarhus University Prescription Database (AUPD). All Danish population has free and unrestricted access to medical care and is assigned a unique identification number (the Central Personal Registry number) upon birth or immigration, which allows unambiguous electronic linkage across the data sources.15
- The DNPR uses the International Classification of Diseases (ICD) system (ICD-8th revision until 1994 and ICD-10th revision thereafter) to collect information on dates and diagnoses of all hospitalizations in Denmark since 1977 and on all outpatient visits since 1995.16
- The DPR includes information on all pathology specimens from any pathology department in Denmark since 1997.17
- The AUPD contains data on all prescription drugs redeemed by Danish citizens at monopolized community pharmacies in Central and North Denmark Regions with complete data since 1996. Drugs are categorized according to the anatomical therapeutic chemical (ATC) code. Prescription data include the date of dispensing, the substance, brand name, and quantity. The dosing instruction and the indication for prescribing are not recorded.14
Identification of cases with CGA/PMR
From the DNPR, we included all patients with an incident event of GCA and/or PMR (ICD-10 codes: M31.5 or 31.6 and 35.3, respectively) diagnosed for the first time between January 1, 1997, and December 31, 2012. For each patient, information on gender, date of birth, and date of GCA/PMR diagnosis (the index date) was collected. For each case, the index date was defined as the date of the diagnosis of GCA/PMR, whereas for each control (see below), the index date was the time at which GCA/PMR occurred for the matched case. Because GCA and PMR may be different diseases, or different progressive aspects of the same disease, we categorized cases into three subgroups according to the diagnosis:
- PMR subgroup including all patients with a diagnosis of PMR without associated GCA at diagnosis or during the follow-up.
- GCA subgroup including all patients with a diagnosis of GCA without associated PMR at diagnosis or during the follow-up.
- GCA+PMR subgroup including all patients with a diagnosis of both GCA and PMR.
A definitive diagnosis of GCA is based on a temporal artery biopsy with documented inflammatory lesions in the artery wall. Thus, for GCA or GCA+PMR subgroups, we identified all patients who had a GCA with a positive temporal artery biopsy (TAB) (Snomed code M40160 and T45270) or a negative TAB using the DPR.
Exclusion criteria for cases were: age <50 years at the time of diagnosis of GCA/PMR, diagnosis of GCA/PMR outside the Central and the North Denmark Region, and patients who had <1 year of residence in this region before their GCA/PMR diagnosis in order to collect enough exposure and covariate data.
Identification of population controls
We used the Danish Civil Registration System to identify 10 population controls for each case. Controls had to be residents of the Central or North Denmark Region, and the same exclusion criteria as for GCA/PMR cases applied. We matched these controls on gender, year of birth, region of residence, and time spent in the region (in years) before the index date.
Assessment of exposure to infection
The study exposure was either hospital-treated infection or community-based anti-infective prescription occurring before the index date. We used DNPR to identify any first-time inpatient admission or hospital outpatient contact for the treatment of an infectious disease in both case and control groups. We examined a range of infections according to the system or organ involved and by the type of pathogen (see Tables S1–S3 for ICD codes). We used the AUPD to collect redemption of anti-infective prescriptions as evidence of community anti-infective treatment. We examined different subgroups of anti-infectives commonly prescribed to treat specific infections (see Table S4 for ATC codes).
Covariates
To control for confounding, we ascertained data on other factors potentially associated with GCA/PMR that may also be associated with infection risks from the DNPR and the AUPD. For each case and control subject, we collected data on diabetes, chronic alcoholism-related conditions, disorders involving immune mechanisms (such as common variable immunodeficiency or Wiskott–Aldrich syndrome), any exposure of immunosuppressive treatment including corticosteroid use, chronic kidney insufficiency, malnutrition, and history of malignant neoplasm (see Table S5 for ICD and ATC codes used).
