Back to Journals » Patient Preference and Adherence » Volume 12
Does knowledge on diabetes management influence glycemic control? A nationwide study in patients with type 1 diabetes in Brazil
Authors Gomes MB, Santos DC , Pizarro MH , Barros BSV , Melo LGN , Negrato CA
Received 13 July 2017
Accepted for publication 10 November 2017
Published 4 January 2018 Volume 2018:12 Pages 53—62
DOI https://doi.org/10.2147/PPA.S146268
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Marilia Brito Gomes,1 Deborah Conte Santos,1 Marcela H Pizarro,1 Bianca Senger V Barros,1 Laura G Nunes de Melo,2 Carlos A Negrato3
1Department of Internal Medicine, Diabetes Unit, State University Hospital of Rio de Janeiro, 2Department of Ophthalmology, State University of Rio de Janeiro, Rio de Janeiro, 3Department of Internal Medicine, Bauru’s Diabetics Association, Bauru, São Paulo, Brazil
Objective: The purpose of this study is to establish demographic and clinical data associated with the knowledge on diabetes management and its influence on glycemic control in patients with type 1 diabetes.
Methods: This was a retrospective, observational, multicenter study conducted with 1,760 patients between August 2011 and August 2014 in 10 cities of Brazil.
Results: Overall, 1,190 (67.6%) patients knew what glycated hemoglobin (HbA1c) means. These patients were older, had longer disease duration, longer follow-up in each center, reported lower frequency of self-reported hypoglycemia, and were more frequently Caucasians and at glycemic goal. Multivariate analysis showed that knowledge on what HbA1c means was related to more years of school attendance, self-reported ethnicity (Caucasians), severe hypoglycemia, economic status, follow-up time in each center, and participation on diabetes educational programs. Good glycemic control was related to older age, more years of school attendance, higher frequency of daily self-monitoring of blood glucose, higher adherence to diet, and knowledge on what HbA1c means.
Conclusion: Patients with a knowledge on what HbA1c means had a better chance of reaching an adequate glycemic control that was not found in the majority of our patients. Diabetes care teams should rethink the approaches to patients and change them to more proactive schedules, reinforcing education, patients’ skills, and empowerment to have positive attitudes toward reaching and maintaining a better glycemic control. Finally, the glucocentric approach to diabetes management should be changed to actions that include patients’ psychosocial aspects aiming to reduce the stress of living with diabetes, improving glycemic control, and avoiding adverse outcomes.
Keywords: type 1 diabetes, diabetes knowledge, diabetes education, glycemic control, diabetes complications
Introduction
Type 1 diabetes (T1D) is a chronic disease with an incidence that varies widely throughout the world and is continuously increasing.1 Nowadays, intensive insulin therapeutic regimens, practice of physical activities, and personally tailored diets are the basis of treatment for patients with T1D.2 These factors are fundamentally important in obtaining and keeping an adequate glycemic control and avoiding chronic complications that are related to diabetes and result in very high costs (direct and indirect) and are associated with high rates of mortality.3,4 Data from the Diabetes Control and Complications Trial (DCCT) and Epidemiology of Diabetes Interventions and Complications (EDIC) studies have shown that intensive glycemic control reduces the risk of diabetes-related chronic complications4 and that intensive insulin treatment is the best approach to treating patients with T1D, always associated with regular practice of physical activities and an individualized diet plan. Besides this, some other tools related to diabetes management such as self-monitoring of blood glucose (SMBG) and knowledge on all these tools by the patients are cornerstone for reaching and maintaining a good glycemic control, which is still a challenge in clinical practice, mainly among minorities.5 In the USA, the Exchange study has shown that only 64% and 43% of children and adolescents, respectively, met a good glycemic control.6 In an international study comparing registries from 19 countries, it was found that only 15.8% had an adequate glycemic control.7 In Brazil, only 13.2% of patients with T1D presented glycated hemoglobin (HbA1c) at target.8
Moreover, many other factors can contribute to poor glycemic control in daily clinical practice such as cognitive dysfunction due to chronic hyperglycemia, poor (or absent) family support, social economic inequalities, and poor continuous educational support in many aspects regarding diabetes and in its management.8–13 A recent study conducted with hypertensive patients regarding knowledge on hypertension and medication adherence showed a lower number of patients with better knowledge presenting a blood pressure of >140/90 mmHg. Otherwise, these patients had a higher adherence mainly to a nonpharmacological treatment of hypertension.14 Regarding diabetes, a study conducted in Mexico showed that patients who perceived themselves at target for HbA1c had a lower mean HbA1c.15 In France, a study performed with 235 patients with T1D showed that 87% of these patients knew what HbA1c means; in both studies, they performed more SMBG.15,16 It seems that all barriers to obtain an adequate glycemic control should be explored in all groups of patients with T1D.5
The objective of the present study was to evaluate the impact of patients’ knowledge on diabetes management and its influence on glycemic control. Information obtained in this study will be important to guide governmental health policies to improve diabetes care in Brazil.
