Back to Journals » Patient Preference and Adherence » Volume 14
Do Preferred Risk Formats Lead to Better Understanding? A Multicenter Controlled Trial on Communicating Familial Breast Cancer Risks Using Different Risk Formats
Authors Henneman L, van Asperen CJ, Oosterwijk JC, Menko FH, Claassen L, Timmermans DRM
Received 30 September 2019
Accepted for publication 7 January 2020
Published 19 February 2020 Volume 2020:14 Pages 333—342
DOI https://doi.org/10.2147/PPA.S232941
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Lidewij Henneman,1 Christi J van Asperen,2 Jan C Oosterwijk,3 Fred H Menko,4 Liesbeth Claassen,5 Daniëlle RM Timmermans5
1Department of Clinical Genetics, Amsterdam UMC, Vrije Universiteit, Amsterdam, the Netherlands; 2Department of Clinical Genetics, Leiden University Medical Center, Leiden, the Netherlands; 3Department of Genetics, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 4Family Cancer Clinic, Netherlands Cancer Institute, Amsterdam, the Netherlands; 5Department of Public and Occupational Health, Amsterdam UMC, Vrije Universiteit, Amsterdam, the Netherlands
Correspondence: Lidewij Henneman
Department of Clinical Genetics, Amsterdam UMC, Vrije Universiteit, PO Box 7057, 1007 MB, Amsterdam, the Netherlands
Tel +31 20-4449815
Email [email protected]
Purpose: Counselees’ preferences are considered important for the choice of risk communication format and for improving patient-centered care. We here report on counselees’ preferences for how risks are presented in familial breast cancer counseling and the impact of this preferred format on their understanding of risk.
Patients and Methods: As part of a practice-based randomized controlled trial, 326 unaffected women with a family history of breast cancer received their lifetime risk in one of five presentation formats after standard genetic counseling in three Dutch familial cancer clinics: 1) in percentages, 2) in frequencies (“X out of 100”), 3) in frequencies plus graphical format (10× 10 human icons), 4) in frequencies and 10-year age-related risk and 5) in frequencies and 10-year age-related risk plus graphical format. Format preferences and risk understanding (accuracy) were assessed at 2-week follow-up by a questionnaire, completed by 279/326 women.
Results: The most preferred risk communication formats were numbers combined with verbal descriptions (37%) and numbers only (26%). Of the numerical formats, most (55%) women preferred percentages. The majority (73%) preferred to be informed about both lifetime and 10-year age-related risk. Women who had received a graphical display were more likely to choose a graphical display as their preferred format. There was no significant effect between the intervention groups with regard to risk accuracy. Overall, women given risk estimates in their preferred format had a slightly better understanding of risk.
Conclusion: The results suggest that the accuracy of breast cancer risk estimation is slightly better for women who had received this information in their preferred format, but the risk format used had no effect on women’s risk accuracy. To meet the most frequent preference, counselors should consider providing a time frame of reference (eg, risk in the next 10 years) in a numerical format, in addition to lifetime risk.
Keywords: risk communication, breast cancer, genetic counseling, patient preference, understanding, risk accuracy
Introduction
Genetic counseling aims to enable counselees to make well-informed decisions with respect to genetic testing and preventive measures, based on the estimated risk of disease. However, effective risk communication is a major challenge because many counselees find it difficult to understand the concept of risk. Breast cancer genetic counseling generally takes place in specialized family cancer clinics. It includes information on the risk of having a hereditary predisposition for breast and ovarian cancer, and if a pathogenic BRCA1/BRCA2 germline mutation is found, the risk of developing breast and ovarian cancer as compared to the population risk. Since most counselees do not have a BRCA1/2 gene mutation, but have only mildly or moderately increased cancer risks, risk counseling for familial breast cancer is considered a key clinical activity. Moreover, the increasing development and use of risk stratification models1 will make breast cancer risk communication become even more important.