Statistical analyses
Descriptive statistics were used to summarize the characteristics of GCA/PMR cases and controls. We used conditional logistic regression to compute crude and adjusted ORs with associated 95% CI for GCA/PMR, among persons with and without hospital- or community-treated infections occurring at least 1 year before the index date. In secondary analyses, we separately examined infections occurring during the last 12 months preceding the index date. This distinction was made because infections shortly before GCA/PMR diagnosis may either indicate reverse causality (ie, early incubating GCA/PMR with malaise, healthcare contacts, or treatment attempts leading to infections) misclassification (early GCA/PMR symptoms such as fever being misdiagnosed as infection) or, alternatively, indicate a short-term triggering effect of infections in the pathogenesis of GCA/PMR. In contrast, infection risk >12 months before GCA/PMR diagnosis may be more reflective of the overall longer-term immune status in individuals. For each exposure period, we performed analyses among case and control pair subsets according to subgroups of GCA/PMR disease: PMR only, GCA only, GCA+PMR, and GCA with positive or negative TAB. In all models, we adjusted for diabetes, chronic alcoholism-related conditions, disorders involving the immune system, any exposure of immunosuppressive treatment, chronic kidney insufficiency, malnutrition, and malignancies. All analyses were conducted using SAS software.
Ethics approval
The Danish Data Protection Agency approved the study. According to Danish law, this registry-based study needed no further ethical approval.
Results
Characteristics of study population
We identified 8,859 incident cases of GCA/PMR in the Central and the North Denmark Regions between 1997 and 2012. We excluded 234 patients who were aged <50 years, 1,167 who did not live in the region on the date of their diagnosis, and 233 who lived <1 year in the region before their diagnosis.
Finally, we included 7,225 cases and 72,250 controls. Median age at the time of diagnosis was 74 years (interquartile range [IQR] 67–81), and 64% were females (Table 1). Potential confounding factors were equally distributed between GCA/PMR patients and controls, except for diabetes, chronic kidney disease, and use of oral corticosteroids, which were more common in GCA/PMR cases.
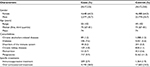  | Table 1 Characteristics of GCA/PMR case and control populations from the Central and the North Denmark Region, 1997–2012 Abbreviation: GCA/PMR, giant cell arteritis and polymyalgia rheumatica. |
Infections occurring at least 1 year prior to the index date and risk of GCA/PMR
After exclusion of infections occurring 12 months preceding the index date, 2,426 (33.6%) cases and 20,806 (28.8%) controls had a history of hospital-treated infectious diseases. The most common diagnoses in both groups were digestive system infections (11.4%) followed by infections of the respiratory tract (9.7%) and the urinary tract (7.7%). Compared to those without infection, patients with history of hospital-treated infection had a higher risk of developing GCA/PMR (OR=1.26, 95% CI: 1.19–1.32). After controlling for various confounders, the adjusted OR for the association between hospital-treated infection was close to 1 (adjusted OR=1.04, 95% CI: 0.98–1.10). Main confounding factors were oral corticosteroid use, diabetes, and chronic kidney disease. When we focused on infections according to systems or organs involved, no subgroup of infection was associated with a materially decreased or increased risk of GCA/PMR (Table 2).
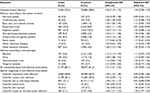  | Table 2 Crude and adjusted OR for GCA/PMR case and control populations associated with hospital-treated infection and community-based anti-infective prescription, excluding events occurring 1 year prior the index date Notes: aOR adjusted for diabetes, chronic alcoholism-related diseases, disorders involving the immune system, immunosuppressive treatment including corticosteroids, chronic kidney insufficiency, malnutrition, and neoplasia (see Table S5 for ATC codes). Abbreviations: GCA/PMR, giant cell arteritis and polymyalgia rheumatica; ATC, anatomical therapeutic chemical. |
In total, 6,147 (85.1%) GCA/PMR patients and 58,677 (81.2%) controls had redeemed anti-infective treatment prescriptions >12 months before the index date. The most common anti-infective treatments prescribed were antibiotics typically used for respiratory tract infections (67.4%), urinary tract infections (29.7%), and soft tissue or skin infections (11.7%) in both groups. Patients with prescription history of an anti-infective treatment had a higher risk of developing a GCA/PMR (OR=1.41, 95% CI: 1.31–1.52) compared to those without it. After controlling for various confounders, this association reduced considerably (adjusted OR=1.07, 95% CI: 0.99–1.16). No subgroups of anti-infective prescriptions were clearly associated with an altered risk of GCA/PMR, except for treatments typically prescribed for herpes simplex virus (HSV) or varicella-zoster virus (VZV) infection (adjusted OR=1.20, 95% CI: 1.07–1.35) (Table 2).