Research design and methods
Our study was retrospective, observational, and nationwide performed from August 2011 to August 2014 in 14 public clinics from 10 cities of Brazil belonging to all geographic regions of the country (North/Northeast, Midwest, Southeast, and South). The methodology has been described elsewhere.12 All patients received free health care from the Brazilian National Health Care System (BNHCS) that furnishes all necessary supplies for diabetes treatment such as Neutral Protamine Hagedorn (NPH) and regular insulin, syringes, needles, glucometers, and strips for SMBG. Each diabetes center presented data from at least 50 outpatients with clinical diagnosis of T1D aged at least 13 years who were regularly attended in these clinics for at least 6 months. Our sample included 1,760 patients with the diagnosis of diabetes made between 1960 and 2014. Patients were classified according to the American Diabetes Association criteria2 as adolescents (13–19 years) and adults (>19 years). Ethics approval for the study was obtained from Pedro Ernesto University Hospital, number 2769/2010. A list of the people involved in the study at each center is available in the Supplementary material. Written informed consent was obtained from all patients or from their parents if the patients were younger than 18 years.
A questionnaire was applied during a clinical visit, and the following variables were assessed: current age, age at diagnosis, diabetes duration, treatment modalities (different types of insulin therapy), frequency of SMBG, smoking status, last month’s self-reported frequency of any hypoglycemia (blood glucose levels ≤70 mg/dL), and severe hypoglycemia (occasions in which the patient needed the assistance of a third party) and hospitalization due to any cause in the last 12 months.17 Body mass index (BMI) was determined by dividing an individual’s weight (kg) by the square of the height (m2).18 Adherence to diet and to insulin therapy was self-reported, and both have been previously described.12,13 Briefly, an adequate adherence to diet was considered when the patient reported at least 80% of the time adherence to the prescribed diet.13 Adherence to insulin therapy was based on self-reported scales that evaluated last month’s medication-taking behavior, using an adaptation of the four questions proposed by Morisky–Green–Levine.12,19 Clinical visits to physicians as well as appointments with nurses and participation on educational programs about diabetes in the last year were also evaluated.
The Brazilian Type 1 Diabetes Study Group (BrazDiab1SG) adopted the following American Diabetes Association (ADA) goals for adequate metabolic and clinical control: HbA1c <7.5% for adolescents and <7% for adults were considered as good glycemic control.2 HbA1c ≥9% was considered as poor control. HbA1c was determined by high-performance liquid chromatography (Bio-Rad Laboratories Inc., Hercules, CA, USA) on the same day of the clinical visit to the physician. The last HbA1c reported by the patient at the time of the clinical visit and the HbA1c levels registered in medical records in the last year were also assessed. Smoking was defined as the current use of any amount of cigarettes.