In current counseling practice, cancer risks are presented in many different formats. Although there is no consensus about the optimal format, some conclusions can be drawn based on previous studies. Verbal terms, such as “high risk” and “moderate risk” may appear straightforward but are interpreted in different ways by both patients and physicians, and may thus lead to confusion and ambiguous messages.2,3 Using numbers (eg, percentages: “15%” or frequencies: “1 in 7”) allows genetic counselors to be exact about the absolute size of the risk (given reliable risk figures), but also has disadvantages because many people have great difficulty in adequately interpreting numerical risk estimates.4 Visual aids or graphical formats are increasingly being used in addition to verbal and numerical risk estimates, and may be particularly beneficial to less literate or numeric individuals.5 Icons (population arrays), for example, allow the illustration of quantitative part-to-whole proportions and can counter denominator neglect since the size of the population is taken into account.6–8 There is, however, conflicting evidence about the degree to which they really help in improving understanding of risk and decision-making.5,9-13 Previously, we have shown that an additional graphical display (icons) did not lead to an increased understanding of breast cancer risks or more preventive intentions.14 Graphical displays have been perceived as helpful by counselees in understanding the risk,15–17 though some graphical formats may also be considered unhelpful or patronizing.16,18
The interpretation of risks also depends on the context in which the risks are framed, such as the time horizon in which they are presented.19 In the Netherlands, in national guidelines on familial breast cancer without an identified BRCA1/BRCA2 mutation, three risk categories are distinguished based on lifetime risks in percentages. These are often used in standard genetic counseling, because each category has a specific breast surveillance scheme. It has been argued that short-term risk projections, conditioned on current age (age-specific, eg, the next 5 or 10 years), may be easier to imagine and be less prone to misconceptions than lifetime projections,20–22 although they may lead to an underestimation of the total risk because the figures presented are relatively small. A recent study, however, showed that women with a BRCA1/2 mutation strongly overestimate their 10-year risk of developing breast cancer.23
Patient preferences are considered important for the choice of risk communication format and for improving patient-centered care. Although clear evidence is lacking,24 it is thought that preferred formats may reflect perceived relevance, familiarity, usability and meaningfulness, and hence be more successful in engaging counselees’ attention.25 In practice, the risk presentation format used does not always meet women’s preferences. Hallowell et al,26 for example, found that over 40% of women did not receive risk information in their preferred format when attending breast/ovarian cancer genetic counseling. Generally, people prefer to receive risk information that includes numbers.24,26,27 The reasons given are that numerical information is precise,24,27 that it sounds accurate24 and trustworthy,28 and that it helps to clarify the decision-making process.26
Preferences about how risk information is presented may depend on personal characteristics, in particular age and education. For example, older women preferred lifetime breast cancer risk estimates because the higher numbers were more persuasive and might encourage them to undergo screening.18 Icons/population arrays are generally not well known,29 but they are evaluated as helpful in promoting understanding,30 especially by people with low numeracy skills.17,31,32 Barnes et al,33 however, showed that tailoring risk communication to patient preferences may not always improve understanding of medical risks, particularly for less numerate women.
To assess individual preferences for the way in which risk information is given, most studies have used hypothetical scenarios or vignettes,15,18,25,27,29,34 qualitative study designs,18,25 a limited choice of formats,35 or included relatively few respondents in a limited setting.26 Moreover, studies generally assess the individuals’ preference without any previous knowledge of risk communication formats, which may have led to confusion because people did not understand the value of the additional formats presented.24,33
The study presented here is part of the large, multicenter BRISC study (Breast cancer RIsk Communication study) (Current Controlled Trials ISRCTN14566836). This was a randomized controlled trial (RCT) based on clinical practice. We asked unaffected women with familial breast cancer about their preferred risk communication format after they had been given their lifetime risk information in different formats in an additional consultation after standard clinical counseling (percentages; frequencies with or without graphical display; frequencies with or without 10-year age-related risk and with or without graphical display (icons)). The trial was performed to evaluate women’s preferences and the effect of different formats of risk communication on the counselees' understanding of their risk and on their psychological well-being, decision-making and satisfaction.36 In this paper, we focus on the impact of the intervention format on women preferences and their understanding of their risk.
We addressed the following research questions: 1) Which risk presentation format do women receiving for familial breast cancer counseling prefer?; 2) Are women’s preferences influenced by the format they received, by their age or by their education level?; 3) Do women who receive their risk estimates in their preferred format have a better understanding of their risk?
Materials and Methods
Participants
The BRISC study was carried out in three (of the nine) family cancer clinics in the Netherlands: VU University Medical Center Amsterdam, University Medical Centre Groningen and Leiden University Medical Centre. Unaffected women with a family history of breast cancer who were first-time attendees for breast cancer counseling were asked to participate in the study.36 A family history of breast cancer was defined as having at least one first-degree and/or second-degree relative with breast cancer, irrespective of whether a BRCA mutation had been detected in the family. Recruitment to participate took place between December 2005 and November 2007. All participants signed an informed consent form.
