Back to Journals » Journal of Pain Research » Volume 11
Do liposomal bupivacaine infiltration and interscalene nerve block provide similar pain relief after total shoulder arthroplasty: a systematic review and meta-analysis
Authors Sun H, Li S, Wang K, Zhou J, Wu G, Fang S, Sun X
Received 20 June 2018
Accepted for publication 26 July 2018
Published 18 September 2018 Volume 2018:11 Pages 1889—1900
DOI https://doi.org/10.2147/JPR.S177716
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Han Sun,* Shuxiang Li,* Kun Wang, Jian Zhou, Guofeng Wu, Sheng Fang, Xiaoliang Sun
Department of Articular Orthopaedics, The Third Affiliated Hospital of Soochow University, Changzhou 213003, Jiangsu, China
*These authors contributed equally to this work
Objective: Controversy still exists regarding the efficiency and safety of liposomal bupivacaine (LB) vs interscalene nerve block (INB) for pain management after total shoulder arthroplasty (TSA). The aim of the present meta-analysis was to perform a relatively credible and overall assessment to compare the efficiency and safety of LB-based infiltration vs INB for pain management after TSA.
Methods: The PubMed, Cochrane Library, Web of Science, and EMBASE were systematically searched. Only studies published up to March 2018 comparing LB vs INB for pain control after TSA were included. The primary outcome extracted from the studies was postoperative pain score at different periods. The secondary outcomes included total opioid consumption, length of hospital stay, and complications.
Results: Seven studies with 707 patients were included in this study. No statistically significant difference was observed between the LB and INB groups in pain scores at 8 hours, 12 hours, 24 hours, postoperative day (POD) 1, and POD 2. The two groups also showed comparable total opioid consumption at POD 0, POD 1, POD 2, and length of hospital stay. The LB group had a significantly higher pain score at 4 hours (standard mean difference =0.65, 95% CI=0.07 to 1.24, P=0.03) but a lower occurrence rate of complications than did the INB group (OR =0.51, 95% CI=0.28 to 0.91, P=0.02).
Conclusion: This meta-analysis revealed that INB provides excellent analgesic effects within 4 hours after TSA, while patients treated with LB infiltration experienced significantly less occurrence rate of complications after TSA. In general, both approaches provide similar overall pain relief and have similar opioid consumption after TSA, with no significant difference in the length of hospital stay. Nevertheless, more high-quality randomized controlled trails with long-term follow-up are still required to make the final conclusion.
Keywords: liposomal bupivacaine, interscalene nerve block, total shoulder arthroplasty, meta-analysis
Introduction
Total shoulder arthroplasty (TSA) is an effective and common surgical treatment, with well-proven efficacy in relieving pain and improving shoulder function in patients experiencing degenerative arthritis.1,2 A previous study indicated that the annual growth rates of TSA were higher than those of total hip and knee arthroplasty. By 2015, a further increase of 192%–322% has been estimated.3 Considering the continuously increasing number of TSAs being performed, establishing a reasonable postoperative pain control program has become essential. Furthermore, poor perioperative pain control can lead to a variety of adverse outcomes, including decreased patient satisfaction, delayed ambulation, increased medical expenses, or unnecessary family burden, and a series of complications caused by prolonged hospitalization.4,5
Interscalene nerve block (INB) can provide reliable analgesic coverage for the entire field of surgery and has been recognized as an effective regional technique for pain control in patients undergoing TSA.6 Compared with general anesthesia, INB is correlated with reduced pain, decreased opioid consumption, better sleep quality, shorter hospital stay, and increased patient satisfaction.7,8 However, concerns remain about the 10%–20% failure rate of nerve blockade and the possibility of neurologic or respiratory complications stemming from INB.9 Recently, local infiltration using liposomal bupivacaine (LB) has been favored by surgeons for its potential to provide extended postoperative pain relief. Compared with traditional local anesthetics, LB has advantages including a relatively longer analgesic effect and less morphine consumption.10–13 Moreover, central sensitization and neuropathic pain may be prevented by decreasing inflammation and blocking pain receptors at the surgical site.14
Several meta-analyses comparing LB and INB for pain control after TSA have been published in 2017.15–17 However, we found that a retrospective study was mistakenly considered a randomized controlled trial (RCT) in two RCT-based meta-analyses.15,16,18 Additionally, we noticed a new RCT and a new retrospective study were published in 2017.19,20 Therefore, we considered it necessary to conduct a new meta-analysis to perform a relatively more credible and overall assessment of the efficiency and safety of LB-based infiltration and INB for pain management after TSA.