To evaluate knowledge on diabetes management, patients were asked to answer six questions (Figure 1).
  | Figure 1 Six questions to evaluate knowledge on diabetes managment. |
Sample calculation and economic status definition
The sample size was calculated based on the BrazDiab1SG’s number of patients found in each Brazilian geographical region12 and the estimated territorial distribution of the Brazilian population reported by the 2000 Brazilian Institute of Geography and Statistics Census (IBGE).20 These data were combined with national estimates of diabetes prevalence derived from a survey conducted by Malerbi and Franco in 1988.21 More than 95% of the estimated number of patients from each geographical region were evaluated. They had their economic status defined according to the Brazilian Economic Classification Criteria that considers education as illiterate/incomplete primary education, complete primary education/incomplete secondary education, complete secondary education/incomplete high school, complete high school/some college, and complete college education.22 Economic classes were stratified as follows: high, middle, low, and very low.
Statistical analysis
Independent continuous variables were compared using independent, two-sided t-tests or ANOVA with Bonferroni correction and were expressed as mean ± SD. Two-sided Z-tests were used for comparisons between discrete variables. Pearson correlation was performed between HbA1c reported by the patient, current HbA1c, and HbA1c value in the last year (evaluated in medical records). Multivariate logistic regression was performed with the patient’s knowledge on what HbA1c means (yes, group 1; no, group 0). Ethnicity (Caucasian or non-Caucasian, as described in medical charts or self-reported), economic status, age, years of study, gender, duration of diabetes, follow-up time in each center, severe hypoglycemia (yes/no), number of clinical visits, appointment with nurses, and participation in educational programs for diabetes were included in the model as independent variables. Multivariate logistic regression was also performed with HbA1c <7.0 or <7.5 and ≥9.0% as dependent (outcome) variables and ethnicity, economic status, age, years of school attendance, adherence to diet, adherence to insulin therapy, knowledge on what HbA1c means or diabetes management, gender, duration of diabetes, duration of follow-up in each respective center, type of insulin regimens, and number of SMBG performed daily as independent variables. In all models, we used the forward Wald stepwise logistic regression analysis. The Nagelkerke’s R2 value was also calculated. SPSS Version 17.0 (SPSS, Inc., Chicago, IL, USA) program was used for all analysis. Odds ratios with 95% CI were also determined. A two-sided P-value of <0.05 was considered statistically significant.
Results
Clinical and demographic data and patients’ knowledge on HbA1c
Clinical and demographic data of the studied population are summarized in Table 1. Data stratified according to patients’ knowledge on HbA1c are described in Table 2. Patients from group 1 were older, had longer diabetes duration and longer years of follow-up at each diabetes center, and were more frequently Caucasians than patients from group 0. A tendency was noted for female gender (P=0.07).
The majority of patients knew what HbA1c means (1,190 [67.4%]) and also knew that HbA1c means the evaluation of glycemic control in the last 3 months (1,096 [62.3%]). A linear trend was observed between patients’ knowledge on what HbA1c means and economic status, with more patients from high and medium classes than patients from other classes (low and very low) found in group 1 (P<0.001). In average, the total studied population had 12.2±3.8 years of school attendance. Patients from group 1 had more years of school attendance than patients from group 0 (P<0.001).
Participants’ glycemic control, insulin therapeutic regimens, and knowledge on HbA1c and diabetes management
Considering insulin therapeutic regimens data, more patients from group 1 were using continuous subcutaneous insulin infusion (CSII) and combining intermediate or long-acting insulin with short-acting insulin than patients from group 0 (P<0.001).
Patients from group 1 had lower HbA1c (current and in the last year) than patients from group 0. HbA1c levels reported by the patients showed a positive correlation with last year’s HbA1c levels found in the medical records (r=0.51, P<0.001) and with the current HbA1c levels (r=0.72, P<0.001). There were more adult patients in group 1 than adolescents (1,022 [85.9%] vs 168 [14.1%], respectively, P<0.0001). Higher HbA1c levels were observed in adolescents than in adults (9.7±2.2 vs 8.8%±2.0%, respectively, P<0.001).