Design
The BRISC study was designed as an intervention RCT with pre- and post-test blocks to study the effects of the risk presentation format on counselees’ understanding, psychological well-being, decision-making and satisfaction. The study protocol has been approved by the VU University Medical Center Ethics Committee, Amsterdam, the Netherlands (protocol no. VUMC 2004/243). Participants provided written informed consent and the study was conducted in accordance with the Declaration of Helsinki. Here we focus on women’s preferences for and evaluation of different risk presentation formats in terms of understanding of their own risk.
Participants (n=326) were randomized in five intervention groups, each of which received an additional 30 mins dedicated risk consultation after an identical standard genetic counseling session. Consensus was reached to standardize the content and structure of the standard genetic counseling sessions prior to the intervention, ie, percentages were used when presenting risks. Randomization was set up as a Latin square design and took place at a “condition round” level. Every round took about 5 months for each condition. During the risk consultation participants’ risk of developing breast cancer was communicated in a different format: format 1 (= standard): lifetime risk in percentages (“X%”) (n=38); format 2: lifetime risk in frequencies (“X in 100”) (n=63); format 3: lifetime risk in frequencies + graphical display (icons; human figures in 10 rows of 10) (n=91); format 4: lifetime + age-related 10-year risk in frequencies (n=69); format 5: Lifetime + age-related 10-year risk in frequencies + graphical display (n=65). The additional consultation (intervention) was given by a so-called risk counselor, immediately after the standard genetic counseling session with a clinical geneticist or genetic counselor. The risk counselor was a researcher, intervention nurse or counselor who was specifically trained for the study. The risk counselor was informed about the counselee’s lifetime breast cancer risk estimation category (“not or slightly increased” (10–20%); “moderately increased” (20–30%); “highly increased” (30–40%)) by means of a “checklist after standard counseling” that was filled out by the genetic counselor at the end of the counseling session. Lifetime breast cancer risk was estimated by the genetic counselor using a model based on the Claus tables.37 For more details on the design and randomization, see Ockhuysen-Vermey et al.36
Measures
In the BRISC study, participants were asked to complete questionnaires at various times. The measures for this study were assessed 2 weeks after women had received the intervention session. Demographics (age, education, marital status, number of children, ethnicity) and other characteristics (family history of breast cancer) were gathered before the genetic counseling session.
Preference
Preference for risk format was measured by asking three questions:
- “If I had to choose, I would prefer to have my risks [of developing breast cancer] explained in: 1) numbers (eg, in percentages); 2) words (eg, ‘small risk’ or ‘high risk’); 3) both numbers and words; 4) a graphical display with numbers (a figure with 10x10 human icons was shown as an example, see14); or 5) a graphical display with words.”
- “If my risks [of developing breast cancer] were to be explained in numbers, I would prefer to hear it as: 1) a percentage (eg, 25%); 2) a certain number out of 100 (eg, 25 out of a 100); 3) one out of a certain number (eg, 1 in 4).”
- “If I had to choose, I would prefer to have my chance [of developing breast cancer] explained in: 1) the chance of getting breast cancer during my whole life; 2) the chance of getting breast cancer within the next 10 years; 3) the chance of getting breast cancer during my life as well as the chance of getting breast cancer within the next 10 years; 4) the chance of getting breast cancer during a different time period, which is. … (free text).”
Women’s understanding of their risk was assessed by measuring “risk accuracy”: a woman’s estimation of her own lifetime breast cancer risk, in frequencies (X out of 100), compared to the risk category communicated to her at intervention, ie, the counselee’s lifetime breast cancer risk estimation category (“not or slightly increased” (10–20%); “moderately increased” (20–30%); “highly increased” (30–40%)). If a woman’s risk estimation fell within the estimated risk category provided by the risk counselor, it was defined as accurate.
Data Analyses
Descriptive statistics were used to describe the sample characteristics. Preferences between subgroups were compared using chi-square tests. Two subgroup analyses using logistic regression were performed: (1) to examine whether a woman’s age influenced the preference for an age-related format, “age” (≤40 years vs >40 years of age) and “format” (age-related vs other formats) were entered as categorical predictor variables; and (2) to examine to what extent a woman’s educational level explained her preferences, “education level” (low vs high and intermediate vs high) and “format” (graphical format vs other format) were used as categorical predictor variables.