Infections occurring 1 year prior to the index date and risk of GCA/PMR
During 12 months preceding the index date, 582 (8.1%) cases and 3,074 (4.3%) controls had a history of hospital-treated infection. After adjustment, patients with a history of hospitalization for an infectious disease had an increased risk of developing GCA/PMR (adjusted OR=1.59, 95% CI: 1.44–1.75). An approximately doubled risk was seen for all major infection types, including respiratory tract infections, skin and musculoskeletal infections, or urinary tract and genital infections (Table 3).
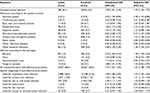  | Table 3 Crude and adjusted OR for GCA/PMR case and control populations associated with hospital-treated infection and community-based anti-infective prescription, including only events occurring 1 year prior the index date Notes: aOR adjusted for diabetes, chronic alcoholism-related diseases, disorders involving the immune system, immunosuppressive treatment including corticosteroids, chronic kidney insufficiency, malnutrition, and neoplasia (see Table S5 for ATC codes). Abbreviations: GCA/PMR, giant cell arteritis and polymyalgia rheumatica; ATC, anatomical therapeutic chemical. |
Identically, 3,367 (46.6%) GCA/PMR patients and 23,561 (32.6%) controls redeemed an anti-infective treatment prescription within 12 months before the index date. After adjustment, patients with anti-infective prescription had a clearly increased risk of developing GCA/PMR (adjusted OR =1.63, 95% CI: 1.48–1.79), mainly driven by anti-infective treatment used for respiratory tract infection (adjusted OR=1.53, 95% CI: 1.45–1.62) (Table 3).
Hospital-treated infections, anti-infective treatments, and risk of different subgroups of GCA/PMR
Among our cases, 5,100 (70.6%) patients had a PMR diagnosis only, 100 (1.4%) had GCA only, and 2,025 (28%) had both GCA and PMR. After exclusion of events occurring in the year prior to the index date, there was an association between hospital-treated infections and the subgroups having a later GCA diagnosis alone or together with PMR (adjusted OR=1.15, 95% CI: 1.04–1.27 and 1.15, CI 95%: 1.04–1.27, respectively) (Table 4).
  | Table 4 Crude and adjusted OR for PMR or GCA subgroups and control populations associated with hospital-treated infection and community-based anti-infective prescription Notes: aOR adjusted for diabetes, chronic alcoholism-related diseases, disorders involving the immune system, immunosuppressive treatment including corticosteroids, chronic kidney insufficiency, malnutrition, and neoplasia (see Table S5 for ATC codes). Abbreviations: GCA, giant cell arteritis; PMR, polymyalgia rheumatica; ATC, anatomical therapeutic chemicals. |
Among GCA or GCA+PMR patients, 510 (24%) had a positive TAB and 1,615 (76%) had a negative TAB. Of note, there was no association with hospital-treated infection or prescription of anti-infective treatment for the TAB positive GCA subgroup (Table 5).
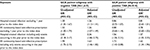  | Table 5 Crude and adjusted OR for positive or negative temporal artery biopsy (TAB) subgroups and control populations associated with hospital-treated infection and community-based anti-infective prescription Notes: aOR adjusted for diabetes, chronic alcoholism-related diseases, disorders involving the immune system, immunosuppressive treatment including corticosteroids, chronic kidney insufficiency, malnutrition, and neoplasia (see Table S5 for ATC codes). Abbreviations: GCA, giant cell arteritis; ATC, anatomical therapeutic chemical; AB, temporal artery biopsy. |
When we focused on infections occurring 12 months before GCA/PMR, OR remained higher for GCA diagnosis alone or together with PMR compared with PMR without GCA (Table 4).
Discussion
This large population-based study provides evidence that patients with history of infection have a slightly increased, rather than decreased, risk of developing GCA/PMR, arguing against the hypothesis of “hyper-immunity.”