More patients from group 1 were at goal for HbA1c than patients from group 0 (P<0.001). More patients from group 1 knew what was the threshold of HbA1c considered as a good glycemic control than patients from group 0 (1,002 [84.2%] vs 89 [15.6%], P<0.001, respectively). Concerning the actions that patients took after observing high glucose levels according to SMBG, the majority of patients from group 1 reported changing insulin doses compared with patients from group 0 (835 [82.1%] vs 301 [74.9%], P=0.001, respectively). No difference was noted concerning changes in diet and in exercises.
Severe hypoglycemic episodes were reported by 251 patients (19.0%). Patients from group 1 reported lower frequency of severe hypoglycemia than patients from group 0 (P=0.004).
SMBG was performed by 1,663 (94.4%) patients with a mean of 3.6±1.4/day. More patients from group 1 knew why they should perform SMBG than patients from group 0 (1,176 [98.8%] vs 496 [87.0%], P<0.001, respectively); they also performed more daily SMBG than patients from group 0 (P<0.001).
Patients from group 1 reported more adherence to diet and more participation on diabetes educational programs. Maximum adherence to insulin therapy was less frequent in group 1 than in group 0 (P=0.01). Overall, 278 patients (15.8%) had a hospitalization for any cause in the previous year, with a mean of 1.8±1.4 hospitalization/year without difference between groups. The number of clinical visits to physicians and the number of appointments with a nurse was similar between groups. The mean BMI was 24.2±4.1 kg/m2, with no difference between the two groups.
Considering the group of patients who knew what HbA1c means (n=1,190), further analysis showed that 808 (67.9%) patients answered correctly to the other questions about HbA1c and knew the value of their last HbA1c and 382 (32.1%) patients knew what HbA1c means but did not answer correctly to any of the other questions. The former patients had lower current HbA1c than the latter patients (8.6±1.9 vs 9.0±2.0, P=0.001, respectively), and more patients from the former group were within the goals for HbA1c than patients from the latter group (144 [18.0%] vs 52 [13.8%], P=0.002), performed more daily SMBG (3.8±1.4 vs 3.6±1.4, P=0.05), and related more adherence to diet (479 [65.3%] vs 190 [55.4%], P=0.002, respectively). No difference was found concerning the frequency of hypoglycemia and maximum adherence to insulin therapy. These data are not described in Table 2.
Multivariate analysis with knowledge on what HbA1c means as dependent variable (yes/no)
Multivariate analysis with knowledge on what HbA1c means as dependent variable showed that all the independent variables, which entered in the model, even after adjustment, could explain only 21% (Nagelkerke’s R2) of a given patient knowing what HbA1c means. The independent variables associated with the knowledge on what HbA1c means were higher years of school attendance, self-reported ethnicity (Caucasians), economic status, follow-up time in each center, self-reported severe hypoglycemia, and participation on diabetes educational programs. Table 3 shows the final adjusted model.
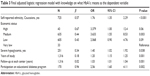  | Table 3 Final adjusted logistic regression model with knowledge on what HbA1c means as the dependent variable |
Multivariate analysis with HbA1c at goal as the dependent variable
Eight hundred fourteen patients were included in this analysis (n=222 with HbA1c at goal and n=592 with HbA1c ≥9.0%). Multivariate analysis performed with HbA1c at goal and HbA1c ≥9.0% as dependent variables showed that all the independent variables that entered in the model, even after adjustment, could explain only 15% (Nagelkerke’s R2) of a given patient reaching the goal for HbA1c. HbA1c at goal was associated with the following independent variables: older age, more years of school attendance, higher frequency of daily SMBG, higher adherence to diet, and knowledge on what HbA1c means. Table 4 shows the final adjusted model.
Using the same model with knowledge on diabetes management (questions related to HbA1c, glycemic control, and SMBG) instead of using only knowledge on what HbA1c means did not change our final results, but the Nagelkerke’s R2 was 20.1%.