Logistic regression and analyses of variance were used to compare the “risk accuracy” between the five intervention groups, and between women who had received the risk estimates presented in their preferred format and women who received the risk in a format that they did not prefer. P-values <0.05 were considered statistically significant. The statistical program SPSS 20.0 for Windows (Chicago, Illinois, USA) was used for analysis.
Results
Two weeks after intervention, 279/326 women (86%) filled out the questionnaire. The main characteristics are presented in Table 1. Overall, 86% of the women had an intermediate to high education level, the mean age was 41 years (standard deviation (SD) 11) and 25% were at high risk (30–40%) of developing breast cancer. Baseline demographic or other participant characteristics did not differ between the groups (p > 0.05).
 |
Table 1 Characteristics of the Study Population |
Preferences for Risk Format
Women’s preferences for formats of risk communication after they had received the additional risk consultation are shown in Tables 2 and 3. Both “numbers and words” and “numbers only” were the most preferred formats with an overall percentage of 37% and 26%, respectively (Table 2). The least preferred format was “words supported by a graphical display” (overall 8%).
 |
Table 2 Preference for Risk Communication Format Among the Different Intervention Groups |
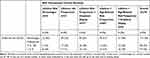 |
Table 3 Preference for Type of Numerical Format Among the Different Intervention Groups |
When choosing between percentages and frequencies, participants from all intervention groups preferred to hear their risks in percentages (overall 55%), followed by frequencies, either in the form of “X in 100” (25%) or in the “1 in X” format (20%) (Table 3). There were no significant differences between preferences for frequencies in the form of “X in 100 or in the form of “1 of X” among the participants of the different intervention groups (Table 3).
Regarding the preference for type of time frame, a majority of women (73%) preferred to be informed about both their lifetime risk and their 10-year age-related risk of getting breast cancer. Overall, 17% of participants preferred to receive only the lifetime risk, and 8% only the 10-year age-related risk (Table 4). Only 2% of the women preferred to have their risk explained in another time frame, such as a 2- or 5-year risk.
 |
Table 4 Preference for Type of Time Frame Among the Different Intervention Groups |
Preferences for Risk Format in Relation to Received Risk Format, Age and Educational Level
Women who had been informed of their risks in frequencies supported by a graphical display (intervention formats 3 and 5) were significantly more in favor of receiving their risks as numbers supported by graphical displays compared to those who had not received a graphical display (formats 1, 2 and 4) (on average 32% (formats 3 and 5) vs 7% (formats 1, 2 and 4); Lχ2(1) = 28.757, p < 0.001) (Table 2).
Women who had received their risks in frequencies in the form of X in 100 (formats 2–5) were, on average, more in favor of receiving their risks in that format than those who had received percentages (on average 26% (formats 2–5) vs 12% (format 1); Lχ2(1) = 3.825, p = 0.050) (Table 3).
Women who had received an age-related risk were slightly, but not significantly, more in favor of hearing their risk in a 10-year age-related format only, as compared with those who had received a lifetime risk (on average 10% (formats 4 and 5) vs 6% (formats 1–3); Lχ2(1) = 1.144, p = 0.284) (Table 4).
Overall, women over 40 were more likely to prefer the age-related format than younger women (12% vs 3%, odds ratio (OR) = 0.20; 95% confidence interval (CI 95) = [0.06 - 0.60]). The graphical display was preferred less by women with a low education level (5%) than those with an intermediate (19%) or high education level (23%) (OR = 0.17; CI 95 = [0.04 - 0.77]).
Preferences for Risk Format in Relation to Understanding of Their Own Lifetime Risk
Overall, at 2-week follow-up, women showed a good understanding of their own lifetime risk of getting breast cancer (ie, the woman’s risk estimation fell within the estimated risk category provided by the risk counselor) (Table 5). There was no significant difference between the intervention groups with regard to risk accuracy (all OR < 1.77; CI 95 = [0.463–6.760]). Women who received their risk estimates in their preferred format were slightly better at estimating their risk accurately than those who received their risk in a format they did not prefer (91% vs 82%, OR = 2.66; CI 95 = [1.174–6.010]). (Table 5).
 |
Table 5 Women’s Risk Accuracy in Each Intervention Group, in Relation to the Received and Prefered Formata |
Discussion
Preferences for risk communication format were assessed among unaffected women with a familial breast cancer risk who, after standard genetic consultation, were offered additional risk counseling using five different randomly assigned risk formats. In accordance with other studies,24,26,27,38 the majority of participants in all five intervention groups preferred to have their risks presented in numbers, either with or without words. Most women preferred to receive both their lifetime risk and their 10-year age-related risk.