Different biological mechanisms might explain the link between increased infections and development of GCA/PMR. Preexisting immune system alterations due to genetic polymorphisms or immunosenescence could increase both infection risk and development of vasculitis in the arterial wall.13 Indeed, many genetic polymorphisms involving genes of the immune system are described in GCA/PMR.18 For example, haplotypes of human leukocytes antigen (like HLA DRB1*04), mutations concerning intracellular signalization molecules (like PTPN22 playing a role in T-cell activation), or mutation of genes encoding proinflammatory cytokines (like tumor necrosis factor-α or interleukin-6) are frequently detected in GCA patients.18–20 All these polymorphisms could lead to a better cooperation between dendritic cells and T cells, inducing aberrant immune cell activation and the development of an unregulated inflammatory response.5 Alternatively, infections could also be directly responsible for GCA/PMR in case of an unregulated inflammatory response. Thus, molecular mimicry, epitope spreading, bystander activation, or exposition of cryptic antigens may all be involved in auto-immunity.21 Immunosenescence describes adaptive and innate immune deregulation in the elderly, including contraction of the immune repertoire, impairment of dendritic cells, and excessive secretion of pro-inflammatory cytokines. This results in a pro-inflammatory environment promoting vasculitis and a decreased bacterial clearance.22,23
Only two previous studies, to our knowledge, have evaluated the risk of infections before GCA diagnosis. Russo et al included 100 biopsy-proven GCA and 100 gender- and age-matched controls.24 The objective of the study was to assess any association between the occurrence of GCA and infections (classified into three groups: possible, probable, and proven infection) 4 months prior to the diagnosis of GCA. Most frequently occurring infections were urinary tract infections, sinusitis, pharyngitis, upper respiratory tract infections, and supposed viral infections. In agreement with our results, the authors demonstrated that recent infections were significantly more common in GCA patients compared to controls, with a relative risk of 3.5 (95% CI: 1.8–7.0). In another recent study, Rhee et al compared 4,559 GCA cases with 22,795 age-, sex-, and practice-matched controls.13 Prior infections (classified as respiratory tract, urinary tract, gastrointestinal tract, conjunctiva, or skin and soft tissue infections) were associated with a higher risk of developing GCA with an incidence rate ratio of 1.26 (95% CI: 1.16–1.36). This association persisted for all time periods but was strongest within 6 months prior to the index date, corroborating our findings.
Previous studies have searched for specific microbial agents as infectious triggers of GCA/PMR.25–31 The herpes virus group, especially, has been the object of intensive research.32 Powers et al analyzed the prevalence of HSV detected by PCR in the temporal arteries of patients with and without biopsy-proven GCA. HSV was more often found in temporal arteries of biopsy-proven GCA patients (21/24, P=0.027).33 In our study, we found no association between VZV infection and risk of GCA/PMR. Likewise, there was only a modest relation between the use of acyclovir (anti-viral treatment used for HSV or VZV) and risk of GCA/PMR with an adjusted OR of 1.20 (95% CI: 1.07–1.35). In comparison, Rhee et al found that herpes zoster infection was associated with a modestly increased risk of GCA (incidence rate ratio=1.17, 95% CI: 1.04–1.31).13 On the other hand, we did not find an association between hospitalization for any virus infection and the occurrence of GCA/PMR. When we focused on GCA patients with positive TAB, we did not find any association with neither hospital-treated infections nor prescription of anti-infectives, including anti-viral treatment for HSV or VZV.
It remains to be elucidated to which degree ours and other findings for recent infections are causal or point toward misclassification, that is, beginning symptoms of vasculitis misdiagnosed as infection, or protopathic bias, that is, vasculitis and its treatment causing infection. Of note, we noticed a large difference in corticosteroid prescription (without restriction concerning the dose or the duration of treatments) in GCA/PMR patients compared to controls (58% vs 25%). This difference was particularly evident during the year preceding the index date (45% vs 7%) and likely explained by corticosteroids used to treat the first symptoms of vasculitis before the final diagnosis was made, because in some case, the treatment must be rapidly initiated.34 The prescription of corticosteroid showed to be the most important confounder in our study, explaining much of the apparent association between infections and GCA/PMR.
The main strengths of our study are a large number of GCA patients, a population-based design, long and complete follow-up, and the ability to adjust for numerous confounding factors. Concerning limitations, we might risk some misclassification bias due to the registry-based nature of our study. Many infections would not be captured by Danish registries because they are treated with neither hospitalization nor anti-infective treatment. In particular, many viral infections that are suspected to act as trigger in the development of GCA/PMR are associated with no or few symptoms. Moreover, as in any observational study, unmeasured confounders may have affected our risk estimates, such as anthropometric, lifestyle, and genetic factors potentially associated with both infections and risk of GCA/PMR.