Discussion
The evaluation of patients’ knowledge on HbA1c in the BrazDiab1SG has shown that the majority of our patients referred to know what HbA1c means and also that it translates how was glycemic control in the last 3 months. Patients who showed a knowledge on what HbA1c means had lower current HbA1c levels, were older, had a longer follow-up in their respective diabetes center, were more frequently Caucasians and mostly from high and medium social classes, and had more years of school attendance and participation on diabetes educational programs. Moreover, knowing the meaning of HbA1c was an important variable related to an adequate glycemic control together with adherence to diet, higher number of SMBG performed daily, and lower rates of severe hypoglycemia. However, a small difference in current HbA1c levels was noted between patients who have more knowledge on diabetes management (including many questions related to HbA1c, glycemic control, and SMBG) and patients who knew only what HbA1c represents; in other words, just knowing what HbA1c means probably made an important difference upon diabetes control outcomes.
Among patients who knew what HbA1c means, fewer patients had HbA1c levels ≥9% and more patients were at goal for good glycemic control. Only years of school attendance was common to both knowledge on what HbA1c means and HbA1c at goal in multivariate analysis, which means that years of school attendance, independent of socioeconomic status and ethnicity, was the most important factor, leading to better diabetes control outcomes. Although we have noted a relationship between knowledge on what HbA1c means, lower rates of severe hypoglycemia, and participation on diabetes educational programs by the patients, we have to emphasize that fewer patients in our study have participated in these programs in comparison to patients with T1D enrolled in a collaborative study conducted in Mexico.15 This could be one among several explanations why a larger proportion of our patients were out of target for HbA1c, independent of the degree of knowledge that they had about what HbA1c means.
Patients who experience hypoglycemia may develop an excessive fear of presenting other hypoglycemic episodes that could function as a stimulus for behavior modifications including the acquisition of more knowledge on diabetes; this fear could also lead patients to keep higher glycemic levels to avoid other hypoglycemic episodes.23 In our study, we have observed that patients who knew what HbA1c means had less severe hypoglycemic episodes, although presenting high HbA1c levels (8.7%), what is in accordance with the findings of this former study.23
We have also to point out that the majority of our patients had reported self-adjustment of insulin doses according to the results of SMBG, mainly patients from group 1, but even so, >30% of these patients still had HbA1c ≥9.0%. The collaborative group study conducted in Mexico showed that although 63.2% of patients with T1D used to practice self-adjustment on insulin doses, their mean HbA1c was 8.8%.15 As has been previously found in the Hvidoere International Study Group and Exchange Study Group, adolescent patients showed higher levels of HbA1c than adult patients.24,25 Different factors have been related to poor glycemic control in patients with T1D including familial support, depressive and anxiety disorders (in patients and parents), and many other altered physiological and psychological processes that are generally found in this age.10 Altogether, these factors could lead to poorer interest and engagement in diabetes educational programs what might have happened in our study once in our sample less adolescent patients reported knowledge on what HbA1c means than adult patients. The perception of all these factors should help diabetes team to focus on educational programs for adolescents to increase their level of knowledge on diabetes and consequently make their self-care behaviors stronger.26
Patients with better knowledge on what HbA1c means had lower HbA1c levels (current and in the last year) than patients who did not know its meaning. HbA1c levels reported by the patients had a positive correlation with last year’s HbA1c levels found in the medical records and with the current HbA1c levels, showing that the level of HbA1c could persist within the same range over a period of time. A recent retrospective study conducted in the USA in patients with T1D with persistent poor glycemic control showed little improvement during the follow-up of 9 years.11 We hypothesize that the same may occur in patients with good glycemic control. Both poor and good glycemic control could have an influence on metabolic memory; the legacy of poor glycemic control could predispose patients to evolve to micro- or macrovascular complications as described in the DCCT; in contrast, good glycemic control could prevent or postpone these complications.27