Regarding the type of numerical format, percentages were most preferred, as was also found by an Australian study,24 which may also reflect women’s experiences and familiarity with percentages in the standard genetic counseling. In contrast, a United Kingdom study by Hallowell et al26 showed that proportions (“1 in X”) were preferred by 44% of women who were counseled for familial breast cancer, whereas 35% chose percentages. This preference for proportions may be related to the fact that these are more commonly used in cancer genetic counseling in the United Kingdom.39
Our results show that women who had received a graphical display (icons) were more likely to choose a graphical display as their preferred format. A qualitative study,18 in which breast cancer risk was communicated using icons, demonstrated that the respondents found the figures were easy to identify with, understandable and conveyed a meaningful message. In our study, women with a lower education level preferred a graphical display (icons) less than those with an intermediate or high education level. These findings differ from a qualitative study by Fortin et al,25 which reported a tendency for those with lower income and/or lower education to give icons a higher ranking than those with higher income/education. Moreover, in a study on cardiovascular medication risk, it was found that graphical displays were preferred over numbers by those with less education and those who were less numerate.17 It is possible that the complexity of graphical displays, especially in format 5 (where an age-related 10-year risk was also presented in icon arrays), made them less appealing to women with less education.
In our study most women preferred age-related time frames in addition to lifetime risk, the latter format is most often used in family cancer genetic counseling. In contrast, Fortin et al’s qualitative study25 showed that when women had to prioritize, more than half preferred lifetime risk over a 10- to 20-year risk format, in order “to see it all”. Also, in contrast to an earlier qualitative study among women in the general population,18 we found that older women preferred an age-related format more than younger women, probably because this is more in line with the counselee’s time horizon. The breast cancer risk varies considerably over a woman’s lifetime, and even more so for women with familial cancer. The residual risk diminishes with age and thus more specific age-related risks may be preferred by this older age group.
It has been recommended that counselors should try and meet individual preferences when communicating genetic risks.24,40 However, for cancer genetic counseling it has been shown that the counselees’ preferred format is not always the one used in practice.26 Observational studies have shown that, in routine genetic consultations, risk expressions are often presented only in a verbal format.24,40,41 A combination of verbal labels and numbers is also quite commonly used in current practice,24,26,40 which is more in line with women’s preferences for a combination of numbers and words. We found that using verbal expression only was one of the least preferred formats; most women preferred percentages, and this format is frequently used in Dutch counseling practice.40,42 Meeting women’s preferences may not always be feasible since different formats, such as age-related risk format or graphical displays, are not always readily available in practice, and it demands flexibility and skill from the counselor, which not all counselors can or will manage.42
Overall women were slightly better at estimating their risk accurately when they received their risk estimates in their preferred format. However, there were no significant differences in understanding of risk between the five intervention groups. In our study, possibly due to the measure used, the accuracy of estimating the risk was relatively high compared to earlier studies,43 leaving little room for improvement or for comparison between the intervention formats. Moreover, it has been argued that the format of risk presentation, whether preferred or not, is simply not very important in their decision-making24 because other aspects, such as their subjective experience with breast cancer in the family, psychological aspects and affect may be more important.44,45 Barnes et al,33 however, found that some individuals did better with their preferred format, but this result was likely mediated by numeracy. Those who were most numerate were more likely to prefer numerical formats and had higher risk comprehension. In contrast, those who preferred graphical formats did worse with these formats.
Strengths and Limitations
Our study has several strengths and limitations. One strength is that it was an RCT designed for a practice-based setting with a large group of women with familial breast cancer risk who were making real-life decisions, in contrast to earlier studies being more qualitative or limited in design. The primary outcome in this part of the BRISC study was women’s preferences in relation to risk understanding in oncogenetic counseling. Although the data were collected already several years ago, not much has changed in the counseling of risks of these women and we believe the findings are still valid and relevant. The design of the study meant we could also study the effect of receiving a risk estimate in a particular format on women’s preferences. Thus, in contrast to other studies, women in our study experienced the effect of having their own risk communicated on their understanding of this risk. Whether respondents preferred a format because they understood the risk better, or respondents understood the risk better and therefore preferred a specific format, cannot be determined. A limitation is that we only evaluated icons as a graphical display, whereas bar or pie graphs could also be used. It has been shown that people, including those from low-income groups, preferred the bar graph over the icons.46 Bar graphs may be particularly helpful when comparing multiple risks,18 and are, for example, available to support shared decision-making for women with a high risk of breast cancer.47 Another limitation is that numeracy skills were not assessed, which could have affected participants’ preferences, although we did include educational level. Finally, some intervention groups were rather small, which limited subgroup comparison.