Methods
Search strategy
We followed the PRISMA reporting guidelines and the recommendations of Cochrane Collaboration when conducting this meta-analysis. Four electronic databases, namely, PubMed (1966 to March 2018), Web of Science (1950 to March 2018), EMBASE (1980 to March 2018), and Cochrane Library (up to March 2018), were searched for potential studies. The following search key terms were used: liposomal bupivacaine, interscalene nerve block, total shoulder arthroplasty, total shoulder replacement, pain control, pain management, and analgesia. We used the Boolean operators “OR” and “AND” to combine the literature searches. The references in full-text articles were manually searched to avoid omitting any potential studies. We imposed no restriction on publication language.
Inclusion and exclusion criteria
Studies were included in the present meta-analysis if they met the following criteria: 1) patients aged ≥18 years who underwent shoulder arthroplasty; 2) the experimental group received LB and the control group received INB for pain control; and 3) at least one of the following outcomes is measured: pain score, opioid consumption, length of hospital stay, and complications. The exclusion criteria included biochemical trials, reviews, case reports, retrospective studies, no assessment of the abovementioned outcomes, or no comparison between INB and LB after TSA.
Two independent authors followed the unified search strategy to screen potentially relevant studies based on the article titles and abstracts. Any inconsistencies between the reviewers were resolved by discussion and consensus with the third author to make a final decision on study inclusion if a consensus could not be reached.
Data extraction
The authors extracted relevant data in duplicate from the included studies by using a standardized form. The following information was extracted: author name, publication year, source and design of study, sample size, inclusion and exclusion criteria, dosage and type of anesthetic drug, duration of follow-up, and outcome measurements. The primary outcome extracted from the studies was the postoperative pain score at different periods. The secondary outcomes included total opioid consumption, length of hospital stay, and complications. If incomplete data were encountered, we tried our best to contact the corresponding authors for more information. If the communication failed, we then extracted the data from figures or calculated them by using the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0.
Risk-of-bias assessment
Two independent reviewers evaluated the risk of bias of the included RCTs on the basis of the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 by using Cochrane Collaboration’s tool for assessing the risk of bias. The score consisted of seven items, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias.21,22 When evaluating the methodological quality of retrospective studies, the Methodological Index for Non-randomized Studies criteria were used.23
Data synthesis
The present study was performed using Review Manager (RevMan Version 5.3, The Cochrane Collaboration, Copenhagen, Denmark). ORs with 95% CI or standard mean difference (SMD) with 95% CI was assessed for dichotomous outcomes or continuous outcomes, respectively. P<0.05 was set as the level of significance. A result was also considered statistically significant if “1” was not included in the 95% CI of OR or “0” was not included in the 95% CI of SMD. The Q test and I2 statistic were used to assess heterogeneity. A fixed-effects model was used if P>0.1 and I2<50%, which indicated homogeneity. On the contrary, a random-effects model was used when P≤0.1 or I2≥50%. The origins of heterogeneity were investigated using the sensitivity analysis.
Assessments of quality of evidence
We assessed the quality of evidence of the outcomes by using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system that included the following items: risk of bias, stable effect, inconsistency, and imprecision.24 The recommended levels of evidence were classified into four categories, including very low, low, moderate, and high. Any disagreement was resolved through discussion with a third reviewer.
Ethics approval and consent to participate
Ethical approval was not necessary because the present meta-analysis was performed on the basis of previous published studies. Consent for publication was also not necessary because no details, images, or videos relating to individual participants are included in this meta-analysis.