It is of note that in our study, after adjustment, the type of insulin regimen did not predict glycemic control. The relationship between the type of insulin regimen and glycemic control is still a matter of controversy.12,24 The lack of association between type of intensive insulin regimen and glycemic control was observed in the International Diabetes Management Practice Study (IDMPS),28 Hvidoere Study,24 and BrazDiab1SG.29 Moreover, a multicenter study conducted in Germany showed that patients on conventional insulin therapy, defined as three or less daily insulin shots, had better HbA1c levels than patients under intensive insulin regimens, including CSII.30 Considering intensive treatment with multiple daily insulin shots, one study has addressed the real-world adherence to insulin therapy in patients with T1D, which could be lower than expected.12 In the Exchange study, although 60% of the patients were using CSII, they still had a mean HbA1c of >8%.6 Two other variables associated with glycemic control were the number of SMBG performed daily and adherence to diet, both conditions closely related to a better diabetes management by the patient and described as predictors of good glycemic control in many studies.8,13,16,28–31 The IDMPS study, which had an arm in South America, has shown that both performing SMBG and participating in educational programs that include patients and multiprofessional teams were the predictors of good glycemic control.28
All the abovementioned facts point to the fact that we should rethink the kind of attention we are delivering to our patients with T1D.24,32 We should look for educational programs with support groups that aim to reach an adequate glycemic control, improve patients’ quality of life, and decrease the psychosocial burden of living with diabetes.33 The care that is delivered to patients with T1D should be centered in each individual patient, respecting this patient’s needs and preferences. It should also be tailored respecting each age group (children, adolescents, and adults).34 We should also plan population interventions with a team formed by several professionals from many different areas, with different skills to support all patients and in particular each one individually. Recently, several interventions have been proposed aiming to improve self-efficacy and patients’ empowerment and have presented better results mainly in the most disadvantaged patients who generally present poorer results regarding glycemic control.34
The major strength of our study is that we have evaluated a large sample of Brazilian young patients with T1D from four geographical regions of the country, representing our highly ethnically mixed population from different socioeconomic backgrounds using the same uniform protocol in all participating centers.
We have also to address some limitations of our study. Taking in account that only years of school attendance was common to both knowledge on what HbA1c means and HbA1c at goal in multivariate analysis, independent of socioeconomic status and ethnicity, we can consider that this variable was the most important factor, leading to better diabetes control. However, in both models of multivariate analysis, all the independent variables explain <25% of a given patient reaching the goal for HbA1c and also having the knowledge for what HbA1c means. We have to consider that other factors that were not assessed in our study could have negatively influenced our patients in not reaching these goals, such as impairment of cognitive function, poor family support, and many other adverse environmental factors. The use of only direct questions about HbA1c and SMBG to evaluate diabetes management could also be another limitation of our study.
Conclusion
In our cohort of Brazilian patients with T1D, a better knowledge on what HbA1c means was related to older ages, longer disease duration, longer follow-up in each center, lower frequency of self-reported hypoglycemia, Caucasian ethnicity, more years of school attendance, higher socioeconomic status, and participation in diabetes educational programs. These patients had also a better chance of reaching an adequate glycemic goal. Professionals involved in diabetes care teams should change their glucocentric approach to more proactive schedules, reinforcing education and patients’ skills to improve diabetes knowledge and empower them to have positive attitudes toward reaching and maintaining a good glycemic control.