Conclusion
In familial cancer counseling, there may be a difference between the format professionals use for communicating risks and their patients’ preferences. In this study, most women preferred to have their lifetime risk combined with a 10-year age-related risk in numerical format (percentages). Our results also suggest that women’s preference for a risk communication format is influenced by their previous experience with the risk format (as given in the additional risk counseling session) as well as with their age and education. Meeting women’s preferences for a particular format overall was associated with a slightly better understanding of their own risk, but there was no effect on women’s risk accuracy depending on the type of risk format used in the additional risk consultation session. Assessing women’s individual preferences will demand time, flexibility and skills from the counselor and therefore may not be feasible in practice. Because most women prefer age-related risk in addition to lifetime risk, counselors should consider adding a time frame of reference (eg, risk in the next 10 years) in a numerical format as standard practice. However, communicating risks in multiple risk formats may result in a more complex counseling process and information overload. Notably, we found women’s understanding of risk was high, regardless of whether women received their risks in their preferred format. Further studies are needed to investigate whether this affects their subsequent decision-making. Moreover, it has been argued that the format of risk presentation, whether preferred or not, may not be a crucial factor for women in familial breast cancer risk counseling, because other aspects such as subjective experiences with cancer in the family are more important in their decision-making.44
Data Sharing Statement
The dataset used is available from the corresponding author on reasonable request.
Acknowledgments
We thank Caroline Ockhuysen-Vermey, Ineke Bakker, Nandy Hofland, Monica Legdeur and Vera Giebels, and all the clinical geneticists and genetic counselors for their efforts in making this study possible. Special thanks are due to all the women who took the time for an extra counseling session and completing the questionnaires. Elisa García is acknowledged for critical review of the manuscript. We thank Kate McIntyre and Jackie Senior for editing the manuscript.
Funding
The study was funded by the Dutch Cancer Society (grant VU 2004-2994). The funder had no role in the study design, collection, analysis and interpretation of data or in writing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee A, Mavaddat N, Wilcox AN, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21:1708–1718. doi:10.1038/s41436-018-0406-9
2. Gurmankin AD, Baron J, Armstrong K. Intended message versus message received in hypothetical physician risk communications: exploring the gap. Risk Anal. 2004;24:1337–1347. doi:10.1111/risk.2004.24.issue-5
3. Timmermans D. The roles of experience and domain of expertise in using numerical and verbal probability terms in medical decisions. Med Decis Making. 1994;14:146–156. doi:10.1177/0272989X9401400207
4. Gigerenzer G, Gaissmaier W, Kurz-Milcke EL, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychol Sci Publ Interest. 2007;8:53–96. doi:10.1111/j.1539-6053.2008.00033.x
5. Garcia-Retamero R, Cokely ET. Designing visual aids that promote Risk literacy: a systematic review of health research and evidence-based design heuristics. Hum Factors. 2017;59:582–627. doi:10.1177/0018720817690634
6. Spiegelhalter D, Pearson M, Short I. Visualizing uncertainty about the future. Science. 2011;333:1393–1400. doi:10.1126/science.1191181
7. Garcia-Retamero R, Galesic M. Who profits from visual aids: overcoming challenges in people’s understanding of risks. Soc Sci Med. 2010;70:1019–1025. doi:10.1016/j.socscimed.2009.11.031
8. Gaissmaier W, Wegwarth O, Skopec D, Muller AS, Broschinski S, Politi MC. Numbers can be worth a thousand pictures: individual differences in understanding graphical and numerical representations of health-related information. Health Psychol. 2012;31:286–296. doi:10.1037/a0024850
9. McDowell M, Gigerenzer G, Wegwarth O, Rebitschek FG. Effect of tabular and icon fact box formats on comprehension of benefits and harms of prostate cancer screening: a randomized trial. Med Decis Making. 2019;39:41–56. doi:10.1177/0272989X18818166
10. Stellamanns J, Ruetters D, Dahal K, Schillmoeller Z, Huebner J. Visualizing risks in cancer communication: a systematic review of computer-supported visual aids. Patient Educ Couns. 2017;100:1421–1431. doi:10.1016/j.pec.2017.02.003