Results
Study selection
By using the key phrases mentioned above, we identified 150 relevant articles from the following databases: 25 from PubMed, 60 from Web of Science, 54 from EMBASE, and 11 from Cochrane Library. Ten studies were screened for eligibility and the full text read after excluding duplicate and irrelevant studies. Thereafter, three reviews were excluded on the basis of the exclusion criteria.15–17 Finally, of the 150 studies, four RCTs and three retrospective studies published between 2016 and 2017 were included in our meta-analysis (Figure 1).18–20,25–28
  | Figure 1 Search results and the selection procedure. Note: Reprodcued from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement.32 |
Study characteristics
The characteristics of the included studies are summarized in Table 1. We identified four RCTs20,25,27,28 and three retrospective controlled studies18,19,26 in our study. The trials compared LB vs INB for pain control after TSA. All seven studies evaluated patients >18 years old who underwent either TSA or reverse TSA. The sample sizes of the included studies ranged from 57 to 214. The mean age across all of the studies was >63 years. The drug dose of the LB or INB group was similar in all studies. The follow-up time ranged from 1 day to 21 weeks.
Quality assessment
Table 2 summarizes our standardized assessment of risk of bias. All of the RCTs described a methodology of randomization. Clear inclusion and exclusion criteria were also provided in all articles. All RCTs had a low risk of concealment of allocation and complete outcome data were reported. None of these studies fully reported the blinding of participants and personnel, and the study by Namdari et al27 even failed to report the blinding of outcome assessment. On the other hand, all the three nonrandomized cohort studies contained a clearly stated aim, endpoints appropriate to the aim of the study, lost to follow-up <5%, an adequate control group, baseline equivalence of groups, and adequate statistical analyses. None of these studies fully meet the criteria of prospective collection of data, unbiased assessment of the study endpoint, and follow-up period appropriate to the aim of the study. There was variable reporting of inclusion of consecutive patients, prospective calculation of the study size, and contemporary groups.
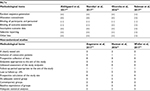  | Table 2 Methodological quality and risk of bias assessment of included studies Note: (+), positive; (-), negative. Abbreviation: RCTs, randomized controlled trials. |
Synthesis of results and meta-analysis
Pain scores at 4, 8, 12, and 24 hours after surgery
Three studies reported the pain scores at 4 hours after TSA.20,27,28 Since there was significant heterogeneity (I2=81%, P=0.006), a random-effects model was employed. The result of the meta-analysis showed that the pain score at 4 hours in the LB group was significantly higher than that in the INB group (SMD =0.65, 95% CI=0.07 to 1.24, P=0.03; Figure 2A).
The pain score at 8 hours after TSA was presented in three studies.20,27,28 A random-effects model was utilized because of high heterogeneity (I2=90%, P<0.001). Data pooled from these studies showed no statistically significant difference between the LB and INB groups in postoperative pain score at 8 hours (SMD =0.41, 95% CI=-0.41 to 1.24, P=0.33; Figure 2B).
The outcomes of pain score at 12 hours after TSA were reported in five studies.19,20,26–28 Given the significant heterogeneity among these studies (I2=53%, P=0.07), a random-effects model was used. The pooled results revealed that the two groups had comparable pain scores at 12 hours (SMD =–0.01, 95% CI=-0.33 to 0.31, P=0.96; Figure 2C).
Seven reports included the pain scores at 24 hours after TSA.18–20,25–28 Obvious heterogeneity was found among these studies (I2=72%, P=0.001); hence, a random-effects model was used. After pooling the results, we found that the pain scores at 24 hours after TSA were similar between the LB group and the INB group (SMD =–0.17, 95% CI=-0.48 to 0.13, P=0.26; Figure 2D).
Pain scores at postoperative day (POD) 1 and POD 2
The pain scores at POD 1 after TSA were provided in four studies.19,20,25,28 A fixed-effects model was used because of low heterogeneity (I2=0%, P=0.48). The difference in pain scores at POD 1 between the LB and INB groups was not statistically significant according to our analysis (SMD =0.10, 95% CI=-0.15 to 0.35, P=0.42; Figure 2E).
Four studies reported the pain scores at POD 2 after TSA.19,20,25,28 No significant heterogeneity was found (I2=0%, P=0.85), and hence, a fixed-effects model was used. Similarly, the pooled results showed that the two groups had comparable pain scores at POD 2 (SMD =0.16, 95% CI=-0.10 to 0.42, P=0.24; Figure 2F).
Total opioid consumption at PODs 0, 1, and 2
A total of six studies provided the outcomes regarding total opioid consumption at POD 0.18–20,25,26,28 Significant heterogeneity was observed (I2=80%, P=0.0002), and hence, a random-effects model was applied. The pooled results demonstrated no statistically significant difference between the LB and INB groups regarding total opioid consumption at POD 0 (SMD =0.21, 95% CI=-0.16 to 0.58, P=0.27; Figure 3A).