Acknowledgments
We thank Mrs Elisangela Santos and Mr Vitor Branco Alves for their technical assistance. This study was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico do Brasil and Fundação do Amparo à Pesquisa do Estado do Rio de Janeiro.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Atlas, IDF. Brussels: International Diabetes Federation; 2015. | ||
American Diabetes Association. Standards of medical care. Diabetes Care. 2015;38(suppl 1):S70–S76. | ||
Cobas RA, Ferraz MB, Matheus AS, et al. The cost of type 1 diabetes: a nationwide multicenter study in Brazil. Bull World Health Organ. 2013;91(6):434–440. | ||
Nathan DM; DCCT/EDIC Research Group. DCCT/EDIC and complications study at 30 years: overview. Diabetes Care. 2014;37:9–16. | ||
Willi SM, Miller KM, DiMeglio LA, et al; for the T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135(3):424–434. | ||
Wood JR, Miller KM, Maahs DM, et al; for the T1D Exchange Clinic Network. Most youth with type 1 diabetes in the T1D exchange clinic registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes Clinical Guidelines. Diabetes Care. 2013;36(7):2035–2037. | ||
McKnight JA, Wild SH, Lamb MJ, et al. Glycaemic control of Type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabet Med. 2015;32(8):1036–1050. | ||
Gomes MB, Coral M, Cobas RA, et al. Prevalence of adults with type 1 diabetes who meet the goals of care in daily clinical practice: a nationwide multicenter study in Brazil. Diabetes Res Clin Prac. 2012;97(1):63–70. | ||
van Duinkerken E, Schoonheim MM, Steenwijk MD, et al. Ventral striatum, but not cortical volume loss, is related to cognitive dysfunction in type 1 diabetic patients with and without microangiopathy. Diabetes Care. 2014;37(9):2483–2490. | ||
Malerbi FEK, Negrato CA, Gomes MB. Assessment of psychosocial variables by parents of youth with type 1 diabetes mellitus. Diabetol Metab Syndr. 2012;4(1):48. | ||
Kim H, Elmi A, Henderson CL, Cogen FR, Kaplowitz PB. Characteristics of children with type 1 diabetes and persistent suboptimal glycemic control. J Clin Res Pediatr Endocrinol. 2012;4(2):82–88. | ||
Gomes MB, Negrato CA. Adherence to insulin therapeutic regimens in patients with type 1 diabetes. A nationwide survey in Brazil. Diabetes Res Clin Pract. 2016;28(120):47–55. | ||
Davison KA, Negrato CA, Cobas R, et al; Brazilian Type 1 Diabetes Study Group (BrazDiab1SG). Relationship between adherence to diet, glycemic control and cardiovascular risk factors in patients with type 1 diabetes: a nationwide survey in Brazil. Nutr J. 2014;7(13):19. | ||
Jankoska-Polanska B, Uchmanowicz I, dudek K, Mazur G. A recent study about relationship between patients’ knowledge and medication adherence among patients with hypertension. Patient Prefer Adherence. 2016;10:2437–2447. | ||
González FJL, Chiquete E; On behalf of the IDMPS-3W Collaborative Group (Mexico). Patients’ empowerment, physicians’ perceptions, and achievement of therapeutic goals in patients with type 1 and type 2 diabetes mellitus in Mexico. Patient Prefer Adherence. 2016;10:1349–1357. | ||
Lecomte P, Romon I, Fosse S, Simon D, Fagot-Campagna A. Self-blood glucose monitoring in people with type 1 and type 2 diabetes living in France. The Entred study 2001. Diabetes Metab. 2008;34:219–226. | ||
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and The Endocrine Society. Diabetes Care. 2013;36:1384–1395. | ||
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: World Health Organization; 2000;256. WHO Obesity Technical Report Series, n.284. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). Censo 2000. Available from: http:/www.ibge.gov.br. Accessed October 8, 2008. | ||
Malerbi DA, Franco LJ. Multicenter study of the prevalence of diabetes mellitus and impaired glucose tolerance in the urban Brazilian population aged 30–69 yr. The Brazilian Cooperative Group on the Study of Diabetes Prevalence. Diabetes Care. 1992;15:1509–1516. | ||