We did not collect data about vaccinations. Vaccine components, like adjuvants, can activate the immune system and induce manifestations grouped under the ASIA syndrome (auto-immune/inflammatory syndrome induced by adjuvants). There are case reports of subjects who developed GCA/PMR following influenza vaccination.35,36 Vaccination, by decreasing infection risk and increasing the development of GCA/PMR could thus be a potential unmeasured confounder in our study.
Conclusion
Our results do not support the hypothesis of “hyper-immunity” leading to GCA/PMR. Instead, incident GCA/PMR is preceded by a slightly increased risk of infection. This finding may support theories that infections may be directly involved in the pathogenesis of GCA/PMR. However, the finding that the association is strongest for infections close to the GCA diagnosis date, and the strong role of corticosteroid treatment as a confounder, points toward presence of considerable protopathic bias.
Disclosure
The authors report no conflicts of interest in this work.
References
Gonzalez-Gay MA, Barros S, Lopez-Diaz MJ, Garcia-Porrua C, Sanchez-Andrade A, Llorca J. Giant cell arteritis: disease patterns of clinical presentation in a series of 240 patients. Medicine (Baltimore). 2005;84(5):269–276. | ||
Petri H, Nevitt A, Sarsour K, Napalkov P, Collinson N. Incidence of giant cell arteritis and characteristics of patients: data-driven analysis of comorbidities. Arthritis Care Res (Hoboken). 2015;67(3):390–395. | ||
Weyand CM, Goronzy JJ. Clinical practice. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med. 2014;371(1):50–57. | ||
Weyand CM, Goronzy JJ. Immune mechanisms in medium and large-vessel vasculitis. Nat Rev Rheumatol. 2013;9(12):731–740. | ||
Han JW, Shimada K, Ma-Krupa W, et al. Vessel wall-embedded dendritic cells induce T-cell autoreactivity and initiate vascular inflammation. Circ Res. 2008;102(5):546–553. | ||
Misra DP, Agarwal V. Innate immune cells in the pathogenesis of primary systemic vasculitis. Rheumatol Int. 2016;36(2):169–182. | ||
Udayakumar PD, Chandran AK, Crowson CS, Warrington KJ, Matteson EL. Hospitalized infections in giant cell arteritis: a population-based retrospective cohort study. J Rheumatol. 2014;41(12):2447–2451. | ||
Michet CJ, Achenbach SJ, Crowson CS, Matteson EL. Hospitalization rates and utilization among patients with giant cell arteritis: a population-based study from 1987 to 2012. Semin Arthritis Rheum. 2015;45(1):70–74. | ||
Unizony S, Menendez ME, Rastalsky N, Stone JH. Inpatient complications in patients with giant cell arteritis: decreased mortality and increased risk of thromboembolism, delirium and adrenal insufficiency. Rheumatology (Oxford). 2015;54(8):1360–1368. | ||
Durand M, Thomas SL. Incidence of infections in patients with giant cell arteritis: a cohort study. Arthritis Care Res (Hoboken). 2012;64(4):581–588. | ||
Schmidt J, Smail A, Roche B, et al. Incidence of severe infections and infection-related mortality during the course of giant cell arteritis: a multicenter, prospective, double-cohort study. Arthritis Rheumatol. 2016;68(6):1477–1482. | ||
Baslund B, Helleberg M, Faurschou M, Obel N. Mortality in patients with giant cell arteritis. Rheumatology (Oxford). 2015;54(1):139–143. | ||
Rhee RL, Grayson PC, Merkel PA, Tomasson G. Infections and risk of incident giant cell arteritis: a population-based, case-control study. Ann Rheum Dis. 2017;76(6):1031–1035. | ||
Ehrenstein V, Antonsen S, Pedersen L. Existing data sources for clinical epidemiology: Aarhus University Prescription Database. Clin Epidemiol. 2010;2:273–279. | ||
Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. | ||
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. | ||
Bjerregaard B, Larsen OB. The Danish Pathology Register. Scand J Public Health. 2011;39(7 Suppl):72–74. | ||
Ly KH, Régent A, Tamby MC, Mouthon L. Pathogenesis of giant cell arteritis: more than just an inflammatory condition? Autoimmun Rev. 2010;9(10):635–645. | ||