11. Chua HF, Yates JF, Shah P. Risk avoidance: graphs versus numbers. Mem Cognit. 2006;34:399–410. doi:10.3758/BF03193417
12. Waters EA, Weinstein ND, Colditz GA, Emmons K. Formats for improving risk communication in medical tradeoff decisions. J Health Commun. 2006;11:167–182. doi:10.1080/10810730500526695
13. Timmermans DR, Ockhuysen-Vermey CF, Henneman L. Presenting health risk information in different formats: the effect on participants’ cognitive and emotional evaluation and decisions. Patient Educ Couns. 2008;73:443–447. doi:10.1016/j.pec.2008.07.013
14. Henneman L, Oosterwijk JC, van Asperen CJ, et al. The effectiveness of a graphical presentation in addition to a frequency format in the context of familial breast cancer risk communication: a multicenter controlled trial. BMC Med Inform Decis Mak. 2013;13:55. doi:10.1186/1472-6947-13-55
15. Dolan JG, Iadarola S. Risk communication formats for low probability events: an exploratory study of patient preferences. BMC Med Inform Decis Mak. 2008;8:14. doi:10.1186/1472-6947-8-14
16. Edwards A, Thomas R, Williams R, Ellner AL, Brown P, Elwyn G. Presenting risk information to people with diabetes: evaluating effects and preferences for different formats by a web-based randomised controlled trial. Patient Educ Couns. 2006;63:336–349. doi:10.1016/j.pec.2005.12.016
17. Goodyear-Smith F, Kenealy T, Wells S, Arroll B, Horsburgh M. Patients’ preferences for ways to communicate benefits of cardiovascular medication. Ann Fam Med. 2011;9:121–127. doi:10.1370/afm.1193
18. Schapira MM, Nattinger AB, McHorney CA. Frequency or probability? A qualitative study of risk communication formats used in health care. Med Decis Making. 2001;21:459–467. doi:10.1177/0272989X0102100604
19. Keller C, Siegrist M, Gutscher H. The role of the affect and availability heuristics in risk communication. Risk Anal. 2006;26:631–639. doi:10.1111/risk.2006.26.issue-3
20. Bryant HE, Brasher PM. Risks and probabilities of breast cancer: short-term versus lifetime probabilities. CMAJ. 1994;150:211–216.
21. Asimakopoulou KG, Fox C, Spimpolo J, Marsh S, Skinner TC. The impact of different time frames of risk communication on Type 2 diabetes patients’ understanding and memory for risk of coronary heart disease and stroke. Diabet Med. 2008;25:811–817. doi:10.1111/dme.2008.25.issue-7
22. Evans DG, Lalloo F. Risk assessment and management of high risk familial breast cancer. J Med Genet. 2002;39:865–871. doi:10.1136/jmg.39.12.865
23. Speiser D, Rebitschek FG, Feufel MA, Brand H, Besch L, Kendel F. Accuracy in risk understanding among BRCA1/2-mutation carriers. Patient Educ Couns. 2019;102:1925–1931. doi:10.1016/j.pec.2019.05.007
24. Lobb EA, Butow PN, Meiser B, et al. Women’s preferences and consultants’ communication of risk in consultations about familial breast cancer: impact on patient outcomes. J Med Genet. 2003;40:e56. doi:10.1136/jmg.40.5.e56
25. Fortin JM, Hirota LK, Bond BE, O’Connor AM, Col NF. Identifying patient preferences for communicating risk estimates: a descriptive pilot study. BMC Med Inform Decis Mak. 2001;1:2. doi:10.1186/1472-6947-1-2
26. Hallowell N, Statham H, Murton F, Green J, Richards M. “Talking about chance”: the presentation of risk information during genetic counseling for breast and ovarian cancer. J Genet Couns. 1997;6:269–286. doi:10.1023/A:1025624221369
27. Wallsten TS, Budescu DV, Zwick R, Kemp SM. Preferences and reasons for communicating probabilistic information in verbal or numerical terms. Bull Psychon Soc. 1993;31:135–138. doi:10.3758/BF03334162
28. Gurmankin AD, Baron J, Armstrong K. The effect of numerical statements of risk on trust and comfort with hypothetical physician risk communication. Med Decis Making. 2004;24:265–271. doi:10.1177/0272989X04265482
29. Hamstra DA, Johnson SB, Daignault S, et al. The impact of numeracy on verbatim knowledge of the longitudinal risk for prostate cancer recurrence following radiation therapy. Med Decis Making. 2015;35:27–36. doi:10.1177/0272989X14551639
30. Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, Fagerlin A. Presenting research risks and benefits to parents: does format matter? Anesth Analg. 2010;111:718–723. doi:10.1213/ANE.0b013e3181e8570a
31. Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med. 2008;35:261–274. doi:10.1007/s12160-008-9037-8
32. Hess R, Visschers VH, Siegrist M. Risk communication with pictographs: the role of numeracy and graph processing. Judgm Decis Mak. 2011;6:263–274.