ABEP [webpage on the Internet]. Brazilian Economic Classification Criteria; 2010. Available from: http://www.abep.org/criterio-brasil. Accessed December 10, 2010. | ||
Nefs G, Bevelander S, Hendrieckx C, et al. Fear of hypoglycaemia in adults with Type 1 diabetes: results from Diabetes MILES – The Netherlands. Diabet Med. 2015;32(10):1289–1296. | ||
Cameron FJ, de Beaufort C, Aanstoot HJ, et al; Hvidoere International Study Group. Lessons from the Hvidoere International Study Group on childhood diabetes: be dogmatic about outcome and flexible in approach. Pediatr Diabetes. 2013;14(7):473–480. | ||
Dashiff CJ, McCaleb A, Cull V. Self-care of young adolescents with type 1 diabetes. J Pediatr Nurs. 2006;21(3):222–232. | ||
Gubitosi-Klug RA; for the DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: summary and future directions. Diabetes Care. 2014;37(1):44–49. | ||
Chan JC, Gagliardino JJ, Baik SH, et al; IDMPS Investigators. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care. 2009;32(2):227–233. | ||
Gomes MB, Cobas RA, Matheus AS, et al. Regional differences in clinical care among patients with type 1 diabetes in Brazil: Brazilian Type 1 Diabetes Study Group. Diabetol Metab Syndr. 2012;4(1):44. | ||
Ziegler R, Heidtmann B, Hilgard D, et al; for the DBV-Wiss-Initiative. Frequency of SBGM correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2010;12:11–17. | ||
Levine BS, Anderson BJ, Butler DA, Antisdel JE, Brackett J, Laffel LM. Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. J Pediatr. 2001;139(2):197–203. | ||
Cradock S, Cranston IC. Type 1 diabetes education and care: time for a rethink? Diabet Med. 2012;29(2):159–160. | ||
Due Christensen M, Zoffmann V, Hommel E, Lau M. Can sharing experiences in groups reduce the burden of living with diabetes, regardless of glycemic control? Diabetic Med. 2012;29:251–256. | ||
Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(12):2126–2140. | ||
Ammentorp J, Uhrenfeldt L, Angel F, Ehrensvärd M, Carlsen EB, Kofoed PE. Can life coaching improve health outcomes? A systematic review of intervention studies. BMC Health Serv Res. 2013;13:428. |
Supplementary materials
Brazilian Type 1 Diabetes Study Group
Executive steering committee: Marilia Brito Gomes (chair) and Carlos Antonio Negrato.
Principal investigators are indicated by an asterisk.
Department of Internal Medicine, Diabetes Unit, State University of Rio de Janeiro, Brazil: Marilia Brito Gomes and Roberta Arnaldi Cobas.
Federal University Hospital of Rio de Janeiro: Melanie Rodacki, MD; Lenita Zajdenverg, MD; and Joana Rodrigues Dantas, MD.
Diabetes Unit, University Hospital of São Paulo, São Paulo: Maria Lúcia Cardillo Corrêa-Giannella, MD; Sharon Nina Admoni, MD; and Daniele Pereira dos Santos, MD.
Bauru’s Diabetics Association, Bauru, São Paulo: Carlos Antonio Negrato, MD, and Maria de Fatima Guedes, MD.
Diabetes Unit, Federal University of São Paulo State, São Paulo: Sergio Atala Dib, MD, and Celso Ferreira de Camargo Sallum Filho, MD.
Diabetes Unit, University of Campinas, São Paulo: Elizabeth João Pavin, MD, and Caroline Takano, MD;
Clinical Hospital of the Federal University of Paraná: Rosângela Roginski Rea, MD, and Nicole Balster Romanzini, MD.
Clinical Hospital of Porto Alegre, Rio Grande do Sul: Mirela Azevedo, MD, and Luis Henrique Canani, MD.
Regional Hospital of Taguatinga, Brasília: Hermelinda Cordeiro Pedrosa, MD; Monica Tolentino; and Cejana Hamu Aguiar, MD.
Diabetes and Endocrinology Center of Bahia: Reine Marie Chaves Fonseca, MD; Ludmila Chaves Fonseca, MD; and Raffaele Kasprowicz, MD.
Diabetes and Hypertension Center of Ceará: Adriana Costa e Forti, MD, and Angela Delmira Nunes Mendes, MD.
Federal University of Ceará: Renan Montenegro Junior, MD, and Virgínia Oliveira Fernandes, MD.
Federal University Hospital of Pará: João Soares Felício, MD, and Flavia Marques Santos, MD.
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