Total opioid consumption at POD 1 was reported in four studies.20,25,26,28 The fixed-effects model was used to perform the meta-analysis as no statistical heterogeneity was found between the included studies (I2=0%, P=0.70). The pooled results revealed that the LB group consumed more opioids than did the INB group at POD 1, but with no statistical significance (SMD =0.22, 95% CI=–0.03 to 0.46, P=0.08; Figure 3B).
Total opioid consumption at POD 2 was provided in only three studies.25,26,28 Significant heterogeneity was found (I2=88%, P=0.0002) in the pooled result; therefore, a random-effects model was employed. The result of the meta-analysis revealed that the LB group consumed similar opioids when compared with the INB group at POD 2 (SMD =0.00, 95% CI=–0.86 to 0.86, P=0.01; Figure 3C).
Length of hospital stay
A total of six studies showed the data on the length of hospital stay.19,20,25–28 A random-effects model was utilized because of high heterogeneity (I2=52%, P=0.06). We found no statistically significant difference between the two groups in the length of hospital stay (SMD =–0.04, 95% CI=–0.31 to 0.23, P=0.78; Figure 4).
  | Figure 4 A forest plot diagram showing the length of hospital stay after total shoulder arthroplasty. Abbreviations: INB, interscalene nerve block; LB, liposomal bupivacaine. |
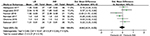
Complications
Complications after surgery were reported in all the included studies.18–20,25–28 In total, 17 of 295 patients in the LB group and 64 of 412 patients in the INB group experienced various kinds of complications during or after the surgery. Our analysis revealed that the LB approach had a significantly less ratio of complications (OR =0.51, 95% CI=0.28 to 0.91, P=0.02; Figure 5). As no heterogeneity was found (I2=0%, P=0.81), the fixed-effects model was used during the analysis.
  | Figure 5 A forest plot diagram showing the occurrence rate of complications during or after total shoulder arthroplasty. Abbreviations: INB, interscalene nerve block; LB, liposomal bupivacaine. |
Sensitivity analysis
Owing to the significant heterogeneity in pain scores at 4 hours (I2=81%), 8 hours (I2=90%), 12 hours (I2=53%), 24 hours (I2=72%), total opioid consumption at POD 0 (I2=86%) and POD 2 (I2=88%), and length of hospital stay (I2=52%), the sensitivity analysis was performed in our meta-analysis to investigate the source of heterogeneity. The sensitivity analysis revealed that the study by Sabesan et al20 led to the heterogeneity in pain scores at 4 and 8 hours while the report of Hannan et al26 was the main contribution of the heterogeneity in total opioid consumption at POD 2, and if we excluded their studies, the high heterogeneity of the two outcomes disappeared immediately (I2=0%). However, when we analyzed the source of heterogeneity in pain scores at 12 and 24 hours after surgery, as well as total opioid consumption at POD 0, the results could hardly achieve material alteration by eliminating any study.
Quality of evidence
The GRADE system was used to evaluate the quality of outcomes in this study. The overall evidence for each outcome was moderate to very low, which may lower the confidence in any recommendations. The detail of each assessment is listed in Table 3.
Publication bias
As the number of included studies in each assessment did not reach the cutoff value, the publication bias and funnel plots might be not reliable and appropriate in this study.
Discussion
When it came to the question about the efficiency of LB compared with INB in pain management after TSA, there seemed to be no definitive answer which leads us to perform this meta-analysis. Compared with previous meta-analyses, this report gives the new knowledge that LB might be associated with higher pain scores at 4 hours and significantly lower occurrence rate of complications than INB after TSA.15–17 No significant difference was found in terms of postoperative pain scores at 8 hours, 12 hours, 24 hours, POD 1, and POD 2 between the LB and INB groups. Moreover, no significant differences were observed in total opioid consumption at POD 0, POD 1, POD 2, and length of hospital stay between the LB and INB groups.