33. Barnes AJ, Hanoch Y, Miron-Shatz T, Ozanne EM. Tailoring risk communication to improve comprehension: do patient preferences help or hurt? Health Psychol. 2016;35:1007–1016. doi:10.1037/hea0000367
34. Price M, Cameron R, Butow P. Communicating risk information: the influence of graphical display format on quantitative information perception-Accuracy, comprehension and preferences. Patient Educ Couns. 2007;69:121–128. doi:10.1016/j.pec.2007.08.006
35. Ghosh K, Crawford BJ, Pruthi S, et al. Frequency format diagram and probability chart for breast cancer risk communication: a prospective, randomized trial. BMC Womens Health. 2008;8:18. doi:10.1186/1472-6874-8-18
36. Ockhuysen-Vermey CF, Henneman L, van Asperen CJ, Oosterwijk JC, Menko FH, Timmermans DR. Design of the BRISC study: a multicentre controlled clinical trial to optimize the communication of breast cancer risks in genetic counselling. BMC Cancer. 2008;8:283. doi:10.1186/1471-2407-8-283
37. van Asperen CJ, Jonker MA, Jacobi CE, et al. Risk estimation for healthy women from breast cancer families: new insights and new strategies. Cancer Epidemiol Biomarkers Prev. 2004;13:87–93. doi:10.1158/1055-9965.EPI-03-0090
38. Trevena LJ, Zikmund-Fisher BJ, Edwards A, et al. Presenting quantitative information about decision outcomes: a risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak. 2013;13(Suppl 2):S7. doi:10.1186/1472-6947-13-S2-S7
39. Hopwood P, Howell A, Lalloo F, Evans G. Do women understand the odds? Risk perceptions and recall of risk information in women with a family history of breast cancer. Community Genet. 2003;6:214–223.
40. Pieterse AH, van Dulmen S, van Dijk S, Bensing JM, Ausems MG. Risk communication in completed series of breast cancer genetic counseling visits. Genet Med. 2006;8:688–696. doi:10.1097/01.gim.0000245579.79093.86
41. Michie S, Lester K, Pinto J, Marteau TM. Communicating risk information in genetic counseling: an observational study. Health Educ Behav. 2005;32:589–598. doi:10.1177/1090198105278562
42. Henneman L, Marteau TM, Timmermans D. Clinical geneticists’ and genetic counselors’ views on the communication of genetic risks: a qualitative study. Patient Educ Couns. 2008;73:42–49. doi:10.1016/j.pec.2008.05.009
43. Smerecnik CM, Mesters I, Verweij E, de Vries NK. de VH. A systematic review of the impact of genetic counseling on risk perception accuracy. J Genet Couns. 2009;18:217–228. doi:10.1007/s10897-008-9210-z
44. Rees G, Fry A, Cull A. A family history of breast cancer: women’s experiences from a theoretical perspective. Soc Sci Med. 2001;52:1433–1440. doi:10.1016/S0277-9536(00)00248-3
45. van Driel CMG, Oosterwijk JC, Meijers-Heijboer EJ, et al. Psychological factors associated with the intention to choose for risk-reducing mastectomy in family cancer clinic attendees. Breast. 2016;30:66–72. doi:10.1016/j.breast.2016.08.016
46. Royak-Schaler R, Klabunde CN, Greene WF, et al. Communicating breast cancer risk: patient perceptions of provider discussions. Medscape Womens Health. 2002;7:2.
47. Kurian AW, Munoz DF, Rust P, et al. Online tool to guide decisions for BRCA1/2 mutation carriers. J Clin Oncol. 2012;30:497–506. doi:10.1200/JCO.2011.38.6060
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