Carmona FD, Mackie SL, Martín JE, et al. A large-scale genetic analysis reveals a strong contribution of the HLA class II region to giant cell arteritis susceptibility. Am J Hum Genet. 2015;96(4):565–580. | ||
Carmona FD, Martín J, González-Gay MA. New insights into the pathogenesis of giant cell arteritis and hopes for the clinic. Expert Rev Clin Immunol. 2016;12(1):57–66. | ||
Moiseev S, Novikov P, Smitienko I, Shchegoleva E. Giant cell arteritis, infections and biologics. Ann Rheum Diseases. 2017;76(9):e29. | ||
Watad A, Bragazzi NL, Adawi M, et al. Autoimmunity in the elderly: insights from basic science and clinics – a mini-review. Gerontology. 2017;63(6):515–523. | ||
Mohan SV, Liao YJ, Kim JW, Goronzy JJ, Weyand CM. Giant cell arteritis: immune and vascular aging as disease risk factors. Arthritis Res Ther. 2011;13(4):231. | ||
Russo MG, Waxman J, Abdoh AA, Serebro LH. Correlation between infection and the onset of the giant cell (temporal) arteritis syndrome. A trigger mechanism? Arthritis Rheum. 1995;38(3):374–380. | ||
Duhaut P, Bosshard S, Calvet A, et al. Giant cell arteritis, polymyalgia rheumatica, and viral hypotheses: a multicenter, prospective case-control study. Groupe de Recherche sur l’Artérite à Cellules Géantes. J Rheumatol. 1999;26(2):361–369. | ||
Wagner AD, Gérard HC, Fresemann T, et al. Detection of Chlamydia pneumoniae in giant cell vasculitis and correlation with the topographic arrangement of tissue-infiltrating dendritic cells. Arthritis Rheum. 2000;43(7):1543–1551. | ||
Alvarez-Lafuente R, Fernández-Gutiérrez B, Jover JA, et al. Human parvovirus B19, varicella zoster virus, and human herpes virus 6 in temporal artery biopsy specimens of patients with giant cell arteritis: analysis with quantitative real time polymerase chain reaction. Ann Rheum Dis. 2005;64(5):780–782. | ||
Lee JL, Naguwa SM, Cheema GS, Gershwin ME. The geo-epidemiology of temporal (giant cell) arteritis. Clin Rev Allergy Immunol. 2008;35(1-2):88–95. | ||
Mohammadi A, Pfeifer JD, Lewis JS. Association between human papillomavirus DNA and temporal arteritis. BMC Musculoskelet Disord. 2012;13:132. | ||
Katz B, Koening C, Patel B, et al; Neuro-Ophthalmology GCA Consortium. Identification of Burkholderia in the Temporal Arteries and Blood of Patients with Giant Cell Arteritis. EHSL-NANOS 2012 Annual Meeting Collection. Available from: http://content.lib.utah.edu/cdm/singleitem/collection/ehsl-nam/id/1377/rec/1. Accessed February 8, 2011. | ||
Nagel MA, White T, Khmeleva N, et al. Analysis of Varicella-zoster virus in temporal arteries biopsy positive and negative for giant cell arteritis. JAMA Neurol. 2015;72(11):1281–1287. | ||
Ly KH, Liozon E, Fauchais A-L, Vidal E. Pathophysiology of giant cell arteritis. Rev Med Interne. 2013;34(7):392–402. | ||
Powers JF, Bedri S, Hussein S, Salomon RN, Tischler AS. High prevalence of herpes simplex virus DNA in temporal arteritis biopsy specimens. Am J Clin Pathol. 2005;123(2):261–264. | ||
Mukhtyar C, Guillevin L, Cid MC, et al. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2009;68(3):318–323. | ||
Soriano A, Verrecchia E, Marinaro A, et al. Giant cell arteritis and polymyalgia rheumatica after influenza vaccination: report of 10 cases and review of the literature. Lupus. 2012;21(2):153–157. | ||
Nesher G. Autoimmune aspects of giant cell arteritis. Isr Med Assoc J. 2014;16(7):454–455. |
Supplementary materials
  | Table S1 List of all collected infections in the study (ICD-10 codes and equivalent ICD-8 codes) |
  | Table S2 Infectious diseases according to systems or organs involved (ICD-10 codes and equivalent ICD-8 codes) |
  | Table S3 Infections according to pathogens (ICD-10 codes and equivalence ICD-8 codes) |
  | Table S4 Community-based anti-infective prescription typically used for common community infections (ATC codes) |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