The primary outcome evaluated in the present study was the pain score at different periods. Most of the included studies used the visual analog scale except for the studies by Sabesan et al, Angerame et al, and Hannan et al which assessed pain levels by using the numeric pain rating scale.19,20,26 The pooled data indicated that the LB group had a higher pain level at 4 hours after surgery than did the INB group; however, similar pain scores were found at 8, 12, and 24 hours after surgery. Some previous studies suggested that LB was created by using a lipid-based delivery system that releases bupivacaine from liposomal particles during a 72-hour time period.13,29 Therefore, some studies speculated that the high pain score in the early postoperative period in the LB group could be attributed to the delayed release of bupivacaine from lipid stores, leading to low bupivacaine levels in plasma. Hence, patients who received LB could supplement the anesthetic appropriately before 4 hours after surgery to compensate for its delayed analgesic effect. Additionally, the two approaches yielded comparable outcomes thereafter, as no significant intergroup differences in pain scores were found at PODs 1 and 2 according to our meta-analysis. So LB has pain control similar to INB after 4 hours after TSA.
Total opioid consumption was also considered a reasonable indicator for assessing the analgesic effect. Opioids, including oral and patient-controlled analgesia, are commonly used as supplementary means of postoperative pain control. The related side effects of opioids include nausea, vomiting, drug dependence, hypotension, and respiratory depression, which inevitably delay functional recovery and reduce patient satisfaction.30,31 Therefore, minimizing opioid consumption might lead to better physical outcomes. Weller et al showed that patients receiving LB consumed more oral morphine equivalent than did those receiving INB at POD 0.18 In 2017, Angerame et al reported that the LB and INB groups had comparable total opioid use.19 A retrospective cohort study conducted by Hannan et al indicated no statistically significant difference in opioid consumption between the two groups at POD 1, while a larger amount of opioid consumption was found in the INB group than in the LB group at PODs 2 and 3.26 By pooling these results, our meta-analysis indicated that the two groups consumed a similar amount of opioids at PODs 0, 1, and 2 after TSA. This result indirectly verified the aforementioned comparable outcomes of pain scores at the same time point between the LB and the INB.
In addition to pain release, complications and patient satisfaction are important elements that affect the application of a technique in pain control. As the LB approach mainly depends on soft-tissue infiltration rather than catheter placement, it was considered safer than the INB approach. This inference was verified by our meta-analysis as significant superiority was found in LB group with regard to the occurrence rates of complications during or after TSA. It should be noted that because of the limited data in the included studies, we could only perform a general analysis of the total occurrence ratio of various kinds of complications. More specifically, for some common complications, such as respiratory distress that was observed in two patients in the LB group and eight patients in the INB group. Moreover, one patient in the LB group and two patients in the INB group suffered from pulmonary embolism, one patient in the LB group and one patient in the INB group experienced deep venous thrombosis, and eighteen patients in the LB group and fourteen patients in the INB group had nausea. Additionally, there were thirty-four catheter leakage/nonfunctioning in the INB group. Therefore, the main beneficial effect of the LB approach may be the lower incidence of catheter-related complications. When it comes to patient satisfaction, only Sabesan et al reported the American Shoulder and Elbow Surgeons (ASES) shoulder score, the Penn Shoulder Score (PSS), and the Subjective Shoulder Value among participants.20 The LB group had significantly better ASES and PSS scores than did the INB group at the last follow-up, which indicated that LB might contribute to better postoperative shoulder function than does INB. However, more high-quality studies are warranted for further investigation.
The length of hospital stay was associated with the curative effect. As previous results revealed that the two groups had comparable pain scores, the length of stay was forecasted to be similar as well. This prediction was then confirmed by our meta-analysis as no statistical difference was found after pooling the results. However, the medical expense during hospitalization may differ between the two groups. Although the included studies provided insufficient data that prevented a meta-analysis from being conducted, two of these studies provided some details on this topic. Okoroha et al28 found that the average wholesale acquisition cost of LB was $315, while the physician fee for INB was $1,583, which was consistent with the result of Weller et al18 ($289.04 vs $1,559.42). Sabesan et al revealed that the cost in the LB group appeared to be $300 cheaper than that in the INB group even with the addition of a single bolus interscalene block, not to mention the significant expense in terms of the need for specialized equipment, anesthesia expertise, and additional time required for catheter placement in the INB group.20 From this perspective, LB is a more cost-effective alternative to INB for pain management.
It should be noted that some factors may influence the outcomes of the study. First, despite the similar mean ages of the patients in each study, the ranges of these ages revealed large difference, which may result in the deviation of therapeutic effect. Second, the types and doses of drugs in the INB group were various in the included studies, which contained ropivacaine and bupivacaine ranging from 20 to 40 mL. These two factors tend to influence the pain release of the INB. Third, the INB approach requires the catheter placement, so the effects and relevant complications of INB are highly dependent on the skill of the operator. Fourth, some of these included studies used the patient-controlled analgesia with opioids for the concomitant pain management, while the others applied the oral morphine equivalent, which may affect the total opioid consumption after TSA. Therefore, more high-quality studies with relevant information are needed for a more classified and detailed analysis.
In summary, INB is more superior in pain release within 4 hours after TSA while LB holds lower occurrence rate of complications. Both the approaches are proven to be effective and safe for the pain management of TSA. However, when referring to applying the knowledge for routing clinical practice, specialized personnel/equipment requirement and medical expense should also be taken into consideration. Based on the as-presented evaluation, a recommendation is that patients with higher request to pain release may consider the INB approach, while LB is more suitable for hospitals without corresponding qualification or patients with poor economic condition.
The current systematic review and meta-analysis has some limitations: (1) only seven studies with 707 patients were included in the present study, which decreased the quality of evidence in our meta-analysis and limited the evaluation of publication bias; 2) because of the limited data in the included studies, it was difficult to perform a meta-analysis of specific complications and functional outcomes, and hence, comprehensive assessments of these two outcomes between the two groups could not be performed; 3) the follow-up time in the included studies was relatively short, and hence, the evaluations of outcomes (eg, complications or patient satisfaction) of long-term follow-up are lacking in this meta-analysis; more studies with follow-up periods >1 year are needed; 4) heterogeneity was found in most results of the pooled estimate, and hence, the reliability of these results might be influenced; and 5) standard deviations in the study by Abildgaard et al, Angerame et al, and Hannan et al were calculated according to the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 or extract from figures, which may have slightly influenced the accuracy of the results.19,25,26
Conclusion
INB provides excellent analgesic effects within 4 hours after TSA, while patients treated with LB infiltration experienced significantly less occurrence rate of complications after TSA. In general, the two approaches provide similar overall pain relief and have similar opioid consumption after TSA, with no significant difference in the length of hospital stay. However, when considering the equipment and skill requirement for the INB approach, LB infiltration is more recommendable to hospitals without enough qualified personnel or patients with poor economic condition. Nevertheless, more high-quality RCTs with long-term follow-up are still required to make the final conclusion.
Acknowledgment
We would like to show sincere appreciation to the anonymous reviewers for their many useful comments on the early version of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am. 2005;87(9):1947–1956. | ||
Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471–479. | ||
Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93(24):2249–2254. | ||
Mahoney A, Bosco JA 3rd, Zuckerman JD. Readmission after shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(3):377–381. | ||
Schairer WW, Zhang AL, Feeley BT. Hospital readmissions after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(9):1349–1355. | ||
Shah A, Nielsen KC, Braga L, Pietrobon R, Klein SM, Steele SM. Interscalene brachial plexus block for outpatient shoulder arthroplasty: postoperative analgesia, patient satisfaction and complications. Indian J Orthop. 2007;41(3):230–236. | ||
Fredrickson MJ, Ball CM, Dalgleish AJ. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg Anesth Pain Med. 2010;35(1):28–33. | ||
Goebel S, Stehle J, Schwemmer U, Reppenhagen S, Rath B, Gohlke F. Interscalene brachial plexus block for open-shoulder surgery: a randomized, double-blind, placebo-controlled trial between single-shot anesthesia and patient-controlled catheter system. Arch Orthop Trauma Surg. 2010;130(4):533–540. | ||
Bishop JY, Sprague M, Gelber J, et al. Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elbow Surg. 2006;15(5):567–570. | ||
Bergese SD, Ramamoorthy S, Patou G, Bramlett K, Gorfine SR, Candiotti KA. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res. 2012;5:107–116. | ||
Bramlett K, Onel E, Viscusi ER, Jones K. A randomized, double-blind, dose-ranging study comparing wound infiltration of DepoFoam bupivacaine, an extended-release liposomal bupivacaine, to bupivacaine HCl for postsurgical analgesia in total knee arthroplasty. Knee. 2012;19(5):530–536. | ||
Golf M, Daniels SE, Onel E. A phase 3, randomized, placebo-controlled trial of DepoFoam® bupivacaine (extended-release bupivacaine local analgesic) in bunionectomy. Adv Ther. 2011;28(9):776–788. | ||
Surdam JW, Licini DJ, Baynes NT, Arce BR. The use of exparel (liposomal bupivacaine) to manage postoperative pain in unilateral total knee arthroplasty patients. J Arthroplasty. 2015;30(2):325–329. | ||
Woolf CJ, Chong MS. Preemptive analgesia--treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77(2):362–379. | ||
Cao X, Pan F. Comparison of liposomal bupivacaine infiltration versus interscalene nerve block for pain control in total shoulder arthroplasty: a meta-analysis of randomized control trails. Medicine (Baltimore). 2017;96(39):e8079. | ||
Wang K, Zhang HX. Liposomal bupivacaine versus interscalene nerve block for pain control after total shoulder arthroplasty: a systematic review and meta-analysis. Int J Surg. 2017;46:61–70. | ||
Yan Z, Chen Z, Ma C. Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: a meta-analysis. Medicine (Baltimore). 2017;96(27):e7226. | ||
Weller WJ, Azzam MG, Smith RA, Azar FM, Throckmorton TW. Liposomal bupivacaine mixture has similar pain relief and significantly fewer complications at less cost compared to indwelling interscalene catheter in total shoulder arthroplasty. J Arthroplasty. 2017;32(11):3557–3562. | ||
Angerame MR, Ruder JA, Odum SM, Hamid N. Pain and opioid use after total shoulder arthroplasty with injectable liposomal bupivacaine versus interscalene block. Orthopedics. 2017;40(5):e806–e811. | ||
Sabesan VJ, Shahriar R, Petersen-Fitts GR, et al. A prospective randomized controlled trial to identify the optimal postoperative pain management in shoulder arthroplasty: liposomal bupivacaine versus continuous interscalene catheter. J Shoulder Elbow Surg. 2017;26(10):1810–1817. | ||
Hartling L, Ospina M, Liang Y, et al. Risk of bias versus quality assessment of randomised controlled trials: cross sectional study. Br Med J. 2009;339:b4012. | ||
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials.1996;17(1):1–12. | ||
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. | ||
Braido F, Baiardini I, Compalati E, Bordo A, Canonica GW. Towards the grade of recommendations, assessment, development and evaluation system: methods and results of budesonide/formoterol maintenance and reliever therapy research. Curr Opin Allergy Clin Immunol. 2011;11(4):361–374. | ||
Abildgaard JT, Lonergan KT, Tolan SJ, et al. Liposomal bupivacaine versus indwelling interscalene nerve block for postoperative pain control in shoulder arthroplasty: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2017;26(7):1175–1181. | ||
Hannan CV, Albrecht MJ, Petersen SA, Srikumaran U. Liposomal bupivacaine vs interscalene nerve block for pain control after shoulder arthroplasty: a retrospective cohort analysis. Am J Orthop (Belle Mead NJ). 2016;45(7):424–430. | ||
Namdari S, Nicholson T, Abboud J, Lazarus M, Steinberg D, Williams G. Randomized controlled trial of interscalene block compared with injectable liposomal bupivacaine in shoulder arthroplasty. J Bone Joint Surg Am. 2017;99(7):550–556. | ||
Okoroha KR, Lynch JR, Keller RA, et al. Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: a prospective randomized trial. J Shoulder Elbow Surg. 2016;25(11):1742–1748. | ||
Richard BM, Newton P, Ott LR, et al. The Safety of EXPAREL® (bupivacaine liposome injectable suspension) administered by peripheral nerve block in rabbits and dogs. J Drug Deliv. 2012;2012:962101. | ||
Hida T, Yukawa Y, Ito K, et al. Intrathecal morphine for postoperative pain control after laminoplasty in patients with cervical spondylotic myelopathy. J Orthop Sci. 2016;21(4):425–430. | ||
Kunopart M, Chanthong P, Thongpolswat N, Intiyanaravut T, Pethuahong C. Effects of single shot femoral nerve block combined with intrathecal morphine for postoperative analgesia: a randomized, controlled, dose-ranging study after total knee arthroplasty. J Med Assoc Thai. 2014;97(2):195–202. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




